Quiz 4 - Nursing Process #2/ ATD (admit/transfer/discharge), Body Mechanics, Physical Assessment
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Admission
entry of a patient into any health care facility
disorientation
a state of mental confusion as to time, place, or identity
separation anxiety
fears and apprehension (a state of worry/anxiety) caused by separation from familiar surroundings and people)
empathy
ability to recognize and to some extent share the emotions and state of mind of another person, and to understand the meaning and significance of that person's behavior
Considerations for Older Adults during Admission, transfer, and discharge
- will probably be seriously ill
- ATD often result in some level of disorientation
- older adults often have problems with vision, hearing, and more likely to become agitated or fearful and stressed
- transfers within the facility can be confusing and upsetting for older adults
- hospitalized older adults have concern that they may not be able to return to their homes and will need institutional placement (care homes/ assisted living/ SNFs)
- appropriate referrals are important such as: home health nursing, therapy, home nutrition programs, homemaking
- because of hearing problems, healthcare workers have to speak slower to older adults. do not rush the pt. Wait for pts to answer questions
- the change in environment sometimes causes disorientation, loss of appetite, and reversal of sleep-wake patterns.
- relocation is very stressful. ensure that significant others such as family/friends can still support, patient is oriented to new environment, and pt has an opportunity to make decisions about his/her care
Cultural consideration for non-English speaking patient
- contact the appropriate resource (usually the social services dept.) for an interpreter.
Admitting a patient
- admission procedure usually beings with admitting dept.
- they obtain important info such as demographic information (name, address, phone #), insurance info, social security #, and emergency contacts.
- An interpreter should be used if pt does not speak English
- depending on time of admission and facility, the collection of this info may become the responsibility of the nurse
- once necessary identification info is collected, an ID band is placed on the pt's wrist (which contain pt's full name, DOB, or Medical record #). Pt's ID band should always be checked before any procedures/treatments.
- if pt has allergies, a RED allergy wrist band is placed.
patient room orientation
Orientation should include the following:
- Explanation of policies applicable to the pt
- how to adjust the bed and the lights
- how to call the nurse from the bed and the bathroom
- how to operate the telephone/ TV/ radio
- how to use the intercom system if one is present
- the location of lounge areas
- the location of shower and bathroom facilities
- the relationship of the room to the nurses' station
patient teaching during patient admission
- formal teaching plan does not begin until assessment is completed and a care plan is developed
- in an emergency situation, teach pt's family about rationale for any procedures and routines to expect in the pt's care
- ensure that the pt is ready to learn when doing teaching. this can be difficult in the acute setting, as pts may be very sick.
- keep information concise, and focus on topics such as nature of pt's illness, meds needed for treatment, and equipment use for care (such as dressings, ambulatory devices)
- explain shift times and shift changes to pt
- discuss any timelines on when pt may possibly return to work...
- confirm understanding of pt, and explain why you are doing what you are doing and what you will be doing.
- be prepared to repeat information and instructions to pt and significant others because admission/transfers can be stressful moments
- before pt leaves facility, ensure pt will do return demonstration of any skills learned
- teach pts or family about medications
- if there will be a need to transfer a pt to a long-term care facility, obtain the help of social services or discharge planners to ensure that the transfer is appropriate and that it meets the needs of the pt.
