Neuro 8 -- Brainstem & Cerebellum 2
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
Nuclei of cranial nerves
Heterogenous — different from spinal nerves — as well as in their additional components some cranial nerves have —
Special visceral innervation (muscles of branchiomeric origin (pharyngeal arch origin))
Special visceral sensation (taste)
Special somatic sensation (vestibular & acoustic information)
Located in the tegmentum of the brainstem (just like reticular formation)
Responsible for processing new information coming from cranial nerves with a sensory component, or giving rise to an output traveling outside the brainstem
Grey matter of spinal cord = 4 functional territories, but in the cranial nerves we can find 7 territories — not all throughout the brainstem but just in specific regions depending on the cranial nerve emerging from that point
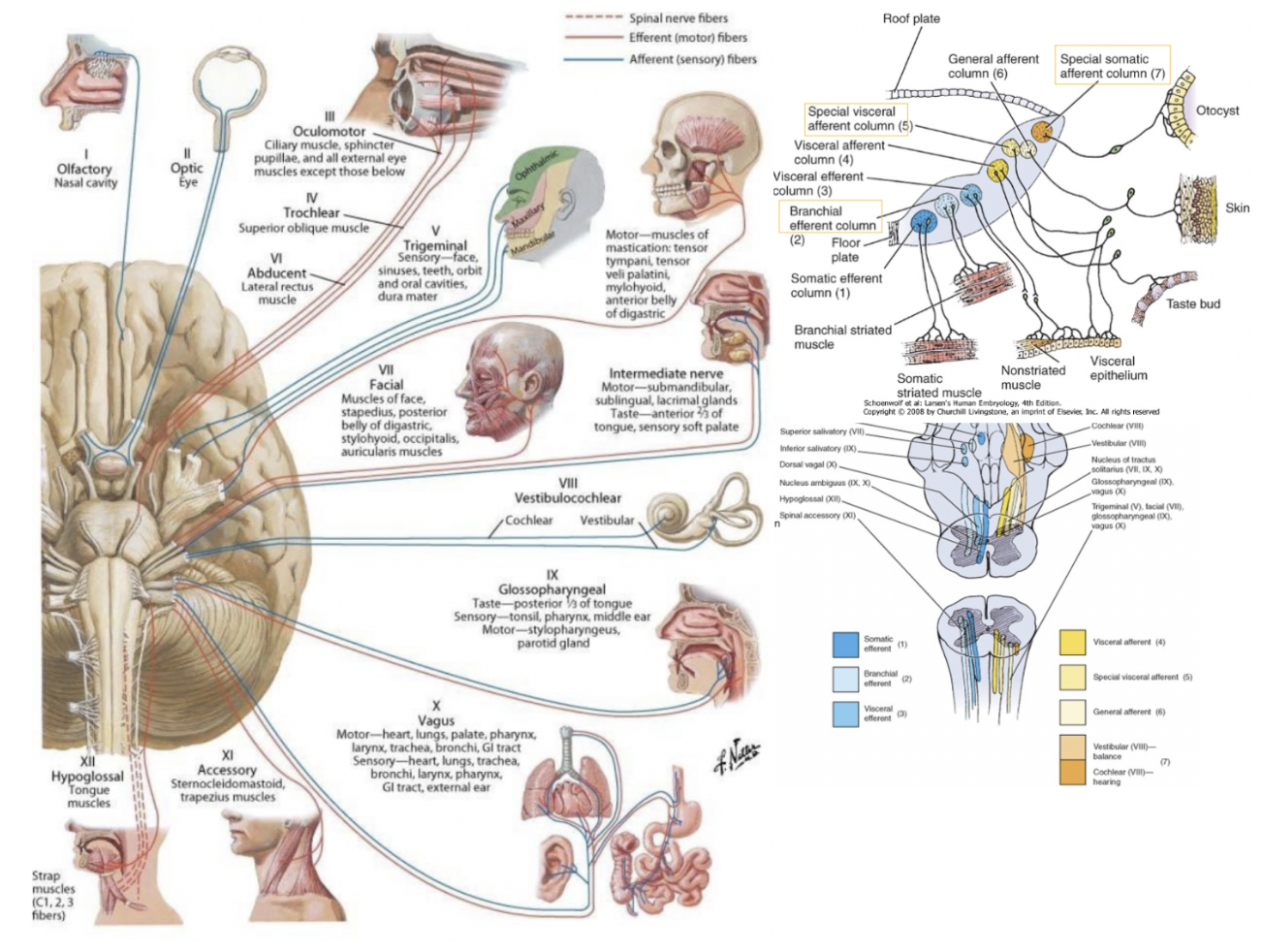
7 components (functional columns) of cranial nuclei
General somatic efferent component (GSE) —
Innervation of muscles with somatic origin (paraxial mesoderm)
Special visceral efferent (SVE) (or special branchio-motor component) —
Motor innervation of branchiomeric musculature (not smooth muscle, even though visceral)
General visceral efferent (GVE) —
Some motor nuclei of the brainstem can control smooth muscle fibers — parasympathetic preganglionic neurons
General visceral afferent (GVA) —
Sensory information from viscera — from periphery to nervous system
Special visceral afferent (SVA) —
Taste
General somatic afferent (GSA) —
Collects information from somatic components
Special somatic afferent (SSA) —
Relates to the vestibular & cochlear component (hearing & balance)
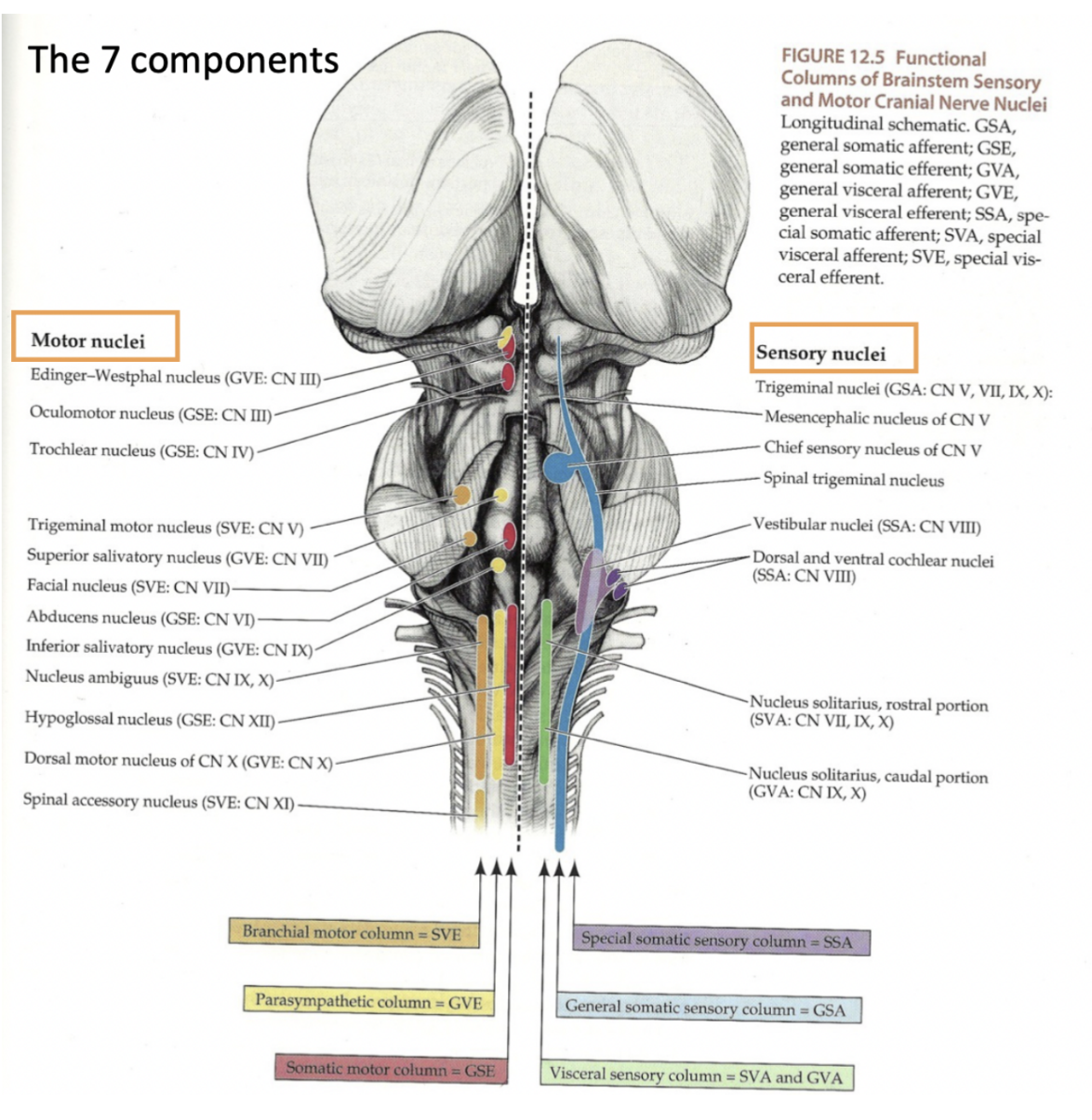
Oculomotor nerve —
3rd cranial nerve — motor neuron — in the mesencephalon
Emerges through the interpeduncular fossa of the brainstem — thus originating from the midbrain
Motor nucleus located in the rostral part of the tegmentum of the midbrain
Innervates most of the extraocular eye muscles
These originate from paraxial mesoderm —thus nerve has a general somatic efferent component
Also contains parasympathetic fibers to the intrinsic smooth muscles of the eye — thus also hase a gneral visceral efferent component
This parasympathetic innervation originates from the Edinger Westphal nucleus — parasympathetic preganglionic nucleus in the tegmentum of the midbrain
