COPD (Chronic obstructive pulmonary disease)
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
What is COPD?
Chronic Obstructive Pulmonary Disease.
It is a collective term for diseases which cause breathing difficulties.
It is characterised by irreversible progressive air flow restriction - air flow becoming worse through airways.
What are examples of COPD?
Chronic bronchitis and emphysema
What are the symptoms of chronic bronchitis?
1. A productive cough (phlegm) for many years
2. Excess sputum produced.
- Produced on a daily basis for several months
What part of the lung is affected by chronic bronchitis?
The bronchioles are effected
What are the symptoms of emphysema?
1. Alveoli are damaged
2. Irreversible enlargement of the terminal air spaces
3. Often developed from chronic bronchitis
What part of the lung is affected by emphysema?
Alveoli
What can COPD be caused by?
Cigarette smoke - main cause
Genetic factors
Air pollution
Burning fossil fuels
Smoking incessance
Working in a dusty environment

What diseases can COPD cause?
One of the long term consequences of COPD (bronchitis and emphysema) is (right) heart failure because the heart has to work harder to pump oxygenated blood around the body.
Other diseases include:
- pulmonary hypertension
- cyanosis
- hypoxia,
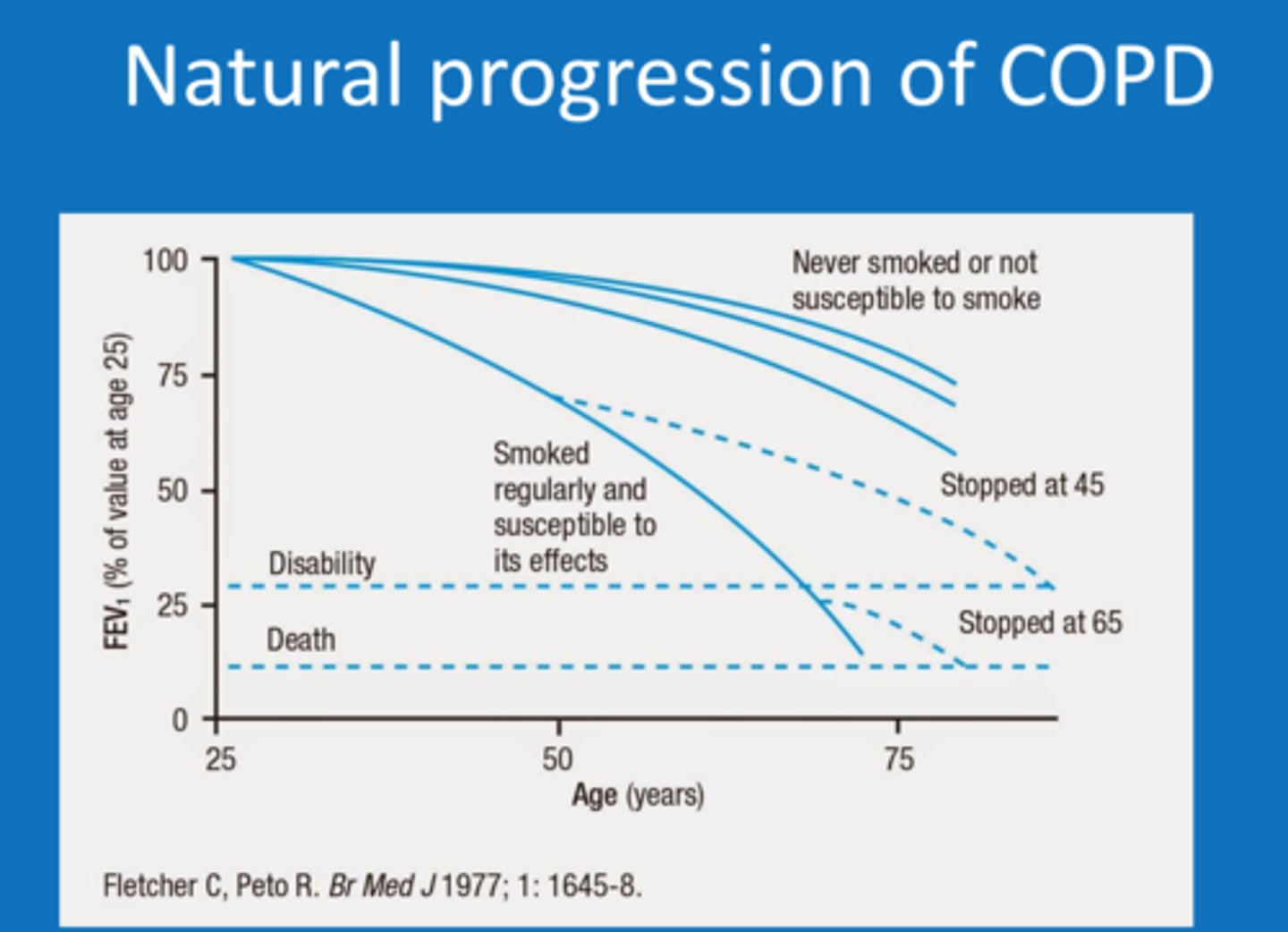
Describe COPD progression
There is a dramatic decrease in lung function as patients get older.
