Cardiovascular Physiology
1/356
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
357 Terms
Cardiovascular System
A circulatory system evolved to support the complexity of large multicellular organisms.
Diffusion alone is insufficient to transport nutrients and remove waste over long distances.
Circulation maintains steep concentration gradients near cells, enabling rapid material exchange.
Hemodynamics
Basic signs of cardiovascular health include cardiac output or arterial pressure, and blood circulation.
Explains the physical laws which govern blood flow.
Looks at the relationship between blood flow, BP, and resistance.
Ohm’s Law
F = ∆P/R
Where F is flow (mL/min)
∆P is the pressure difference between two fixed points (mmHg).
R = resistance to flow (mmHg/mL/min)
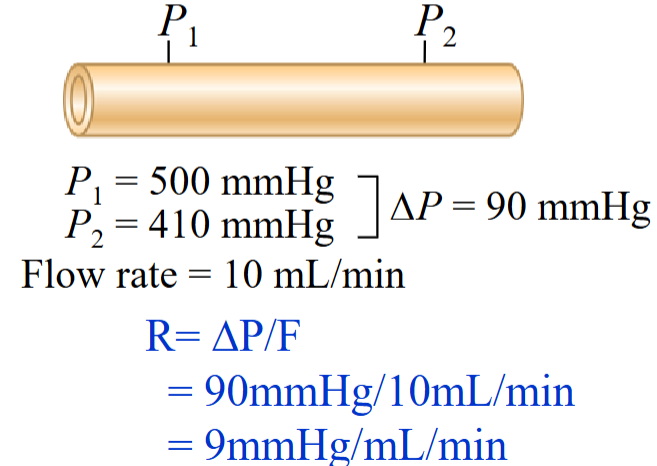
Flow
Blood flow is directly related to the pressure difference between two fixed points and inversely proportional to resistance.
High to low pressure.
It is the pressure difference between two points that creates flow, not the absolute pressure at each point.
To have flow, ∆P > R.
Hydrostatic Pressure
Pressure exerted by a fluid.
The major mechanism for changing flow in the cardiovascular system is to alter the resistance of the BVs (specifically arterioles).
This will change flow and perfusion of the tissues + organs in our body.
Blood Friction
Blood is not a homogenous fluid.
Although plasma is composed of water, it also contains molecules such as electrolytes and proteins such as albumin and fibrinogen.
Formed elements of blood: RBCs, WBCs, and platelets.
Interactions between these components in blood produces friction.
Resistance.
Viscosity
Friction between molecules of a flowing fluid.
Hematocrit affects viscosity.
# of RBCs in the blood.
The more viscous the blood is, the more friction is produced, the greater the resistance to flow.
Has a limited range and does not contribute significantly to resistance.
Concentric
Blood flows through in vessels in concentric layers.
The movement of adjacent layers of blood flow through a vessel helps to reduce energy losses in the flowing blood by minimizing viscous interactions between the adjacent layers of blood and the wall of the blood vessel.
Length
Determines amount of contact between moving blood and stationary wall of vessel.
A vessel with longer length will produce more friction.
Blood flows through vessel in concentric layers.
Diameter
Determines amount of contact between moving blood and stationary wall of vessel.
Can change based on constriction or dilation.
A large diameter blood vessel = less friction.
Small diameter blood vessel = more friction.
Poiseuille’s Equation
R = 8ηl / πr⁴
R = resistance to blood flow
η = viscosity of blood
l = length of vessel
r = radius of vessel (raised to fourth power)
Poiseuille’s Equation Relationship
The relationship between viscosity, vessel radius, and vessel length, defined by this equation, which states that resistance is equal to 8ηl / πr⁴.
Applies to laminar flow.
