Pharmocology Exam 2
1/70
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
Emphysema
COPD
Risk factors: smoking, environment, inhaled irritants
cause: irritant is inhaled, the lung responds through Leukocytes releasing proteolytic enzymes into alveoli, and alveoli become inflamed
Alveoli stop being elastic, so gas exchange is decreased (air trapped in the bottom of the lungs)
Chronic Bronchilits
Continuous inflammation and low-grade infection of the bronchi
Excessive mucus secretion
does not really go away + do not breathe as well
Asthma
Recurrent and Reversible Shortness of Breath
Lung airway narrows
Alveolar ducts and alveoli remain open + Airflow is obstructed
Symptoms: Wheezing & Difficulty breathing
2 components:
bronchoconstriction
inflammation
Status Asthmaticus
Prolonged asthma attack that does not respond to typical drug therapy
May last several minutes to hours
medical emergency!
Beta Agonist Bronchodilators
Short-acting beta agonists (SABA)
Rescue inhaler
Albuterol
Long-acting beta agonists (LABA)
For long term management
Salmeterol
Albuterol (Proventil, Ventolin)
RESCUE INHALER
Class - Beta 2 Agonist Bronchodilator
SHORT ACTING
Indications
Asthma
COPD
Mechanism of Action - Dilates bronchioles by relaxing the bronchiole smooth muscle
Adverse effects
Tremor
Paradoxical bronchospasm
Tachycardia
Nursing Implications
Patient teaching: rescue inhaler
Use of spacer
Assess Lung sounds + CV status
Worked = less wheezing
Ipratropium (Atrovent)
Class: Anticholinergic bronchodilator
Indication: COPD
Mechanism of action:
Induces bronchodilation
Blocks muscarinic receptor in airway smooth muscle.
Adverse effects:
Increased IOP with angle closure glaucoma
Paradoxical bronchospasm
Safety:
Usual dose – 2 inhalations/ 4x day
Pregnancy Category C
Peds >12 years old
Assess Lung sounds
Give second or in combo with albuterol
Patient Teaching: How to administer
Evaluate: Pulmonary status + ADR
Theophylline (Theo-Dur)
Class: Xanthine derivative bronchodilator
Indication: Asthma + COPD
Mechanism of action
• Cause bronchodilation by increasing cAMP which causes smooth muscle relaxation
Adverse effects
Nausea, vomiting
Tachycardia, palpitations
Hyperglycemia
Safety
Do not use with other stimulants-caffeine
Do not smoke cigarettes or use tobacco
Nursing Implications
Patient teaching: still keep rescue inhaler
Oral
Fluticasone (Flovent)
Class: Corticosteroid (inhaled)
Indications: Asthma + COPD
Mechanism of action: Reduces inflammation in the airways
Adverse effects
Oral candidiasis 31% (whenever inhaling steroids)
Safety
Do not use for acute distress! Not a rescue inhaler.
Pregnancy Category C
Peds approved
Patient teaching
Rinse mouth and spit out water after dose
Oral care
Evaluation
Not as strong as systemic corticosteroids
you cannot just switch
Prednisone
class: glucocorticoid
indication: Adrenocortical insufficiency, inflammatory diseases or conditions, allergies, organ transplantation, respiratory illness exacerbation
mechanism of action: inhibits inflammatory and immune responses
Adverse effects
hypertension
psychosis
hyperglycemia
abdominal obesity
Safety:
DO NOT STOP TAKING IT ABRUPTLY
adrenocortical insufficiency
may exacerbate or activate infections
diminished response to vaccines
Pregnancy category D
peds: give every other day to avoid growth suppression
Montelukast (Singulair)
Class: Leukotriene antagonist
Indications: Asthma + Allergies
Mechanism of Action
Blocks leukotriene receptors in airway
Blocks inflammatory response responsible for asthma + allergies
Adverse effects:
Headache
Nausea + diarrhea
Major personality changes
Suicidal Thoughts
Safety
March 2020 FDA warning about neuropsychiatric effects
Implementation
Give in the evening
Not used as a rescue medication
Histamine
A natural chemical in the body that causes inflammation
Allergic rhinitis
Anaphylaxis
Angioedema
Insect bite reactions
Urticaria (hives) & pruritus (itching)
Antihistamines
end in -ine
H1 antagonists (a.k.a. “H1 blockers”, “antihistamines”) - allergy meds
diphenhydramine (Benadryl)
H2 antagonists (a.k.a. “H2 blockers”): Reduces gastric acid in peptic ulcer
disease
Mechanism of action:
Blocks action of histamine at H1 receptor sites
Competes with histamine for binding at unoccupied receptors
Limitations: Cannot push histamine off the receptor if already bound
Prevents the actions of histamine rather than reversing them
Give early in treatment before all the histamine binds to the receptors
Anticholinergic effects:
Dry mouth
Difficulty urinating
Drowsiness
Diphenhydramine (Benadryl)
Class: Histamine 1 antagonist, 1st generation
Indications: Allergies, hives (urticaria), pruritis (itching), Sleep aid
Mechanism of Action
Blocks H1 receptors in respiratory, GI tract, & blood vessels.