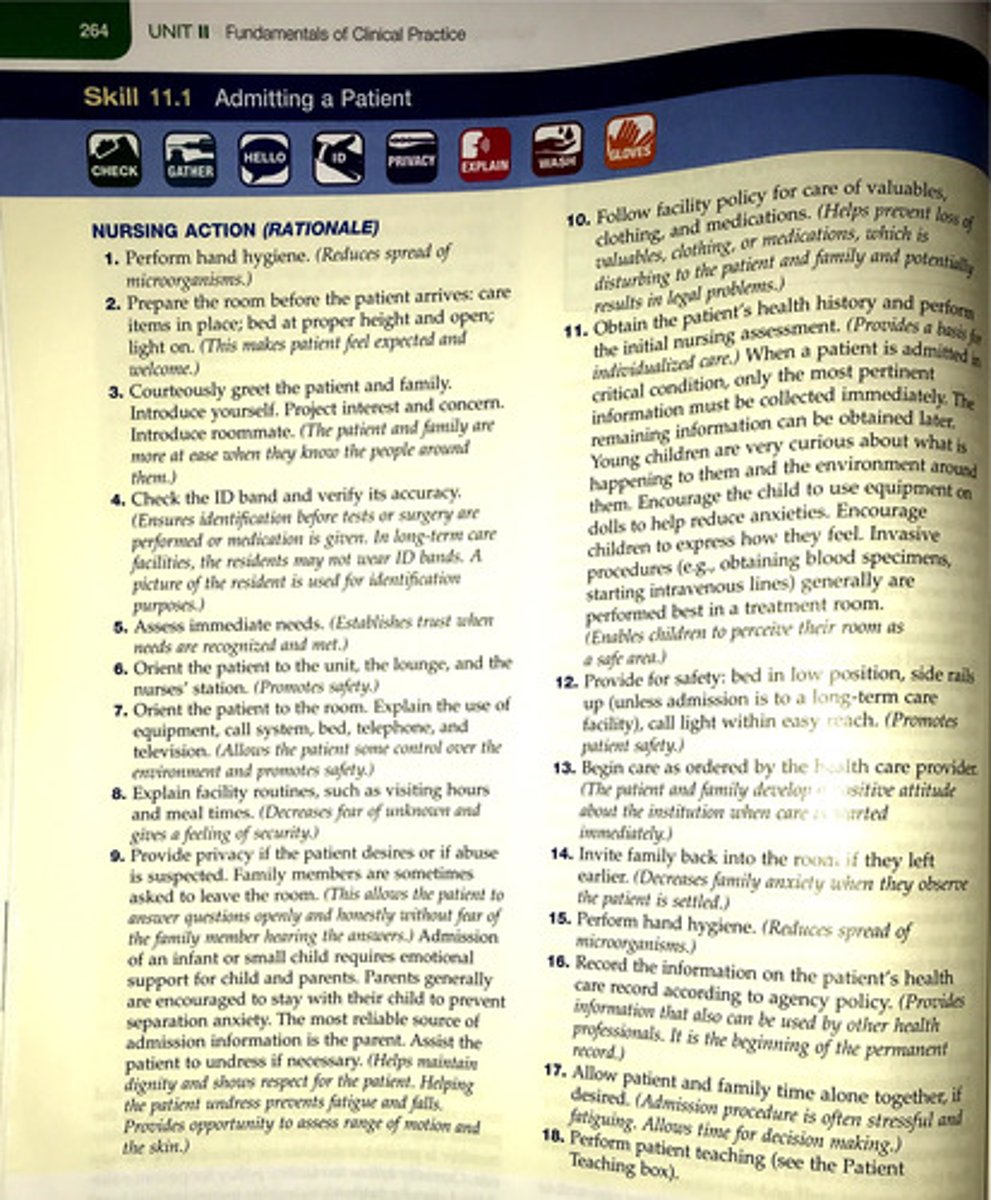
Step by step process of Admitting a Patient
See attached photo.
1. Perform hand hygiene (reduce spread of microbes)
2. Prepare the room before pt arrives. Bed in proper height. Lights on (helps to make pt feel expected and welcome)
3. Courteously greet the pt and family. Introduce yourself. Project interest and concern. Introduce roommate (if any) -- (the pt and family are more at ease when they know the people around them)
4. Check the ID band and verify its accuracy. (ensure that correct pt is receiving care. In long-term care facilities, pts may not wear ID bands. a picture of the resident is used for identification purposes)
5. Assess immediate needs of the pt (establishes trust when needs are recognized and met)
6. Orient pt to unit, the lounge, and nurses' station (promotes safety)
7. Orient the pt to the room. Explain the use of equipment, call system, bed, telephone, and TV ( allows the pt some control over the environment and promotes safety)
8. Explain facility routines, such as visiting hours and meal times. (decreases fear of unknown and gives feeling of security)
9. Provide privacy if the pt desires or if abuse is suspected. Family members are sometimes asked to leave the room. (this allows the pt to answer questions openly and honestly without fear of the family member hearing the answers).
