A&P - 5.1 Layers of the Skin
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
integumentary system
skin and its accessory structures
functions of the integumentary system
protection - of underlying tissues and organs against impact, abrasion, fluid loss, and chemical attack
excretion - of salts, water, and organic wastes by integumentary glands
maintenance of normal body temperature - through either insulation or evaporative cooling, as needed
production of melanin - which protects underlying tissue from ultraviolet radiation
production of keratin - which protects against abrasion and serves as a water repellent
synthesis of vitamin D3 - a steroid that is subsequently converted to calcitriol, a hormone important to normal calcium metabolism
storage of lipids - in adipocytes in the dermis and in adipose tissue in the hypodermis
detection - of touch, pressure, pain, and temperature stimuli, and the relaying of that information to the nervous system
introduction to skin
most accessible organ
skin (integument) accounts for approximately 16% of your total body weight
skin’s surface is constantly worn away, attacked by micro-organisms, irradiated by sunlight, and expose to environmental chemicals
integument
a tough outer protective layer
the tissue surrounding an organism’s body or an organ within, such as skin
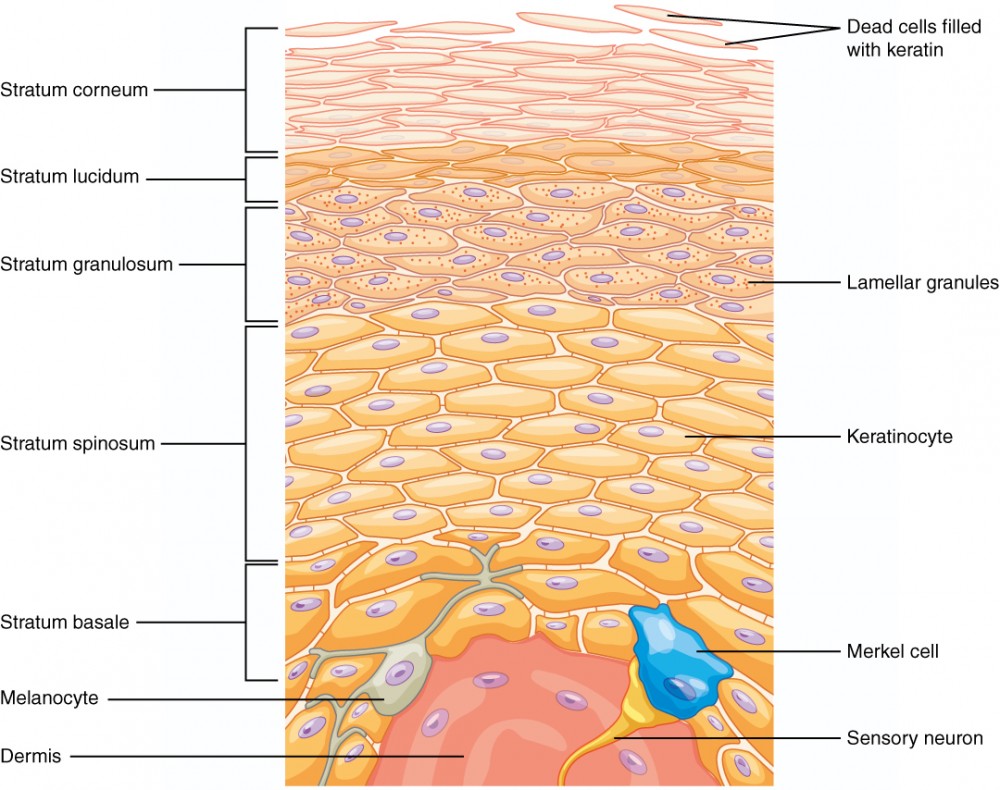
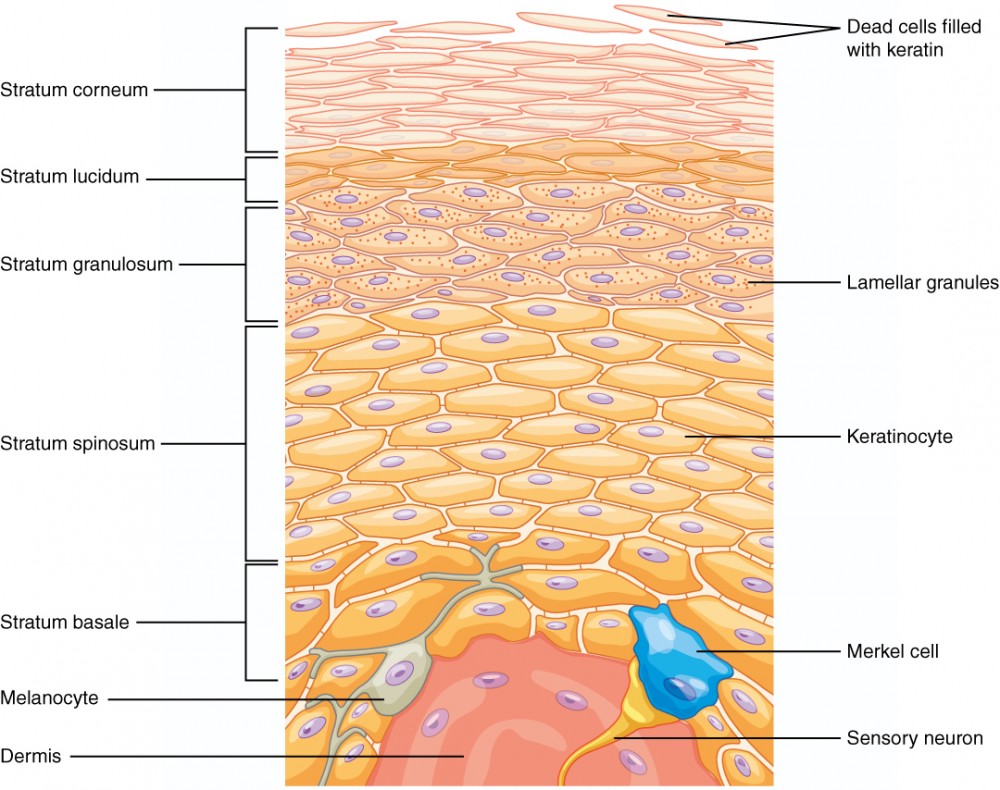
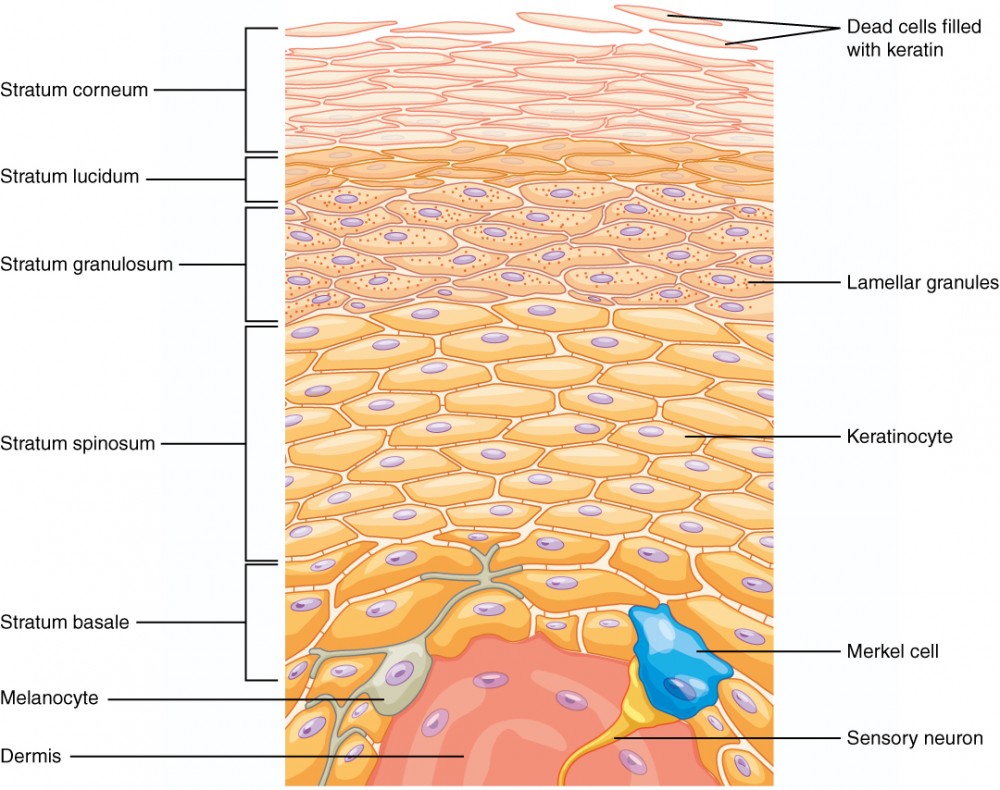
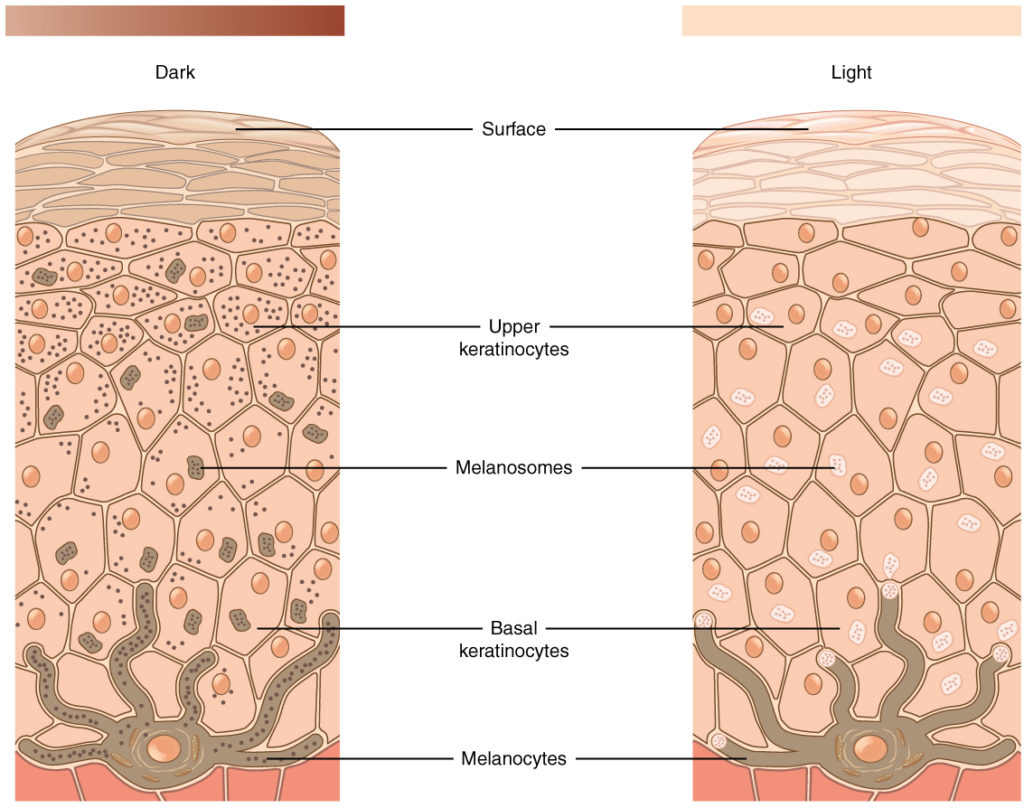
layers of skin
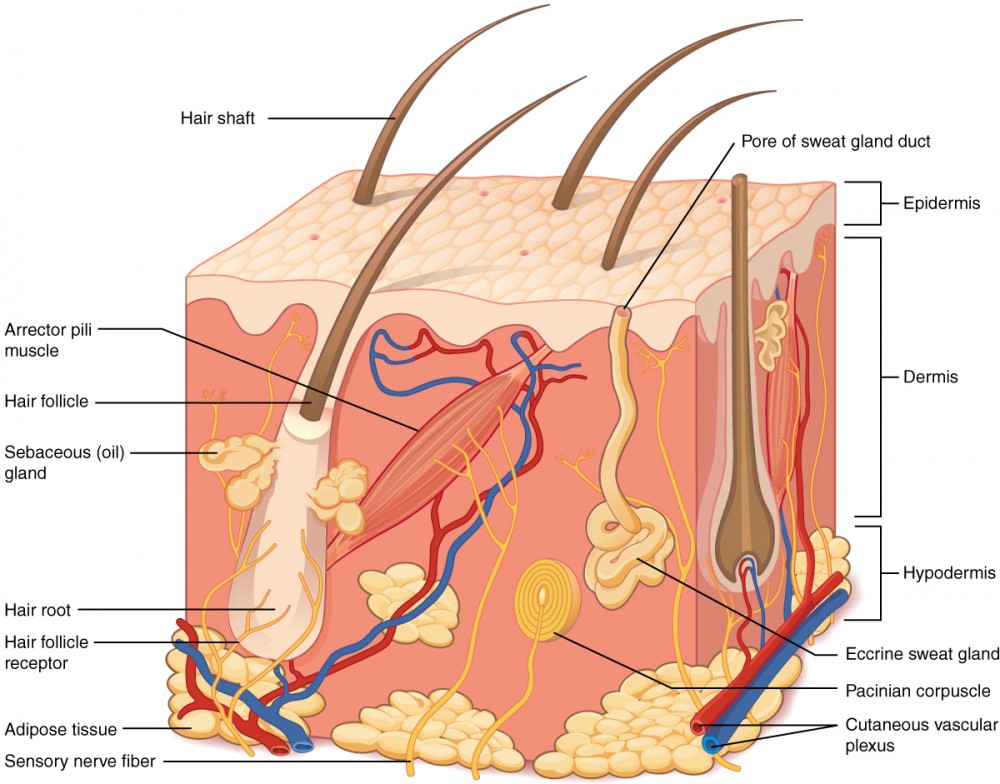
two main layers:
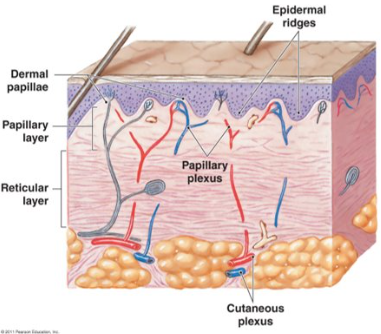
epidermis - made of closely packed epithelial cells
dermis - made of dense irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures
hypodermis - beneath the dermis lies the hypodermis, which is composed mainly of loose connective and a lot of adipose tissue
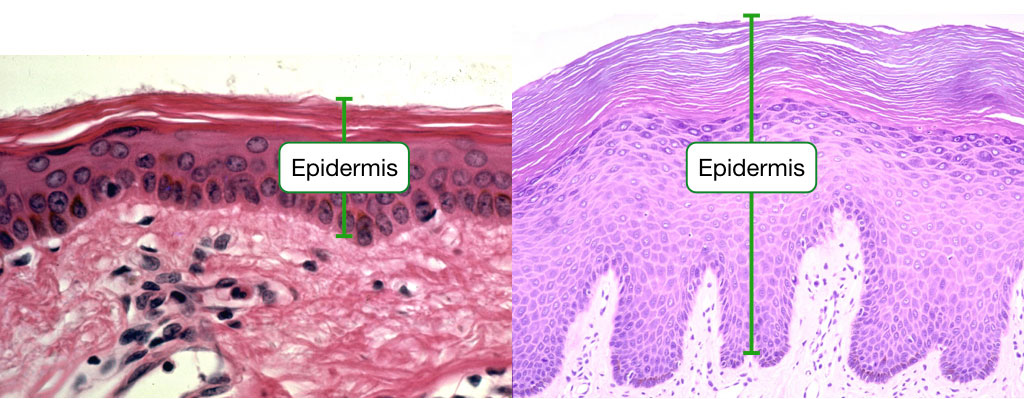
epidermis
outermost tissue layer of the skin
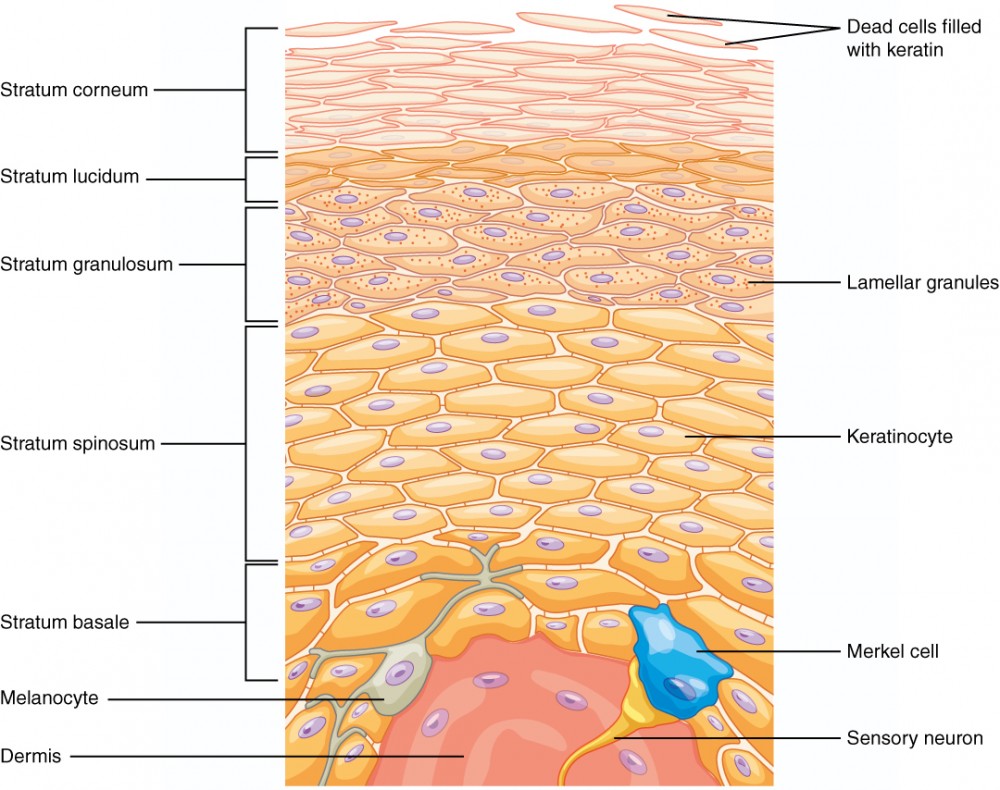
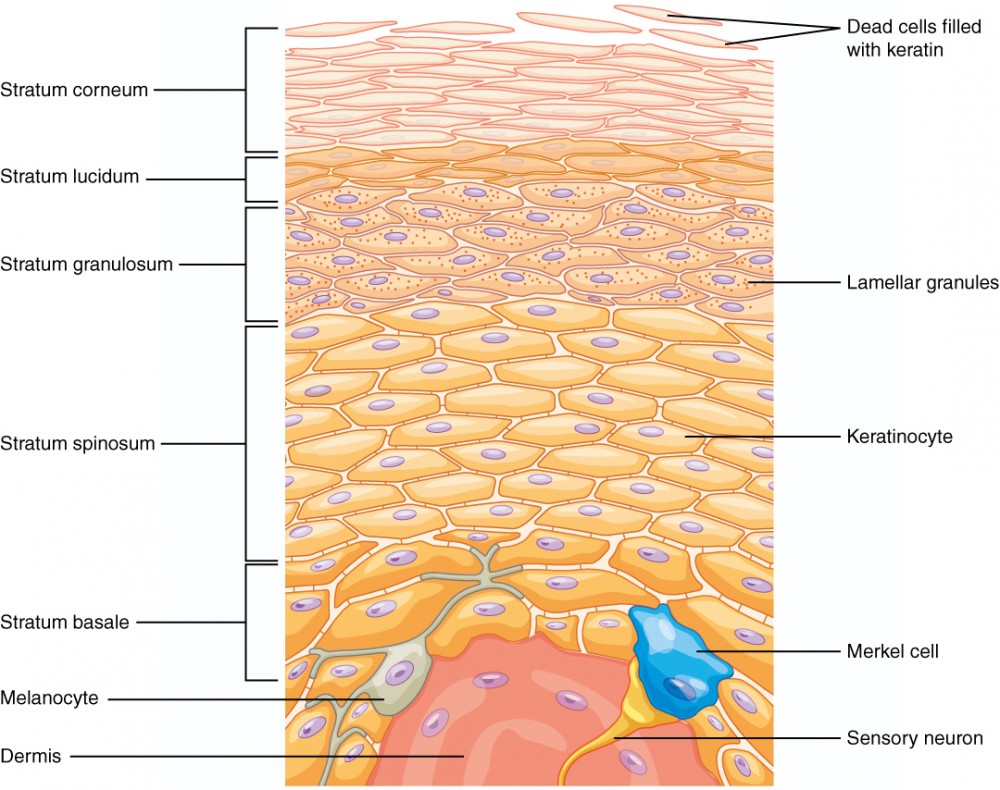
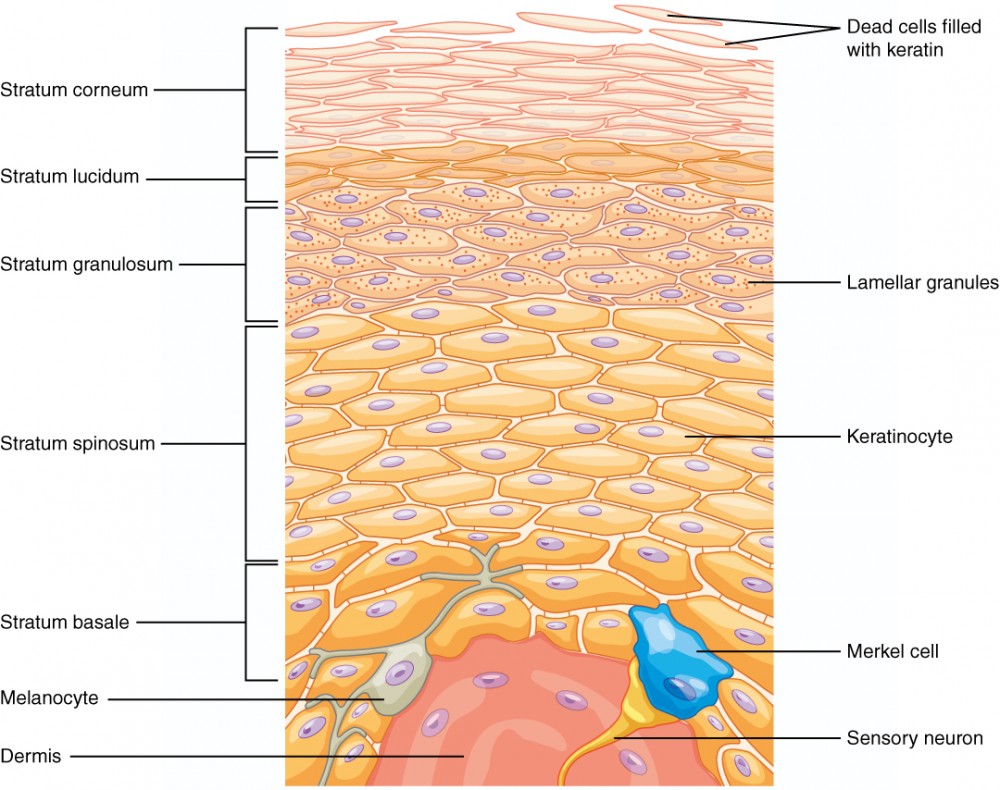