Adverse effects
Anticholinergic side effects
Sedation
Safety
Can cause drowsiness, use caution when driving or operating machinery
Elders – higher risk of sedation and confusion
Pregnancy Category B
Nasal Decongestants
reduce congestion that occurs with allergic rhinitis, sinusitis, common cold
Pseudoephedrine: limits on quantities purchased due to potential to be altered to make meth
MOA: alpha 1 adrenergic activation
vasoconstriction of blood vessels
turbinates shrink, opening nasal passages
Phenylephrine (Neo-Synephrine)
Class: alpha 1 adrenergic agonist
ADR: anxiety, agitation, insomnia
rebound congestion - avoid more than 3 days
precautions: contraindicated in clients with narrow-angle glaucoma, uncontrolled heart disease, hypertension or dysrhythmia
Cough
Cough reflex:
Initiated by irritation of the respiratory tract sensory receptors
Two Basic Cough Types:
Productive (congested, removal of secretions)
Non-productive: dry cough
Antitussives
Drugs used to stop or reduce coughing
Opioid and non-opioid
Used only for nonproductive coughs
Nursing Process:
Avoid in very productive cough
Track total dosage given
See HCP for cough >7days
NOT FOR LONG TERM USE
Codeine
Class: Opioid antitussive
Indications: Non-productive cough
Mechanism of Action
Suppresses cough center in CNS
decreases sensitivity of cough receptors
Adverse Effects:
Dizziness
Drowsiness
Respiratory depression (especially in kids
Nursing Implications
Not available OTC
Has analgesic properties
Restricted use in children
Mix w/ sprite + jolly ranchers
Dextromethorphan “DM”
basically same as Codine
Class: Non-opioid antitussive
Indications: Non-productive cough
Mechanism of Action:
Suppress the medullary cough reflex
decreases sensitivity of the stretch receptors in the respiratory tract
Adverse effects:
Dizziness
Drowsiness
Nausea
Safety
Can be found in OTC combination cold medicine
Drug of abuse (can cause hallucinations)
Pregnancy Category C
Peds - not for OTC use in children <4 years of age
Expectorants
Drugs which aid in mucus removal
Reduces secretion viscosity
Indications: Relief of productive coughs associated with:
Mechanism of Action:
make mucus easier to cough up by stimulating secretory glands to put more water into mucus
Guaifenesin (Mucinex, Robitussin)
Class: Expectorant
Indications: Relief of productive cough
Mechanism of Action: Thins secretions + Increases efficiency of cough
Adverse effects: Nausea + Vomiting
Safety
Pregnancy Category C
Peds – Approved > 4 yr
Administer with plenty of water
Risk for overdose with other drugs
Blood Pressure
BP = CO x SVR
Blood Pressure = Cardiac Output x Systemic Vascular Resistance
CO = heart rate x stroke volume
SVR = the resistance to the blood flow
Renin-Angiotensin-Aldosterone System (RAAS)
regulates BP
ACE inhibitors = “-PRIL”
Angiotensin receptor blockers = “-SARTAN”
Captopril (Capoten)
Class: ACE inhibitor
Indication: HTN, HF, used alone or in combination with diuretics or other antihypertensives, renoprotective effects on kidneys
Mechanism of action: decrease SVR → vasodilation and cause diuresis
inhibit ACE (AI → AII)
inhibits vasoconstriction → decreases SVR
inhibits aldosterone → water is not retained
Adverse Effects: Dry, non-productive cough, hypotension, hyperkalemia, ANGIOEDEMA
Losartan (Cozaar)
Class: Angiotensin Receptor Blocker (ARB)
Indication: hypertension, HF
Mechanism of action:
block the binding of Angiotensin II to it’s receptor
