Lec+10+Principles+Infec+Dis+%26+Epi+2024+v2
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
case fatality rate vs mortality rate
case fatality rate (CFR, severity) = # of deaths / time
mortality rate: # deaths/time period
attack rate
the proportion of people who become ill with a disease in an at-risk population initially free of the disease (from beginning to end of an outbreak)
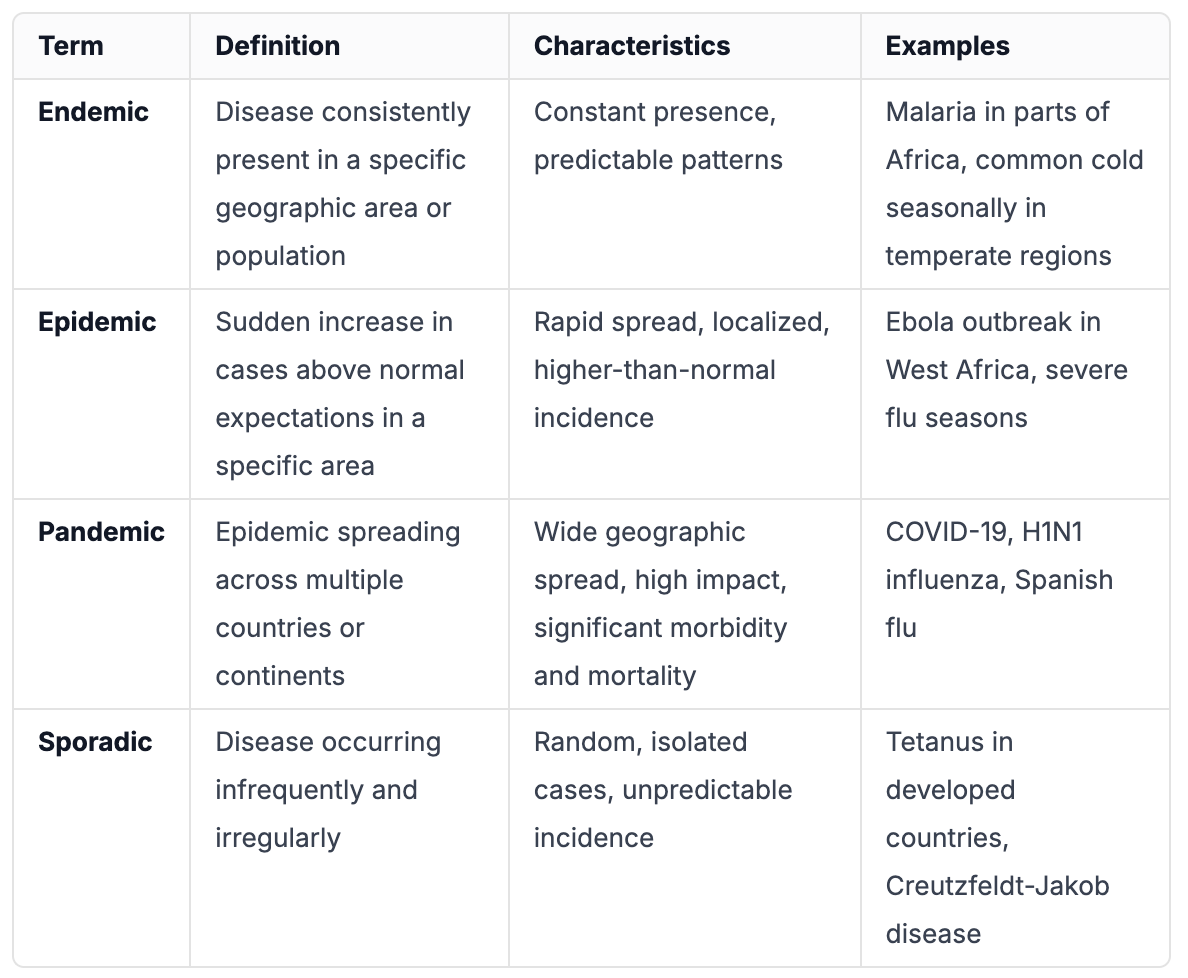
endemic vs epidemic vs pandemic vs sporadic
chain of infection
Certain conditions must be met in order for a microbe or infectious disease to be spread from person to person.