Cardiovascular System Functions
To deliver oxygen and nutrients and remove waste products of metabolism
Fast chemical signaling to cells by circulating hormones or neurotransmitters
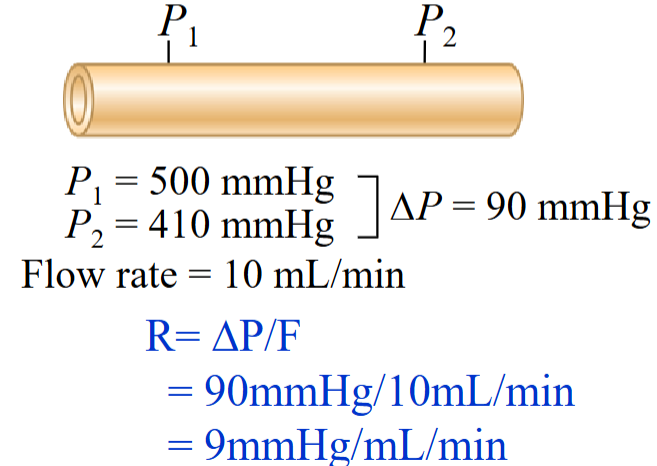
Thermoregulation
Mediation of inflammatory and host defense responses against invading microorganisms
Main Organs
Heart (the pump)
Blood vessels (the pipes)
Blood (the fluid to be moved)
Thermoregulation
A homeostatic process that maintains a steady internal body temperature despite changes in external conditions.
Heart
The pump; pumps the blood through the circulatory system by rhythmic contraction and dilation.
Blood Vessels
Channels that carry blood throughout your body.
Blood
The fluid being moved.
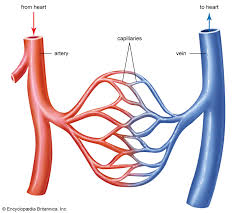
Arterioles
Small branching vessels with high resistance.
Capillaries
Transport blood between small arteries and venules; exchange of materials.
Smallest BV in the body.
Play an important role in the exchange of materials.
Permeable to plasma and most solutes, except plasma proteins.
Arteries
Part of the circulation system by which blood (oxygenated) is conveyed from the heart to all parts of the body, away from the heart.
Veins
Part of the blood circulation system of the body, carrying in most cases oxygen-depleted blood toward the heart.
Venule
A very small vein, especially one collecting blood from the capillaries.
Closed Circulatory System
Blood confined to vessels.
Generates greater pressures.
Moving blood to be pumped faster in our bodies.
Atria
Thin-walled
Low pressure chambers
Receive blood returning to the heart
The left and right atria are conduits that receive blood turning back to the heart.
Ventricles
Forward propulsion of blood.
Thicker walls than the atria and responsible for the forward propulsion of blood.
Septa
A wall, dividing a cavity or structure into smaller ones.
Interatrial Septum
Separates left and right atria.
Interventricular Septum
Separates left and right ventricles.
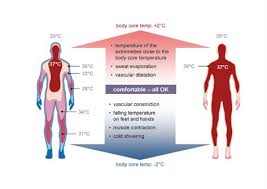
Dual pump
Left Side: pumps highly oxygenated blood to the systemic circuit.
Right Side: pumps poorly oxygenated blood to the pulmonary circuit.
Most arteries carry highly oxygenated blood away from the heart.
Carrying Blood
Vessel Type | Normal Function | Exception |
|---|---|---|
Arteries | Oxygenated blood away from heart | Pulmonary arteries: deoxygenated to lungs |
Veins | Deoxygenated blood to the heart | Pulmonary veins: oxygenated from lungs |
Pulmonary Circulation
Blood to and from the gas exchange surfaces of the lungs
Blood entering lungs = poorly oxygenated blood
Oxygen diffuses from lung tissue to blood
Blood leaving lungs = oxygenated blood
Systemic Circulation
Blood to and from the rest of the body
Blood entering tissues = oxygenated blood
Oxygen diffuses from blood to body tissues
Blood leaving tissues = poorly oxygenated blood
Left Heart
Receives blood from pulmonary circulation and pumps to systemic circulation.
Right Heart
Receives blood from systemic circulation and pumps to pulmonary circulation.
Series Flow
Within the cardiovascular system.