blocking vasoconstriction (vasodilation)
blocking aldosterone secretion (decreased preload)
Adverse Effects:
fatigue, chest pain
cough less likely than with ACE inhibitors
Calcium Channel Blockers
Mechanisms of action:
relaxes coronary arteries and increases blood supply to the heart
dilates peripheral arteries → decreases workload of the heart
Decreases BP
diltiazem also decreases heart rate and contractility
Diltiazem (Cardizem)
Class: calcium channel blocker
Indications: hypertension, angina, dysrhythmias, cerebral artery spasms, heart failure
Mechanism of action:
causes relaxation of smooth muscle by blocking calcium binding
decreases SVR
decreases HR
Adverse effects
hypotension, tachy or bradycardia, constipation or nausea, rash
alpha blockers
Mechanism of Action #1: arterial and venous dilation, reducing peripheral vascular resistance and blood pressure
indication: hypertension
Mechanism of Action #2: effect on receptors on prostate gland and bladder decrease resistance to urinary outflow, thereby reducing urinary obstruction and relieving symptoms
indication: Benign prostatic hyperplasia
Common suffix: -osin
Doxazosin (Cardura)
Indication – hypertension, benign prostatic hyperplasia (BPH)
Mechanism of Action – alpha-1 receptor antagonist
Adverse Effects: orthostatic hypotension, tachycardia, vertigo, sexual dysfunction
Nursing Implications: First dose syncope
Beta blockers
Indications:
Angina – decreases demand for myocardial oxygen
Cardioprotection – inhibits stimulation from circulating catecholamines
Dysrhythmias
Hypertension – ability to reduce sympathetic stimulation of the heart, reducing heart rate and force of contraction
Heart Failure
Glaucoma (topical use)
Migraine headache prophylaxis
Common suffix: -olol, -alol
Adverse Effects: Bradycardia, hypotension,
Contraindications: Asthma/COPD, heart block, pregnancy
Metoprolol (Lopressor, Toprol XL)
Class: Beta Blocker
Indication – angina, MI, cardiac dysrhythmias, hypertension, heart failure
Mechanism of Action – antagonist @ beta adrenergic receptors
Safety
do not discontinue abruptly (black box warning): May precipitate MI, angina, cause rebound hypertension
High alert drug
pregnancy category C/not indicated
Direct Vasodilators
Indication: hypertension, angina
mechanism of action: directly cause peripheral vasodilation by causing smooth muscle relaxation,
decrease SVR
Patient Teaching for antihypertensives
Should not be stopped abruptly → rebound hypertensive crisis → stroke
Medication is only PART of therapy:
diet, stress level, weight, and alcohol intake
Avoid smoking and sodium, limit stress, and decrease caffeine intake
Encourage supervised exercise
AVOID Hot tubs, showers and baths, hot weather, or prolonged
sitting, standing → hypotension → syncope
Report: HF symptoms
Impotence is an expected effect
Should not take any other medications w/out approval
Heart Failure (HF)
The heart cannot pump enough blood to supply the body’s demand for oxygenated blood
Failure of the ventricle to eject blood efficiently results in:
fluid volume overload
chamber dilation
elevated intracardiac pressure
Symptoms:
unusual shortness of breath or difficulty breathing
Edema
weight gain
chest pain, palpitations
excessive fatigue
Cause: anything that causes ischemia or high BP
Types of HF
Left-sided HF: blood backs up into the lungs
fluid volume overload,
chamber dilation
increased intracardiac pressure.