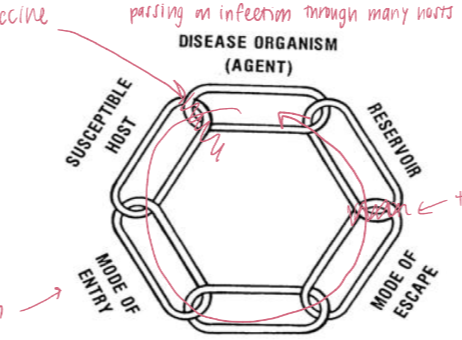
can only occur when all six links in the chain are intact. By breaking this chain at any of the links, the spread of infection is stopped
definitive vs intermediate host
Definitive host – protist or helminth attains maturity or passes sexual stage
Intermediate host – protist or helminth is in larval or asexual state
types of reservoirs
human: carriers
animal: zoonoses
environmental: soil (bacteria), water
reservoir vs non-reservoir
reservoirs does not experience the symptoms of disease when infected by the pathogen, whereas non-reservoirs show symptoms of the disease
how microorganisms enter the body
Skin (including percutaneous, bites, wounds,burns)
Eyes (e.g., bacterial, viral)– Gastrointestinal tract
Respiratory tract
Urogenital tract
Placenta
Portal of entry can be important
Yersinia pestis: pneumonic versus bubonic
where microorganisms leave the body
Body fluids
Feces
Respiratory
airborne droplets
Urine
Semen
Blood (transfusion, accidental needle-stick, IVDU)
Milk
modes of transmission
Direct Transmission -- direct contact
horizontal
direct contact
direct projections
vertical
congenital
perinatal
Indirect Transmission:
direct exposure to agent in soil, infected animal
Vehicle-borne
Vector-borne
Mechanical
Biological
Airborne Transmission
Sexually transmitted
direct transmission of disease
Horizontal
Direct contact -- touching, biting, kissing or sexualintercourse
Direct Projections -- droplet spray onto mucousmembranes of conjunctiva, eye, nose or mouth duringsneezing, coughing, spitting, or talking (<1 meter)
Vertical:
Congenital -- congenital disorders are structural and functional defects present at birth and are the result of cross-placental infection
Perinatal – shortly before, during, and after birth
Direct exposure to agent in soil, infected animal in placenta
indirect transmission of disease
Vehicle-borne (no multiplication in or on vehicle)
Contaminated fomites (inanimate materials or objects)such as toys, handkerchiefs, clothes, bedding, cooking or eating utensils, doorknobs, elevator buttons
Water (e.g., fecal-oral)
Food (e.g., fecal-oral)
Milk
Biological products (blood, plasma, organs)
Inoculation, injection, piercing
Vector-borne: arthropods that transmit diseases tohumans, e.g., ticks, flies, fleas, lice, mosquitoes
Mechanical vectors (e.g., flies and Vibrio cholerae)
Transmission passively
Disease transmission does not require replication inthe vectors
Biological vectors (e.g., mosquitoes and dengue virus)
Active transmission–
Pathogen replicates in vector; often necessarycompletion of microbial life cycle in vector
An incubation period is required before transmissionof infective form
airborne transmission of disease
dissemination ofmicrobial aerosols to a suitable portal of entry, usually by the respiratory tract
Aerosols – small residue result from evaporationof fluid from droplets
Particles 1-5 um are easily drawn into the alveoli of lungs, remain suspended for long periods
Dust, soil particles small droplets - can be drawn
Ro
reproductive rate
the number of people that one sick person will infect is
host microbe relationships
Mutualism: both benefit (bacteria in digestive tract, vitaminK)
Parasitism: parasitic microbe benefits, host is harmed (Note: spectrum—slight harm to death)
Commensalism: one species benefits, other neither benefits nor is harmed skin bacteria
Antagonism: both species harm each other
levels of host-microbe relationships
Colonization – “normal flora”
Infection – replication of any parasite in or on the host
Subclinical/asymptomatic infection
Disease – any disturbance of the normal functioningof the host by parasite
types of pathogens
pathogen: An organism that is capable of causingdisease
Non-pathogen: An organism that is not usuallycapable of causing disease
Opportunist: An organism that only causes diseasewhen the host is compromised
AIDS
Immunosuppressive drugs
iceberg concept of infection
metaphor used in epidemiology and public health to illustrate the spectrum of disease severity and the proportion of cases that are visible versus those that are hidden. This concept helps in understanding that the cases of disease we see (the tip of the iceberg) are only a small fraction of the total number of cases that actually exist.
