Oral histology EXAM 2
1/172
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
173 Terms
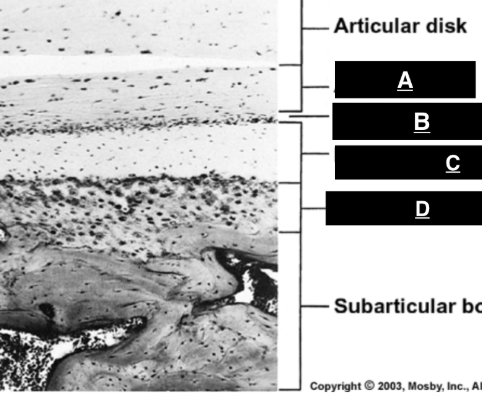
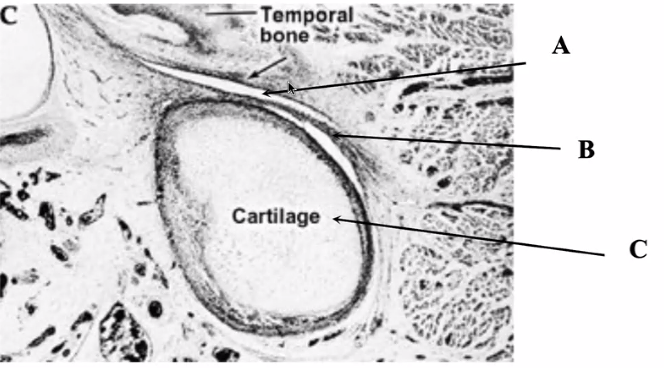
articular zone
identify A
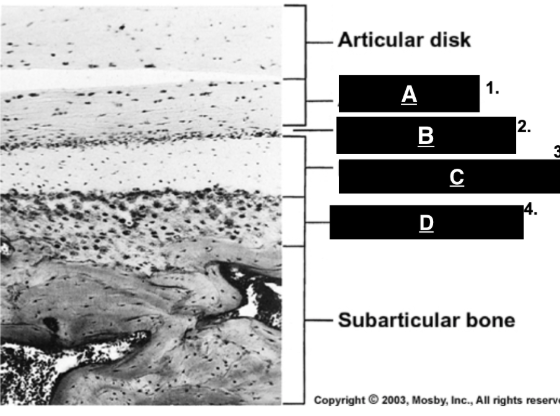
proliferative zone
identify B
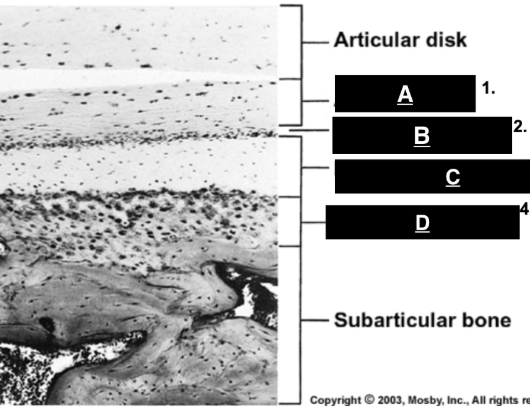
fibrocartilaginous zone
identify C
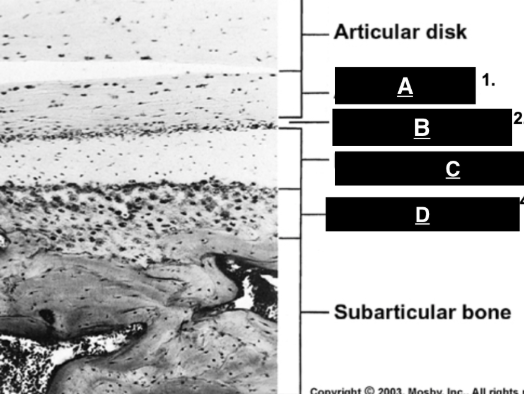
calcified cartilage
identify D
capsule
surrounds joint, attaches to neck of condyle and temp bone
synovial membrane
lines inner part of capsule (not disc and articular surface)
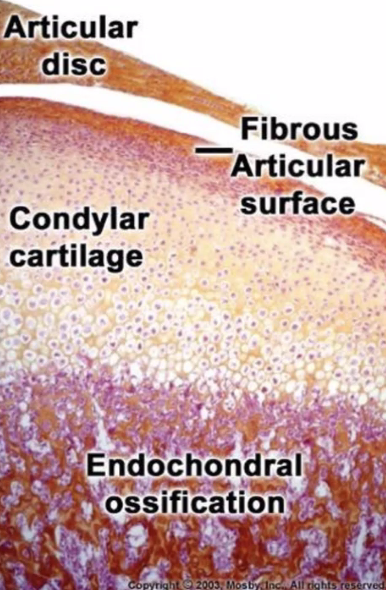
articular disc
fibrocartilaginous structure continuous with capsule that separates the joint cavity and improves fit of bones.