Right-sided HF: blood backs up into the body
venous congestion,
pedal edema
jugular venous distention,
ascites,
hepatic congestion
HF meds
Goals of treatment:
increase cardiac output
decrease workload of the heart
Positive inotropic drugs
drugs that increase force of contraction
Positive chronotropic drugs
drugs that increase heart rate
Positive dromotropic drugs
drugs that accelerate conduction
Digoxin (Lanoxin)
class: cardiac glycoside
Indications: systolic HF and atrial fibrillation
Mechanisms of action:
positive inotropic effect: (stronger contraction)
negative chronotropic effect: (slower HR)
negative dromotropic effect: (decreased conduction)
Narrow therapeutic Index drug: normal = 0.5 – 2 ng/mL
TOXICITY greater w/ low potassium or magnesium
digoxin binds to the K+ site of the Na+/K+-ATPase pump
low serum potassium levels increase the risk of digoxin toxicity
Adverse Effects:
Toxicity → brady/tachycardia, nausea, yellow halos
Antidote: Digoxin Immune Fab (Digibind)
Nursing Implications:
before giving dose, count apical pulse for 1 full minute
HOLD DOSE & CONTACT PRESCRIBER IF:
apical pulse < 60 or > 100 bpm
S/S toxicity
Patient teaching:
avoid giving with high fiber foods
patients should IMMEDIATELY report a weight gain of:
2 lb or more in 1 day or
5 lb or more in a week
Kidney functions + processes
3 basic functions
cleansing of extracellular fluid (ECF) and maintenance of ECF volume and composition
maintenance of acid-base balance
excretion of metabolic waste and foreign substances
3 basic renal processes
filtration: occurs at the glomerulus
reabsorption: 99% of H20, electrolytes and nutrients undergo reabsorption
active tubular secretion: occurs at the proximal convoluted tubule
Diuretics
Act on the kidneys to INCREASE the production of urine → eliminating water
Na+ and H2O play a major role in the regulation of: BV & BP
Decrease Preload
We use drugs that target kidneys to:
decrease hypertension
draw water off the body (decrease edema)
Loop Diuretics
End in “-nide” or “-mide”
Works in Loop of Henle
Drug effects:
Reduces:
BP, PVR, SVR, Central Venous Pressure, left ventricular end diastolic pressure
STRONGEST + MOST POWERFUL DIURETIC
Furosemide (Lasix)
Class: loop diuretic, prototype
Indications: pulmonary edema, edematous states, hypertension, liver impairment (ascites)
Mechanism of Action: acts on ascending loop of henle to block reabsorption of water
Contraindications: hypersensitivity, hypersensitivity to sulfonamide antibiotics, anuria, hypovolemia, electrolyte depletion
Nursing Implications: rapid onset (PO 60 min, IV 5 min)
Assess: renal function + K levels, hearing, lung sounds, urine output
Take Potassium
Adverse Effects:
Hypokalemia
Hypotension
Ototoxicity (give through IV slow or patient will lose hearing)
Thiazide and Thiazide-type Diuretics
Basically same as Loop Diuretics
DO NOT WORK FOR KIDNEY FAILURE
Hydrochlorthiazide (Hydrodiuril)
Class: Thiazide Diuretic
Indications: essential hypertension, HF, edema, diabetes insipidus
Mechanism of Action: inhibition of the resorption of Na, K, Cl, resulting in osmotic water loss @ the distal convoluted tubule
result is increased Na+ in the filtrate, which causes less H2O resorption, which means more H2O is lost in the urine
Adverse Effect:
HYPOKALEMIA
HYPOnatremia
photosensitivity
Nursing Process:
Eat potatoes, bananas, leafy greens, etc.
Potassium-Sparing Diuretics
Mechanisms of action:
Aldosterone antagonists – blocks aldosterone in the distal nephron,
promotes the excretion of Na+ and H2O, but the retention of K+
Non-aldosterone antagonist K+ sparing diuretics
Spironolactone (Aldactone)
class: Potassium-sparing diuretic
indications:
hypertension
to reverse K+ loss caused by thiazide
edematous states
HF
primary hyperaldosteronism
PMS
PCOS
acne in women
Adverse Effects:
HYPERKALEMIA
low BP
Tumors
Drug-Drug Interactions:
Thiazide and Loop diuretics
any agent that raises
potassium levels
Lithium
NSAIDS
Coronary Heart Disease Drugs
Antilipemics
HMG-Co-A Reductase Inhibitors → atorvastatin (Lipitor)
Antianginals
Nitrates → NTG (nitroglycerin)
How does Cholesterol relate to CHD?