Admission of an infant or small child requires emotional support for child and parents. Parents are generally encouraged to stay with the child to prevent separation anxiety.
10. Follow facility policy for care of valuables, clothing, and meds. (helps prevent loss of valuables, clothing or meds, which is disturbing to the pt and family and potentially results in legal problems)
11. Obtain pt's health history and initial nursing assessment. (provides a basis for individualized care) If the patient is in a critical condition, only the most important information must be collected immediately. The rest can be obtained later.
12. Provide for safety: bed in low position, side rails up, call light within easy reach (promotes pt safety)
13. Begin care as ordered by the healthcare provider (the pt an family develop a positive attitude about the institution when care is started immediately).
14. Invite family back into the room if they left earlier (decreases family anxiety when they observe that pt is settled)
15. Perform hand hygiene. (reduce spread of microbes)
16. Record the info on the pt's healthcare record according to agency policy. (provides info for other healthcare providers. beginning of permanent record)
17. Allow pt and family time alone together, if desired (admission procedure is often stressful and fatiguing. Allows time for decision-making)
18. Perform pt teaching
Assessment and data collection
The Joint Commission (TJC) requires each hospitalized pt to have an admission assessment prepared by a registered nurse (RN) within 24 hrs of admission. The RN then is allowed to delegate aspects of data collection, for example, to the LPN/LVN.
Managing Emergency Admissions
- for the pt admitted through the Emergency department (ED), immediate treatment takes priority over routine admission process.
- After ED treatment, the pt arrives on the nursing unit with a temporary ID bracelet, a physician's order sheet, and a record of treatment. Get report from previous nurse who took care of pt
- Document any on-going treatment, such as IV infusions, in the nursing notes.
- When the patient's condition allows, proceed with the routine admission procedures
Role of LVN in the nursing process for Patient Admission
- participate in planning care for pts based on pt's needs
- review pt's plan of care and recommend revisions as necessary
- review and follow defined prioritization for pt care
- use clinical pathways, care maps, or care plans to guide and review pt care
Assessment
- assessment of pt begins at admission.
- subjective and objective data are collected during assessment.
- Most facilities have a pt database form to assist in organizing these data
Diagnosis (patient problem)
- the pt being admitted to most healthcare facilities is required to have a nursing care plan initiated by the RN within the first 24 hrs of admission.
Common pt problems for a newly admitted pt include:
- Anxiousness
- Potential for injury
- Insufficient knowledge regarding admission process/illness
- Fearfulness r/t admission to health care facility
Expected Outcomes and Planning
Planning involves the development of pt-centered goals baed on the pt problem statements formed.
Example:
Goal 1: Pt will voice understanding of care planned while in facility
Goal 2: Pt will not suffer accidental injury while in facility
Implementation/Intervention
Nursing interventions related to admission include the following:
- orient the pt to the facility to ease the pt's anxiety
- establish nurse-patient rapport directed at fostering a therapeutic nurse-patient relationship
- confirm through discussion and questions that the pt understands the diagnostic tests and procedures
- monitor the pt's ability to ambulate alone
- monitor the pt's ability to operate the hospital bed, call light, and the emergency button
Transfer
a change in condition of a pt- whether improving or becoming more critical, necessitates TRANSFER (moving a pt from one unit to another = INTRA-agency transfer) or sometimes to other healthcare facilities = INTER-agency transfer)
Continuity of care
coordination of services provided to patients before they enter a health care setting, during the time they are in the setting, and after they leave the setting.
- documentation of the pt's condition before and during transfer and adequate communication among nursing staff ensures CONTINUITY OF CARE and provides legal protection for the transferring facility and its staff.