(The oculomotor nerve originates from 2 nuclei in the midbrain[1]: Oculomotor nucleus. Accessory parasympathetic nucleus (Edinger-Westphal nucleus))
Fibres of the GVE innervation along their course will find a ganglion — ciliary ganglion — where they will synapse & then innervate the smooth muscles
Superior orbital fissure, just like trochlear
![<ul><li><p>3rd cranial nerve — motor neuron — in the <u>mesencephalon</u></p></li><li><p>Emerges through the interpeduncular fossa of the brainstem — thus originating from the midbrain</p><ul><li><p>Motor nucleus located in the rostral part of the tegmentum of the midbrain</p></li></ul></li><li><p>Innervates <u>most</u> of the extraocular eye muscles</p><ul><li><p>These originate from paraxial mesoderm —thus nerve has a general somatic efferent component</p></li></ul></li><li><p>Also contains parasympathetic fibers to the intrinsic smooth muscles of the eye — thus also hase a gneral visceral efferent component</p><ul><li><p>This parasympathetic innervation originates from the <u>Edinger Westphal</u> nucleus — parasympathetic preganglionic nucleus in the tegmentum of the midbrain</p><ul><li><p>(The oculomotor nerve originates from 2 nuclei in the midbrain[1]: Oculomotor nucleus. Accessory parasympathetic nucleus (Edinger-Westphal nucleus))</p></li></ul></li><li><p>Fibres of the GVE innervation along their course will find a ganglion — <u>ciliary ganglion</u> — where they will synapse & then innervate the smooth muscles</p></li></ul></li><li><p>Superior orbital fissure, just like trochlear</p></li></ul>](https://knowt-user-attachments.s3.amazonaws.com/85666d31-f261-4886-aa2f-b132ec6204af.png)
Trochlear nerve
4th cranial nerve — only nerve originating dorsally — in the mesencephalon
Only has a general somatic efferent component — innervates one of the extraocular muscles — the superior oblique
Its motor nucleus is located in the caudal portion of the tegmentum of the midbrain
The only nerve whose fibers cross after their origin from the brainstem —
Cross the superior medullary velum — contralateral innervation
Exits at the level of the superior orbital fissure
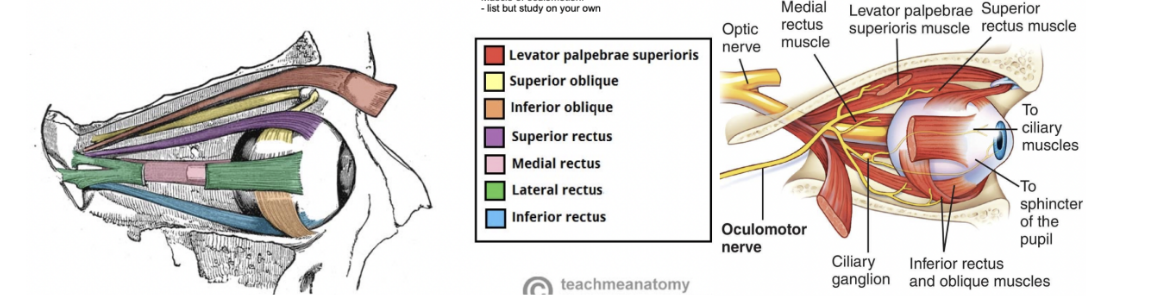
Muscles of oculomotion (extrinsic eye muscles) —
