Female hormonal system (ovarian cycle)
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
Female hormonal system hormones
GnRH secreted by hypothalamus
LH and FSH (sex hormones) secreted by anterior pituitary hormones
Estrogen and progesterone secreted by ovaries
What is Female monthly sexual cycle its duration and its importance
Intro
Normal female reproductive years of female by monthly rythmic changes in female hormone secretion rate and corresponding physical changes in ovary and other sex organs
Rhythmic pattern called female monthly sexual cycle ( menstrual cycle informally)
Duration: 28 days avarage but range 20-45 days
Importance
Single ovum normally released from ovaries so only 1 foetus will begin to grow at a time
Uterine endometrium prepared in advance for implantation of fertilised ovum at required time of the month
Ovarian cycle phases and meiosis stages ( luteal doesn’t have)
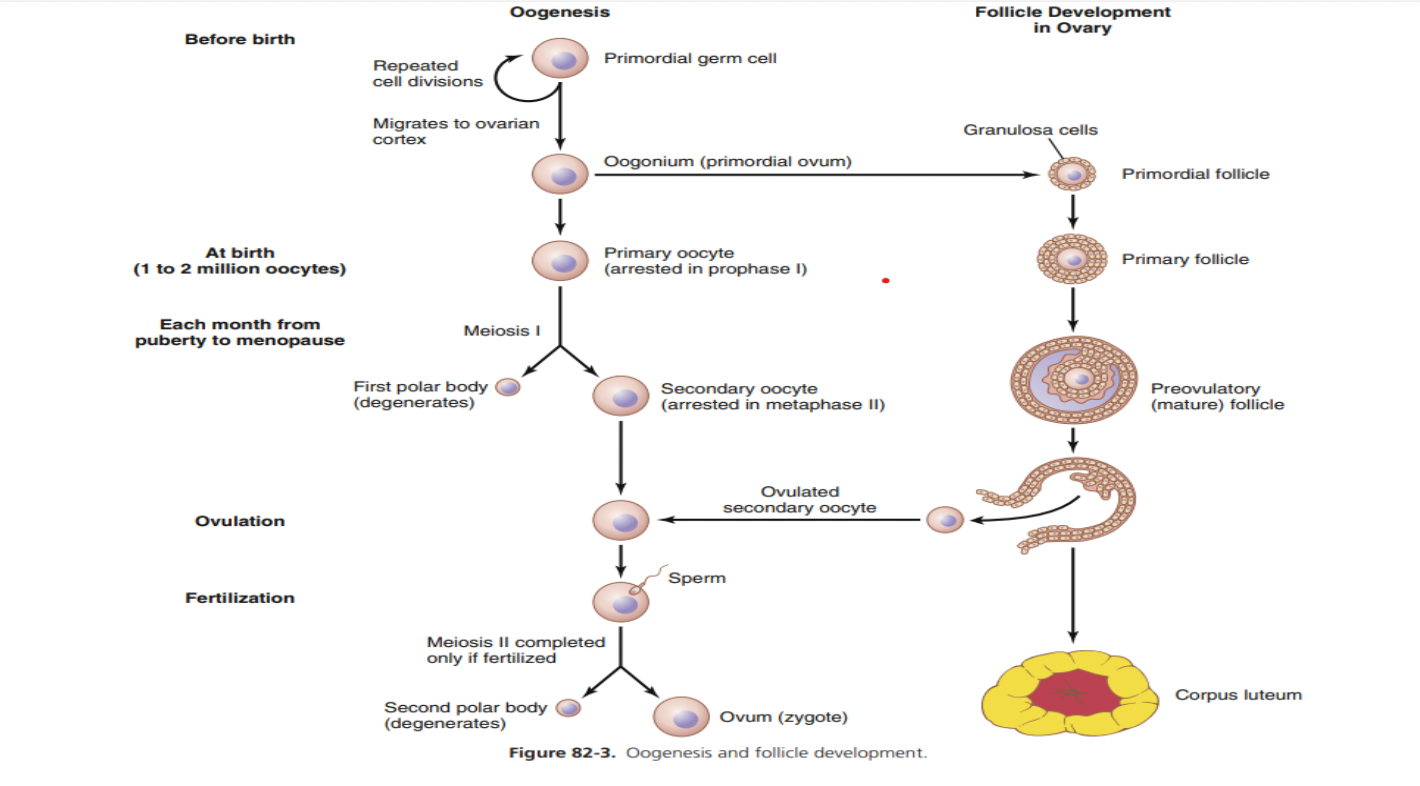
Follicular phase = starts at prophase I → Finishes meiosis I
Ovulatory phase = Arrests at Metaphase II Meiosis
Luteal phase
Ovarian cycle : Follicular phase ( Puberty , Steps + explanation of formation of primary follicles)
Puberty
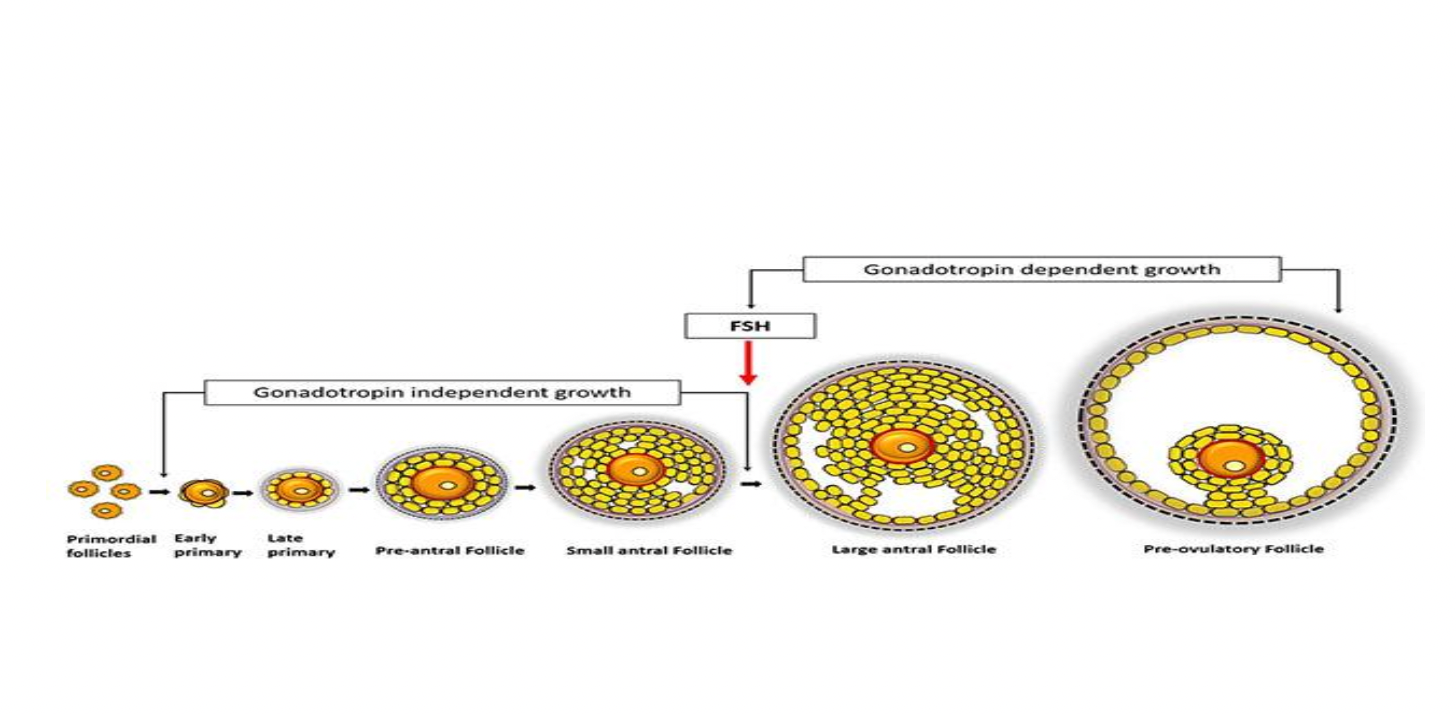
Puberty = 400,000 primordial follicles
Each follicle composed of ovum (1ry oocyte) surrounded by single flat layer of granulosa cells
During each cycle 20 primordial follicles start to grow
Steps: Formation of primary follicle → Development of astral and vesicular follicles → Graafian follicle formation
Formation of primary follicles
Ovum moderate enlargement → Single follicular cell layer becomes cuboidal and divides to form several granulosa cell layers → Primary follicles
Follicular phase (Formation of antral and vesicular follicles)
How are theca cells forms?