Special considerations for Transferring Patients
- arrange transportation via ambulance with social services dept. (if pt requires it), for transfer to another facility. Ensure all necessary equipment is assembled to provide care during transport
- ensure documentation is complete when pt is being transferred to another facility.
- if pt is being transferred to another facility, ensure that all appropriate pt care measures have been performed (such as suctioning of airway, administration of meds, change soiled dressings, bathing of incontinent pt, and emptying of collection devices)
discharge planning
systematic process of planning for pt care after discharge from a hospital or healthcare facility.
Transferring a Patient: Step by step process
1. Perform hand hygiene (reduces spread of microbes)
2. Check health care provider's order for transfer. (verifies if and when pt is to be transferred)
3. Inform pt and family of the transfer.
( reduces fear of unknown, and strengthens nurse-pt relationship)
4. Notify receiving unit of the transfer and when to expect the pt. (allows preparation time to best welcome new pt)
5. Gather all the pt's belongings and necessary care items to accompany the pt (builds trust and prevents loss of items)
6. Assist in transferring the pt, usually via stretcher or wheelchair (ensures pt safety, pt's condition determines mode of transportation)
7. Introduce patient and family to nurses on new unit and to roommate. (establishes the beginning of new therapeutic nurse-pt relationship and gives a sense of belonging)
8. Provide a brief summary of medical diagnosis, treatment care plan, and medications. Review medical orders with nurse assuming care. Situation, background, Assessment, and Recommendation (SBAR) is the common format used for reporting this information. If transferring to another facility, complete an inter-agency transfer form. (For continuity of care, prevents errors)
9. Explain equipment, policies, and procedures that are different on the new unit. (reduces anxiety)
10. Perform hand hygiene (reduce spread of microbes)
11. Record condition of pt and means (mode) of transfer. The nurse on the new unit also records an assessment of the pt's condition on arrival. (if properly executed, the pt's medical record reflects all care given and pt's response(
12. For an intra-agency transfer, the other departments must be notified. (keeps records current and prevents errors)
13. An INTER-agency transfer usually is made via air or ground ambulance or via private car. Make sure pt is dressed or covered appropriately for environmental comfort. If O2 is necessary, a small transport oxygen tank usually is used.
14. Infants generally are transported in an isolette (incubator) that is later returned to the sending health care facility.
15. Perform pt teaching
Discharge Teaching Goals
- Carefully follow diet
- comply with their medication therapy
- know about possible complications
- know when to seek follow-up care
- manage their activity level
- recognize their need for rest
- understand their illness
- understand their treatments
- be certain to include family in DC teaching to ensure proper care at home
Home care instructions
- pt who needs care at home after DC from healthcare facility often is referred to Home Health agency (an organization that provides health care in the home)
- DC from a Home Health agency involves the same kind of teaching as DC from the hospital. The nurse is responsible to ascertain (find out) if the pt needs more care
- assess availability and skill of primary caregiver
- assess additional resources that may be available to help such as close friends
- Evaluate emergency preparations: for example, signaling device or phone is set up within pt's reach
Referrals and discharge planning
Continuity of care for the pt can be improved by approaching DC planning with an INTER-Disciplinary approach:
Dietitian - provides proper food & nutrition teaching/planning
Social Worker - provides counseling on major life crises such as terminal illness and family problems. Assists in finding community resources such as equipment... assists in finding financial resources to cover medical costs.
Physical Therapist (PT) - Assists in examination and treatment of physically disabled people, as well as in rehabilitating strength of pts
Occupational Therapist (OT) - teaches pts to adapt to physical or cognitive challenges by learning new vocational skills or activities of daily living
Speech Therapist (ST) - assists pts with disorders that affect normal oral communication and pts with swallowing disorders
Clinical Nurse Specialist - consults with nursing staff on appropriate nursing interventions for complex nursing diagnoses; provides pt and family teaching
Home health care nurse - provides follow up DC visits to a pt's home for the delivery of nursing services
Discharging a patient
1. Perform hand hygiene
2. Ensure there is DC order
3. If there is no DC order, and the pt insists on leaving the facility, have the pt sign the AMA (against medical advice) form. Do your best to make the pt stay, but generally, pts cannot be held against their own wishes.