Oculomotor nerve divides into superior & inferior branches in the anterior part of the cavernous sinus —
Superior branch innervates the superior rectus & the levator palpebrae
Inferior branch innervates medial rectus, inferior rectus, & inferior oblique
7 extrinsic eye muscles — only 2 of which are not innervated by CN3 —
Lateral rectus — innervated by abducent nerve (VI)
Superior oblique — innervated by trochlear nerve (IV)
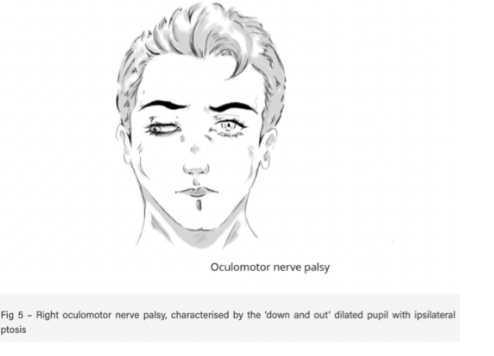
Clinical drop — oculomotor nerve palsy
Condition resulting from damage to oculomotor nerve — most common structural causes —
Raised intracranial pressure (compresses the nerve against temporal bone)
Posterior communicating artery aneurysm
Cavernous sinus infection
Trauma
Other pathological causes —
Diabetes, multiple sclerosis, myasthenia gravis, & giant cell arteritis
Symptoms —
Ptosis — drooping upper eyelid, due to paralysis of levator palpebrae superioris & unopposed activity of orbicularis oculi muscle
“Down & out” position of eye at rest — due to paralysis of superior, inferior, & middle rectus, and inferior oblique (therefore the unapposed activity of lateral rectus & superior oblique) — leading patient to be unable to elevate, depress, or adduct the eye
Dilated pupil — due to unopposed action of dilator pupillae muscle
Clinical drop — examination of the trochlear nerve
Examined in conjuction with oculomotor & abducens nerves by testing eye movements —
Patient is asked to follow a point (commonly the tip of a pen) with their eyes without moving their head
Target is moved in an “H-shape,” and the patient is asked to repot any blurriness of vision or diplopia (double vision)
Clinical drop — Palsy of the trochlear nerve
Causes —
Microvascular damage from diabetes mellitus or hypertensive disease
Other causes — congenital malformation, thrombophlebitis of the cavernous sinus, and raised intracranial pressure
Symptoms —
Commonly presents with vertical diplopia — exacerbated when looking downwards & inwards (such as when reading or walking down the stairs)
They can also develop a head tilt away from the affected side
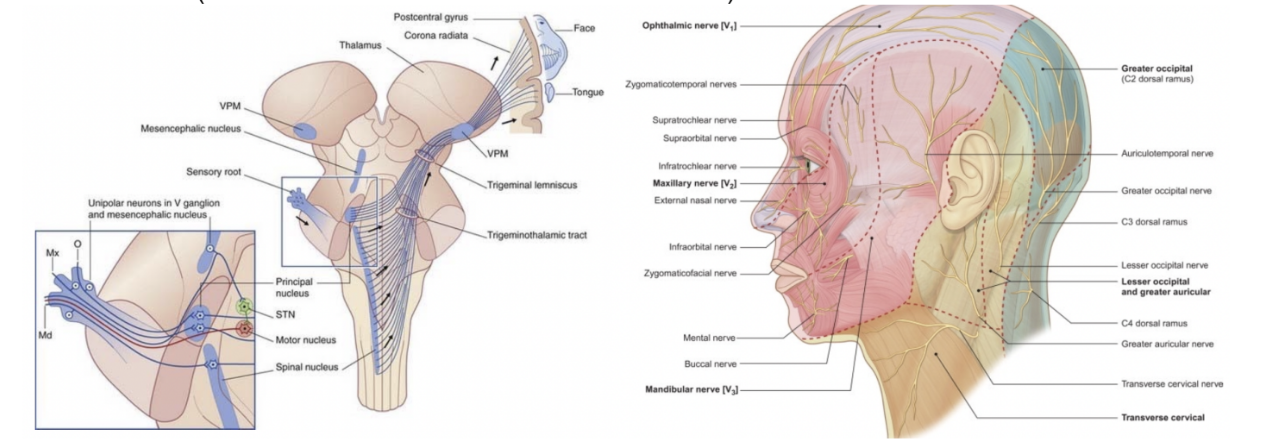
Trigeminal nerve
5th cranial nerve — has both a motor & sensory nucleus — located in the metencephalon (pons)
Motor nucleus — located in pons, and has a special visceral efferent (SVE) component — innervates the muscles of mastication & others of branchiomeric origin
