Pathology: Diseases of the Esophagus
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
the esophagus extends from what structure to what structure?
from cricoid cartilage to esophagogastric junction
what type of epithelium characterizes the esophagus?
normal non-keratinizing squamous epithelium
what is the function of the lower esophageal sphincter?
prevents reflux of gastric contents into esophagus
what type of muscle is the upper portion of the esophageal wall? lower portion?
upper → striated muscle
lower → smooth muscle
esophageal obstructions can be divided into 2 main categories:
mechanical (atresia, stenosis)
functional (achalasia)
when are esophageal obstructions often discovered?
shortly after birth due to regurgitation while feeding (atresia and fistulas)
what is atresia?
thin, non-canalized cord replaces part of esophagus
where are atresias often located?
usually near tracheal bifurcation
atresia results in what symptoms?
aspiration, suffocation, pneumonia
what are 2 types of mechanical esophageal obstructions?
atresia and stenosis
what is stenosis?
narrowing of esophagus due to fibrous thickening of submucosa and atrophy of muscularis propria
(can be congenital or acquired)
t/f: stenosis is most commonly acquired rather than congenital
true
atresia is often associated with ______.
fistula (connects esophageal pouch to bronchus or trachea)
stenosis may result from…?
inflammation and scarring (caused by chronic GERD or irradiation)
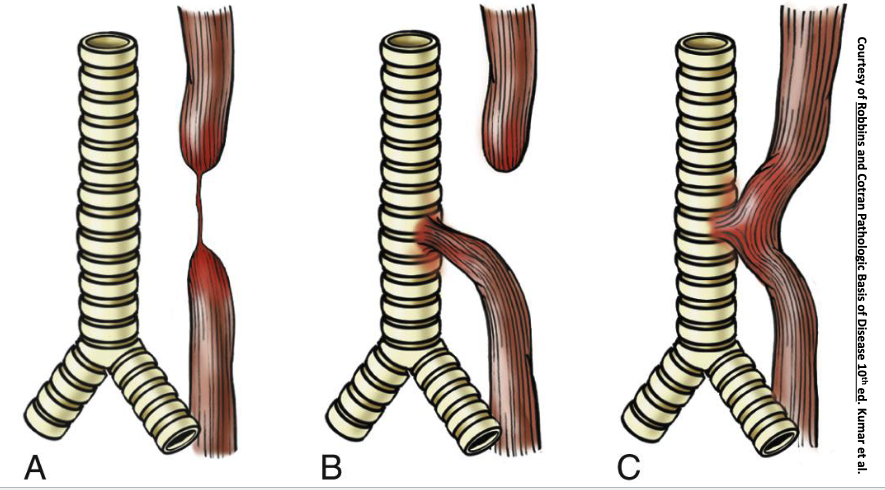
examples of atresia
functional obstructions can result from…?
impaired smooth muscle relaxation of LES
achalasia is associated with a triad of:
incomplete relaxation fo LES
increased LES tone
esophageal aperistalsis
characteristics of primary achalasia?
idiopathic
Failure of distal esophageal inhibitory neurons
Can affect vagus nerve
characteristics of secondary achalasia?
Failure of LES to relax
esophageal dilatation
destruction of myenteric plexus
secondary achalasia can arise in what disease?
Chagas disease (caused by Trypanosoma cruzi infection)
esophageal varices result from…?
portal hypertension
esophageal varices are seen in 50% of patients with what condition?
cirrhosis
what is the first pass effect?
Venous blood from gastro-intestinal tract goes to liver via portal vein
t/f: esophageal varices can be asymptomatic
true
what are esophageal varices?
Results from portal hypertension
Important cause of esophageal bleeding
Dilated vessels that can protrude into lumen of distal esophagus
can rupture and cause massive bleeding
esophageal varices
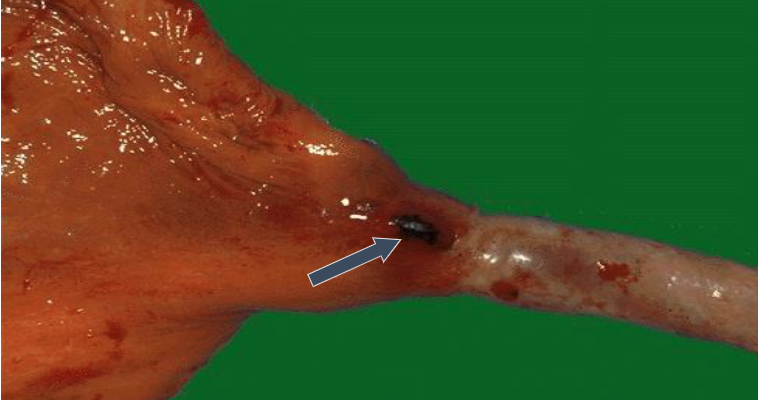
what are 2 possible causes of lacerations of the esophagus? which is the most common cause?