composed primarily of keratinocytes arranged into layers called strata
image shows the difference between thin and thick skin
thin skin epidermis has 4 strata layers
thick skin epidermis has 5 strata layers (palms and soles)
keratinocytes
cell that produces keratin and is the most predominant type of cell found in the epidermis
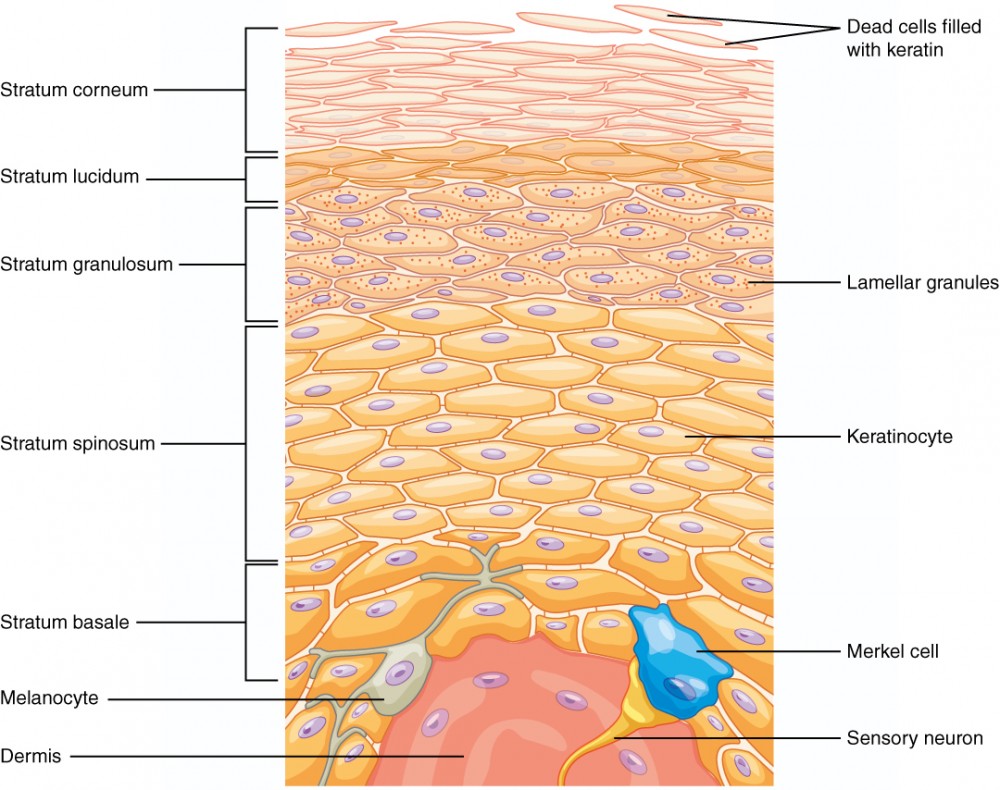
strata (layers) of the epidermis
stratum corneum
stratum lucidum
stratum granulosum
stratum spinosum
stratum basale
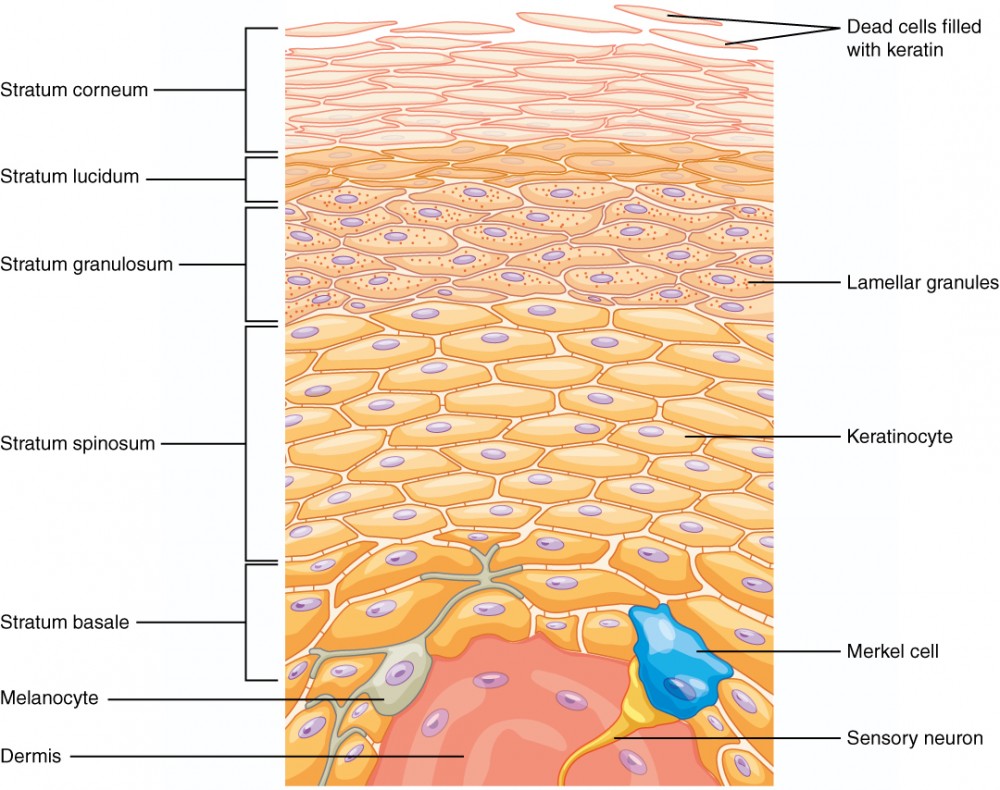
stratum corneum
the “horny layer”; outermost layer (most superficial layer)
15-30 layers of dead keratinized cells (corneocytes) held together by desmosomes
corneum; dead skin falling off
water resistant, not waterproof since we lose water through insensible perspiration (unable to see or feel) and sensible perspiration (sweat)
desmosome
structure that forms an impermeable junction between cells
stratum lucidum
the “clear layer” THICK SKIN ONLY
layer of the epidermis between the stratum granulosum and stratum corneum'