Blood must pass through the pulmonary and systemic circuits in sequence
Parallel flow
In the systemic circuit, each organ is supplied by a separate artery.
Blood does not flow between organs.
Each organ receives fully oxygenated blood and regulates its own flow.
Exception: Liver
Also receives blood from digestive organs via the portal vein.
This blood is partially deoxygenated.
Pericardium
A fibrous sac that encloses the heart and great vessels.
Stabilization of the heart in thoracic cavity
Protection of the heart from mechanical trauma, infection
Secretes a pericardial fluid to reduce friction
Limits overfilling of the chambers, prevents sudden distension
Pericardium - Stabilization
The outer layer of the pericardium is attached to components within the thoracic cavity, including the coastal cartilage, diaphragm, and sternum.
The ligamentous attachments limit the hearts motion within the chest cavity.
Pericardium - Infection
A fluid-filled sac that protects mechanical truama to the cehest.
Also protects from infection.
Pericardium - Friction
The fluid lubricates layers of the heart as it contracts and twists in the pericardial space.
Pericardium - Distension
As it is a fibrous sac, its distensibilituy is limited.
Does not stretch properly; will resists a rapid increase in cardiac size, preventing over-distension.
Fibrous Pericardium
Outermost layer of the pericardial sac.
Provides, protects. and stabilizes heart in the thoracic cavity (attaches to structures in the chest such as the coastal cartilage, diaphragm, and sternum).
Composed of connective tissue.
Serous Pericardium
Composed of the parietal and visceral pericardium.
Layer composed of cells that secrete a fluid.
Parietal Pericaridum
Composed of cells that secrete a fluid.
Lies underneath the fibrous pericardium and is attached to it.
Pericardial cavity
Pericardial fluid decreases friction.
Separates the parietal pericardium from the visceral pericardium.
Visceral Pericardium
The innermost layer of the paracardial sac.
Lies next to the heart and a part of the heart wall.
Layers of the Pericardium
At the base of the great vessels, the parietal layer folds over and continues as the visceral layer on the heart surface.
The fibrous and parietal pericardium are fused.
The parietal and visceral layers are separated by the pericardial cavity.
These layers secrete fluid into the cavity to reduce friction.
Pericarditis
Pericarditis is inflammation of the pericardium.
Causes include bacteria, trauma, fungi, viruses, or malignancy.
Increases capillary permeability, leading to fluid buildup in the pericardial cavity.
Severe cases compress the heart, limit movement, and prevent proper chamber filling.
Cardiac tamponade
Compression of heart chambers due to excessive accumulation of pericardial fluid.
Can be treated aspiring the fluid with a needle and treating the cause of fluid buildup.
Heart is unable to pump blood.
Decreases ventricular filling.
Left Ventricle
thicker (wall) than the right ventricle.
Develops higher pressure.
The increased thickness allows the left ventricle to generate higher pressures as it contracts.
the increased pressure allows the left ventricle to pump blood around the entire systemic circulatory system.
Right Ventricle
Pouch-like in shape.
Only needs to pump blood to the lungs, so it does not need to develop increased pressures.
Myocardium
Muscular wall.
Cardiac muscle (myocytes), BVs, nerves.
Endothelium on BVs
The heart valves and the BVs are lined by endothelium, which forms a interface between the blood and the heart chamber of the BV wall, providing a smooth surface for blood to flow over.
The three layers are bound on both ventricles and atria, with variation between the two.
The ventricles have more muscle.
Endocardium
Endothelium covering inner surfaces of heart and heart valves
Myocyte
Cardiac muscle cell.
Branched (“Y”) and joined longitudinally
Allows for greater connectivity; one Y-shaped myocyte may be attached to two different myocytes.
Striated, one nucleus per cell, many mitochondria (energy; ATP).
Intercalated disk
Interdigitated region of attachment.
Desmosones and gap junctions.
The opposing membrane of two different myocytes are closely opposed and very intertwined at their region of attachement.
