CNS Imaging
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
What is the leptomeningeal layer?
The combination of the arachnoid and pia mater
This is where metastatic spread of cancers can occur
What are the imaging modalities used for CNS imaging?
- X-ray
- CT
- MRI
- Selective angiography/arteriography
- Ultrasound
- PET scan
What do we use x-rays for in CNS imaging?
Initial screening exam, mainly in outpatient settings (not done as much in inpatient)
Has multiple views but is less sensitive
What are the different types of CT scans we can do for CNS imaging?
- Without contrast (start with this for any kind of trauma)
- With contrast
- CT angiography
When do we use CT angiography in CNS imaging?
For SAH to see all of the different blood vessels in the brain
How do CSF spaces and CSF appear on CT?
Black (because it contains water)
Which is darker on CT: gray or white matter?
White matter
What is the initial study of choice for ALL neurologic issues?
CT of the head without contrast
What are the different non-pathologic calcifications we can see on CT scan of the head/brain?
- Calcified choroid plexus
- Pineal gland
- Falx and tentorium
- Basal ganglia
What is the imaging modality of choice for facial fractures?
CT of the facial bones without contrast
Favored over x-rays
What is the most common facial fracture?
Orbital blow out (usually due to direct blow to the orbit, orbital floor and medial wall fracture)
What are some hints to the presence of facial fractures that can be seen on CT?
- Orbital emphysema (air inside the orbit)
- Protrusion of fat/musculature outside of the orbit
- Fluid in sinuses (especially maxillary)
What are the different facial x-ray views?
- Waters view
- Caldwell view
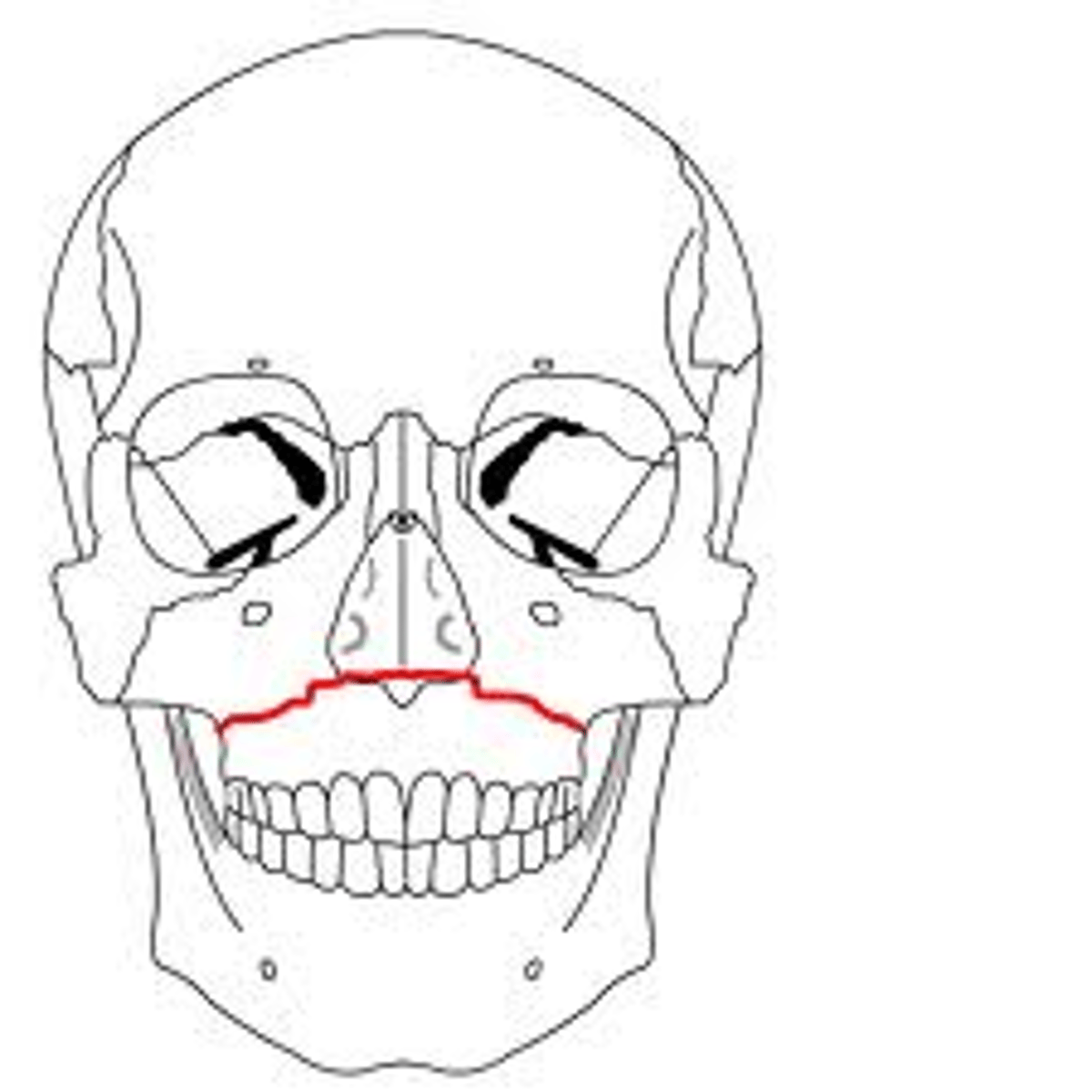
What is a Lefort type I fracture?
