Eating Disorders and Obesity (Chapter 9)
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Anorexia Nervosa
pursuit of thinness that is relentless and involves behaviours that result in a significantly low body weight
Rats and Starvation
one study found that rats (especially females) that are hungry had less anxiety
staying hungry can be a way to control some type of anxiety
Two Types of Anorexia
restricting type — every effort is made to limit the quantity of food consumed
binge-eating/purging type — some restriction but mainly eat a lot and then purge it
Bulimia Nervosa
uncontrollable binge-eating and effort to prevent resulting weight gain by using inappropriate behaviours
clinical picture is similar to the binge-eating/purging type of anorexia
Two Types of Bulimia
purging — use laxitives/throw up to prevent weight gain
non-purging — increase exercise to prevent weight gain
Clinical Aspects of Eating Disorders
people with anorexia and bulimia share a common preoccupation with their shape and weight
during an average binge, someone with bulimia nervosa may consume as many as 4800 calories
afterwards they will vomit, fast, exercise excessively, or abuse laxatives
people with bulimia nervosa are often preoccupied with shame, guilt and self-deprecation, and efforts at concealment
Binge-Eating Disorder
has some clinical features in common with bulimia nervosa, but people with BED do not engage in inappropriate “compensatory” behaviours
much less dietary restraint in BED
associated with being overweight or obese
Age of Onset for Anorexia Nervosa
16-20
Age of Onset for Bulimia
21-24
Age of Onset for Binge Eating
30-60
Gender Differences in Eating Disorders
recent estimates suggest that there are 3 females for every 1 male with an eating disorder
on established risk factor for eating disorders in men is homosexuality
Prevalence of Binge Eating Disorder
most common form of eating disorder
worldwide lifetime prevalence is around 2.21%
lifetime prevalence is around 2.7% in females and 1.7% in males
prevalence is higher in obese people (6.5 - 8%)
many young people — particularly adolescent girls and young adult women — show some evidence of disturbed eating patterns or have distorted self-perceptions about their bodies
Rates of Anorexia in Sexual Minorities
1.71%
Rates of Bulimia Nervosa in Sexual Minorities
1.25%
Rates of Binge-Eating in Sexual Minorities
2.17%
Percentages of Girls and Boys with Body Image Problems
41.5% of girls
24.9% of boys
Medical Complications of Anorexia Nervosa
mortality rate is more than 5x higher than that for young females ages 15-34 in the general US population
effects the whole body
Anorexia Nervosa — Effects on Brain and Nerves
can’t think right
fear of gaining weight
sad
moody
irritable
bad memory
fainting
changes in brain chemistry
Anorexia Nervosa — Effects on Heart
low blood pressure
slow heart rate
fluttering of the heart (palpitations)
heart failure
Anorexia Nervosa — Effects on Hormones
period stops
bone loss
problems growing
trouble getting pregnant
if pregnant — at higher risk for
miscarriage
having a c-section
baby with low birth weight
postpartum depression
Anorexia Nervosa — Effects on Hair
thinning
brittle
Anorexia Nervosa — Effects on Blood
anemia
other blood problems
Anorexia Nervosa — Effects on Muscles and Joints
weak muscles
swollen joints
fractures
osteoporosis
Anorexia Nervosa — Effects on Kidneys
kidney stones
kidney failure
Anorexia Nervosa — Effects on Body Fluids
low potassium
low magnesium
low sodium
Anorexia Nervosa — Effects on Intestines
constipation
bloating
Anorexia Nervosa — Effects on Skin
bruise easily
dry skin
growth of fine hair all over body
get cold easily