Mallory-Weiss syndrome (most common)
Boerhaave syndrome (severe)
Mallory-Weiss syndrome results from…?
acute alcohol intoxication with severe vomiting
what type of lacerations are caused by Mallory-Weiss syndrome?
Esophagus will have linear and superficial tears and crosses gastro-esophageal junction
what type of lacerations are caused by Boerhaave syndrome?
Rupture of distal esophagus
Transmural tears can affect mediastinum and result in mediastinitis
which cause of esophageal lacerations requires surgery?
Mallory-Weiss syndrome = no surgery
Boerhaave syndrome = surgery needed
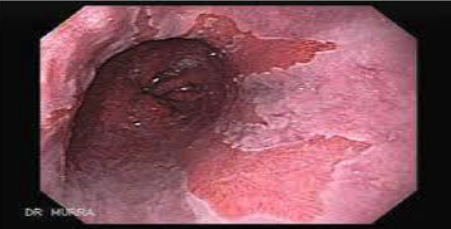
MALLORY–WEISS TEAR
why is Boerhaave’s syndrome more severe than mallory-weiss?
Boerhaave’s is a complete rupture → chest pain + shock
mallory-weiss is an incomplete tear only affecting mucosa and submucosa
what is inflammation of esophagus?
esophagitis
what are the various types/causes of esophagitis?
infectious
eosinophilic
reflux
infectious esophagitis is more common in what pt populations?
immunosuppressed
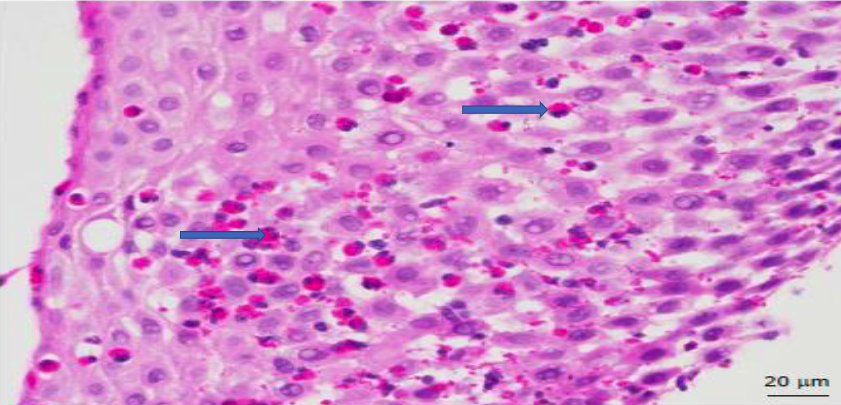
what are the most common infections that cause infectious esophagitis?
Fungal (Candidiasis)
Cytomegalovirus
shallow ulvers and nuclear/cytoplasmic inclusions
Herpes simplex virus
“punched out” ulcers
INFECTIOUS ESOPHAGITIS-HERPES SIMPLEX VIRUS
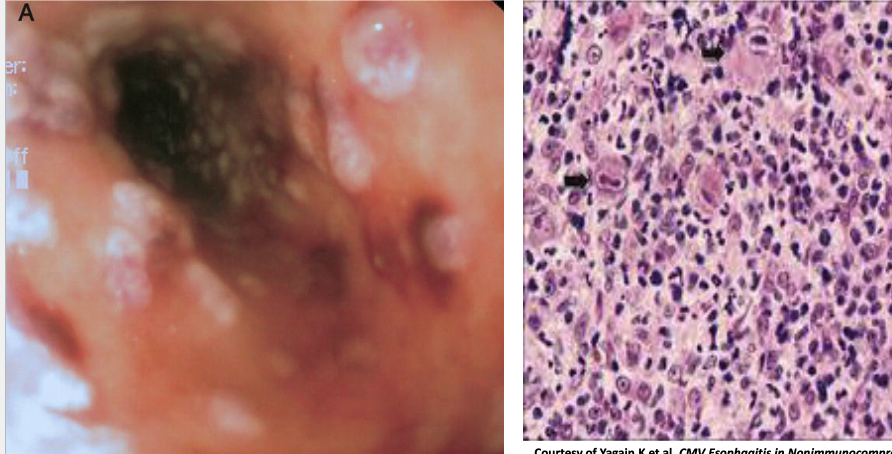
INFECTIOUS ESOPHAGITIS-CYTOMEGALOVIRUS
what is the Chronic immunologic disorder characterized by symptoms related to esophageal dysfunction + eosinophilic inflammation?