Only branch of trigeminus with a motor component — mandibular branch — masticatory muscles (medial pterygoid, lateral pterygoid, masseter & temporalis), but also innervates the anterior belly of digastric, mylohyoid, tensor veli palatini, and tensor tympani
Large general sensation territory at level of head & of face — general somatic afferent (GSA) component, thus presnece of a sensory nucleus in the pons belonging to trigeminus
Sensations (from trigeminus) carried into the brain through 3 nuclei —
Pontine/principal (found in the pons)
Mesencephalic nucleus (in the midbrain)
Bulbospinal or spinal nuclei
Sensory ganglion of the trigeminus = ganglion of Gasser
not in brainstem — root goes to this ganglion then breaks off into the 3 branches
Exits at the level of the foramen rotundum, ovale, and superior orbital fissure
Abducens nerve
6th cranial nerve, innervating lateral rectus muscle (extraocular) — located in metencephalon (pons)
Only has a somatic general efferent component (GSE)
Originates from the pons, with its motor nucleus very clos to the midline & very superficial — so much so that it forms a protrusion of the floor of the 4th ventricle
Moreover, close to it — motor nucleus of facial nerve, whose fibers run over the abducens nucleus as they exit the brainstem —
Loop formed by fibers of facial nerve around nucleus of abducens nerve — Genu of the facial nerve
Also protrudes at level of floor of 4th ventricle
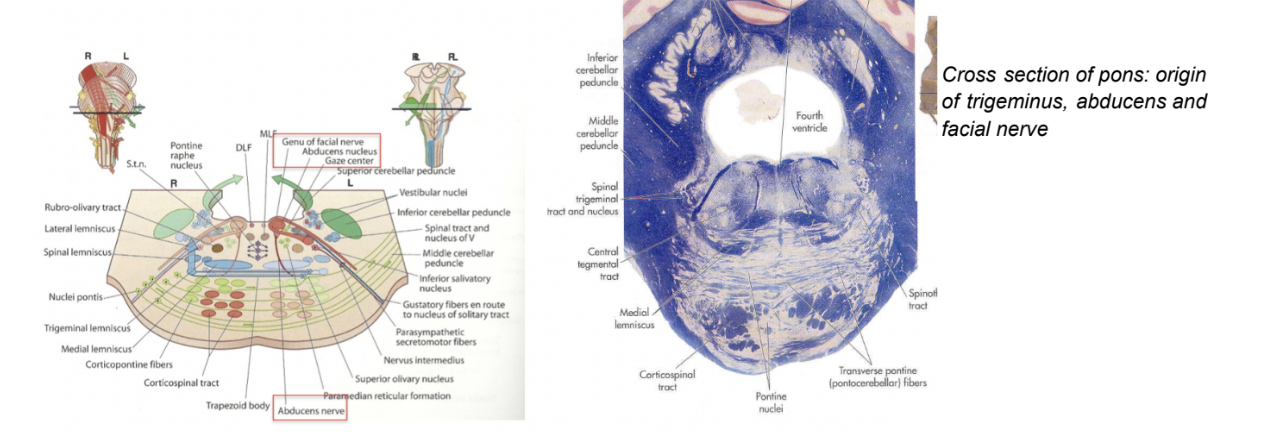
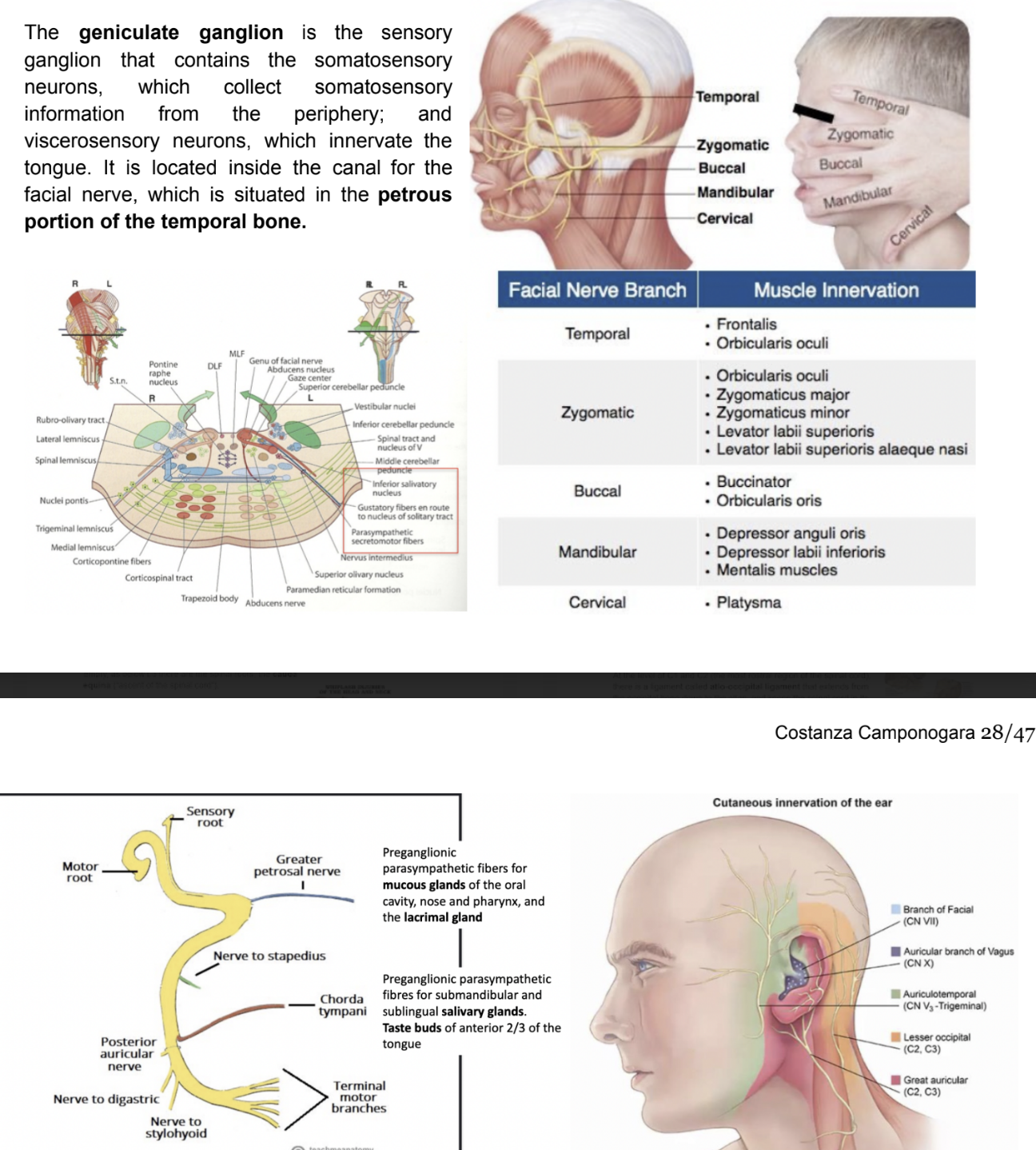
Facial nerve
7th cranial nerve — originates from the pons (metencephalon) — in particular its motor nucleus can be found in the pons
Exits from the brainstem at level of supra-olivary groove — in the bulbopontine groove
Made by a larger bundle of fibers, forming the facial nerve proper, and a smaller bundle of fibers, forming an intermediate component of the facial nerve
Has many different afferent & efferent components —
Special visceral efferent (SVE) (branchiomeric) — innervates muscles of facial expression
Linked to a motor nucleus in the tegmentum of pons
General visceral efferent (GVE) — specifically a parasympathetic preganglionic component — comtrongs sublingual, submandibular, lacrimal, nose, palate, & pharynx glands