found only in thick skin covering the palms, soles of the feet, and digits
flattened, densely packed dead cells filled with keratin
keratin
type of structural protein that gives skin, hair, and nails its hard, water-resistant properties
stratum granulosum
the “grainy layer”
layer of the epidermis superficial to the stratum spinosum
3-5 layers of keratinocytes that have stopped dividing and started producing keratin
cells grow thinner and flatter and cell membrane becomes less permeable
keratohyalin
granulated protein found in the stratum granulosum which accumulates as lamellar granules within the cells
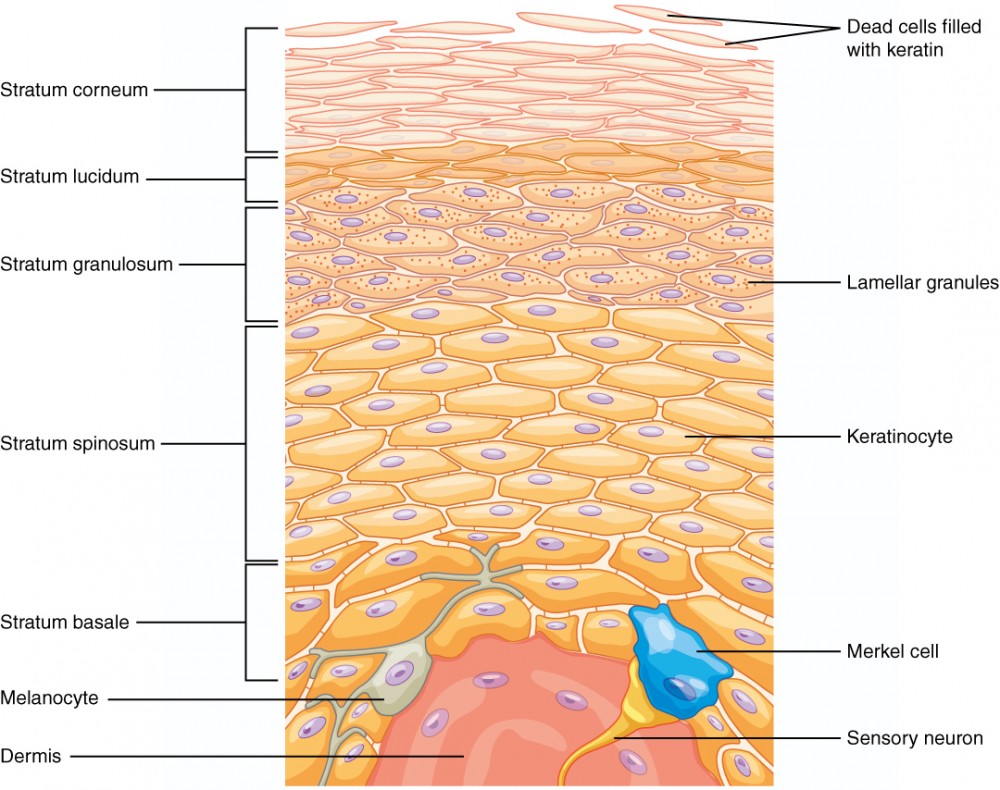
stratum spinosum
the “spiny layer”
layer of the epidermis superficial to the stratum basale, characterized by the presence of desmosomes
8-10 layers of keratinocytes bound together by desmosomes
contains dendritic (langerhans) cells defending against microorganisms and superficial skin cancers
langerhans cells