It is often asymptomatic because we can function with 20% reduction in lung function. Therefore many people with COPD are undiagnosed.
COPD tends to be diagnosed later there is a serious decrease in lung function.
Viral and bacterial infections can further decrease lung function. This is related to the fact that COPD patients have a lot of sputum.
Describe COPD incidence
COPD accounts for 5% of deaths globally.
2nd most common cause for emergency hospital admissions.
Costs NHS £1.9 billion per year
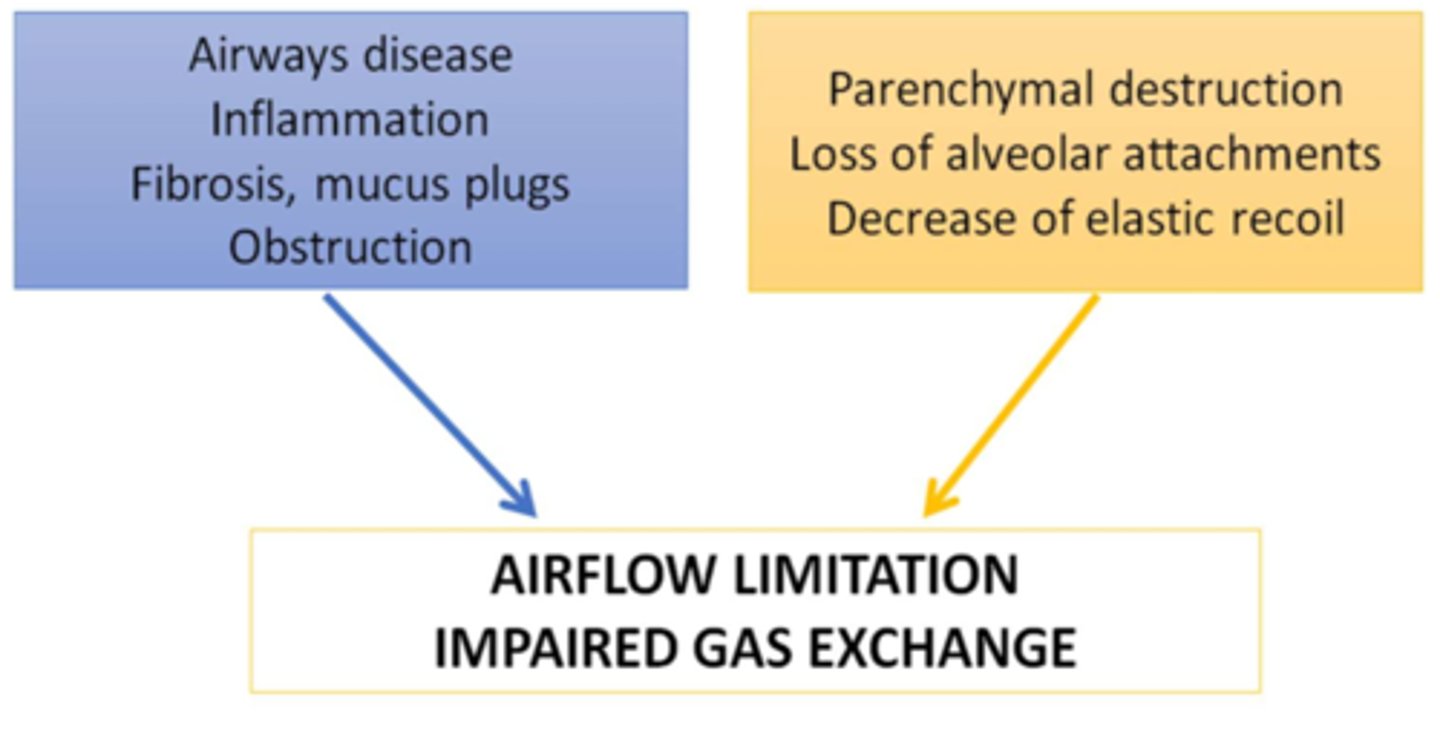
Describe COPD pathophysiology
Smooth muscle layer is larger
Increased mucous product
Not as much space in lumen for air exchange
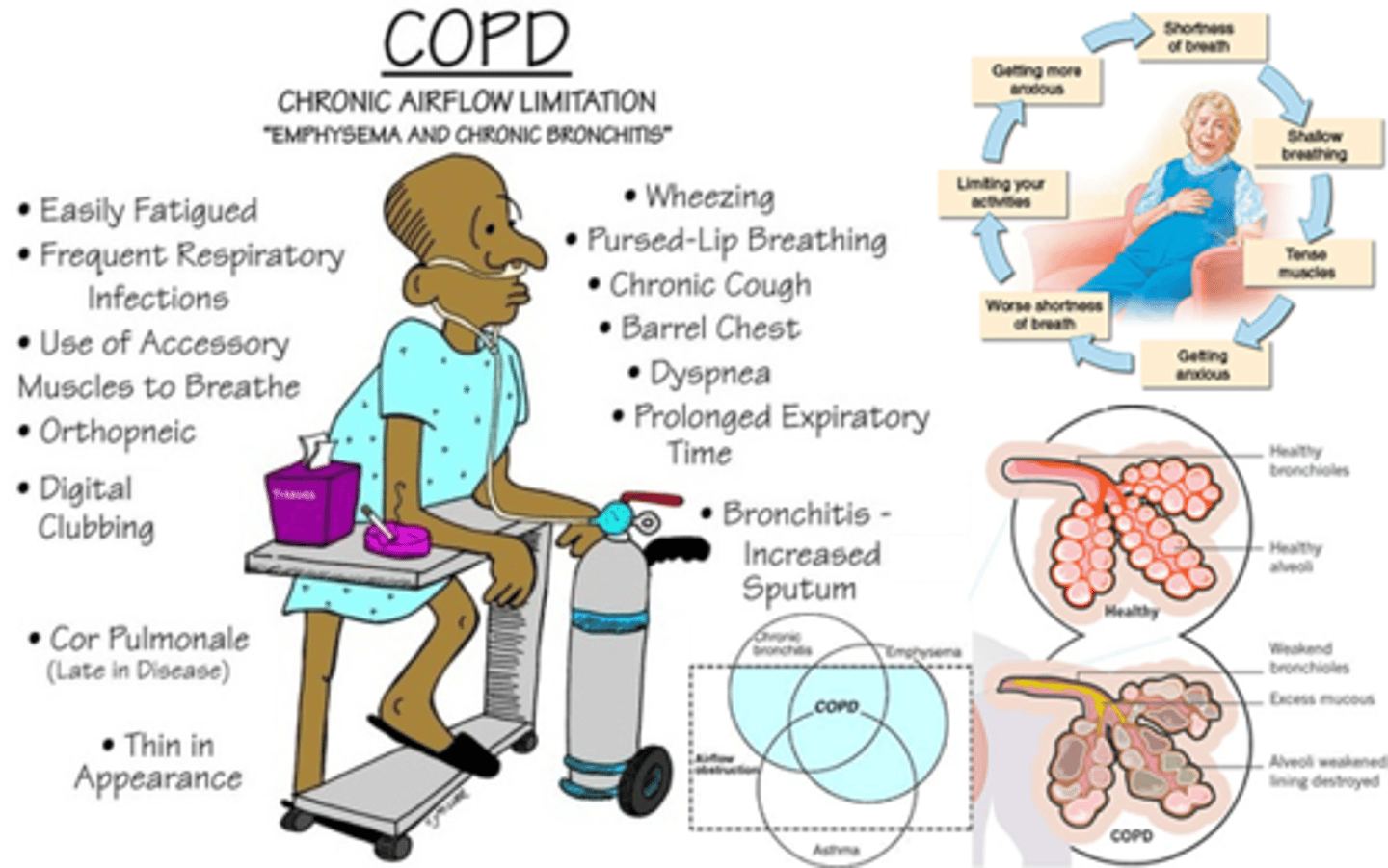
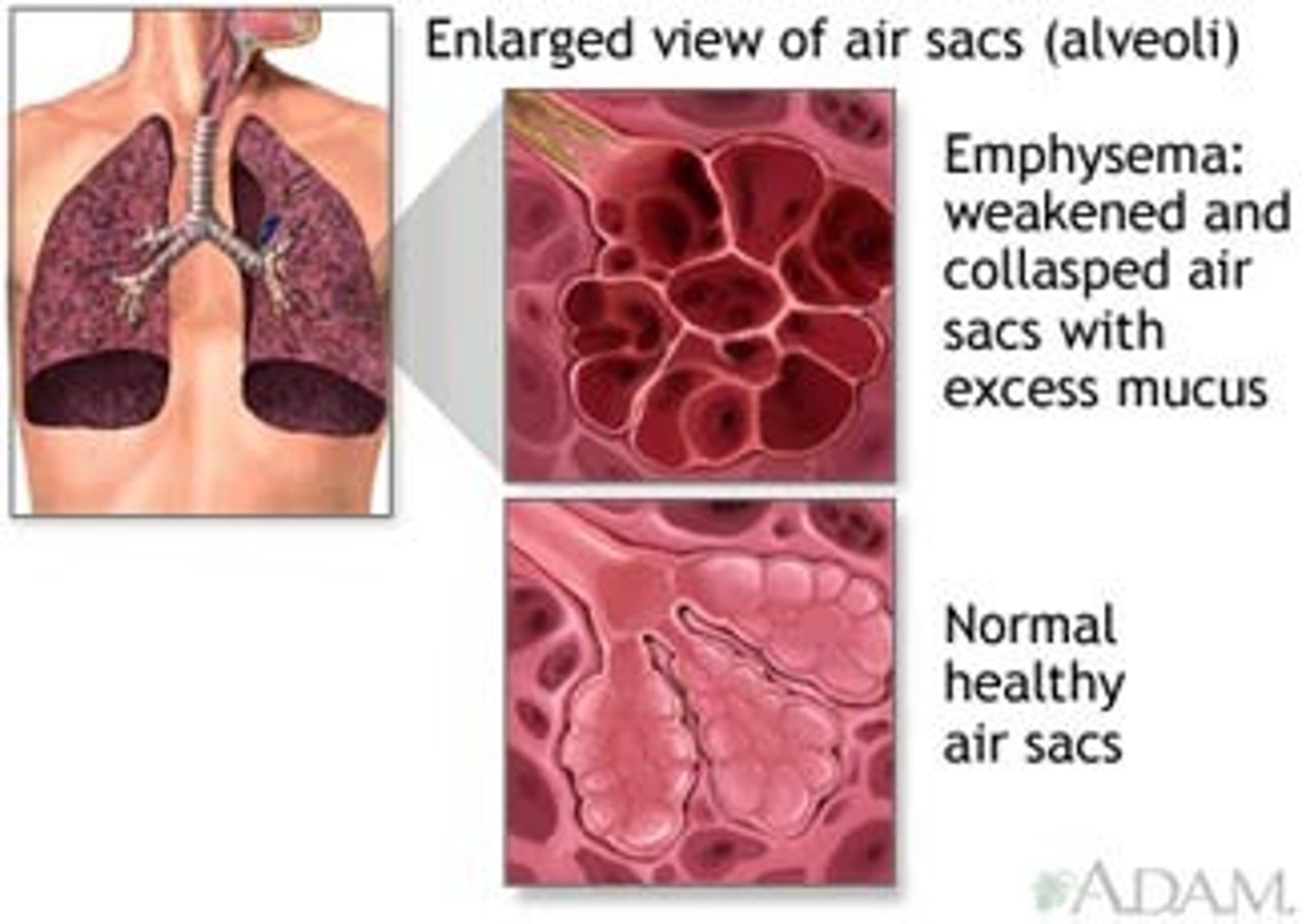
Describe emphysema pathophysiology
Alveoli in the lungs become destroyed, therefore decreased surface area for gas exchange