Fracture that proceeds through the maxillary bone, at the base of the nasal bones
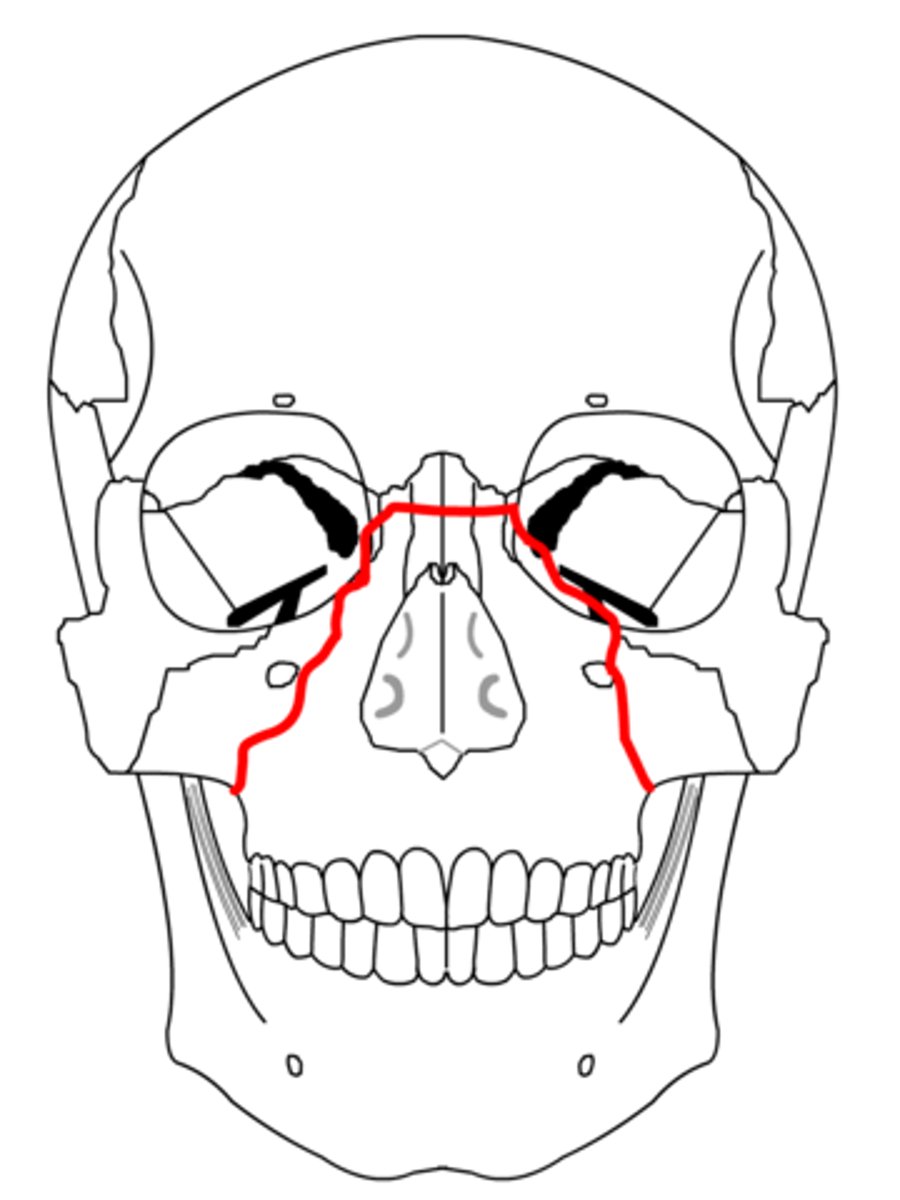
What is a Lefort type II fracture?
