Obstructive Lung Disorders (Asthma, COPD, Sleep Apnea, Cystic Fibrosis, Bronchial Disorders)
1/111
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
112 Terms
allergic/atopic asthma
chronic inflammatory disease causing narrowed airways reversible by bronchodilators
S/sx: wheezing, dyspnea, cough, chest tightness
→no cure, can be managed by bronchodilators and avoiding triggers to prevent exacerbations
allergic/atopic asthma
What is the second leading chronic condition in children, behind obesity?
allergic/atopic asthma
Etiology
1. Genetic
2. Enviromental (exposure to dust mites, molds, pollen, etc)
3. Tobacco smoke early on
4. Viruses/bacterial (RSV commonly associated with risk)
5. Obesity (strong link)
6. Occupational Exposures (bakers, farmers, detergent)
allergic/atopic asthma
Pathophysiology
Associated with IgE antibody hyper-reactivity
1. IgE binds to mast cells
2. mast cells release histamine, prostaglandins and leukotrines (inflammatory markers) = bronchial smooth muscle constriction
3. “bronchial spasms” → chronic inflammation leads to airway remodeling
allergic/atopic asthma
Confirm Diagnosis
1. Spirometry: decreased FEV/FVC1 ratio (obstructive pattern) that markedly improves with albuterol inhaler
OR
Methacholine/histamine challenge (rarely done, makes symptoms and PFT temporarily worse)
NO CXR, CT imaging, Labs
allergic/atopic asthma
Treatment
based on step-up (step-down) therapy
*always check for adherence to medication before stepping up with medication
rule of 2’s
Asthma considered uncontrolled if…
- uses rescue inhaler >2x a week
- >2x nighttime awakenings requiring albuterol/month
- >2x rescue medication refills in the past year
Way to determine need to step up to next level treatment
Albuterol
Beta2 Agonist (_____ (SABA), formoterol (LABA)); bronchodilators, rapid response in asthma treatment
MOA-relaxes airway smooth muscles, stabilize mast cell and prevent release of histamines
SE:Tachycardia, jitteryness
NIH/UptoDate Step 1 treatment (for everyone)
Fluticasone
Inhaled Corticosteroid (ICs);
MOA: Work via Anti-inflammatory effects,
Helps to prevent irreversible airway changes
SE: Hoarseness, oral thrush**Gargle/rinse mouth with water after use
NIH/UptoDate Step 2 treatment (add to Beta 2 agonist)
Singulair (Montelukast)
Adjunct Asthma Medication
leukotriene receptor antagonist (LTRA)
NIH/UptoDate Step 5 treatment (add to increased strength ICs)
oral corticosteroids (OCS)
Can be used daily for very severe asthma, often used short term for asthma flares
NIH/UptoDate Step 6 treatment (add on)
pulmonology consult
What is always recommended when managing step-up therapy for an asthma patient in steps 4-6 (NIH/UptoDate guidelines)?
Step 4: increase strength of inhaled steroid
Step 5: increase strength of steroid and add adjunctive therapy
Step 6. Add Oral steroids (chronic maintenance)
GINA
Step 1 and 2: low-dose inhaled corticosteroid-LABA prn (Budesonide-Formoterol, Symbicort)
Steps 3,4,5: increase low-dose maintenance ICS-LABA
Which asthma treatment guideline?
NIH/UptoDate
Step 1: Albuterol PRN for symptoms
Step 2: Albuterol PRN + inhaled corticosteroid (ICS)
Step 3: Albuterol PRN + inhaled corticosteroid + LABA
—pulmonology consult
Step 4: increase strength of inhaled steroid
Step 5: increase strength of steroid and add adjunctive therapy
Step 6. Add Oral steroids (chronic maintenance)
Which asthma treatment guideline?
LABA
NEVER use _____ as monotherapy for asthma [Black Box Warning]!