How are secondary follicles antral and vessicular follicles formed?
Rapid proliferation of granulosa cells leads to more cell layers→ Spindle cells (derived from ovarian stroma) collect in many layers outside granulosa cells → Mass of cells called theca (interna and externa)
After few days granulosa cells secrete follicular fluid that has high conc of oestrogen → fluid accumulation leads to antrum within mass of granulosa cells → Antral follicle
Great accelerated growth of antral follicle → Vesicular follicle (larger follicle)
Follicular phase:
Theca interna vs externa?
Accelerated growth of antral follicle is due to?
Theca interna vs externa
Theca interna - Highly vascular epitheliod cell layer that secrete oestrogen and progesterone
Theca externa - Outer layer less vascular connective tissue capsule surrounding follicle
Great accelerated growth of antral follicle due to:
Estrogen secreted into antral follicle cause granulosa cells ↑number of FSH receptors so more sensitive to FSH from pituitary
FSH and estrogen promote LH receptors on granulosa cells → Rapid increase in follicular secretion
Follicular phase: Formation of Mature Graafian follicle . How is it characterised. Possible cause of atresia
Mature Graafian follicle formation
(after secondary follicles formed…)
After week or more of growth 1 follicles outgrow the rest and the others involute and become atretic. Mature follicle now called mature Graafian follicle.
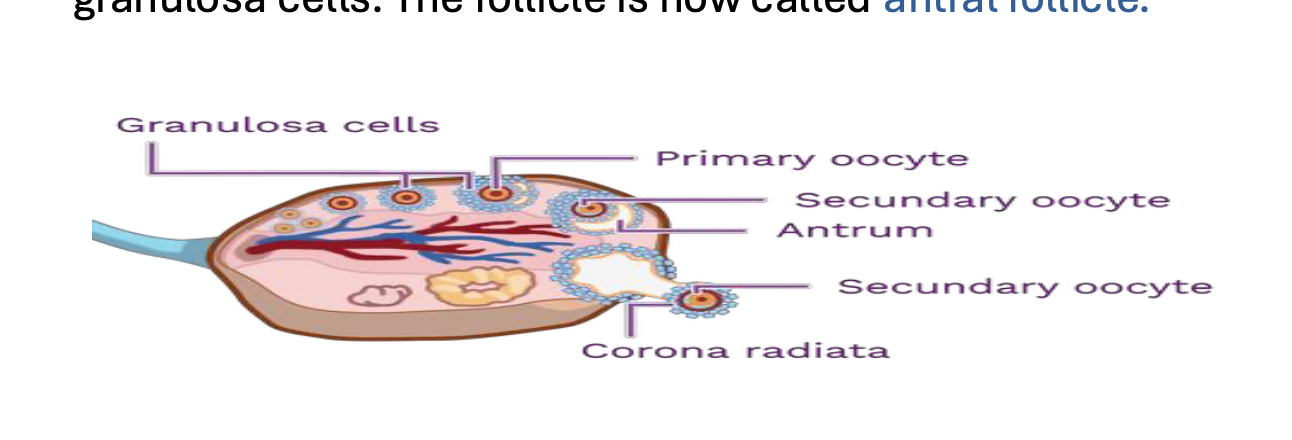
Mature Graafian follicle characterised by presence of
Ovum (2ry oocyte) surrounded by zona pellucida (thin memb)
Corona radiata ( granulosa cell layers surrounding ovum)
Antrum with follicular fluid
Several layers of granulosa cells
Surrounded by basal lamina then theca interna and theca externa
Cause of Atresia : unknown but could be cuz…
Large estrogen amount secreted into growing follicles act on hypothalamus to inhibit ↑ FSH secretion preventing loss of developed follicle growth and the 1 follicle that grows is cuz high estrogen content.