Preganglionic parasympathetic neurons located in superior salivatory nucleus — sends fibers out of branstem to reach submandibular, sublingual, and sphenopalatine ganglia
Special visceral afferent (SVA) — formed by fibers directed to collect information from the tongue, generating taste — information is relayed to most rostral pat of nucleus of solitary tract — located in medulla oblongata
General somatic afferent component (GSA) (quite small) — small cutaneous territory referring to general sensation from skin of the ear, with this information relayed to the bulbospinal trigeminal nucleus
Geniculate ganglion — sensory ganglion containing fibers for the tongue (SVA)
Clinical relevance — corneal reflex
Involuntary blinking of eyelids — stimulated by tactile, thermal, or painful stimulation of the cornea
In the corneal reflex, the ophthalmic nerve acts as the afferent limb, detecting the stimuli, while the facial nerve is the efferent limb, causing contraction of the orbicularis oculi muscle
If the corneal reflex is absent, it is a sign of damage to the trigeminal/ophthalmic nerve, or the facial nerve
Damage to the facial nerve
Due to the wide range of functions of the facial nerve, damage to it can produce a variety of symptoms, depending on the site of the lesion —
Intracranial lesions —
Ocur during intracranial course (proximal to stylomastoid foramen) — paralyses or severely weakens muscles of facial expression, with other symptoms depending on location of lesion —
Chorda tympani — reduced salivation & loss of taste on ipsilateral (same side) 2/3 of tongue
Nerve to stapedius — ipsilateral hyperacusis (hypersensitivity to sound)
Greater petrosal nerve — ipsilateral reduced lacrimal fluid production
Most common cause — infection related to external or middle ear
If no definitive cause can be found — labeled Bell’s palsy
Extracranial lesions —
Extracranial course of facial nerve (distal to stylomastoid foramen) — only motor function is affected, resulting in paralysis or severe weakness of facial expression muscles
Various causes —
Parotid gland pathology — tumour, parotitis, surgery
Infection of the nerve (ex. herpes_
Compression during forceps delivery (neonatal mastoid process not fully developed)
Idiopathic — if no definitive cause — Bell’s palsy
Vestibulocochlear nerve