Eosinophilic esophagitis
Eosinophilic esophagitis is associated with what type of diseases?
atopic diseease (atopic dermatitis, asthma, allergic rhinitis)
what the symptoms of Eosinophilic esophagitis in adults? children?
adults → food impaction and dysphagia
children → food intolerance or GERD-like symptoms
what is the histopathology of Eosinophilic esophagitis?
Infiltration of eosinophils in superficial aspect of lamina propria and epithelium
Helps to distinguish from GERD and Crohn disease
what are treatment options for Eosinophilic esophagitis?
Dietary restrictions to food allergens
Corticosteroids
Proton pump inhibitors
Eosinophilic esophagitis (increase eosinophils noted)
what is the most frequent cause of esophagitis and most common outpatient gastrointestinal diagnosis?
Reflux esophagitis (GERD)
what is Reflux esophagitis (GERD)?
Gastric contents enter the lower esophagus
Lower esophageal sphincter is relaxed or decreased in tone
Increased abdominal pressure, Alcohol/tobacco use, Pregnancy, Hiatal hernia contribute to GERD
common in adults 40+
what are symptoms of Reflux esophagitis (GERD)?
heartburn
dysphagia
Regurgitation of sour-tasting gastric contents
what are some complications of Reflux esophagitis (GERD)?
Esophageal ulceration
Hematemesis-vomiting blood
Stricture development
Barrett esophagus
what is the treatment for Reflux esophagitis (GERD)?
Proton pump inhibitors
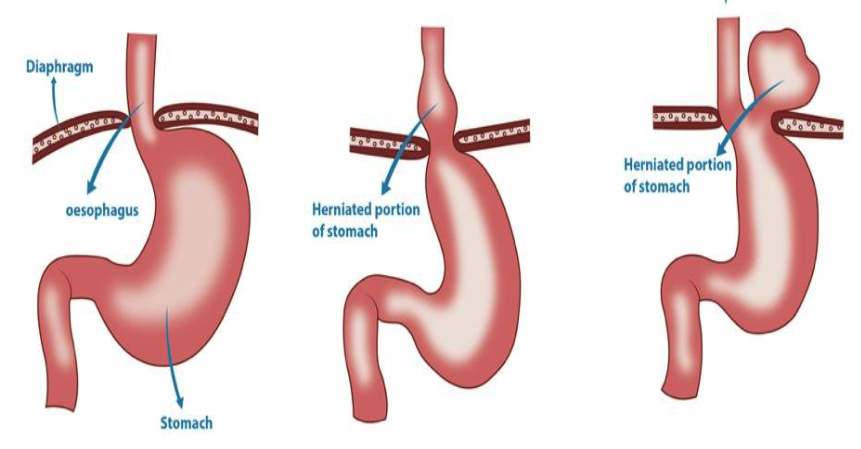
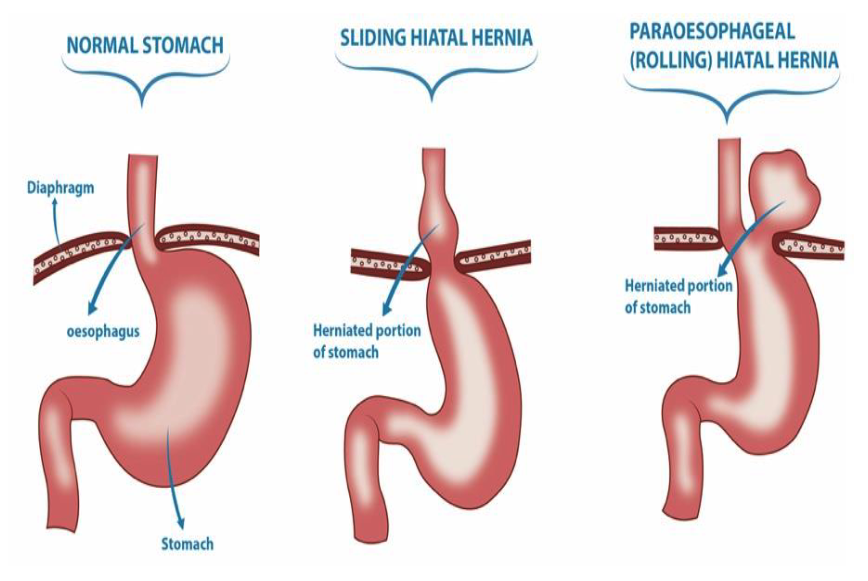
what is the Separation of diaphragmatic crura with protrusion of stomach into the thorax called?