4. Notify the family or the person who will be transporting the pt home.
5. Verify that pt / family understands DC instructions of care (Meds, special diet, exercise, F/U care)
6. Gather equipment, supplies, and prescriptions that the pt is to take home.
7. Assist the pt in dressing and packing items to go home.
8. Check clothing and valuables list made on admission according to policy.
9. Transfer the pt and belongings to the vehicle outside.
- many facilities escort the pt vi wheelchair
- many pts are DC'd via gurney
- assist the pt into the vehicle. Help with the personal belongings. Use good communication and wish pt well.
10. Perform hand hygiene
11. Document entire DC procedure
- teaching
- pt's condition
- method of DC
12. When the pt is a child, the parents must be included in all aspects of teaching.
discharge against medical advice (DAMA)
Discharge against medical advice is used on a discharge order to indicate that the patient requested to leave a medical facility although the medical supervisor advised against it.
- Notify the MD right away
- if the pt refuses to sign the AMA form, do not detain the pt. Doing so is a violation of the patient's legal rights.
- after the pt leaves, document the incident thoroughly in your notes and notify the healthcare provider
What is the Patient Self-Determination Act?
federal legislation (law) that requires all clients admitted to a health care facility to be asked if they have advance directives, and provide pts with info about their right to accept or reject medical treatment
True or False.
The pt has the right to be treated with courtesy, dignity, and respect.
TRUE!!!!!!!
True or False.
DC planning begins when a pt is admitted to a healthcare facility
True
When admitting a patient to the hospital, the nurse observes that the patient is distracted and tense. What does this behavior suggest as a common reaction to hospitalization?
a. Relief about being cared for
b. Fear of the unknown
c. Feeling of powerlessness
d. Concern about cost
ANS: B
Fear of the unknown may be the most common reaction to hospitalization.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 313
OBJ: 3 | 5 TOP: Admission KEY: Nursing Process Step: Assessment
MSC: NCLEX: Psychosocial Integrity
A nurse is admitting a patient to an acute care facility. During the admission procedure, what nursing intervention would best help reduce patient anxiety?
a. Transport the patient by wheelchair.
b. Inform the physician that the patient is admitted.
c. Greet the patient by name.
d. Collect financial information during the interview.
ANS: C
Greeting the patient by name is one of the most important aspects of admission.
PTS: 1 DIF: Cognitive Level: Application REF: Page 316
OBJ: 1 | 4 | 5 TOP: Admission KEY: Nursing Process Step: Implementation
MSC: NCLEX: Psychosocial Integrity
What essential part of the admission procedure is performed by the RN?
a. Securing the patients valuables
b. Confirming the type of insurance coverage
c. Obtaining a health history
d. Familiarizing the patient with the room
ANS: C
Admission assessment is performed by the RN.
PTS: 1 DIF: Cognitive Level: Knowledge REF: Page 318
OBJ: 5 | 6 TOP: Admission KEY: Nursing Process Step: Assessment
MSC:NCLEX: Safe, Effective Care Environment
When should discharge planning begin?
a. The day before discharge
b. On the first day postoperatively
c. Shortly after admission
d. When the doctor orders it
ANS: C
Discharge planning begins shortly after admission.
PTS: 1 DIF: Cognitive Level: Knowledge REF: Page 323
OBJ: 5 | 8 TOP: Discharge KEY: Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
Where can a nurse refer the family of a patient to find a source of financial aid to meet medical expenses?
a. A local bank
b. A clinical nurse specialist
c. The hospital administration
d. Social services
ANS: D
Often a patient will require services of various disciplines within the hospital. Social services can assist with meeting medical financial obligations.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 326 Health Promotion
OBJ:8TOP:Social services
KEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
When a patient demands to be discharged without a physicians order and is leaving the unit with his belongings, what should the nurse ask the patient to sign?
a. A form exercising the patients rights
b. A discharge against medical advice form
c. An informed consent
d. An advanced directive
ANS: B
If a doctor cannot convince the patient to stay, the patient should sign an against medical advice form.