Desmosomes
Anchor cells together in tissues subject to considerable stretching
Mechanically couple cells.
Contains cadherins → anchors cells together.
Connections are strong.
Gap Junctions
Communicating junctions
Transmembrane channels linking adjacent cells
Electrically couple heart cells
Small molecules and ions
Spreading action potentials across the atria or ventricles
Myocardium
Consists of interlacing bundles of cardiac muscle fibers.
Arranged spirally around circumference of heart
Wringing Effect
When the cardiac muslce contracts and shortens, a wringin effect is profuced, efficiently pushed blood upwards towards the exit of major arteries.
Figure 8 - Step 1
Chamber walls contract like a squeezing fist, applying pressure to the blood.
Cardiac muscle fibers are arranged in a figure 8 around the atria and base of the great vessels.
Deeper ventricular fibers also form a figure 8, extending toward the apex.
Superficial ventricular layers wrap around both ventricles.
Figure 8 - Step 2
Atrial contraction pushes blood into the ventricles.
Ventricular contraction reduces chamber diameter and pulls the apex upward in a twisting motion.
This spiral motion directs blood upward toward the major arteries.
Spiral arrangement ensures efficient ventricular emptying.
Valves
Thin flaps of flexible, endothelium-covered fibrous tissue attached at the base to the valve rings.
Leaflets or cusps.
Collagen.
The semilunar valves or atrial vales are found between the ventricles and the arteries where the ventricles pump their blood.
Valve Rings
Cartilage.
Site of attachment for the heart valves.
Stabilizes position.
Valve Blood Flow
One-way valves open due to forward pressure gradients.
No energy or muscles are required—movement is passive.
Valve opens when pressure is greater behind it.
Valve closes when pressure is greater in front, preventing backflow.
Valves cannot open in the reverse direction.
Valve - Unidirectional Flow
There is unidirectional flow of blood through heart.
The orientation of the four valves ensures unidirectional flow.
Important so blood flowing into doesn’t mix with the blood flowing out.
Atrioventricular (AV) Valves
AV valves are located between atria and ventricles.
Prevent backflow into atria during ventricular contraction.
Open when atrial pressure exceeds ventricular pressure, allowing ventricular filling.
Close when ventricular pressure exceeds atrial pressure.
Tricuspid Valve
Right AV valve
Three leaflets (cusps)
Bicuspid valve (Mitral Valve)
Left AV valve
Two leaflets (cusps)
AV Valve Apparatus
Cusps, chordae tendineae and papillary muscles.
Prevents eversion of the AV valves into the atria during contraction of the ventricles.
Valves open and close due to pressure gradients, not from contraction and relaxation of papillary muscles.
AV Valve Apparatus - Relaxed
the aortic semilunar valve is close, the bicuspid valve is open, the chordinae tendinae are slack and they have low tension.
The papillary muscle and the cardiac muscle are relaxed.
The left ventricles will fill with blood as the bicuspid valve is open and when the aortic valve is closed.
Left artia → open AV valve → left ventricke.
AV Valve Apparatus - Contract
As the left ventricle fills, it contracts and increases internal pressure.
When ventricular pressure exceeds atrial pressure, the bicuspid valve closes.
Papillary muscles contract, pulling chordae tendineae taut to prevent valve prolapse.
Once ventricular pressure exceeds aortic pressure, the aortic valve opens, allowing blood to exit.
Chordae tendineae
Tendinous-type tissue
Extend from edges of each leaflet to papillary muscle
Papillary Muscles
Cone shaped muscles
Contraction of papillary muscle causes the chordae tendineae to become taut
Holds the valve in closed position.
Arterial (Semilunar) Valves
Between the ventricle and artery
Pulmonary Valve
Pulmonary trunk, right ventricle
Aortic Valve
Aorta, left ventricle
No chordae tendineae, papillary muscles
Prevent the backflow of blood from the arteries into ventricles when ventricles relax
Semilunar Valves
No valve apparays associated with the semilunar valves.