Fracture that extends up through the orbital floor, through the orbital wall and down the nasal bones
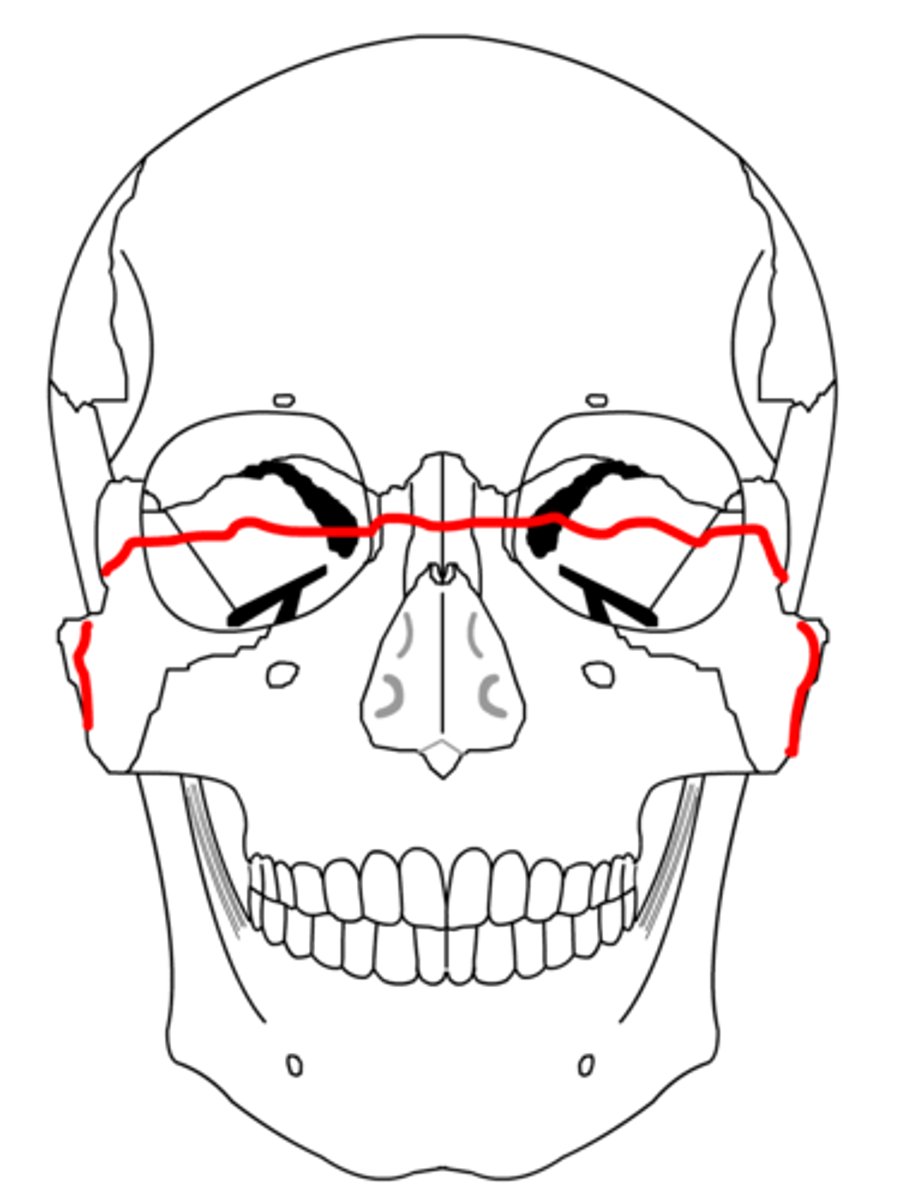
What is a Lefort type III fracture?
Midface fracture, fracture through the lateral and medial orbital wall, across the nasal bridge and all the way down to the other side
What are the 3 different types of skull fractures?
- Linear
- Depressed
- Basilar
What are 4 diagnostic clues on physical exam that point to a basilar skull fracture?
- Raccoon eyes (periorbital ecchymosis)
- Battle's sign (bruising over mastoid bone)
- CSF otorrhea
- CSF rhinorrhea
What are extra axial fluid collections? What are examples?