hiatal hernia
t/f: hiatal hernias can be cause for LES incompetence
true
what are the symptoms of hiatal hernias?
can be asymptomatic
similar to GERD symptoms (heartburn, regurgitation of gastric juices)
what are the 2 types of hiatal hernias?
Sliding
Paraesophageal (Rolling)
which type of hiatal hernia is this?
Stomach herniates through diaphragmatic hiatus through which the lower esophagus normally passes
sliding
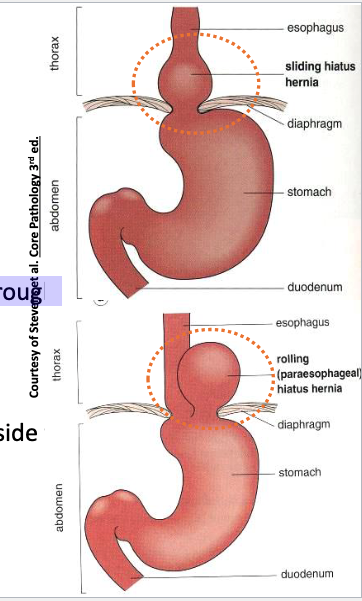
which type of hiatal hernia is this?
Stomach protrudes through a separate defect alongside the esophagus
Paraesophageal (Rolling)
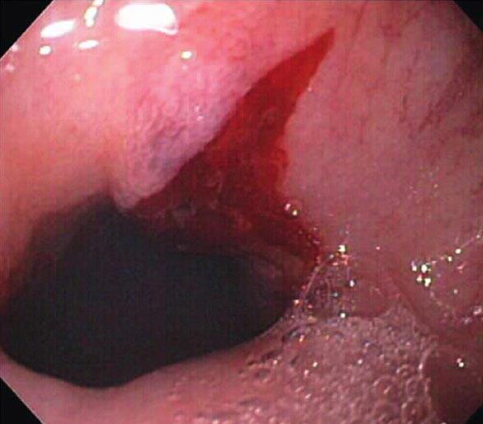
how is Barrett esophagus diagnosed?
endoscopy and biopsy
what is the clinical presentation of Barett esophagus?
Patches of red, velvety mucosa
Extends upward from gastro-esophageal junction
Barrett esophagus is a complication of what other condition?
chronic gastro-esophageal reflux disease (GERD) (10%)
Barrett esophagus presents and increased risk for _________.
adenocarcinoma but most do not develop (0-2-1% per year)
what condition is a premalignant condition characterized by metaplasia of columnar squamous cells to tall, columnar glandular epithelium?
Barrett esophagus (affects lower 1/3 of esophagus)
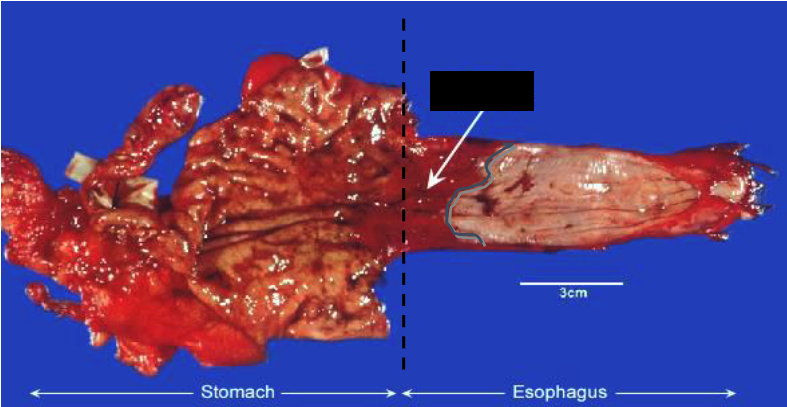
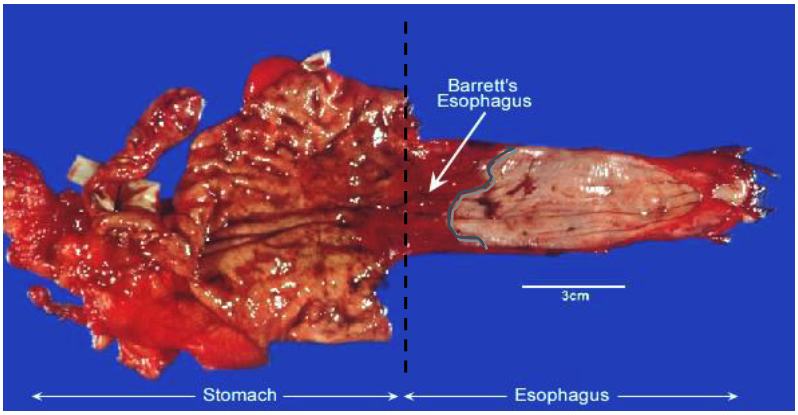
BARRETT ESOPHAGUS
Esophageal adenocarcinoma Can arise from …?