PTS: 1 DIF: Cognitive Level: Application REF: Page 327, Box 13-6
OBJ: 10 TOP: Discharge KEY: Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
The nurse must be sensitive to an older adult patient experiencing separation anxiety when admitted to the hospital. When a child experiences separation anxiety they will usually cry. What will an older adult often demonstrate when experiencing separation anxiety?
a. Withdrawal
b. Anger
c. Depression
d. Regression
ANS: C
The older adult may demonstrate depression as a result of separation anxiety entering the hospital.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 314
OBJ: 3 TOP: Admission KEY: Nursing Process Step: Assessment
MSC: NCLEX: Psychosocial Integrity
Upon admission, the nurse notes that a patient without family members present has a billfold filled with cash. Where can the nurse suggest the money be placed?
a. In a sealed envelope in the bedside table
b. In the care of hospital security
c. Locked in the narcotic cupboard
d. In the hospital safe
ANS: D
Valuables should be locked in the hospital safe.
PTS: 1 DIF: Cognitive Level: Application REF: Page 316
OBJ:6TOP:Care of valuables
KEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
If a patient has an order for an interagency transfer where does the nurse explain that the patient will be moved?
a. A double room to a private room
b. One unit of the hospital to another
c. One room of the unit to another
d. One facility to another
ANS: D
The interagency transfer moves a patient from one health care agency to another.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 322
OBJ: 7 TOP: Transfer KEY: Nursing Process Step: Implementation
MSC: NCLEX: Psychosocial Integrity
Before the actual discharge occurs, what must the nurse ensure ?
a. The patient is well enough to go home.
b. The patient has not been overly medicated.
c. The patient understands the discharge instructions.
d. The patient has adequate transportation.
ANS: C
It is essential that the patient be fully aware of the discharge instructions before being discharged.
PTS:1DIF:Cognitive Level: Application
REF: Pages 323, 325-326, 328 Skill 13-3 OBJ: 5 | 9
TOPischargeKEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
A patient who is alert and oriented is threatening to leave the hospital against medical advice (AMA). What action should the nurse take?
a. Forcibly detain and restrain the patient.
b. Administer a sedative hypnotic medication.
c. Prevent patient from leaving until an AMA form is signed.
d. Notify the physician that the patient is threatening to leave AMA.
ANS: D
When a patient threatens to leave AMA, the physician should be notified immediately. If the physician fails to convince the patient to remain in the facility, the physician will ask the patient to sign an AMA form releasing the facility from legal responsibility for any medical problems the patient may experience after discharge. If the physician is not available, the nurse should discuss the discharge form with the patient and obtain the patients signature. If the patient refuses to sign the AMA form, the patient should not be detained. This violates the patients legal rights. After the patient leaves, the nurse should document the incident thoroughly in the nurses notes and notify the physician. A rational adult patient who will not sign the AMA form cannot be forcibly detained.
PTS: 1 DIF: Cognitive Level: Application REF: Page 327, Box 13-6
OBJ:10TOP:Against medical advice
KEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
How can the nurse demonstrate cultural sensitivity to a Haitian American patient?
a. By providing a well-lit room 24 hours a day
b. By writing out all instructions given to the patient
c. By allowing the patient to keep leaves in her room
d. By asking the physician to provide all directions to the patient
ANS: C
Many Haitians believe that leaves have a special significance in healing. Leaves may be found in the clothes and on various parts of the body. Leaves are thought to have mystical power related to regaining or keeping health.