Structure of alveoli changes (becomes stiffer) as it undergoes fibrosis. Therefore not all air is removed from sac, so gas exchange isn't occurring as efficiently.
Compare and contrast asthma vs COPD
1. Both have increased growth of goblet cells
2. Both get hyperresponsiveness but in COPD there is a limited hyperresponsiveness
3. Air flow reduction isn't variable in COPD, it is a continued decrease. In asthma, air flow reduction is very variable.
4. In asthma there are more eosinophils sputum, in COPD neutrophils (neutrophil-rich sputum) cause damage
5. In COPD, there is Th1 and cytotoxic T cells implicated in disease pathogenesis, whereas in asthma it is onlyTh2 cells
6. In asthma there is subepithelial fibrosis whereas in COPD there is peribronchial fibrosis.
Describe the mechanism of airflow reduction in COPD
There is a thickened smooth muscle wall caused by:
- smooth muscle hyperplasia.
- increased stiffness of airway wall (peribronchial fibrosis)
- inflammatory cells can infiltrate (i.e. macrophages, neutrophils and lymphocytes).
There is also blocking of airways by excess mucous
What are the two mechanisms of mucous production in airways?
Mechanism 1: from mucous glands in airway wall
- Mucous gland increases in size so it generate more mucous
Mechanism 2: goblet cells found on airway surface
- Undifferentiated epithelial cells differentiate into goblet cells
- These goblet cells can also undergo hyperplasia
Describe how excess mucous is produced in COPD
Mucous hypersecretion in COPD is caused by:
- goblet cell hyperplasia
- enlargement of mucous gland
- reduced airflow through bronchi
What controls mucous production?
- Neuronal input
- Inflammatory mediators
Describe how neurones control mucous production
There is stimulation from cholinergic nerves in mucous-secreting cells.