The risk of CHD in patients with cholesterol levels of 300 mg/dL is 3-4x greater
Lipoproteins
Very-low-density lipoprotein(VLDL)
From the liver
Transports endogenous lipids to the cells
Low-density lipoprotein (LDL)
deliver cholesterol to cells
used in membranes or for the synthesis of steroid hormones
High-density lipoprotein (HDL)
Responsible for “recycling” of cholesterol
“good cholesterol”
What lowers cholesterol?
Exercise increases HDL + lowers bad cholesterol
FOODS: fatty fish, olive oil, whole grains, fruits, vegetables, red wine, tea, etc.
There is a genetic predisposition to high cholesterol
Statins
end in -statin
Mechanism of Action: Lower blood cholesterol by decreasing the production of cholesterol.
Inhibit HMG co-A reductase (enzyme necessary for liver to produce cholesterol)
Adverse Effects:
Constipation
Myalgias (muscle aches/pains)
Rhabdomyolysis (damaged muscle gets into the bloodstream) - limit grapefruit juice
Contraindications: Pregnancy+ Liver Disease
Patient Teaching
Report signs of myopathy immediately
Caution with grapefruit juice
Evaluation
Cholesterol, lipid profiles
Liver enzymes
Muscle pain, weakness
Anti-anginal Drugs
GOAL = BALANCE OXYGEN SUPPLY AND DEMAND IN THE MYOCARDIUM
Causes of Angina
SUPPLY:
when blood supply to the heart is inadequate → PAIN
damaged cardiac cells/tissue resulting from inadequate O2 supply = ISCHEMIC HEART DISEASE
primary cause: ATHEROSCLEROSIS
blood vessels become narrow with fatty deposits in the walls
DEMAND:
the harder the heart works, the more oxygen it needs
heart rate
contractility
Types of Angina
CHRONIC STABLE ANGINA
caused by atherosclerosis
triggered by exertion, better w/ rest
UNSTABLE ANGINA
caused by coronary artery disease
precedes MI, gets progressively worse
VASOSPASTIC ANGINA
spasms in smooth muscle vasculature of the heart
occurs at rest
Goals of Antianginal Therapy
Mechanisms of Action
decrease HR
decrease contractility
decrease preload (by venous dilation)
decrease afterload (by decreasing diastolic bp)
Calcium Channel Blockers
diltiazem(Cardizem)
Beta-Blockers
metoprolol,atenolol
Nitrates
nitroglycerin (NTG) (Nitrostat, Nitrobid)
Nitroglycerin (NTG)
class: antianginal, vasodilator
indication: all types of angina
mechanism(s) of action:
dilates all blood vessels, including coronary arteries
reduces preload and myocardial oxygen demand
adverse effects
reflex tachycardia
hypotension
tolerance
Pharmacokinetics: large 1st pass
effect when given orally
Sublingual tablets or spray: FAST
IV: emergency
Paste/Ointment: slow
Transdermal patches: slow
Nitroglycerin (NTG) Patient Education
IF ANGINA PAIN OCCURS:
STOP ACTIVITY & sit or lie down and take a SL tablet
IF there is no relief in 5 minutes, call 911 + take a 2nd SL tablet
if there is no relief in 5 minutes, take a 3rd SL tablet
DO NOT TRY TO DRIVE TO THE HOSPITAL
burning/tingling sensation will be felt with sublingual dosage (still potent)
keep a fresh supply of SL medication on hand
Stored in an airtight, glass bottle with a metal cap and no cotton filler
Do NOT use with phosphodiesterase 5 inhibitors (ex. Viagra, Levitra, etc.)
will cause profound hypotension
Drug free 10-12 hours DAILY (tolerance)
Encourage angina journal
Anticoagulants
Have no direct effect on a blood clot that is already formed
Prevent intravascular thrombosis by decreasing blood coagulability
Used prophylactically to prevent:
Clot formation (thrombus)
An embolus (dislodged clot)
Inhibit the action or formation of clotting factors, prevents clot formation
EX: Heparins, Vitamin K antagonists (warfarin), Direct Oral Anticoagulants
Indications:
Used to prevent clot formation in certain settings in which clot formation is likely:
MI
Unstable angina
Atrial fibrillation
Indwelling devices, such as mechanical heart valves
Major orthopedic surgery- post op prevention of blood clots
Heparin
Classification – Anticoagulant
Mechanism of action – Inactivates clotting factors. Factor Xa/thrombin inhibitor. Does not lyse clots.