[Formoterol (Foradil), Salmeterol (Serevent), Aformoterol (Brovana), Indacaterol (Arcapta), Olodaterol (Striverdi), terbutaline]
↑risk of hospitalization and asthma-related death
→always use in combination with inhaled corticosteroids to eliminate risk
NIH/UptoDate Step 3 treatment
peak flow meter
tool used at home to get quick estimate of lung function (when asthma symptoms are well controlled)
atopic triad
1. Seasonal Allergies (allergic rhinitis)
2. Asthma
3. Eczema (atopic dermatitis)
Components of the ________
asthma exacerbation
acute worsening of asthma symptoms not responding to typical maintenance therapy (can be life threatening)
→precipitated by specific trigger (dust, pollen, infections)
→previous history of severe episodes are predictive
mild
_____ asthma exacerbation
-diffuse wheezing, slight shortness of breath
Tx: nebulized Albuterol or DuoNeb treatment in office
moderate
_____ asthma exacerbation
-increased respiratory effort/risk factors for severe
Tx: albuterol/DuoNeb + Oral/IM steroids (dexamethasone, prednisone, prednisolone)
severe
_____ asthma exacerbation
(marked respiratory distress)
Tx: albuterol/DuoNeb + IM steroids + call 911 for transport to ER
moderate
What type of asthma exacerbation is most common?
Tx: albuterol/DuoNeb + Oral/IM steroids (Dexamethasone, prednisone, prednisolone)
Dexamethasone
What steroid is given in conjunction with albuterol/DuoNeb to treat most adult asthma exacerbations (moderate/severe)?
→Has a long half life and stays in system w/ one time dose
Prednisone
Which steroid should be continued 5-7 days to prevent future flares in conjunction with albuterol/DuoNeb for adult asthma exacerbations (moderate/severe)?
→Do not need to taper if under 10 days
*Prednisolone can be used as an Rx for kids because it is liquid
untreated asthma
Complications of _________
1. recurrent flares (frequent hospitalization - $$$)
2. Chronic inflammation (bronchiectasis/COPD like symptoms)
3. Increased risk of pulmonary infections
4. Pregnancy complications
5. Disputed/poor sleep
6. Short life expectancy (if uncontrolled)
intrinsic asthma
non-allergic asthma usually an adult onset without atopic history NO seasonal allergies or eczema
→may be associated with elevated eosinophils
NOT associated with elevated serum IgE levels
intrinsic asthma
Which variant of asthma typically has an adult onset with NO history of seasonal allergies or eczema?
eosinophilic asthma
more severe, difficult to treat variant of asthma with adult onset
→associated with obesity, nasal polyps and chronic sinusitis
Pathophysiology
high levels of eosinophils (WBC type) in the airways and lungs
→eosinophils release inflammatory markers histamine and leukotriene causing airway constriction
eosinophilic asthma
Which variant of asthma is difficult to treat because it does not respond well to inhaled/oral corticosteroids?
Treatment
immunoglobulins: Benralizumab (Fasenra), Mepolizumab (Nucala), Reslizumab (Cinqair)
Aspirin Induced Asthma (AERD)
adult onset variant of asthma triggered by aspirin/NSAIDS
Pathophysiology
NSAIDs inhibit COX-1 enzyme → reduced prostaglandin production increases leukotriene production → bronchoconstriction and nasal congestion
Samter’s triad
nasal polyps/chronic sinusitis, asthma and aspirin sensitivity
Clinical presentation of Aspirin Induced Asthma (AERD)
Aspirin Induced Asthma (AERD)
Diagnosis
suspect in patients with respiratory symptoms after taking NSAIDs (30min-3 hours after)
Treatment
AVOID NSAIDs
Use leukotriene receptor antagonists (Singulair/Montelukast) if symptoms are not controlled with NSAID avoidance and typical asthma treatments
COPD
progressive lung disease associated with long term smoking (usually 20+ pack years - 90% of patients)
-Includes both Chronic Bronchitis & Emphysema
-majority of patients have combination phenotype
Etiology
-chronic exposure to air pollution, chronic chemical exposure (smoking), fumes from cooking
-1-3% have genetic mutation alpha-1 antitrypsin
COPD
Pathophysiology
-narrowing of airways, excessive mucus production, loss of cilia and destruction of alveoli
Clinical presentation
-progressive dyspnea
-chronic (productive) cough
-DOE (dyspnea on exertion)
-fatigue
-frequent respiratory infections
COPD
Diagnosis
chronic cough for 3+ months in a year for 2 consecutive years
Ddx
-Congestive heart failure (primary)
-Asthma (reversible)
-Lung Cancer (not mutually exclusive to either diagnosis)
-Interstitial lung disease
-Bronchiectasis Tuberculosis
-GERD
-Medication side effects (ACE inhibitors)
COPD
Spirometry: obstructive pattern: decreased FEV1/FVC ratio (<0.7) NOT reversible with bronchodilators
Diffusing Capacity of Lungs for Carbon Monoxide (DLCO):
-normal in bronchitis and asthma
-LOW in emphysema (destruction of alveoli reduces gas exchange)
COPD
Which obstructive lung disease is treated with LABA + LAMA combination inhaler (recommended for most patients: Group B)?