Ach binds to M3 (muscarinic) receptors leading to increased mucous production.
Describe how inflammatory mediators control mucous production
Inhaled irritants trigger the sensory nerves (antidromic response).
Sensory-efferent nerves release neuropeptides released e.g. neurokinins (NK) and SP.
These neuropeptides act on neurokinin receptors on mucous-secreting cells.
What is the role of elastases?
Proteases which break down proteins e.g. elastin in connective tissue in the lungs.
Describe how inflammation is caused in COPD
1. Increased cytokines:
- Inflammatory cells can produce inflammatory mediators which damage cells in the respiratory system e.g.
- increased mucin secretion from epithelium in vitro
- induced elastase production
Proteases such as elastases are normally inhibited but reactive oxygen species inhibit protease inhibitors and increase protease activity.
2. Leukocyte products
- Reactive oxygen species - act on signalling cascade involving inflammation. Can activate expression of inflammatory genes AND damage the epithelium.
- Chemoattractant (IL-8, LTB4) - bring more leukocytes to the area to cause more damage.
3. Leukocytes infiltrate the site e.g.
- macrophages: break down connective tissue, stimulate mucous production
- CD8+ T cells (implicated in inflammatory cascade)
- neutrophils in infection
What are the consequences of inflammation in COPD?
1. Epithelial damage
- Decrease ciliary cell function
- Increase mucus secretion from goblet cells
- Mucus cell hyperplasia - more and larger cells
- Increased bronchial permeability
- Airway oedema and protein exudation (increased protein in fluid in lumen)
2. Stimulation of sensory nerves
- Neurogenic inflammation
- Cough
Describe how inflammation in COPD causes cough
Cough reflex is triggered when we detect the trigger chemical.
Cough in order to get rid of it. Sensory nerves are stimulated which send a signal to diaphragm and intercoastal muscles (diaphragm contracts).
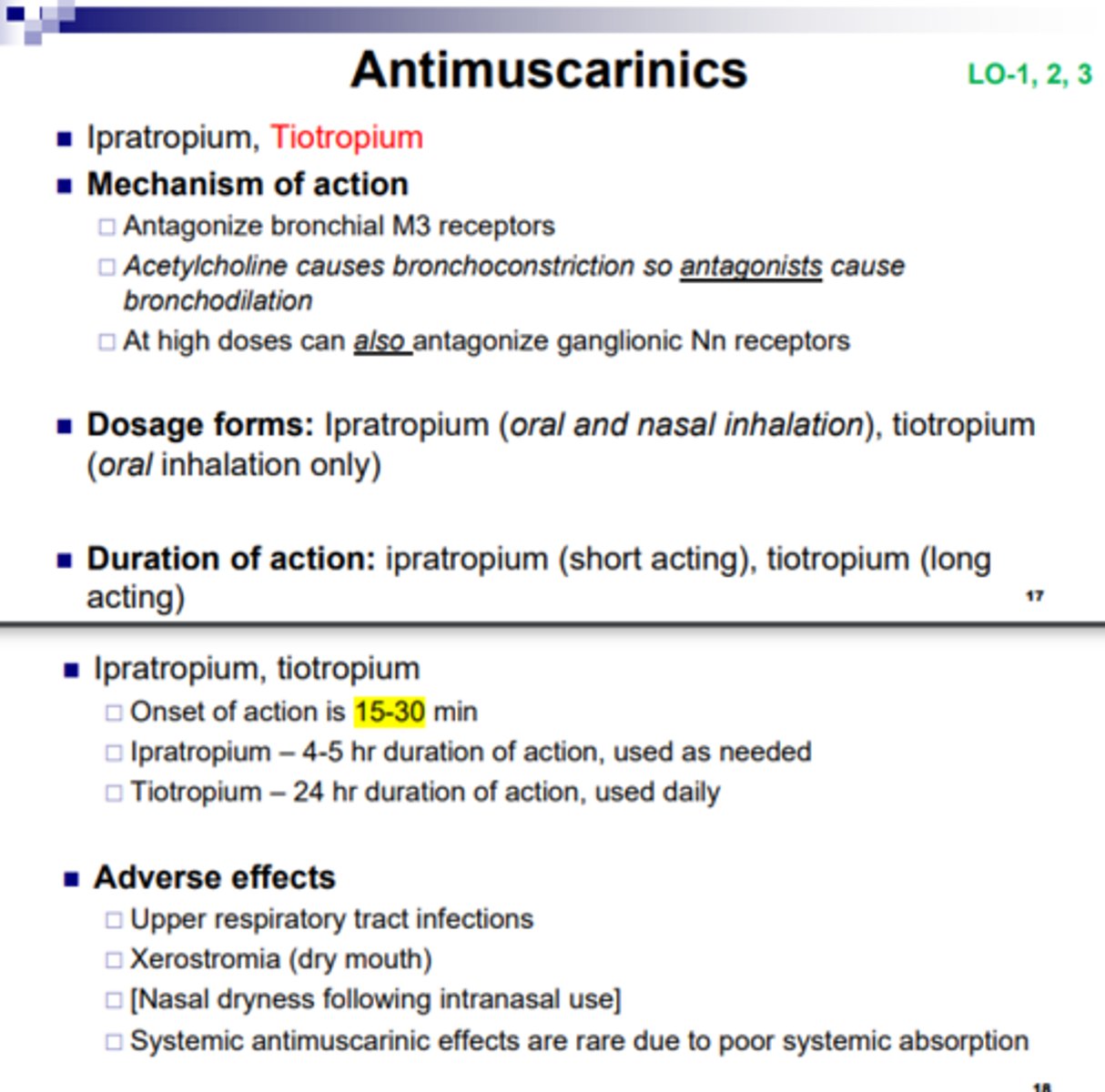
Describe bronchodilators as a treatment for COPD
Bronchodilators aren't used as treatment often because bronchoconstriction is not a major cause of the airway obstruction.