8th cranial nerve — some sensory nuclei located in medulla and some in caudal portion of the pons (myencephalon & metencephalon)
Special somatic afferent nerve — carries hearing & balance information coming from cochlear & vestibular parts of the middle ear
2 cochlear nuclei — superior & inferior (/dorsal & ventral)
4 vestibular nuclei — superior, inferior, medial, & lateral
Nuclei are found in the tegmentum of the pons & of the medulla
Vestibular neuritis
Inflammation of the vestibular branch of the vestibulocochlear nerve —
Aeitology(causes) of the condition not fully understood, but some cases are though to be due to reactivation of the herpes simplex virus
Presents with symptoms of vestibular nerve damage —
Vertigo (false sensation of oneself or surrounding spinning)
Nystagmus (repetitive, involuntary to-&-fro oscillation of the eyes
Loss of equilibrium (especially in low light)
Nausea & vomiting
Usually self-resolving — treatment is symptomatic, usually in form of anti-emetics or vestibular suppressants
Labryinthitis
Inflammation of the membranous labyrinth, resulting in damage to vestibular & cochlear branches of vestibulocochlear nerve
Symptoms = similar to vestibular neuritis — also include indicators of cochlear nerve damage — sensorineural hearing loss & tinnitus (false ringing or buzzing sound)
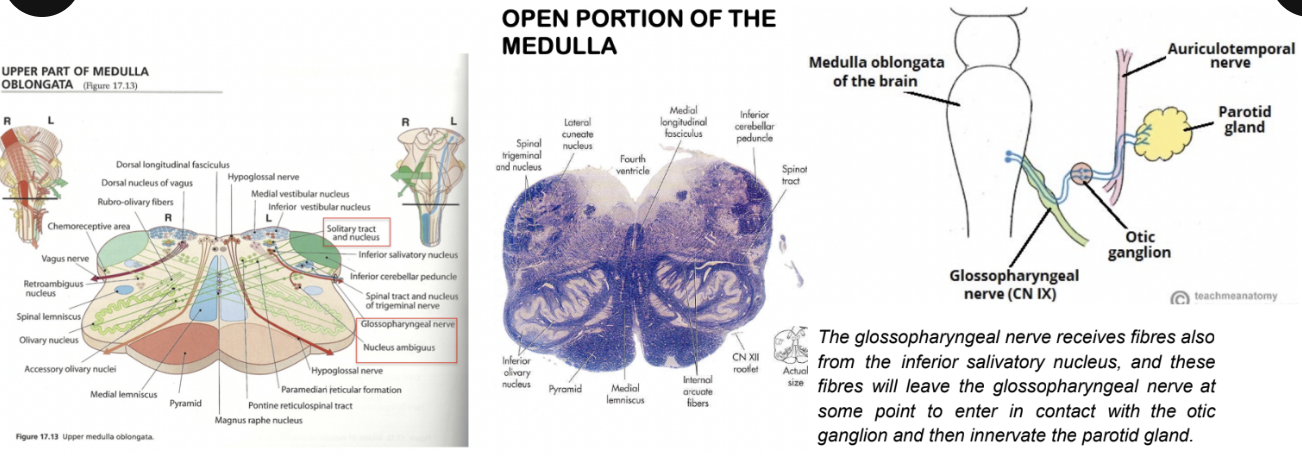
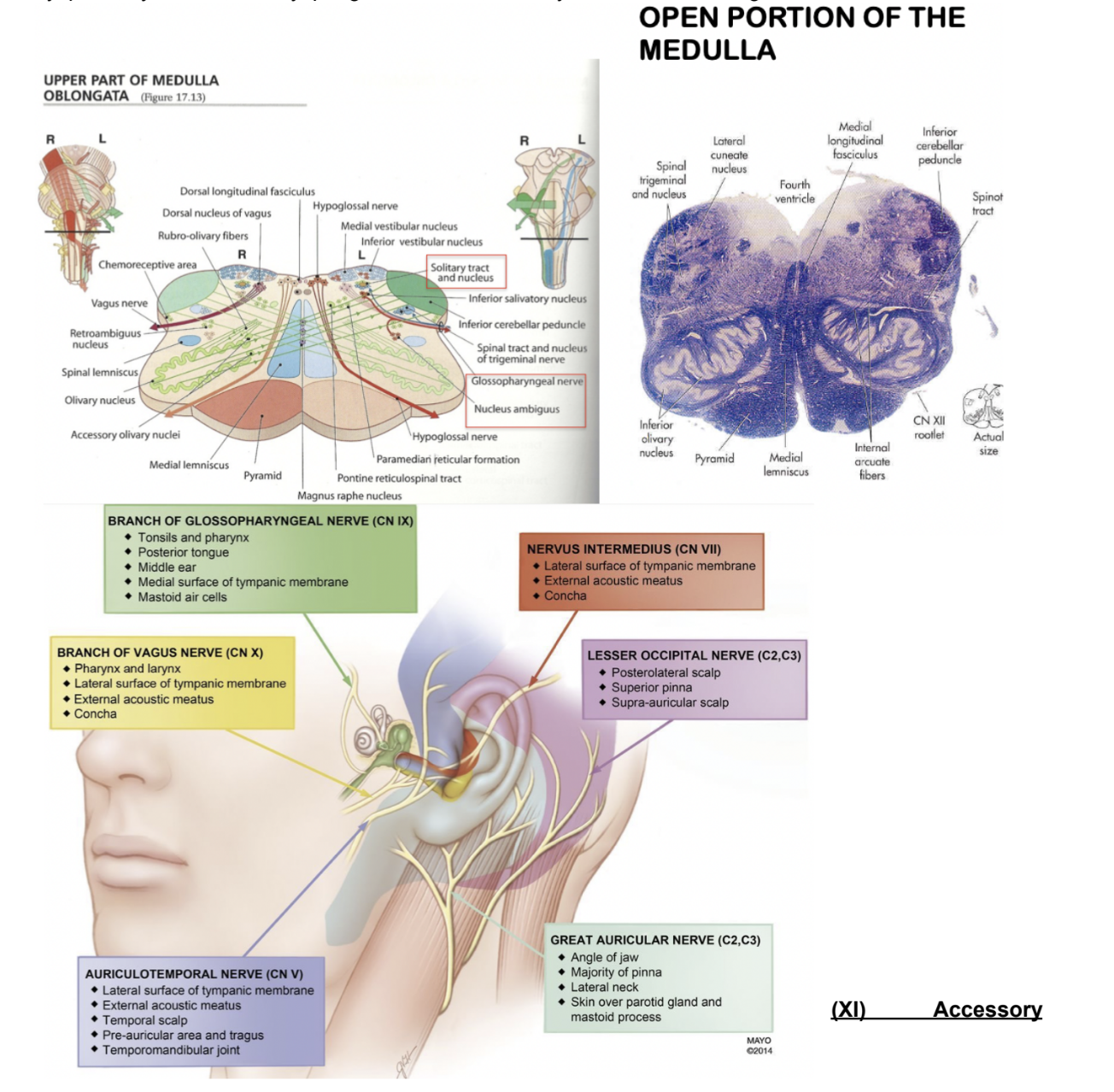
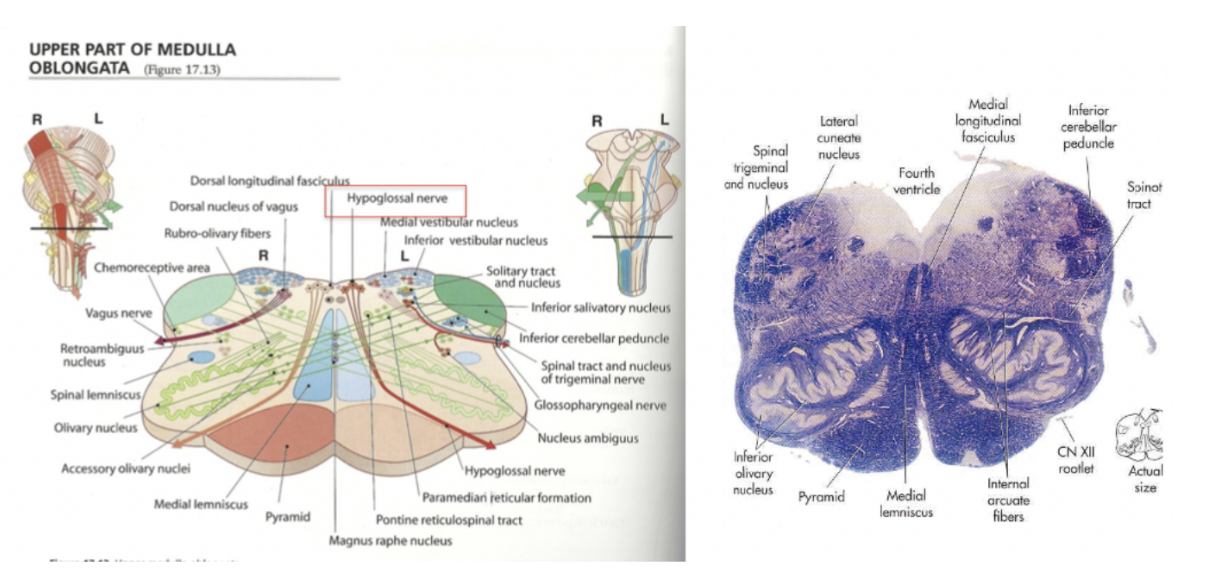
Glossopharyngeal nerve
9th cranial nerve, located in the medulla, with 5 components —
SVE (branchiomotor) component — originates from nucleus ambiguous, innervates stylopharyngeus muscle
GVE component — formed by parasympathetic preganglionic fibers directed to the parotid gland —
Originates from inferior salivatory nucleus, with its fibers passing through the otic ganglion
SVA component — originates from nucleus of solitary tract in medulla, collects taste information
GVA component — collects information from viscera such as carotid body & sinus, pharynx, & middle ear — originates from nucleus of solitary tract
GSA — collects general sensation from the ear, relaying it to the bulbospinal trigeminal nucleus
(small territory around ear lobe shared by facial & vagus nerve)
2 sensory ganglia — superior & inferior (or petrosal ganglia), and it exits at the jugular foramen
Gag reflex