specialized dendritic cell found in the stratum spinosum that functions as a macrophage
dendritic are apart of your immune system (guards); when something goes through they send the signals
stratum basale
the “basement layer”; innermost layer
deepest layer of the epidermis, made of epidermal stem cells
attached to the basement membrane
most cells here are basal cells
melanocytes and merkel cells are also found here
basal cell
type of stem cell found in the stratum basale and in the hair matrix that continually undergo cell division, producing the keratinocytes of the epidermis to replace more superficial keratinocytes
cuboidal-shaped stem cell that is a precursor of the keratinocytes of the epidermis
merkel cell
receptor cell in the stratum basale of the epidermis that responds to the sense of touch
dermis
layer of skin between epidermis and hypodermis, composed mainly of connective tissue and containing blood vessels, hair follicles, sweat glands, and other structures
supports the epidermis
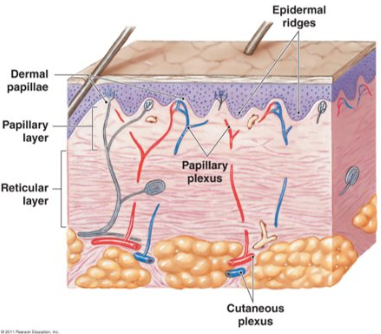
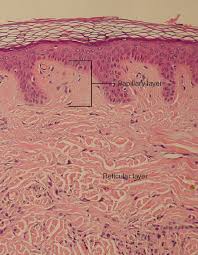
layers of dermis
papillary layer
reticular layer
hypodermis
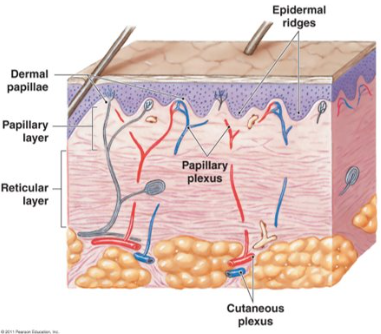
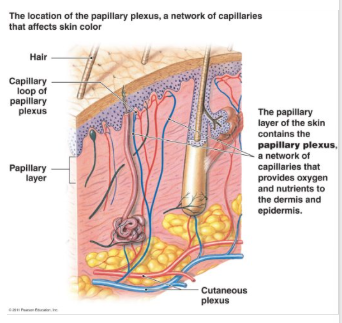
papillary layer
named for dermal papillae in this region
composed of loose areolar connective tissue
contains capillaries, lymphatic vessels, and sensory neurons
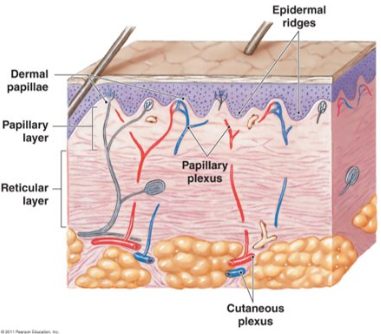
ridges of the skin
spatial relationship between epidermal ridges and dermal papillae
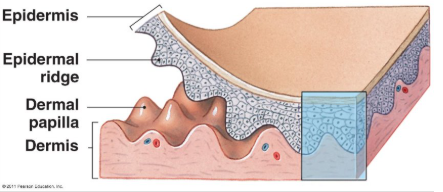
dermal papillae
extension of the papillary layer of the dermis that increases surface contact between the epidermis and dermis
dermal papillae are your fingerprints
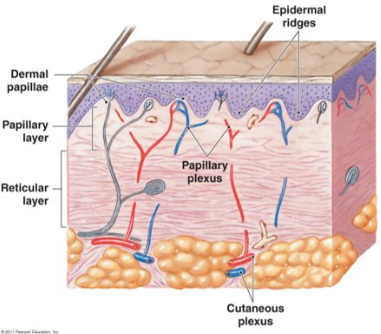
reticular layer
interwoven meshwork of dense irregular connective tissue
contains both collagen and elastic fibers
collagen fibers from this layer blend into both the papillary layer above and the hypodermis below
contains blood vessels, lymphatic vessels, nerve fibers, and accessory organs (hair follicles, sweat glands)