The arties into which the ventricles eject their blood do not contract.
As a result, when the semi-lunar valves close and the ventricles begin to relaz, they do not need musclar craces the hold them in a closed postion.
Pressure is not high enough to force eversion/
Cardiac Skeleton
Fibrous skeleton is dense connective tissue.
Separates atria from ventricles.
Electrically inactive—blocks direct impulse spread.
AV node and Bundle of His are the only electrical link between atria and ventricles.
Provides structural support.
Anchors valve leaflets and myocardium.
Helps coordinate depolarization by isolating conduction paths.
Coronary Circulation
Movement of blood through tissues of the heart.
Blood in heart chambers does not exchange nutrients with myocardial cells.
Diffusion from chamber blood is too slow to meet metabolic demands.
The heart requires a constant O₂ and nutrient supply for ATP production.
Relies heavily on aerobic metabolism with little anaerobic capacity.
Coronary Arteries
Originate at aortic sinuses at base of ascending aorta.
the aortic sinus is at dilation or an out-pocketing of the ascending aorta.
The left and right coronary arteries lead a branching network of smaller vessels that run along the surface of the heart and dive deeper into the heart wall.
Coronary Veins
Drain into the coronary sinus, which empties into the right atrium.
Coronary Sinus
The cardiac veins collect deoxygenated blood from the myocardium (heart muscle).
These veins drain into a large vessel which acts is a collection site for this blood.
Then empties directly into the right atrium, allowing the deoxygenated blood from the heart tissue to re-enter the circulation.
Systole (Contraction)
Myocardial blood flow almost ceases.
Compression reduces vascular diameter, increases resistance, and decreases blood flow.
Diastole (Relaxation)
Myocardial blood flow peaks
Coronary Artery Diseases
Coronary artery disease due to atherosclerosis of coronary arteries
Atherosclerosis
Arteries supplying blood to heart become hardened and narrow due to plauqe in arterial walls.
Begins with an injury to an artery wall such as smoking, high BP, or increase of blood lipids and cholestrol.
Plaque
Fat, cholesterol, calcium, other substances in the blood
Reduces lumen of vessel and blood flow
A fatty stretch develops at the site and smooth muscle grows over the lesion.
Fibrous tissue covers the smooth muscle and calcium invades the tissue to harden it, forming a plaque.
Angina
chest pain or discomfort
blood flow to heart muscle is reduced
Myocardial infarction
Heart attack.
Blood supply to the heart is completely blocked, muscle dies.
Occurs if the plaque is so large it covers the artery.
The Cardiac Syncytium
Cardiac muscle cells (myocytes) communicate with each other, called a syncytium
Set of cells that act together
Functional Syncytium
The cardiac muscle cells are so tightly bound that when one of these cells become excited, the AP spreads to all of them.
if one cell is excited, the excitation spreads over both ventricles (or both atria)
2 syncytia: atrial syncytium and ventricular syncytium
All-or-None Property
The synchronous excitation and contraction of myocardial cells is required to produce the force necessary to pump blood throughout the body.
Cardiac Muscle
Contractile Cells: mechanical work of pumping, propel blood; do not initiate action potentials.
Conductive Cells: initiates APs.
Action potentials lead to contraction of heart muscle cells.
Automaticity (autorhythmicity)
Cardiac muscle contracts in the absence of neural or hormonal stimulation, as a result of APs it generates itself.
Contractile Cells
Mechanical work of pumping, propel blood; do not initiate action potentials.
Contract when stimulated by an AP passed to them through gap junctions.
Adjacent cells that have been stimulated by an AP or stimulated by a conductive cell.
Conducting Cells
Specialized myocytes (1%) initiate and conduct action potentials.
Do not rely on nervous or hormonal stimuli.
Contain few myofibrils and do not contribute to contraction or blood movement.
Conducting system.
Membrane Potential
Difference in electrical potential between the interior and exterior of a cell
More negative inside than outside at rest
Provides an electrical force that influences the movement of ions across a membrane.