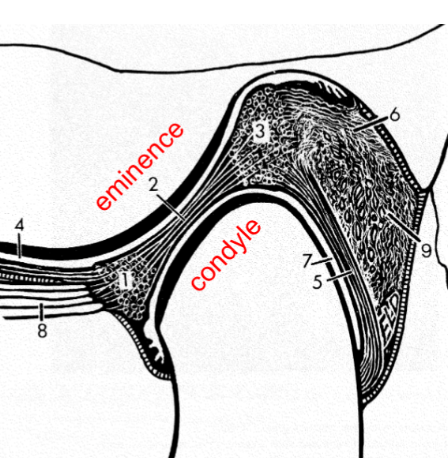
superior joint cavity
what is 4
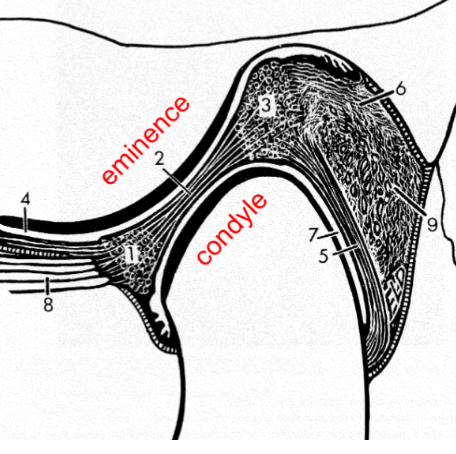
inferior lamina
what is 5
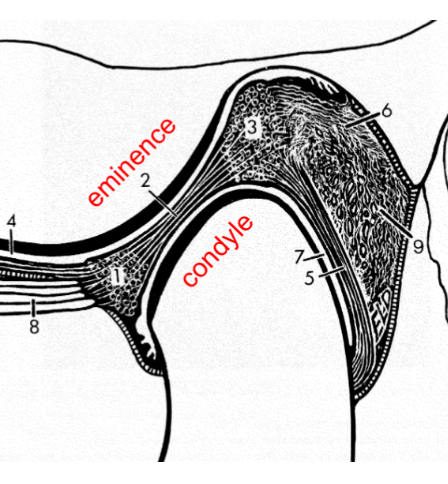
superior lamina
identify 6
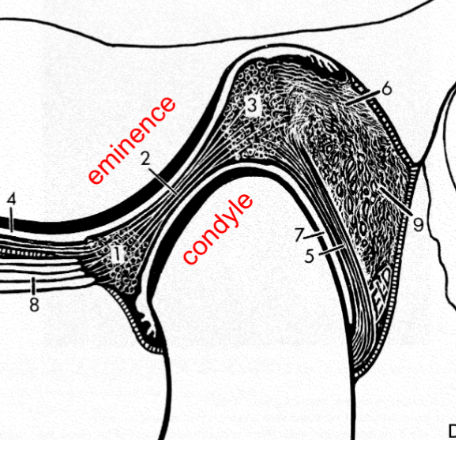
inferior joint cavity
identify 7
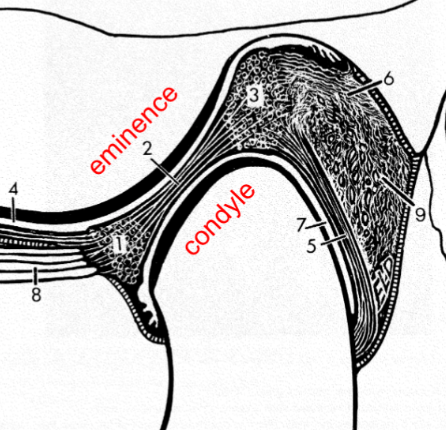
lateral pterygoid
what is 8
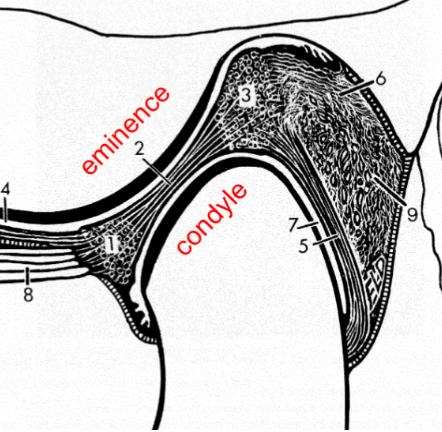
retrodiscal pad
identify 9
free, ruffini’s, pacini’s, golgi
four types of nerve endings in TMJ
free nerve ending
what is the major type of nerve ending in the TMJ
free nerve ending
nociceptor (pain) in the TMJ
ruffini’s corpuscle
nerve ending in TMJ functioning in dynamic PROPRIOception
pacini’s corpuscle