elastin fibers
fibers made of the protein elastin that increase the elasticity of the dermis
cleavage lines
correspond to the orientation of collagen fibers in the dermis, and are generally parallel to the orientation of the underlying muscle fibers
this is how the collagen fibers run; when surgeons cut you they want to follow this pattern because you’ll get less of a scar
hypodermis
separate skin from deeper structures (isn’t technically apart of your skin)
connective tissue connecting the integument to the underlying bone and muscle - connects the dermis to the rest of the body
stabilizes position of skin relative to underlying tissue
allows independent movement
provides insulation / padding
dominated by adipose tissue
important energy storage site
lost of fat in this area (fatty layer; to insulate, cushion, and attach)
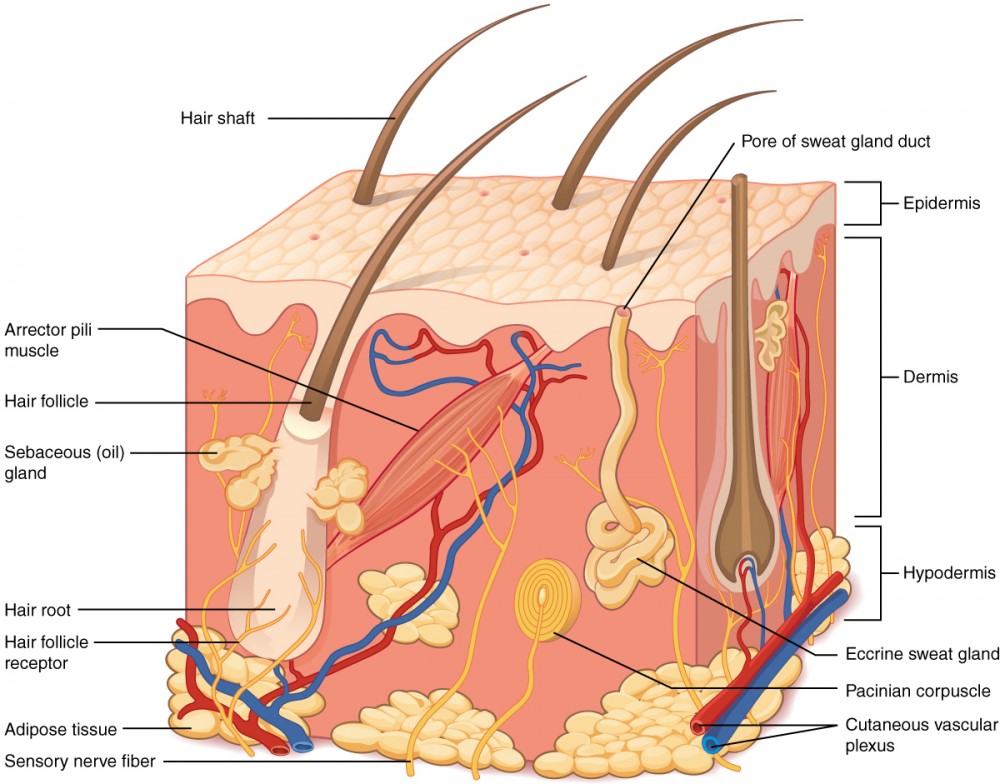
pigmentation
factors influencing skin color:
epidermal pigmentation via the amount of melanin and carotene
dermal circulation
melanocyte