NON-intracerebral fluid (usually blood) collections
Examples include:
- Subdural hematoma (SDH)
- Epidural hematoma (EDH)
- Subarachnoid hemorrhage (SAH)
What does it mean if there is midline shift on a brain image?
Brain structures move away from a mass lesion (mass, bleed, abscess)
What does it mean if there is a mass effect on a brain image?
Compression and deformation of an area of the brain or internal structures due to a mass lesion (mass, bleed, abscess)
What are some features of epidural hemorrhages?
- Do NOT cross suture lines
- Follows outer layer of dura
- Can cross falx and tentorium
- Biconvex, lens shaped
What vascular structure is usually injured in epidural hemorrhages?
Middle meningeal artery
Epidural hemorrhages have a high association with what specific injury?
Skull fractures
What is the classic trimodal presentation of epidural hemorrhages?
- Initial LOC
- Awake and alert (intervening lucidity)
- Rapid decline of mental status within 6 hours of injury
What are some features of subdural hemorrhages?
- Follow inner layer of dura
- CAN cross suture lines
- Do NOT cross midline
- "Crescent-shaped" or concave
What vascular structure is most often injured in subdural hemorrhages?
Cortical bridging veins
How can we identify intracerebral hematomas on CT scan?
Highly attenuated, well-demarcated lesion often surrounded by a rim of hypoattenuation, indicative of cerebral edema
Where do intracerebral hematomas often occur?
Inferior frontal and temporal lobes
What is a diffuse axonal injury?
White matter shearing and axonal injury that is typically diagnosed via MRI
Where do diffuse axonal injuries usually occur?
- Cerebral hemisphere at grey/white matter junctions
- Corpus callosum
- Internal capsule
- Stem
What is the epidemiology of subarachnoid hemorrhages?
30-65 y/o, M > F
Primary subarachnoid hemorrhages are usually due to:
Aneurysmal or AVM ruptures
Where do primary SAHs usually occur?
- Circle of Willis (85%)
- Vertebro-basilar arterial system (14%)
- Cervical/thoracic arterial system (1%)
Secondary subarachnoid hemorrhages are usually due to:
HTN or trauma
What is the classic presentation of subarachnoid hemorrhages?
"Worst headache of your life", thunderclap headache
What is the imaging modality of choice for diagnosis of a subarachnoid hemorrhage?
CT of the head without contrast
Followed by CT angiogram with IV contrast (to identify vascular structure origin of SAH)
What are the two types of cerebral edema?
- Vasogenic
- Cytotoxic
What is vasogenic edema?
- Malignancy/infection associated
- Extracellular accumulation of fluids (SDH, EDH, etc.)
- Due to abnormal permeability of BBB
What is cytotoxic edema?
Cellular edema due to cell death due to ischemia
What are the different types of brain herniation?
- Subfalcine
- Transtentorial
- Tonsillar
- Central
- Uncal
- Brainstem
What is the initial imaging modality for a CVA?
Head CT/brain CT without contrast
What is a cerebrovascular accident (CVA)?
Episode of neurology dysfunction caused by brain, spinal cord, or retinal ischemia with evidence of infarction on imaging
Deficits last >24 hours
What is a transient ischemic attack (TIA)?
A transient episode of neurologic dysfunction caused by focal brain, spinal cord or retinal ischemia, without acute infarction
Deficits resolve typically in <1 hour
What are the different classifications of CVA?
- Thrombotic
- Embolic
- Hemorrhagic
What causes thrombotic CVAs?
Atherosclerosis
What causes embolic CVAs?
Most common sources include ICA, CCA bifurcation, and Afib
How can we identify embolic CVAs on CT scan?
Hyperdense MCA sign
What is hydrocephalus?
Dilation of the ventricles due to accumulation of excess CSF in the ventricular system
What are the two main types of hydrocephalus?
- Communicating
- Non-communicating
What is communicating hydrocephalus? How does it commonly present on CT scan?
NO obstruction to CSF flow
Classic CT head finding: dilatation of the 4th ventricle
What is non-communicating hydrocephalus?
Most common, typically due to some sort of mass
There is obstruction to normal CSF flow
How does normopressure hydrocephalus (NPH) present?
Hydrocephalus on CT head + urinary incontinence + gait disturbances
How does cerebral atrophy present on imaging?