COPD
Additional Treatment
1. supplemental oxygen (when O2 <88%)
2. Roflumilast (Daliresp): improves lung function/reduces exacerbations
3. Azithromycin: prophylactic in severe cases
4. Vaccinations, Regular Exercise. Smoking Cessation
5. Pulmonary Rehab referral
COPD
What condition is treated based on severity (objective and subjective findings):
Objective:
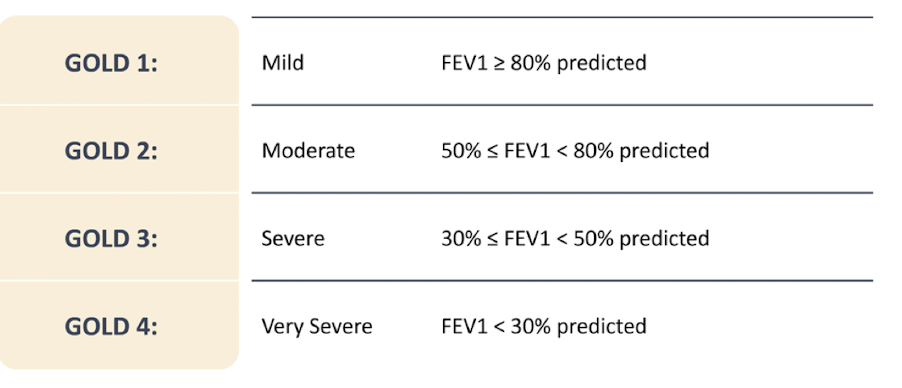
1. Spirometry findings (GOLD grade-primarily FEV1 percentage)
2. Number and severity of exacerbations (“severe” if hospitalized)
Subjective:
1. MRC dyspnea Scale
2. CAT assessment
COPD
What obstructive lung disease are the GOLD Guidelines used to grade severity of airflow obstruction based on post-bronchodilator FEV1?
LABA/LAMA combos
Tiotropium and Olodaterol
Glycopyrrolate and Indacaterol
Glycopyrrolate and Formoterol
Aclidinium and Formoterol
Umeclidinium and Vilanterol
Treatment of COPD (Groups B/E)
emphysema
COPD phenotype: Etiology
Progressive destruction of alveolar membrane leading to decreased surface area of alveoli and impaired gas exchange
-difficulty getting air out “pink puffers”
emphysema
COPD phenotype: Pathophysiology
1. Alveolar cellular breakdown (big and floppy)
→ loss of surface area, hypoxia and hypercapnia (↑CO2)
2. Terminal bronchioles narrow
→ difficult exhaling, hyperinflation and air trapping
3. Capillaries stiffen and narrow
→ decreased blood flow, impaired gas diffusion
emphysema
COPD phenotype: Clinical Presentation
marked dyspnea on exertion
-pursed lip breathing (increase bronchial pressure, helps expel more CO2)
-prominent accessory breathing muscles
-thin and frail (from increased work breathing)
”pink puffers”
Physical exam
hyperinflation of lungs, hyperresonnance to percussion, barrel chested, difficulty getting air out of lungs
emphysema
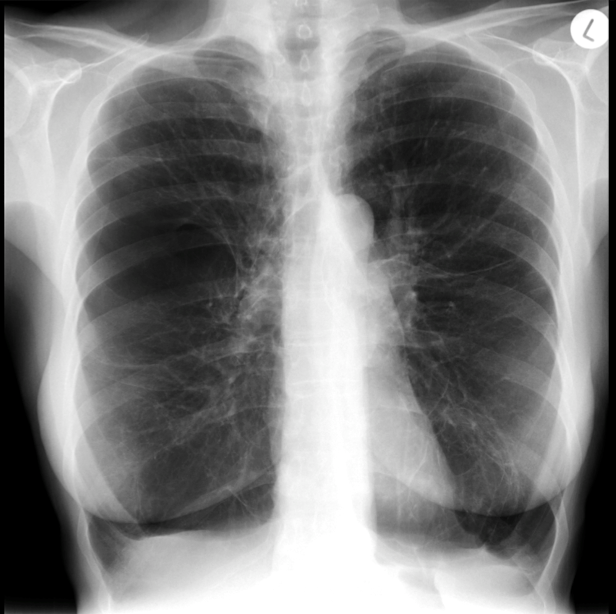
COPD phenotype: CXR findings
Lung Hyperinflation (lungs appear darker than expected)
Lung Hyper-expansion (long lungs, more than 6 anterior ribs or more than 10 posterior ribs)