Beta-2 agonists have limited effects
Muscarinic antagonists have some use
Give examples of bronchodilators which could be used in COPD treatment
Muscarinic antagonist:
- Tiotropium
- Aclidinium
These are DPIs
Describe tiotropium mechanism of action
It binds to M3 receptors to prevent acetylcholine binding to M3 receptors on glandular cells. This decreases muscle contraction. It also blocks parasympathetic stimulation of secretion
It only has a transient effect on M2 receptors so it maintains an element of Ach negative feedback
Describe phosphodiesterase inhibitors as a treatment for COPD
There are many different PDE isoforms, but we only use PDE4 inhibitors.
If we inhibit PDE4 in airway smooth muscles it causes bronchodilation.
If we inhibit PDE4 in leukocytes it stops:
- TNF alpha release
- Chemotaxis and degranulation
by increase intracellular cAMP in airway smooth muscles.
Give examples of phosphodiesterase inhibitors which could be used in COPD treatment
Phosphodiesterase inhibitors:
- Roflumilast
- Theophylline (weak and non-selective)
Describe mucolytics as a treatment for COPD
They break down mucous by breaking down the disulphide bonds in cysteine. N-acetyl cysteine has anti-oxidant activity.
Give an example of a mucolytic which could be used in COPD treatment
N-acetylcysteine
Describe corticosteroids as a treatment for COPD
Corticosteroids reduce inflammation
- Inhaled steroids are for acute exacerbations (flares)
- There is a small benefit from inhaled steroids for maintenance
- Given in combination with muscarinic antagonists
Give examples of corticosteroids which could be used in COPD treatment
beclomethasone, budesonide
Describe proteases, specifically elastases
Proteases are released in inflammation but there is a natural inhibitor to stop its release.
Elastases are proteases which degrade alveoli.
Elastases are produced by neutrophils and macrophages.
Alpha1 anti-trypsin is the natural inhibitor for elastases.
Alpha1 anti-trypsin is found in the liver
Describe the role of proteases in emphysema
Lung elastases are strongly implicated in emphysema.
In emphysema, there is an imbalance in the formation of proteases and antiproteases.
Elastase degrades elastin in the basement membrane in connective tissue
Smoking increases activity of elastase. Smoking can cause oxidant stress which also decreases activity of serpins (natural inhibitor of some proteases)
Give examples of antiproteases which could be used in emphysema treatment
- Alpha1-antitrypsin augmentation therapy could be used in patients with an alpha1-antitrypsin deficiency
-Elastase inhibitors: these have not been as effective as expected in clinical trials
Give examples of antioxidants which could be used in emphysema treatment
-Vitamins C and E
-N-acetyl cysteine
-Limited evidence for efficacy
-Omega-3 ?
What are future therapies which may be used in COPD treatment? Give examples
1. IL-5 therapies
- There are is a large number of eosinophils in some individuals so anti-IL-5 and anti-IL-5 receptor antibodies can be used.
2. Thioredoxin
- regulates redox status (stops reactive oxidant species) and protease/anti-protease balance
- blocks NF and MAPK signalling
3. Brensocatib
- Inhibits neutrophil elastase
- In Phase II clinical trial
Give examples of anti IL-5 therapies
-Benralizumab, mepolizumab, reslizumab
(Anti IL-5 and anti-IL-5 receptor antibodies)
Why don't asthma drugs in COPD?
1. Bronchodilators
- Airway flow reduction is due to tissue remodelling and secretion of mucous in COPD it is not due to bronchoconstriction like in asthma.