PTS:1DIF:Cognitive Level: Application
REF: Page 315, Cultural Considerations OBJ: 4 TOP: Cultural awareness
KEY:Nursing Process Step: Implementation
MSC: NCLEX: Psychological Integrity
A nurse is caring for a Haitian American patient. How might the nurse demonstrate cultural sensitivity?
a. Discarding any leaves the patient may have brought with them
b. Assigning the patient to a room with any Haitian American patient
c. Instructing the patient to ride in a wheelchair when discharged
d. Allowing the patient to walk out of the hospital when discharged
ANS: D
Some Haitian Americans associate wheelchairs with being sick. Therefore, on discharge, the patient who is allowed to walk out of the hospital will be more likely to feel that care has been effective. A poor patient with a Haitian background and a wealthy patient with a Haitian background, although from the same country, may find the same room assignment together in the hospital very distasteful.
PTS:1DIF:Cognitive Level: Application
REF: Page 315, Cultural Considerations OBJ: 4 TOP: Cultural awareness
KEY:Nursing Process Step: Implementation
MSC: NCLEX: Psychological Integrity
MULTIPLE RESPONSE
How can the nurse help reduce the stress of a hospital admission? (Select all that apply.)
a. Show the patient how bedside equipment works.
b. Explain the need to establish a clear source of reimbursement.
c. Give simple explanation of policies.
d. Involve the patient in the plan of care.
e. Keep family interventions to a minimum.
ANS: A, C, D
An empathic reception reduces anxiety of admission; for instance, demonstrating how bedside equipment works, explaining hospital policies, and involving the patient in the plan of care from the start all help to reduce the stress of a hospital admission. Securing financial information is not a role of the nurse, and family interventions are frequently helpful in reducing stress.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 314-318
OBJ:4 | 5TOP:Stress reduction
KEY:Nursing Process Step: Implementation
MSC: NCLEX: Psychosocial Integrity
The nurse adheres to the discharge standards set by The Joint Commission (TJC), which include that patients will receive instruction regarding which aspect(s) of care? (Select all that apply.)
a. Medications
b. Rehabilitation techniques
c. Referral to community agencies
d. Medical equipment to be used
e. Obtaining health insurance
ANS: A, B, C, D
The Joint Commission (TJC) standards require that a patient have information pertinent to medication, rehabilitation instructions, referral to community agencies, instruction in using any medical equipment, family care responsibility, diet, and how to obtain further treatment if necessary.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 324
OBJ:9TOP:TJC standards for discharge
KEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
COMPLETION
The nurse completes thorough documentation before, during, and after a transfer to ensure _______ of _______.
ANS:
continuity, care
Clear documentation before, during, and after a transfer ensures that the patients condition is being monitored and maintains the continuity of care.
PTS: 1 DIF: Cognitive Level: Comprehension REF: Page 322
OBJ:5 | 7TOPocumentation
KEY:Nursing Process Step: Implementation
MSC:NCLEX: Safe, Effective Care Environment
Some _____________________patients consider sundown Friday to sundown Saturday to be the Sabbath, which is a time of rest.
ANS:
Orthodox Jewish
Some Orthodox Jewish patients consider sundown Friday to sundown Saturday to be the Sabbath, which is a time of rest. These patients may avoid the use of any electronic equipment, so the nurse should find alternatives to the use of this equipment if possible.
PTS:1DIF:Cognitive Level: Knowledge
REF: Page 315, Cultural Considerations OBJ: 3 TOP: Orthodox Jewish culture
KEY:Nursing Process Step: Implementation
MSC: NCLEX: Psychosocial Integrity
Because of the stress caused by hospitalization, the nurse assesses a newly admitted older adult patient for ________________.
ANS:
disorientation
In a normally alert and oriented older adult, medical conditions that necessitate hospitalization often result in some level of disorientation.
PTS:1DIF:Cognitive Level: Application
REF: Page 314, Life Span Considerations OBJ: 3 | 5
TOP: Disorientation in older adults KEY: Nursing Process Step: Assessment
MSC: NCLEX: Psychosocial Integrity