Flattened diaphragms
Barrel Chest (lateral View)
Small heart
Increased retrosternal airspace (lateral view)
chronic bronchitis
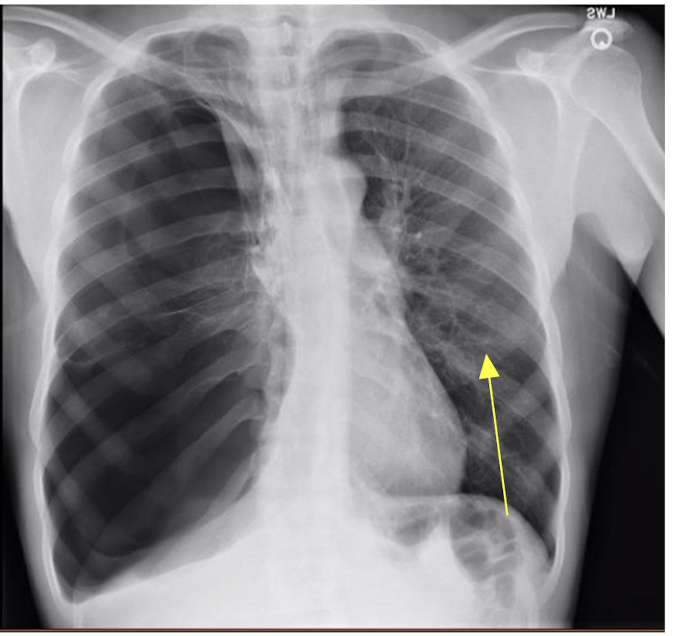
COPD phenotype: CXR findings
-Increased bronchovascular markings
-hyperexpansion of lungs “long lungs”
-Cardiomegaly

chronic bronchitis
COPD phenotype: Clinical Presentation
productive cough (hallmark)
obesity
low oxygen saturation
”blue bloaters”
Physical Exam
wheezing, ronchi, difficulty getting air into lungs
chronic bronchitis
COPD phenotype: Etiology
chronic inflammation of the bronchi (irreversible)
“blue bloaters”
chronic bronchitis
COPD phenotype: Pathophysiology
smoking leads to inflammation of airways →
chronic inflammation leads to structural/functional changes:
1. Narrowed airways (wheezing and dyspnea)
2. Goblet cell hyperplasia (increase mucus production, chronic productive cough)
3. Loss of cilia (decreased mucus/debris clearance, ↑↑risk infection)
infection
What triggers the majority of COPD exacerbations (flares)?
→also air pollution, idiopathic causes
COPD exacerbations
acute worsening of respiratory symptoms relative to patient baseline
Clinical Presentation
increased cough, sputum production, worsening dyspnea, increased inhaler use
COPD exacerbations
Physical Exam
PE: wheezing, tachypnea, tachycardia, fever
Workup: viral NAAT for influenza, COVID, RSV
CXR to exclude pneumonia/other pathology
Guidelines
determine if patient is stable for outpatient treatment (mild, no respiratory distress)
inpatient treatment with respiratory distress, emergent vitals, significant barriers to care/follow up
COPD exacerbations
Treatment
albuterol (nebulized) + oral steroids (prednisone x 5 days) +
antibiotics (Levofloxacin, when viral/flu testing is negative);
-antivirals (Paxlovid/Tamiflu for positive viral testing)
continue LABA/LAMA daily maintenance
Alpha-1 Antitrypsin Deficiency (AATD)
What genetic mutation causes 1-3% of emphysematous changes in younger, non-smoking patients?