cell found in the stratum basale of the epidermis that produces the pigment melanin
melanin
produced my melanocytes
pigment that determines the color of hair and skin
protects you from ultraviolet (UV) light
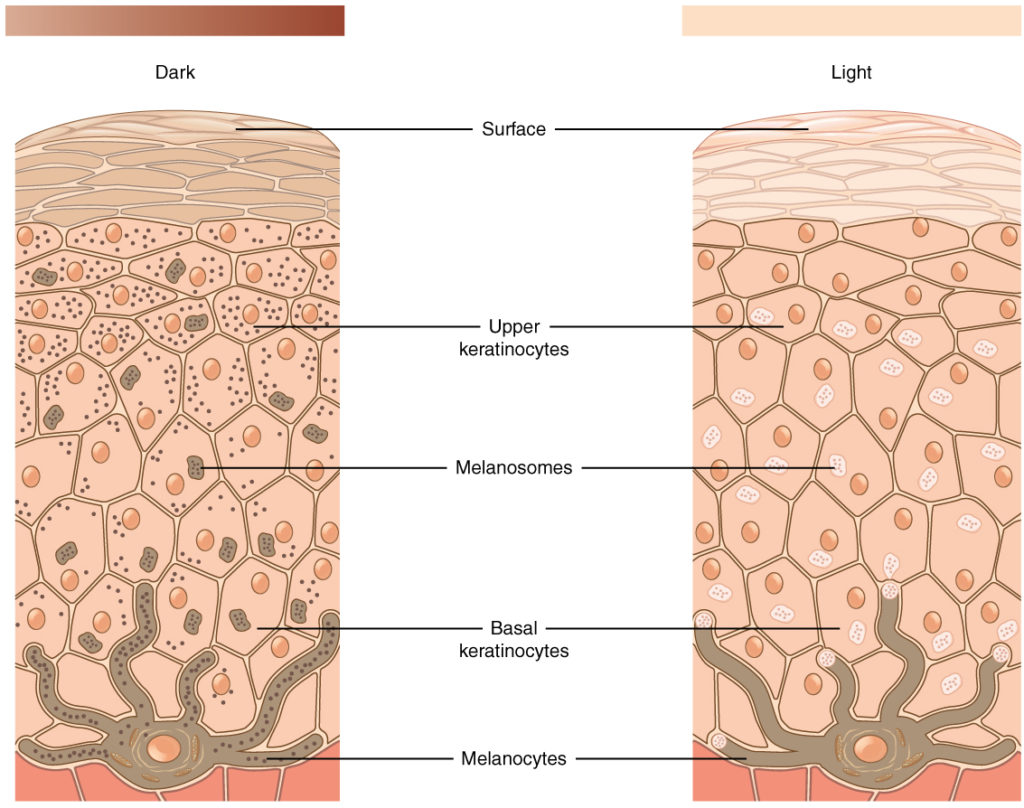
melanosome
intercellular vesicle that transfers melanin from melanocytes into keratinocytes of the epidermis
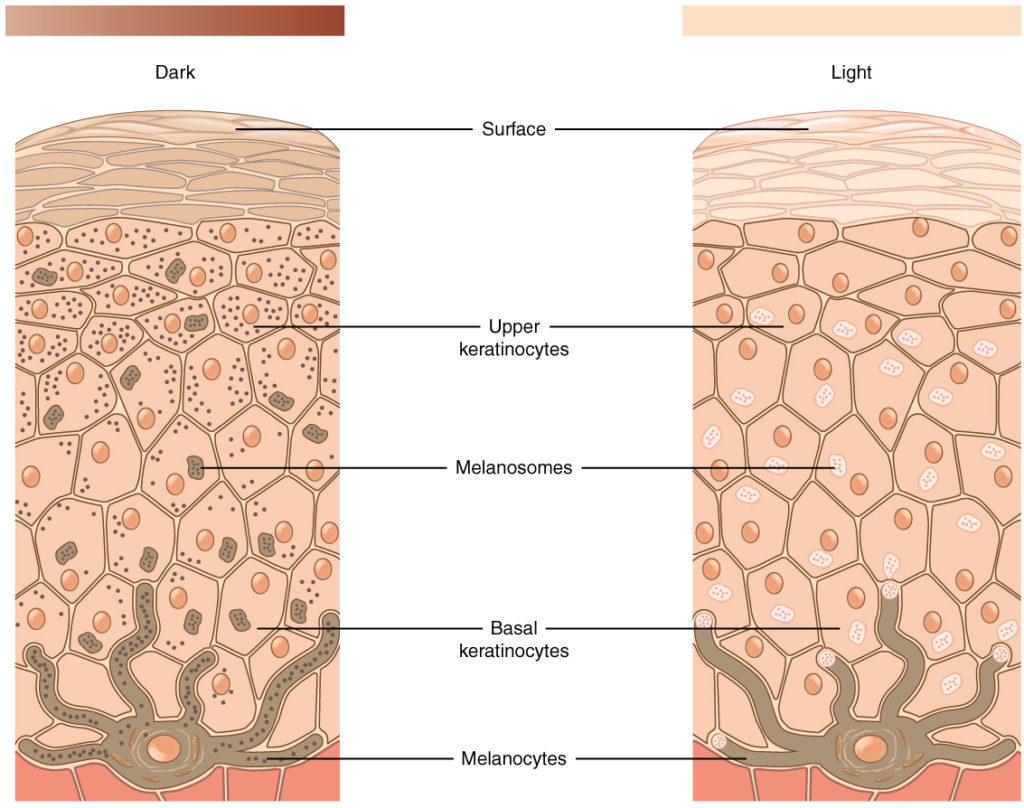
albinism
genetic disorder that affects the skin, in which there is no melanin production

vitiligo
skin condition in which melanocytes in certain areas lose the ability to produce melanin, possibly due to an autoimmune reaction that leads to loss of color in patches

dermal circulation
hemoglobin is red pigment found in red blood cells
blood flows to dermis through subpapillary plexus
more blood flow to region results in redder color
less blood flow to the region initially results in pale color
sustained reduction of blood flow decreases available oxygen
lower oxygen levels make hemoglobin darker red
from surface view, skin has bluish color (cyanosis)