Glosssopharyngeal nerve supplies sensory innervation to the oropharynx, thus carrying the afferent information for gag reflex
When a foreign object toughes the back of the mouth, this stimulates CN9, beginning the reflex
The efferent nerve in this process is the vagus nerve — CN10 — however as it is triggered by CN9, an absent gag reflex signifies damage to the glossopharyngeal nerve
Vagus nerve
10th cranial nerve, originating from the medulla at the level of the retro-olivary groove — very large territory of innervation with 5 components —
SVE (branchial motor) component —
Innervates muscles of larynx & pharynx, with nucleus ambiguous giving rise to these fibers
GVE —
All viscera in thorax & abdomen are innervated through parasympathetic preganglionic fibers —
Originate from dorsal motor nucleus of vagus nerve in medulla, and then are linked to many ganglia & ENS (enteric NS)
GVA —
Collects informatin from all the viscera in which it passes — originate from nucleus of solitary tract
(same nucleus that collects taste info in its most rostral part)
GSA —
Collects general sensation from the ear (with facial & glossopharyngeal brings information from most of territory of the head)
Related to bulbospinal trigeminal nucleus
SVA —
Collects taste information from the tongue, originating from nucleus of solitary tract
Taste information from the tongue
In anterior 2/3 of tongue — collected from intermediate component of facial nerve
Slightly more posteriorly — collected by glossopharyngeal nerve
At level of taste buds at root of tongue, epiglottis, and initial part of larynx & pharynx — vagus nerve
Here we find 2 sensory ganglia — superior & inferior or nodose ganglia
Superior contains somatosensory neurons
Inferior contains viscerosensory neurons
Innervation of muscles of pharynx
Most pharyngeal muscles are innervated by pharyngeal branches of the vagus nerve —
Superior, middle, & inferior pharyngeal constrictor muscles
Palatopharyngeus muscle
Salpingopharyngeus muscle
Muscles of the larynx
Palatoglossus & majority of muscles of soft palate
Since vagus nerve innervates muscles responsible for movement of soft palate, in case of problems in the vagus nerve, we have —
Ipsilateral paralysis of the soft palate, muscles of pharynx & larynx
This can cause dysphonia, dyspnea, dysarthria, & dysphagia
Could have a loss of cough reflex
Accessory nerve