Ovulatory Phase (Define ovulation, Occurs when, Mechanism and hormonal control of ovulation)
Ovulation: release of haploid (23) 2ry oocyte into peritoneal cavity
Occurs : (On Day 14)
14 days before onset of next ovulatory cycle
14 days after menstruation onset in normal 28 day female sex cycle
Mechanism and hormonal control of ovulation
Theca cells secrete estrogen. It peaks 48hrs before ovulation
High blood estrogen give + feedback on anterior pituitary → ↑ LH secretion up to 6-10 folds (LH surge) and ↑ FSH secretion by 2-3 folds
FSH and LH act synergestically to cause rapid follicle swelling
LH cause rapid FSH secretion that contain progesterone for the first time
Within few hrs LH surge triggers (needed for ovulation):
1ry oocyte completes meiosis I = 2ry oocyte + 1st polar body.
Stigma degenerates, and follicle ruptures → releasing 2ry oocyte.
Finally, the combined follicle swelling & simultaneous degeneration of the stigma cause follicle to rupture with discharge of ovum.
The Luteal Phase (Formation of corpus luteum and fate of corpus luteum)
Formation of the corpus luteum:
During first few hrs after ovum expulsion from follicle remaining granulosa and theca cells enlarge in diameter and become filled with yellow looking lipid material and total mass of cells = Corpus luteum
Process of luteinization is mainly dependent on LH.
Fate of corpus luteum:
If fertilisation doesn’t occur: Corpus luteum of menstruation. Function till cycle day 22 then degenerates and stops function two days before next cycle.
If fertilisation occurs: Corpus luteum of pregnancy. Function tilll 12th wk of gestation by HCG (human chorionic gonadotropin) action, then placenta takes over function.
Diagnosis of ovulation
Symptoms : Pelvic pain , ↑ vaginal discharge , midcycle vaginal bleeding (sudden blood estrogen level drop after ovulation)
Basal body temp : Day of ovulation ↑ 0.2 - 0.5 due to thermogenic effect of progesterone secreted by corpus luteum. Elevated basal temp remain till cycle day 26.
Pregnandiol (progesterone metabolite) detection in urine
Endometrial biopsy: if ovulation occurs endometrium in secretory phase (progestational phase)
Cervical mucous examination: preovulatory phase cervical mucous characterised by ferning and spinnbarkeit phenomena which disappears if ovulation occurs
Spinnbarkeit phenomenon : If cervical mucous drop placed between 2 slides, long mucous threads appear between slides when they are separated
Ferning phenomenon: if drop of mucous spread on slide and left to dry → crystal formed will be arranged in feather like shape
Annovulatory cycle (Definition, 3 causes, 3 Characterised by)
Definition: Cycles in which ovulation fails to occur during menstrual cycle
Causes:
Occur in first 12-18 months after menarche (1st menstrual cycle) and before menopause onset
During oral contraceptive use
Some diseases
Annovulatory cycle characterised by
No corpus luteum formed so progesterone effect on endometrium absent
Estrogen continue endometrium proliferation → endometrium becomes thick enough to break down and begins to slough (menstruation) due to estrogen drop after graafian follicle degeneration.
Shortened (irregular) female sexual cycle