yellow skin
brittle nails
Medical Complications of Bulimia Nervosa
mortality rate = 2x
electrolyte imbalances and low potassium (risk of heart abnormalities)
ipecac syrup, a poison that causes vomiting, can damage the heart muscle
patients usually develop calluses on their hands from sticking them down their throats
tears to the throat can also occur
because the contents of the stomach are acidic, patients damage their teeth when they throw up repeatedly
mouth ulcers and dental cavities are a common consequence of repeated purging
small red dots around the eyes, caused by the pressure of throwing up
swollen parotid (salivary) glands, caused by repeated vomiting (“puffy cheeks” or “chipmunk cheeks”)
Course and Outcome of Eating Disorders
anorexic individuals are 18x more likely to die by suicide than comparably aged women in the general population
even after a series of treatment failures, it is still possible for women with anorexia nervosa to become well again
long-term prognosis for bulimia nervosa tends to be quite good, with high rates of remission
patients with binge-eating disorder also have high rates of clinical remission
even when “well”, many individuals who recover from anorexia and bulimia still harbour residual food issues
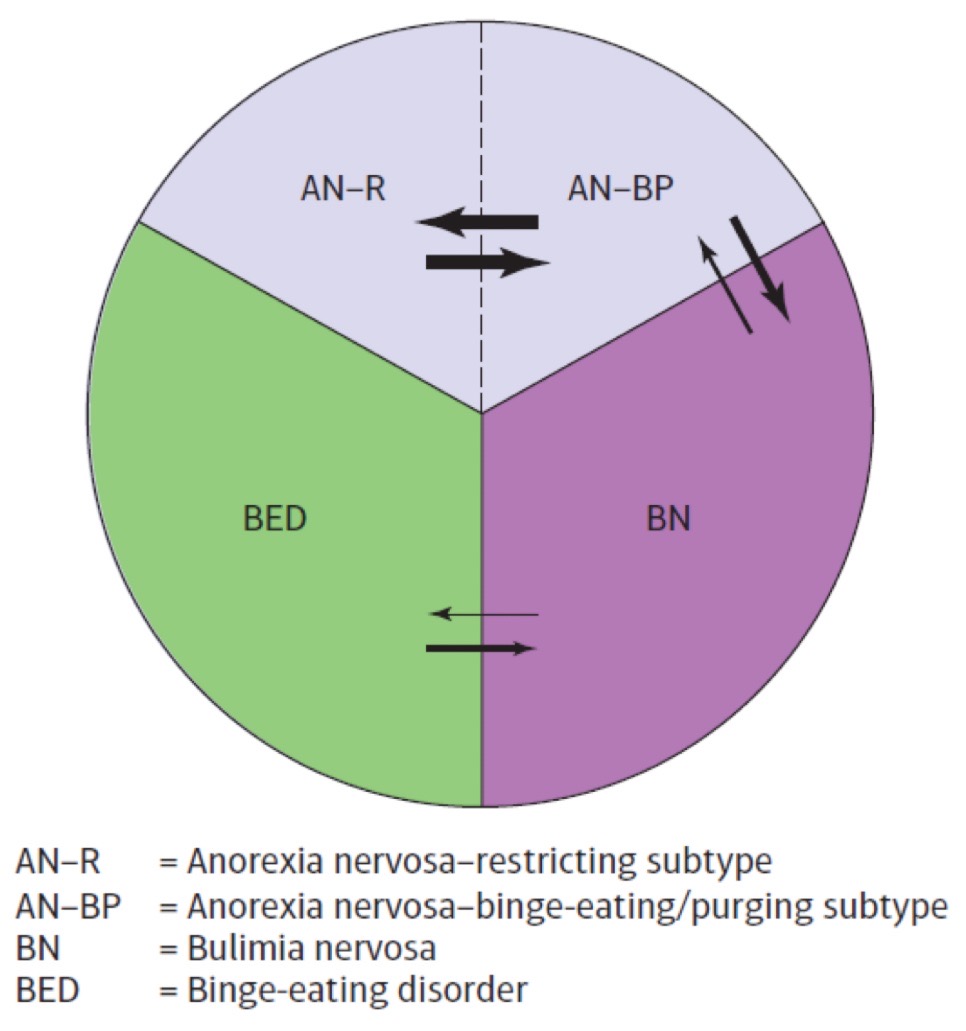
Diagnostic Crossover in Eating Disorders
diagnostic crossover is common in eating disorders with transitions between the two subtypes of anorexia nervosa being very common
transitions from the binge-eating/purging subtype of anorexia nervosa to bulimia nervosa also often occur
Association of Eating Disorders with Other Forms of Psychopathology
70% of patients with an eating disorder will report another comorbid problem
anxiety disorders are most common followed by mood disorders, self-harm, and substance abuse
obsessive-compulsive disorder often found in patients with anorexia nervosa and bulimia nervosa
comorbid personality disorders are frequently diagnosed in people with eating disorders
Cluster C disorders are associated with both anorexia nervosa and bulimia nervosa
Cluster B disorders are more typically associated with bulimia nervosa
Personality disorders are similarly reported in around 30% of patients with BED
Genetic Risk Factors for Eating Disorders
the risk of anorexia for relatives is 11.4x greater than for the relatives of normal controls
the risk of bulimia for relatives is 3.7x higher than for the relatives of healthy controls
studies suggest anorexia nervosa and bulimia nervosa are heritable disorders
recent genome-wide association study found focus for anorexia nervosa
Brain Abnormalities — Risk Factors in EDs
one brain area that plays an important role in eating is the hypothalamus
internal control mechanism (automatic control like hunger)
Set Points — Biological Risk Factors in EDs
our bodies have well-established tendency to resist variation from some sort of biologically determined set point or weight that our individual bodies try to defend
Biological Risk Factors for EDs — Serotonin
implicated in:
obsessionallity
mood disorders
impulsivity
modulation of appetite and feeding behaviour (higher serotonin promotes eating)
active area of research
Reward Sensitivity — Biological Risk Factors for EDs
theory that reward and punishment systems get contaminated:
normally rewarding stimuli such as food become aversive
stimuli associated with self-starvation become valued
Sociocultural Risk Factors for EDs
media such as Vogue and Cosmopolitan exert a great deal of influence in defining the culture’s “ideal body shape” and creating pressures to be thin
social pressures toward thinness may be particularly powerful in higher socioeconomic status background