- Cortical, especially temporal lobe atrophy
- Similar loss of gray AND white matter
- Ventricular dilatation due to loss of brain tissue
How does multiple sclerosis present on imaging?
Periventricular, corpus callosum lesions
What is the imaging study of choice to diagnose multiple sclerosis?
MRI
What is the initial imaging modality to assess for brain tumors?
CT brain with and without contrast, then MRI
What is the most common brain tumor in adults?
Glioma
How do brain tumors present on CT imaging?
Usually significant edema, mass effect, and enhances with contrast
How do metastatic brain lesions present on CT imaging?
- Usually multiple, well-defined, round lesions near grey white junction
- Hypodense or isodense on non-IV contrast CT of the head
What is a meningioma?
- Most common extraaxial mass
- Grows from the dura in towards the brain
- Can cause mass effect and midline shift
What is a Schwannoma?
- Acoustic neuroma
- Masses that can occur at theoretically all CN levels, but most commonly occur at the level of CN VIII
- Will present with unilateral hearing loss
What is the study of choice for Schwannomas?
MRI
What are the different anatomical parts of the vertebrae?
- Vertebral body
- Intervertebral disc
- Pedicle
- Transverse processes
- Superior and inferior articular processes
- Lamina
- Vertebral foramen
- Spinous process
What is the upward projection of C2?
Dens or odontoid process
What is the best way to view the odontoid/dens?
Open mouth PA view
What is the superior articular facet?
Articulating surface of the vertebral body that lines up with the inferior articular facet of the vertebral body ABOVE it
EX. superior articular facet of T2 articulates with the inferior articular facet of T1
What is the inferior articular facet?
Articulating surface of the vertebral body that lines up with the superior articular facet of the vertebral body BELOW it
What is the ligamentum flavum?
Strongest spinal column ligament that runs anterior to and posterior to the lamina