2. Anti-inflammatory Glucocorticosteroids
- Oxidative stress decreases steroid activity
- Neutrophil apoptosis is inhibited by Glucocorticosteroids. Neutrophils cause damage in COPD.
- Apoptosis of eosinophils by Glucocorticosteroids isn't useful in COPD (only useful in asthma where eosinophils are causing most damage)
Describe glucocorticoid effects in COPD
1. Glucocorticoids bind to glucocorticoid receptors
2. Inhibits HAT (histone acetyl transferase) which represses gene expression
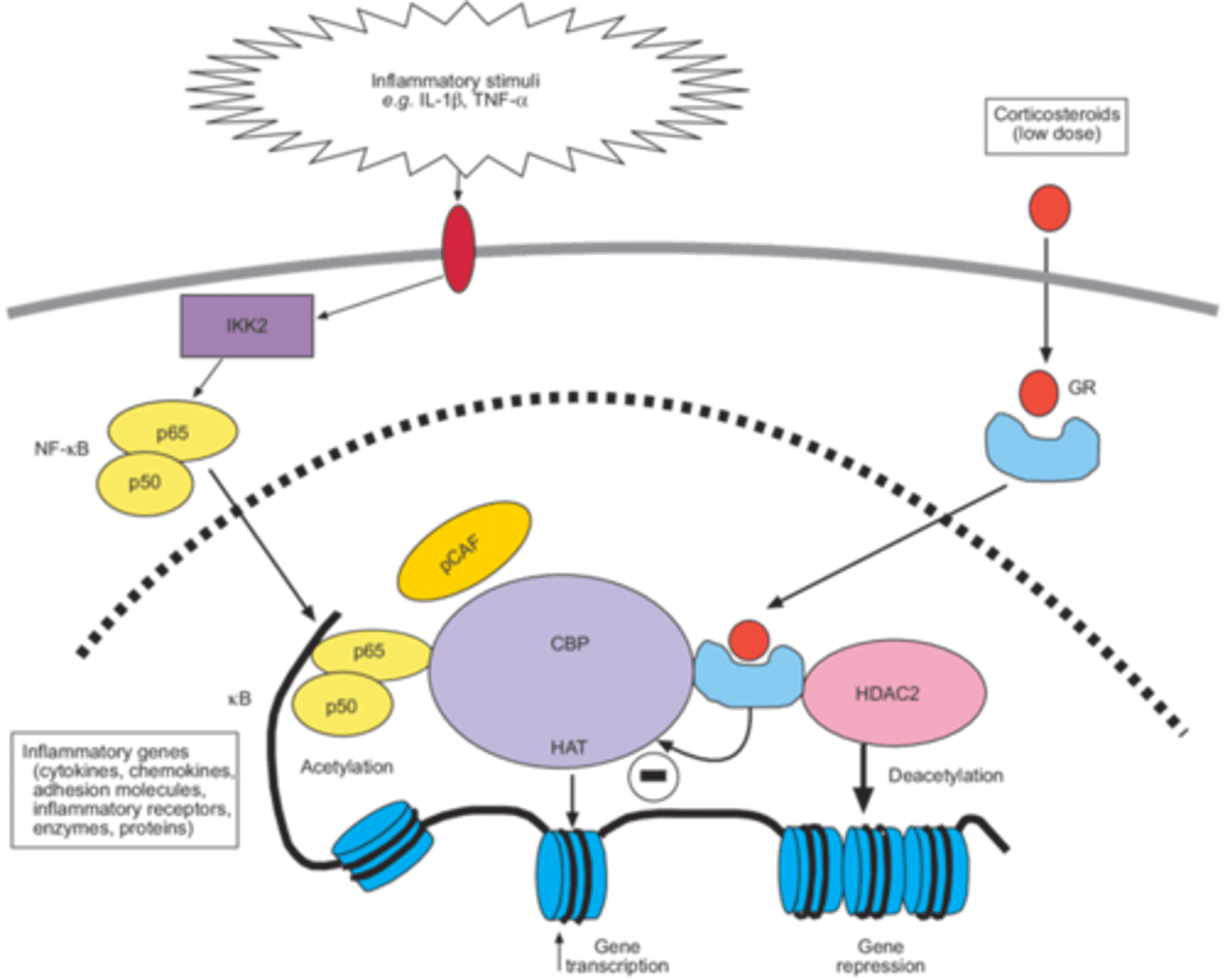
Describe the effect of smoke and glucocorticoid in COPD
Cigarette smoke decreases glucocorticoid receptor binding. Therefore, there is:
- Increased activity of HAT (histone acetyltransferase): so more transcription e.g. of inflammatory genes
- Decreased effect of HDAC (histone de-acetylases) so there is decreased suppression of transcription of inflammatory genes.