disordered eating attitudes may predate parent-child conflict
Sociocultural Factors — Anorexia Family Characteristics
rigidity
parental overprotectiveness
excessive control
marital discord
Sociocultural Factors — Bulimic Family Characteristics
high parental expectations
perceiving one’s family to be less cohesive
other family members who are dieting, preoccupied with appearance, or prone to make critical comments about shape/weight
Individual Risk Factors — Gender, Gender Identity and Sexual Orientation
being female is a strong risk factor for developing eating disorders, particularly anorexia nervosa and bulimia nervosa
individuals with a marginalized gender or sexual orientation identity are at increased risk
internalizing thin idea associated with body dissatisfaction, dieting, and negative affect
self-objectification is linked to disordered eating
perfectionism is pursuit of unattainably high standards combined with intolerance of mistakes
may help maintain bulimic pathology through the rigid adherence to dieting that then drives the binge/purge cycle
predates disordered eating in those with anorexia nervosa
also have a genetic basis
Individual Risk Factors — Body Dissatisfaction
sociocultural pressure to be thin
risk factor for development or worsening of eating disorders
Individual Risk Factors — Negative Emotionality
causal risk factor for body dissatisfaction
may also maintain binge eating
predicts dietary restraint in anorexia nervosa
Treatment of Anorexia Nervosa
patients often have little motivation to engage in treatment
high dropout rate from therapy
immediate concern is to restore weight
Treatment of Anorexia — Medications
the antipsychotic medication olanzapine may be benficial
Treatment of Anorexia — Family Therapy
most effective treatment option for adolescent patients
best-studied approach: Maudsley Model
randomized controlled trials show that patients treated with family therapy for 1 year do better than control group
Maudsley Model
typical treatment program includes 10-20 sessions over 6-12 months
parents as a support team
focus on developing healthier relationships
Treatment of EDs — Cognitive Behaviour Therapy
very effective in treating bulimia nervosa
limited success in treating anorexia nervosa
Treatment of Bulimia — Medications
use of antidepressants (anti-anxiety) is common
goal = decrease frequency of binges, improve mood, and decreases preoccupation with shape and weight
Treatment of Bulimia — Cognitive-Behavioural Therapy
leading treatment for Bulimia; superior to medications
“Behavioural” = meal planning, nutritional education, ending binging-and-purging cycles
“Cognitive” = changing the cognitions and behaviours that initiate or perpetuate a binge cycle
new development: transdiagnostic approach to treatment and CBT-E
Treatment of Binge-Eating Disorder
due to the high level of comorbidity with depression, antidepressant medications are sometimes used to treat the disorder
appetite suppressants and anticonvulsant medications are also used
studies suggest that for racial ethnic minorities with BED, interpersonal psychotherapy might work best
BMI and Obesity
body mass index (BMI) is a measure of a person’s weight relative to height
obesity is defined on the basis of having a BMI above 30
Overweight (BMI)
25.0-29.9
Ideal Weight (BMI)
19.0-25.0
Obesity — Medical Issues and Prevalence
increased risk for high cholesterol, hypertension, heart disease, arthritis, diabetes, and cancer
reduced life expectancy of 6-14 years
more prevalent in ethnic minorities (except Asians)
more prevalent in males than in females
Obesity — Weight Stigma
judgement and discrimination from others