Adverse Effects:
Bleeding
Heparin induced thrombocytopenia (HIT)
Overdose or toxicity: protamine sulfate = reversal agent
Safety:
High alert med
Toxicity:
Symptoms: hematuria, melena (blood in the stool), petechiae, ecchymoses, and gum or mucous membrane bleeding
Stop drug immediately
IV protamine sulfate: 1 mg of protamine per 100 units of heparin.
Assessment
Baseline coagulation labs, PT, PTT, INR
Implementation
Double-check check dose with another nurse
SubQ
Patient Teaching – report bleeding, bleeding precautions
Evaluation
Partial thromboplastin time (PTT) or Activated PTT (aPTT)
Monitor for signs of hemorrhage
Enoxaparin (LMWH)
Classification - Anticoagulant
Indications: prevent blood clots
Mechanism of action: anti-Factor X and anti-thrombin activity. Does not lyse clots.
Black Box warning: Epidural or spinal hemorrhage, delay catheter placement until enoxaparin has lapsed, hold dose for 4+ hours after placement or removal of catheter
Warfarin (Coumadin)
Mechanism of action:
Vitamin K antagonist: inhibits vitamin K synthesis by bacteria in the GI tract
Inhibits production of vitamin K-dependent clotting factors II, VII, IX, and X
Final effect prevention of clot formation
Pharmacokinetics: longer acting than heparin
Adverse Effects:
Bleeding
Toxicity
Discontinue the warfarin.
May take 36-42 hours before the liver can resynthesize enough clotting factors
Vitamin K1 can hasten the return to normal coagulation.
Severe bleeding
Safety
Black Box warning – Major/fatal bleeding, monitor PT/INR, prevent bleeding risks
Antidote: Vitamin K
Pregnancy category X
Implementation
High alert drug!
Patient Teaching
Avoid activities the risk cuts, bruising, or injury. Soft toothbrush, etc
Keep same diet
Evaluation
INR
Signs of bleeding
Antiplatelet drugs
Mechanism of Action: prevent platelet adhesion
Ex: aspirin (Ecotrin) + clopidogrel (Plavix)
Indications:
Prevention of stroke or transient ischemic attack (TIA)
Post MI prevention of thrombus
aspirin (acetylsalicylic acid, ASA)
Classification: Salicylate, NSAID, Antiplatelet agent
Mechanism of Action: inhibits the activation of Thromboxane A2→inhibits the enzyme cyclooxygenase in the platelet→ prevents formation of thromboxane
leads to less platelet aggregation, less vasoconstriction
makes it difficult to form platelet plug
Irreversible effect: antiplatelet effects last 7-10 days
Dosage: 81-325mg/day for antiplatelet effect
Safety:
Narrow therapeutic index at high doses
Don’t use with renal, hepatic failure, ulcers
Developmental concerns
Don’t use in 3rd trimester