Barrett esophagus
long-standing gastro-esophageal reflux disease (GERD)
Esophageal adenocarcinoma is 7 times more common in men/women?
men
which portion of the esophagus do esophageal adenocarcinomas usually occur?
distal or lower third of esophagus & can invade gastric cardia (stomach)
what are some symptoms of esophageal adenocarcinomas?
Dysphagia
Progressive weight loss
Chest pain
Vomiting
what is the histopathology of esophageal adenocarcinomas?
Formation of glands
Mucin production
pts w esophageal adenocarcinomas have a 5-year survival rate of…?
<25%

ESOPHAGEAL adenocarcinoma
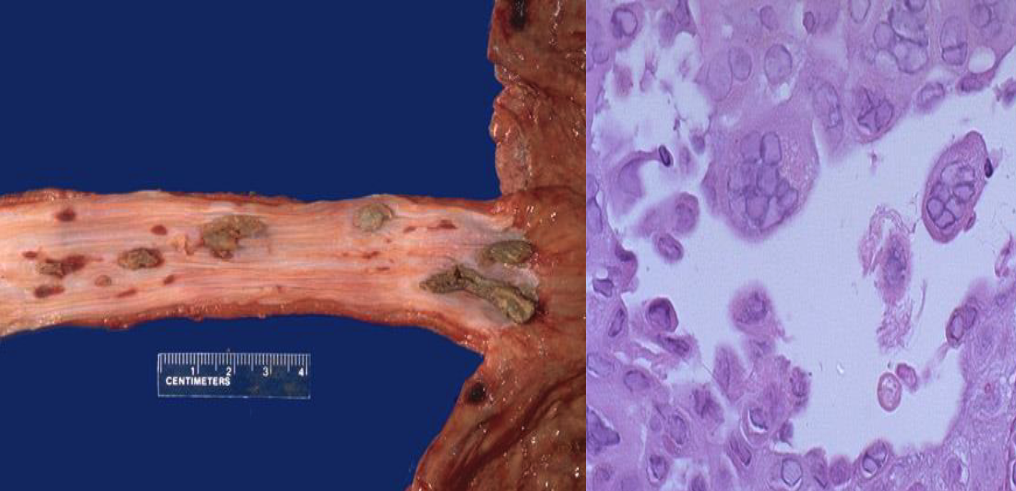
what are risk factors of Esophageal squamous cell carcinoma?
Alcohol and Tobacco use
Achalasia
Frequent consumption of very hot beverages
Plummer-Vinson syndrome
what portion of the esophagus does Esophageal squamous cell carcinoma usually occur?
middle 1/3
what are some symptoms of Esophageal squamous cell carcinoma usually occur?
Dysphagia-difficulty swallowing
Odynophagia-pain on swallowing
Obstruction
epidemiology of Esophageal squamous cell carcinoma?
adults >45 yo
4x more common in men than women
what is the 5-year survival rate of Esophageal squamous cell carcinoma?
<10%

ESOPHAGEAL SQUAMOUS CELL CARCINOMA
Plummer-Vinson syndrome is a risk factor for …?
esophageal squamous cell carcinoma
epidemiology of Plummer-Vinson syndrome?
Have severe iron deficiency anemia
Affects middle-aged and elderly women of Scandinavian origin
Squamous cell carcinoma occur where? (plummer-vinson syndrome)
upper one-third in posterior cricoid area