→liver damage common
Alpha-1 Antitrypsin Deficiency (AATD)
Which variant of COPD should be suspected?
→young patient, non-smoker, has COPD/emphysema symptoms
→elevated liver enzymes without an obvious cause
→adult onset asthmatics that DO NOT improve on spirometry with bronchodilators
Alpha-1 Antitrypsin Deficiency (AATD)
Pathophysiology
AATD protein normally protects the body from autoimmune destruction of the lungs by neutrophil elastase enzyme
→mutation causes deficient AATD protein, increased neutrophil elastase enzyme damages healthy lung tissue
Alpha-1 Antitrypsin Deficiency (AATD)
CXR findings
diffuse emphysematous changes
”panlobular emphysematous changes” (hallmark)
may see emphysematous bullae
cystic fibrosis
Pathophysiology
autosomal recessive genetic disease, mutation affecting CFTR membrane protein involved in chloride ions
-protein dysfunction= ↓↓secretion of chloride from cell
outer membrane dehydration and thick, viscous secretions in the lungs, pancreas, liver, intestine, productive tract → chronic infections and loss of lung function
CFTR protein
Which protein is affected by an autosomal recessive mutation in cystic fibrosis disrupting the chloride ion gradient (↓extracellular chloride, ↑ intracellular chloride) and thick mucus on outer layer of cells?
cystic fibrosis
Which autosomal recessive condition has a hallmark symptom of thick extracellular mucus and decreased clearing in the respiratory system → chronic infections/inflammation/loss of lung function?
cystic fibrosis
Etiology
childhood infections: Staph aureus/H. influenza
teenage/Adult Infections: Pseudomonas or Staph aureus
Management
Recommend routine sputum cultures (every 3 months) and antibiotics for pulmonary exacerbations
pseudomonas
Which cystic fibrosis exacerbation is treated with respiratory fluroquinolones (Levaquin) and chronic azithromycin and inhaled tobramycin (after sputum culture)?
obstructive pattern
What pattern does cystic fibrosis show on pulmonary function test?
→FEV1 correlated to survival
cystic fibrosis
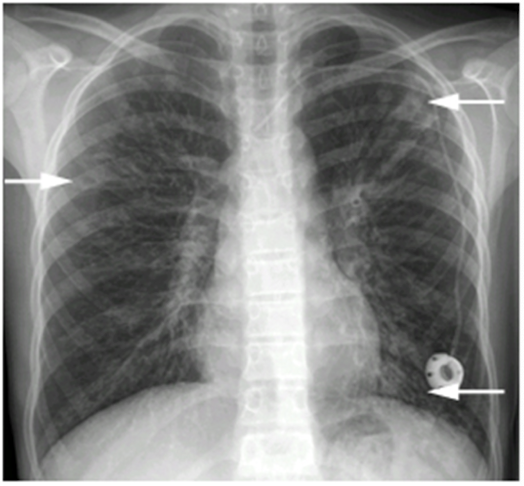
CXR
-lungs hyperinflated
-increased bronchial markings (bronchiectasis) “tram tracks”
-flattened diaphragms
-kyphosis of spine common late in disease
cystic fibrosis
Extrapulmonary manifestation: Pancreatic Effects
→mucus blocks pancreatic secretions → pancreatic enzyme deficiency/pancreatitis
1.Decreased fat absorption – steatorrhea (fatty, oily stool)
-Vitamin ADEK malabsorption, decrease Bone Mineral Density (vit D)
2. Decreased protein metabolism – malnutrition
• Failure to thrive
3. Insulin insufficiency – cystic fibrosis related diabetes
cystic fibrosis
Extrapulmonary manifestation: GI Effects
-Meconium ileus (newborn)
-small bowel obstruction after infancy (mimic appendicitis)
-progressive biliary disease/cirrhosis, cholelithiasis (gallstones)