Peds – don’t use without specific prescription
Reye’s syndrome
Assessment
Why are you giving it
Contraindications: anticoagulants
Implementation
Give with a full glass of water
Patient Teaching
Max dosage in day: 3-4 g
Reduce amount with tinnitus
Evaluation
Tinnitus
Apply direct pressure longer for bleeding
Clopidogrel (Plavix)
Classification – Platelet Aggregation Inhibitor, ADP inhibitor
Mechanism of action – Irreversibly binds to platelet ADP receptor, prevents platelet aggregation. Platelet lifespan 7-10 days
Adverse Effects:
Bleeding
Flu-like symptoms
GI symptoms
Safety
herbal supplements may increase risk of bleeding
Ginkgo biloba, feverfew, evening primrose oil
interactions: PPI’s reduce antiplatelet effects
Black Box warning for CYP2C19 poor metabolizers – low dose or other treatments
Stop one week before surgery
Evaluation
CBC, Platelets
Thombolytic Drugs
Mechanism of action: breaks down existing clots by activating the conversion of plasminogen to plasmin (breaks down clots)
Ex: streptokinase (NMNEC), alteplase
Indications:
Myocardial infarction
Pulmonary embolism
DVT or arterial thrombosis
Catheter occlusion
Acute ischemic stroke
T-PA Tissue plasminogen activator (Alteplase)
Classification - Thrombolytic
Pharmacodynamics – Binds to fibrin, activates plasminogen to plasmin, initiates fibrinolysis. Dissolves clot
Adverse effects:
Internal, intracranial, or superficial bleeding
Cardiac dysrhythmias
Toxicity
Contraindications
Active internal bleeding
Recent major surgery, trauma, stroke
Severe uncontrolled hypertension
AV malformation
Aneurysm
Implementation
monitoring
Time is critical
IV sticks before administering
Patient Teaching: report headache, stroke S/S
Evaluation
Signs of reperfusion
Ventricular dysrhythmias
Resolution of S/S
Bleeding
never give with drugs that enhance bleeding
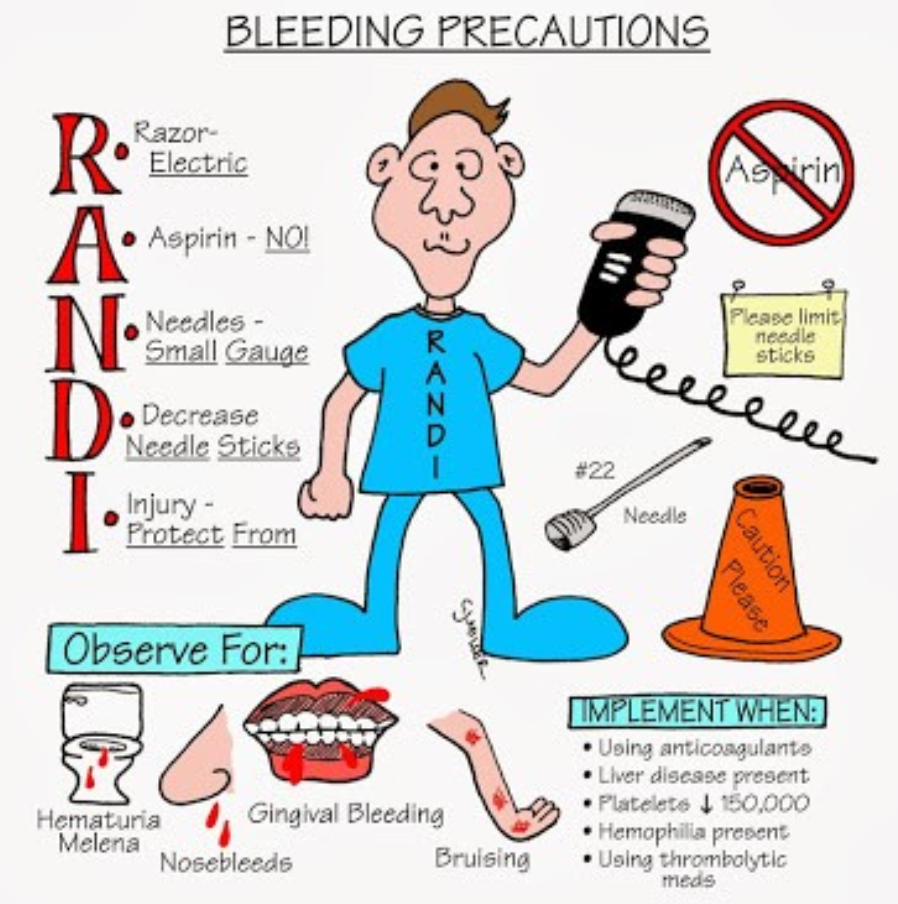
Bleeding precautions
Epoetin alfa
Hematopoietic Drug
E for Erythrocyte
Mechanism of action: promote synthesis of blood components.
Beneficial during cancer treatment because it counteracts bone marrow suppression
Synthetic erythropoietin
Stimulates red blood cells in the bone marrow
Adverse Effects:
Hypertension related to increased HCT
heart failure
malignancies
Patient Safety:
report headache, sudden chest pain, unilateral weakness, numbness or paralysis, vision changes, N/V or seizure
Interventions: monitor - hemoglobin+ BP
Contraindications
hypersensitivity
uncontrolled HTN
malignancies
Administration
baseline BP, CBC, H & H, BUN
do not shake vial or mix with other drugs