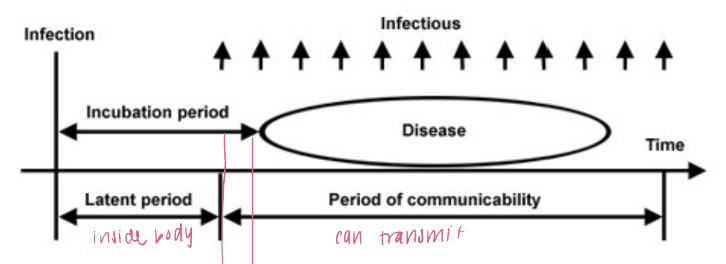
incubation period
he time interval between initial contact with an infectious agent and the first appearance of symptoms associated with the infection
epidemiologic triad

microbial virulence
capacity of an infectious agent, compared together closely related infectious agents, to produce disease in a host. Virulence depends on a variety of microbe and host factors
types:
Entry and adhesion
Colonization and infection
Invasion
Exotoxins
Endotoxins
host pathogen co evolution
pathogens evolve to maximize their transmission and survival
If severity decreases the likelihood of transmission (e.g., by reducing host mobility), then less virulent pathogens will be favored. Pre-mature death of host can result in death of virus and can lead to non-transmission.
If virulence aids transmission (e.g., extreme fluid release of diarrheal diseases, coughing in respiratory diseases)then the more virulent pathogens will out-compete
Attenuation (weakening) by sub-culturing on/in laboratory
infectivity
Entry – Adherence
Specific molecules for adherence to host cells
Colonization and Infection
Nutrient availability – e.g., the battle for iron
Host: transferrin, lactoferrin
Bacterial pathogens: siderophores
toxins (microbial virulence)
potent poisons produced bymicroorganisms
Destroy host cells
Interfere with normal function– Many exotoxins are phage-encoded
Two main types of toxins
Exotoxins (proteins
Toxic proteins released from growing cells; generally heat labile
Travel from site of infection and cause damage at distant site
Subset of exotoxins – enterotoxins – exotoxins affecting the gastrointestinal tract, usually small intestine
types
cytolytic toxins
AB toxins
superantigen
Endotoxin (LPS)
Gram negative bacteria – LPS
Cell bound, released when cell lyses
Heat stable
host factors
Genetics– cell receptors– genetic traits (sickle cell trait and malaria)– HLA type (MHC)
Age: old and young usually more susceptible
Gender – e.g., structure of urinary tract (UTI)
Pregnancy
Nutritional status
Co-morbidities: obesity, diabetes, hypertension
Hormonal balance– Glucocorticoids can depress immune system (stress, lack ofsleep)
Integrity of organ system
Abnormal urinary tract predisposes to urinary tract infections
Smoking can predispose to respiratory tract infections
Integrity of immune system – immunocompromise
Immune status: previous exposure or vaccination
Behavior: smoking, diet, drinking, sexual practices,exercise
Structural inequities affect risk factors for infectious diseases
Lack of access to nutritious foods in inner cities, presence of processed foods, sodas obesity
RF plus lack of access to health care hypertension, diabetes
lack of access to hospitals/ICUs
unplanned urban settlements with poor waste and sanitation
Environmental Factors for infectious diseases
Physical
Weather, climate, geology
Ecological zone
Biological
Sources of food, water, and air–
Presence of vectors, flora and fauna
Social and cultural
Density, crowding, adequate housing, war,sanitation, availability of health care
Agricultural practices
primary prevention of diseases
Methods to avoid occurrence of disease.
Most population-based health promotion efforts are of this type
secondary prevention of disease
methods to diagnose and treat existent disease in early stages before it causes significant morbidity.
how to interrupt Chain of Infection
Eliminate source of agent
Prevent further exposures– Detect & treat cases
Personal hygiene: hand-washing, control coughing, sneezing, prevent airborne transmission
Disposable needles
Safe drinking water (hand-washing)
Waste-handling, management
Proper food-handling
Barriers: condoms, bed nets, respiratory