Protects the cord and nerve roots
What is the role of the anterior and posterior longitudinal ligaments?
Important in keeping the nucleus pulposus where it should be within the intervertebral space
What is unifacet dislocation?
One vertebral body subluxes (moves), but its movement is <25% of the width of the VB
What causes unifacet dislocation?
Flexion and rotation mechanism of injury
What is the imaging modality of choice for unifacet dislocation?
Lateral XR or sagittal CT
What is bilateral facet dislocation?
Superior vertebral body (in its entirety) subluxes over the inferior vertebral body by >50% of the width of the vertebral body
What causes bilateral facet dislocation?
Usually occurs due to injury/disruption to anterior longitudinal ligament and posterior longitudinal ligament
Which facet dislocation has more neurological deficits: unilateral or bilateral?
Bilateral
What is a Jefferson fracture?
Fracture of the anterior and posterior arches of C1
Usually bilateral, 4 possible fracture locations
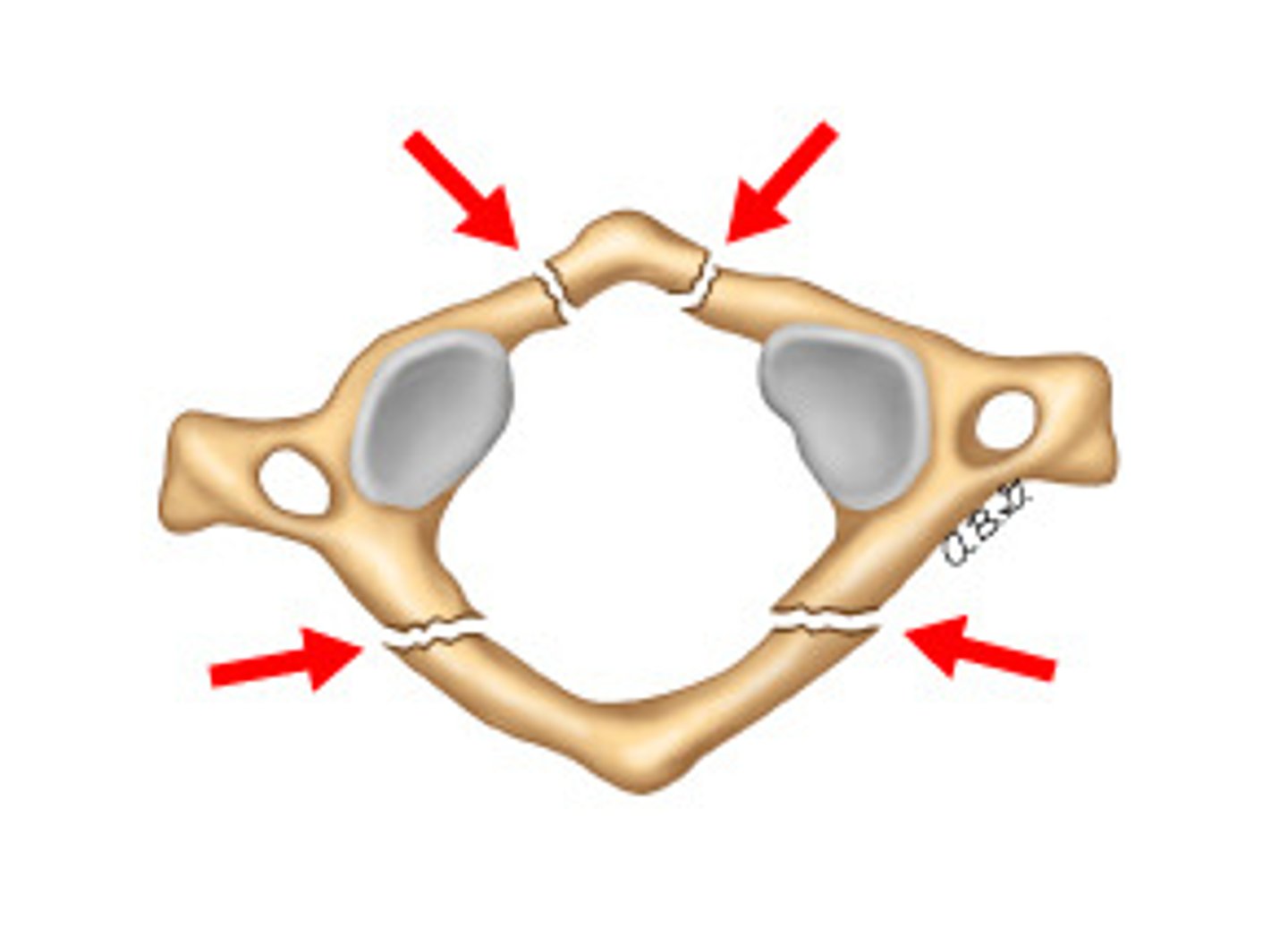
What causes a Jefferson fracture?
Axial load mechanism (something falling and hitting someone on the head)
What is the hallmark of a Jefferson fracture when viewed through an open mouth X-ray?
Lateral offset of C1 lateral masses
What is a Hangman's fracture?
Fracture of C2 where the posterior elements of C2 separate from anterior vertebral body
Vertebral body of C2 subluxes over C3 vertebral body

What causes a Hangman's fracture?
Hyperextension/compression mechanism
Which is more likely to have neurological deficits: Jefferson fracture or Hangman's fracture?
Jefferson fracture
What is a burst fracture?
Axial loading mechanism will cause the disc above the vertebral body to drive into the vertebral body below --> the vertebral body will rupture
What are the most common locations of a burst fracture?
- C-spine
- T-spine
- Upper L-spine
What are the different classifications of odontoid fractures?