meconium ileus
newborn is unable to pass first stool, 10-20% of newborns with cystic fibrosis
symptoms: abdominal distention, crying, vomiting
cystic fibrosis
Extrapulmonary manifestation: GU Effects
95% of AMAB patients are infertile (absence of Vas Deferens)
AFAB infertility (common)
Delayed puberty
cystic fibrosis
Other Extrapulmonary manifestations
Anemia
DVT
Electrolyte imbalances
Kidney stones
Aquagenic wrinkling - wrinkling palms after water
Spontaneous pneumothorax
Spontaneous hemoptysis
cystic fibrosis
Diagnosis
Patient must have:
-Clinical symptoms consistent with cystic fibrosis OR
-A positive newborn screen OR
-A sibling with cystic fibrosis
AND
-↑ Sweat Chloride Test >60 (routine newborn screening)
- Presence of two disease-causing mutations in the CFTR gene (one from each parent)
-Abnormal nasal potential difference (NPD)
chloride sweat testing
testing done to confirm newborn screening for cystic fibrosis after patient is 2 weeks old
→sweat cells have higher levels of chloride in cell (>60mmol/L)
Elexacaftor-tezacaftor-ivacaftor (ETI) (Trikafta)
approved for people >2yo with cystic fibrosis
MOA: CFTR modulator can almost completely prevent symptoms by targeting the abnormal protein to make it functional and open chloride ion channel
*Not all genetic mutations will respond to ETI therapy
→Take with fatty foods twice daily, avoid grapefruit, dosing age/weight dependence
Side effects: monitor elevated liver functions (AST/ALT)
Percussion vest (daily therapy) to help with mucus clearing
Ivacaftor
approved for kids 1 month to 2 years old with cystic fibrosis
→switch to ETI at age 2
Percussion vest (daily therapy) to help with mucus clearing
cystic fibrosis
-Manage hydration (helps keep mucus thin)
-Manage inflammation (steroids for flares)
-Azithromycin (maintenance for pseudomonas on culture)
-Treat infections with antibiotics
-Prevent Infections
-Increase sputum clearance – percussion vest, massage
-Nutrition (tight glucose control with diabetes)
-Treat complications
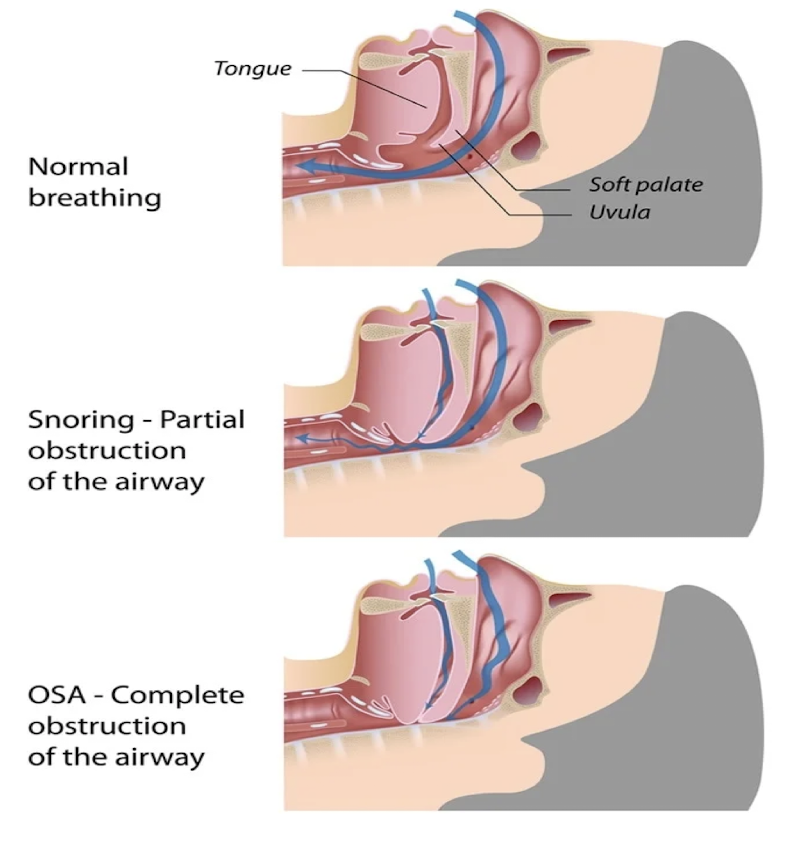
Obstructive Sleep Apnea (OSA)
Repeated episodes of upper airway obstruction during sleep (most common)
- Poor sleep impacts EVERYTHING
- obesity and alcohol use (most common)
S/S: Snoring (common, but not always present)
-morning headaches (bifrontal/squeezing), daytime sleepiness, mood changes, lack of concentration, nighttime awakenings w/ choking/gasping
Obstructive Sleep Apnea (OSA)
Risk Factors
Obesity, neck circumference, alcohol use
-Craniofacial Bone Structure
-Tongue size
-Tonsil size (esp. kids)
-Male sex
-Older age
-Smoking? – possible weak link
-Diabetes, CAD and previous stroke - weak associations
Obstructive Sleep Apnea (OSA)
Pathophysiology
-weight of surrounding adipose tissue in the neck and tongue causes pressure/partial airway collapse → apneic episodes
Physical exam