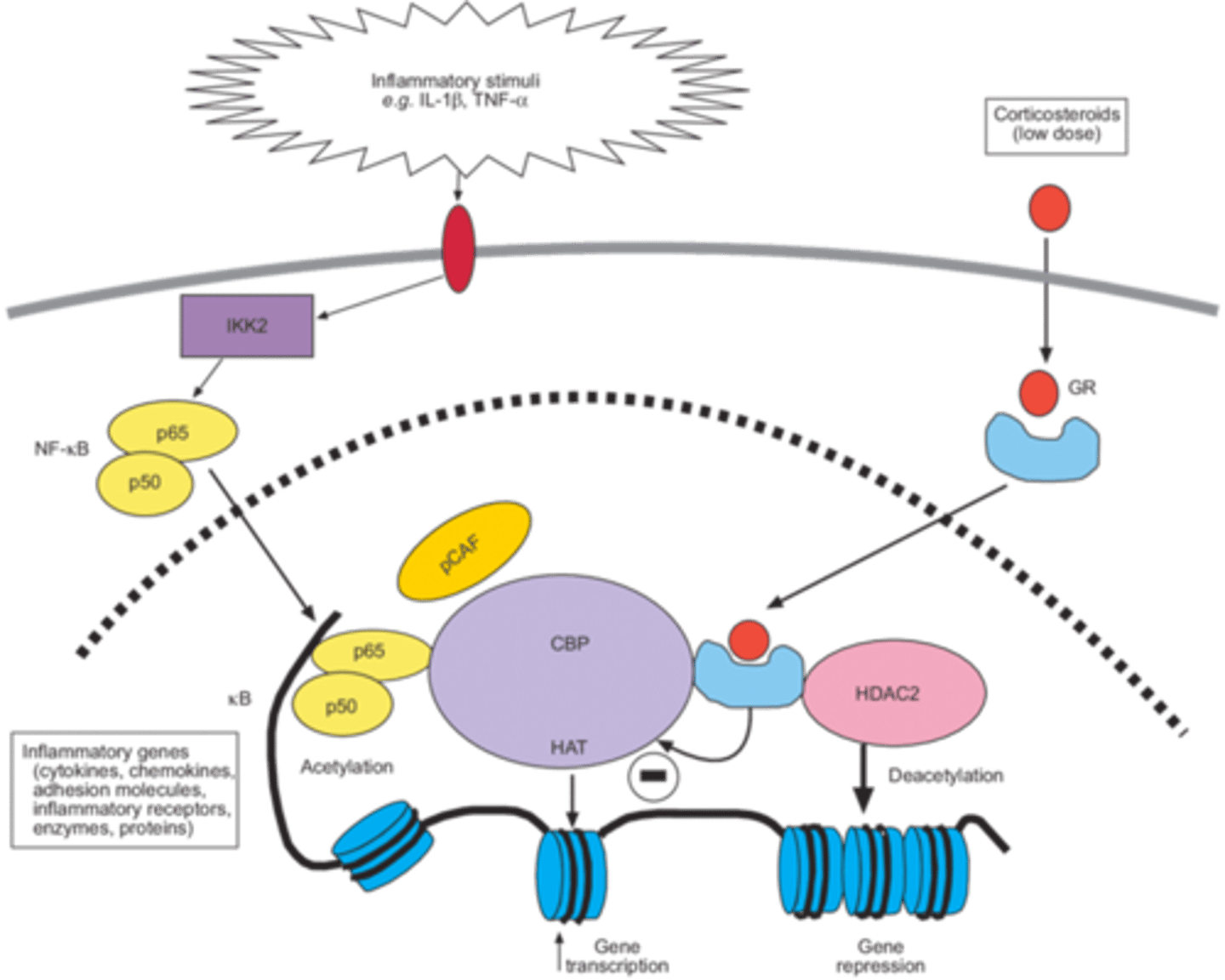
Describe how cigarette smoke could decrease HDACs (histone deacetylases) in COPD
1. Cigarette smoke generates oxygen free radicals
2. Inflammatory leukocytes produce nitric oxide
3. Combine together to form peroxynitrite
4. Peroxynitrite targets histone deacetylase, leading to HDAC destruction
5. Results in increased inflammatory gene transcription
- Not inhibited by glucocorticoids
Describe vaping
Vaping products contain nicotine
Could also contain: carcinogens, toxic chemicals, and toxic metal nanoparticles
Vaping triggers lung inflammation and injury and potentially oxidative stress (oxidative stress markers have been identified in serum).
Why wouldn't vaping be allowed on the market as a drug?
Vaping would not be allowed on the market as a drug because:
- Insufficient clinical data
- Long term effects are not understood
- Poor regulation and monitoring
- Additives poorly defined
Give examples of glucocorticoids which could be used in COPD treatment
Budesonide, formoterol