11th cranial nerve, with a spinal & cranial part —
Many of its fibers originate from C1-C5 spine
Cranial part — fibers originating from medulla oblongata
Fibers originating from spinal cord enter skull via foramen magnum, joining to components originating by medulla oblongata
SVE — fibers originating from spinal cord motoneurons are responsible for innervation of — trapezius & sternocleidomastoid muscles
Fibers originating from cranial component, once exiting jugular foramen, abandon XI nerve to join the vagus nerve (accessory)
Hypoglossal nerve
12th cranial nerve — located in medulla
GSE — innervates intrinsic muscles of the tongue, which have a somatic origin — characterized by branches of motor nucleus located in tegmentum of medulla
Clinical relevance — examination & palsy of accessory nerve
Examination —
Patient is asked to rotate their head & shrug their shoulders — both normally & against resistance
Simply observing the patient may also reveal signs of muscle wasting in sternocleidomastoid & trapezius in cases of long-standing nerve damage
Palsy —
Most common cause of accessory nerve damage is latrogenic —
Prodcedures such as cervical node excision biopsy or central line insertion can cause trauma to the nerve
Clinical features —
Muscle watering & partial paralysis of sternocleidomastoid — resulting in inability to rotate head or weakness in shrugging shoulders. Damage to the muscles can also result in an asymmetrical neckline
General rule of cranial nerves & components —
The nerves that emerge close to the midline are thosee that are mostly characterised only by GSE components, while the furthest from the midline also have SSE components — (see book-like opening in NS development)
Cranial nerves “recap”
Cranial nerves emerge ventrolaterally except for the 4th (trochlear) nerve — emerges dorsally
Nerves emerging close to midline are mostly characterized by GSE components, while furthest from midline also have SSE components
Cranial nerves can be grouped by their components —
Visceromotor Parasympathetic (GVE) —
III, VII, IX, X
Motor Somatic (GSE) —
III, IV, VI, XII
Motor Branchial/Visceromotor (SVE) —
V, VII, IX, X, XI
Sensory Somatic General (GSA) —
V, VII, IX, X
Sensory Somatic Special (SSA) —
VIII
Sensory Visceral general (GVA) —
IX, X
Sensory Visceral Special (SVA) —
VII, IX, X