-narrow or crowded oropharynx (Mallampati Score, Friedman tongue position)
-obesity (BMI>30)
-large neck circumference (>17in males; >16in female)
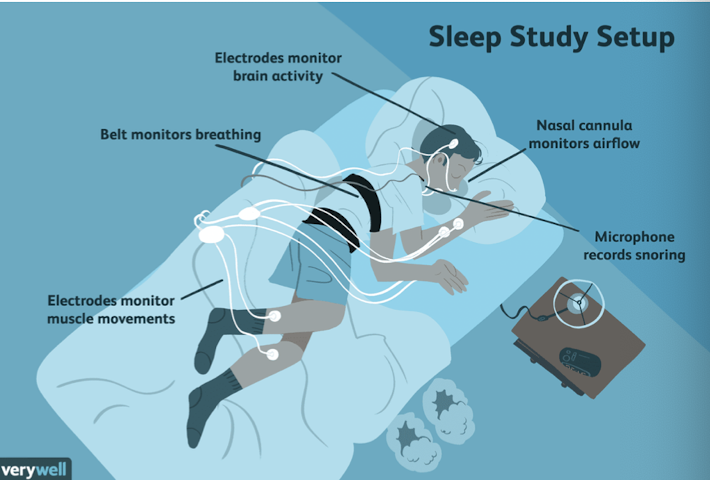
Obstructive Sleep Apnea (OSA)
GOLD STANDARD for DIAGNOSIS:
overnight sleep study or polysomnography (PSG) in sleep lab
→especially airline pilots, police, bus drivers, security workers
Alternative
Home testing → for high likelihood symptoms, if negative send for further testing in lab
Obstructive Sleep Apnea (OSA)
Diagnosis
1. 5-14 apneic/hypopnea episodes per hour AND one sleep related condition (daytime sleepiness, fatigue, snoring, apneas
hypertension, mood disorder, CHF, stoke, DM2, A. Fib, CAD)
or
2. 15+ apneic/hypopnea episodes per hour
Obstructive Sleep Apnea (OSA)
Treatment
Mild cases: weight loss may be curative
Moderate/Severe: Weight loss + PAP therapy
→CPAP therapy: lifelong, “continuous positive airway pressure” prevents airway collapse
*surgery can be an option if refractory to PAP therapy
→Tonsillectomy (kids), uvuloplasty, maxillomandibular advancement, nasal polyp removal
-bariatric surgery (weight loss)
-hypoglossal nerve implant surgery
Obstructive Sleep Apnea (OSA)
Patient Education
Weight Loss may help with symptoms
Avoid alcohol
Avoid sleeping on back
Physical activity
Exercise
Smoking cessation
PAP treatment adherence
Pediatric Sleep Apnea
Risk Factors: Obesity and tonsillar hypertrophy
~affects an estimated 1-5% of kids
S/S: Associated with decreased growth and weight (reverses with treatment)
Dx: polysomnography in sleep center (home testing NOT recommended)
Tx: tonsillectomy, weight loss, CPAP
Pt ED: avoid second hand smoke, weight loss
Central Sleep Apnea (CSA)
Associated with heart failure, stroke, chronic opioid use
-Apneic episodes from nervous system disruption, chemoreceptors failure to respond to CO2 levels
(no airway obstruction)
- May be associated with Cheyne-Stokes breathing
Cheyne-Stokes breathing
breathing pattern characterized by repeated hyperventilation followed by apneic episodes (central sleep apnea)
→associated with heart failure and strokes, poor prognosis
Central Sleep Apnea (CSA)
Pathophysiology
-central chemoreceptors fail to respond adequately to increasing CO2 levels that control respirations and causes apnea/hypoventilation
→hypoventilation can cause respiratory acidosis
S/S: Snoring (common, but not always present)
- Daytime sleepiness, mood changes, lack of concentration, awakenings w/ choking/gasping, morning headaches
Central Sleep Apnea (CSA)
Tx: Acetazolamide (Diamox)
- Goal: Improve symptoms/overall health outcomes
- Mild OSA = Weight loss (may be curative)
- Mod/Severe = Weight loss + PAP therapy
Pt ED:
- reduce opioids, treat underlying heart failure, phrenic nerve stimulation
Acetazolamide (Diamox)
What medication can be used to treat central sleep apnea?