weight discrimination is increasing; media is a powerful source
perpetuates weight-based stereotypes
often depicts overweight or obese people in a negative light
weight bias is seen against women who are obese
bias is also seen among healthcare professionals
Obesity and the DSM
obesity is not an eating disorder in DSM-5-TR
some view obesity as a food addiction
the idea the neuroadaptations in the dopamine system plays a key role in obesity is still a relatively new idea
The Role of Genes in Obesity
thinness seems to run in the family
genetic mutation associated with binge-eating is found in only 5% of the obese population
all obese people with the gene reported problems with binge eating
only 14% of obese people without the genetic mutation had a pattern of binge eating
evidence suggests that BMI is polygenic and likely influenced by a large number of common genes
Hormones Involved in Appetite and Weight Regulation
Leptin
inability to produce leptin is associated with morbid obesity
overweight individuals tend to have high levels of leptin, but are resistant to it’s effects
Ghrelin
in Prader-Willi syndrome, chromosomal abnormalities lead to high levels of ghrelin and extreme obesity
Sociocultural Influences on Obesity
diathesis-stress perspective is most appropriate
North America = perfect storm
artificial combination of high fat and high sugar contributes to addictive-like eating
foods with low nutritional value (high fat, high sugar) are also less expensive and much easier to find than foods with high nutritional value
food advertising triggers automatic and unconscious eating
Family Influences on Obesity
family attitudes toward food — their consequences are likely to remain with us for a long time
high-fat, high-calorie diet (or an overemphasis on food) may lead to obesity in family members
eating (or overeating) may be used as a way to alleviate emotional distress or show love
overfeeding infants and young children causes them to develop more adipose (fat) cells and predisposes them to weight problems
if someone close to us becomes obese, chances that we become obese increases by as much as 57%
Stress and “Comfort Food”
when under stress, people and animals eat foods high in fat or carbohydrates
weight gain may be explained in terms of learning principles
we are all conditioned to eat in response to a wide range of environmental stimuli
anxiety, anger, boredom, and depression may lead to overeating
eating in response to such cues is then reinforced because the taste of good food is pleasurable and emotional tension is reduced
Pathways to Obesity
combination of genetic, environmental, and sociocultural influences
binge eating is a predictor of later obesity
binge eating may be caused by:
social pressure to conform to the thin ideal, which leads to dieting followed by binge eating when willpower runs out
depression, low self-esteem, and peer rejection
Treatment of Obesity — Lifestyle Modifications
a first step — a low calorie diet, exercise, and some form of behavioural intervention
among popular diets, a study found Atkins diet lost the most weight
weight watchers — only commercial weight-loss program with efficacy in RCT
“crash” diets and extreme treatments are outmoded and ineffective approaches
Treatments of Obesity — Medications
several medications are approved by the FDS for use in conjunction with a reduced-calorie diet
orlistat (xenical)
lorcaserin (belviq)
contrave
semagultide (wegovy)/ozempic/mounjaro
only modest effects
Treatment of Obesity — Bariatric Surgery
most effective long-term treatment for mobidly obese
reduces food consumed at any time (reduction of stomach size)
weight loss averaging between 44 and 88 pounds