- Type I: involves just the tip of the odontoid/dens, rare
- Type II: body of odontoid process, most common
- Type III: body of C2 involved
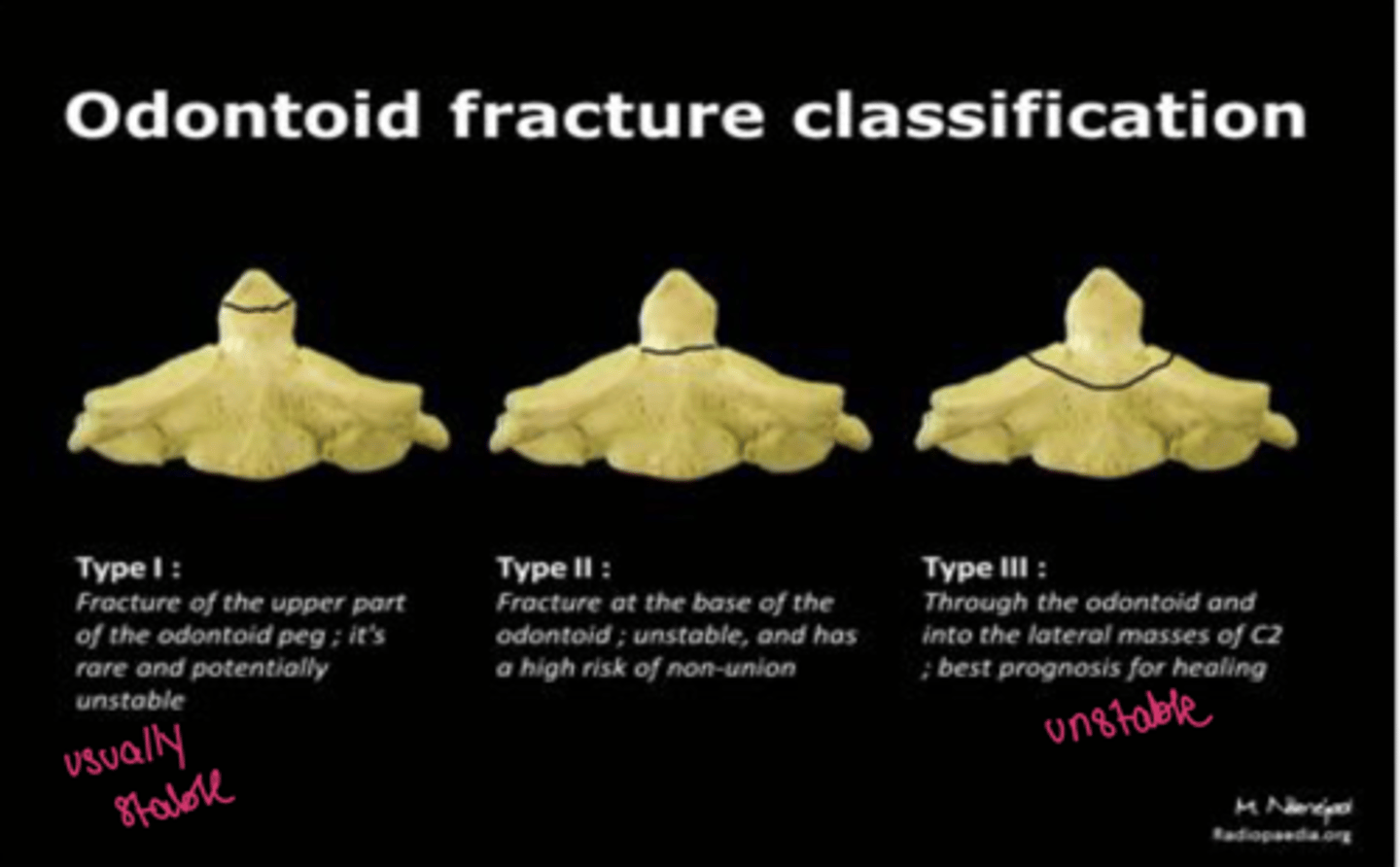
Which odontoid fracture is most common?
Type II
What is a clay shoveler's fracture?
Oblique fracture of the spinous process
Usually occurs in the lower C-spine (most commonly C6 or C7)
What causes a clay shoveler's fracture?
Hyperflexion mechanism
What is the most common location for bony mets?
Axial skeleton (spine, pelvis, skull, ribs)
What part of the vertebral body is more common to have metastatic disease and why?
Posterior vertebral body due to increased blood supply
Metastatic lesions of the bones can be either:
- Osteoblastic
- Osteolytic
What are the most common etiologies of back pain?
What are possible pathologic findings associated with back pain?
- Muscular/ligamentous strains
- Disc degeneration
- Arthritis of joints
- Compression fractures (osteoporosis)
What is the most common disc that is herniated?
L4-L5
What are symptoms of a lumbar herniated disc?
- Back pain
- Sciatica like symptoms (radicular pain, hyperesthesia)
What is the most common direction of disc herniation?
Posterolateral herniation
What is the imaging modality of choice for diagnosis of herniated discs?
MRI
What is degenerative disc disease?
Dehydration of nucleus pulposus causing the disc to flatten
Causes compression of the disc space (two vertebral bodies will start to rub on each other --> will produce osteophytes)
What is the initial imaging study of choice for degenerative disc disease?
X-rays
What are elements of diffuse idiopathic skeletal hyperostosis (DISH)?
- Thick, bridging calcifications between 4 consecutive vertebral bodies
- Usually lower thoracic or lower cervical spine
- Usually anterior
- Disc spaces/facet joints PRESERVED
- SI JOINTS ARE NORMAL