- Causes central acidosis which leads to respiratory compensation and increase in ventilation
obesity hypoventilation syndrome
Epidemiology/Etiology
associated with obstructive sleep apnea, affects 10-20% of patients with obesity (middle age/males)
-higher prevalence with BMI >40
impaired ventilation and respitaroy muscle function as a result of severe obesity
obesity hypoventilation syndrome
Pathophysiology
—chronic hypoventilation (↑ CO2) due to impaired breathing mechanism → hypoxemia and hypercapnia, especially during sleep
Clinical Presentation
-daytime hypoventilation (dyspnea, lethargy, morning headaches)
-OSA symptoms (snoring, apneas)
-cyanosis, peripheral edema, right sided heart failure (advanced cases)
obesity hypoventilation syndrome
What syndrome of chronic hypoventilation puts patients at risk for pulmonary hypertension and cor pulmonale (right sided heart failure)?
Tx: weight loss, CPAP/BiPAP, supplemental oxygen, manage heart failure/pulmonary hypertension
obesity
What is the biggest risk factor for sleep apnea?
polysomnography (PSG)
What is the gold standard for diagnosing obstructive sleep apnea?
Bronchitis
inflammation of the bronchi causing prolonged cough >2 weeks
-one of the most common complaints in acute care
-often follow viral URI infection (RARELY bacterial, no antibiotics)
Bronchitis
Which bronchial disease is one of the most common complaints in acute care causing prolonged cough >2 weeks?
Bronchitis
Etiology
-most commonly caused by viruses (post-viral irritation/inflammation)
→also by irritants such as wildfire smoke, second hand smoke or air pollutants *RARELY a bacterial infection (antibiotics typically not indicated)
Pathophysiology
URI → inflammation → increased mucus production + inflamed bronchial walls trigger cough reflex, narrow airways leading to wheezing
Bronchitis
Clinical Presentation
prolonged cough (hallmark symptom; ~1-4 weeks, usually 18 days)
-cough can be dry or productive, worse at night
-also wheezing, mild dyspnea, MSK chest pain from cough
-NO systemic symptoms (fever, chills, malaise, myalgias; more likely pneumonia)
Diagnosis
Clinical Diagnosis: Recent URI, Prolonged cough
-normal vitals, well appearing patient
Bronchitis
Treatment
self-limiting disease
-usually NO antibiotics indicated (exceptions based on comorbidities)
Treatment is symptomatic
-cough medicine PRN: Dextromethorphan (OTC suppressant), Guaifenesin (OTC expectorant), Benzonatate (Rx: Tessalon Perles)
-Albuterol inhaler (wheezing)
steroids
What medication is NOT recommended for bronchitis?
Bronchiolitis
Which bronchial disease affects infants and young kids (<3 yo) most commonly by RSV viral infection and is the leading cause of hospitalization in infants/young kids?
Bronchiolitis
inflammation of the small airway (bronchioles) in infants and young kids <3yo
Etiology
most commonly RSV, leading cause of hospitalization in infants/young kids
Causes some form of respiratory distress