nerve ending in TMJ functioning in dynamic MECHNOreception
golgi tendon organ
proprioceptor near MYOTENDINOUS junction that senses changes in MUSCLE TENSION
fibrocartilage
what is the TMJ disc made of
fibrochondrocytes
cells found in TMJ disc that produce and maintain fibrous and cartilaginous matrix.
fibrous connective tissue (type 1 collagen) and GAGs
components of TMJ disc extracellular matrix
avascular and lacks innervation
Characterizes the TMJ disc which affects its healing capacity
where disc meets capsule
where is the nerve and blood supply of the TMJ
mediolateral
direction of fiber in ANTERIOR and POSTERIOR bands
anteroposterior
direction of fiber in INTERMEDIATE band
articular disc
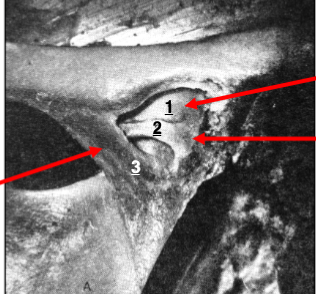
identify 1
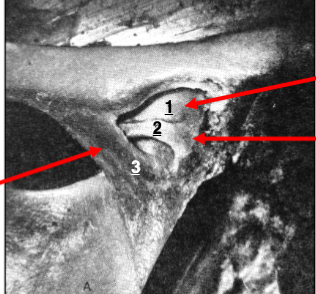
horizontal ligament
identify 2
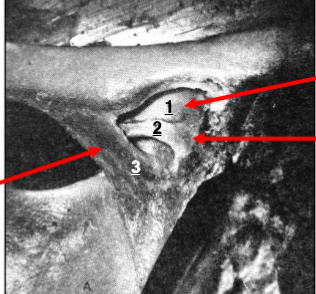
oblique ligament
identify 3
auriculotemporal, masseteric, deep temporal (all CN V3)
what nerves innervate the TMJ
AP direction of collagen fibers
why is the TMJ disc stronger in AP direction
forms primitive jaw (malleus)
what happens to the meckel’s cartilage
intramembranous
what type of ossification forms the mandible
condensation stage
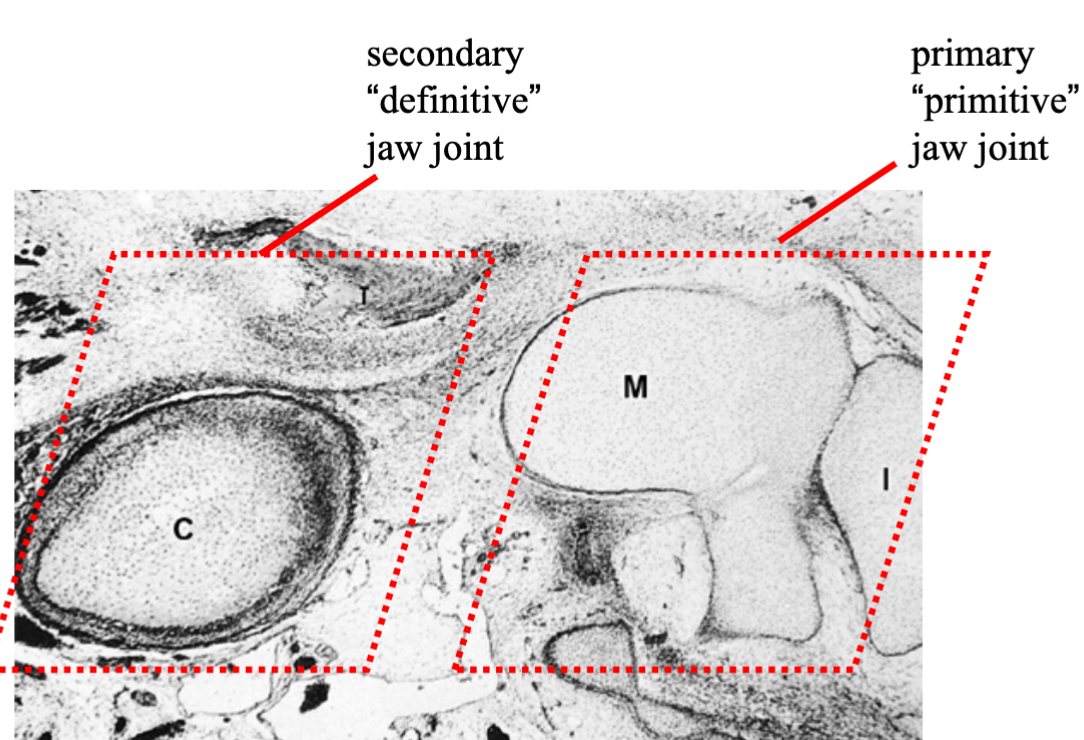
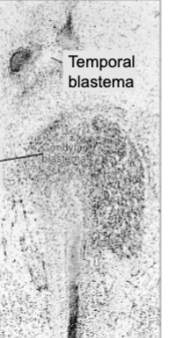
stage of TMJ formation where mesenchyme forms condylar blastema that grows towards temporal blastema
temporal blastema
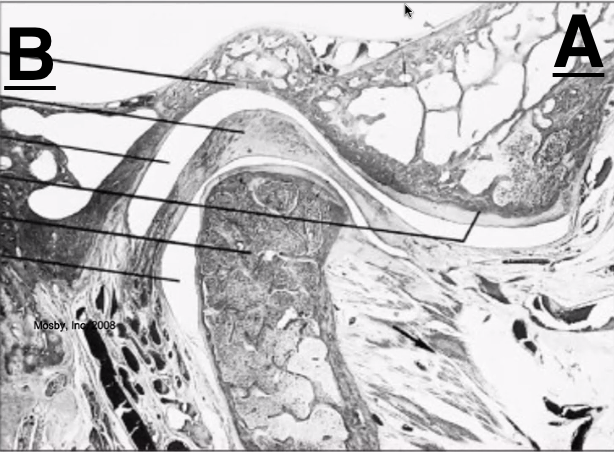
what is A
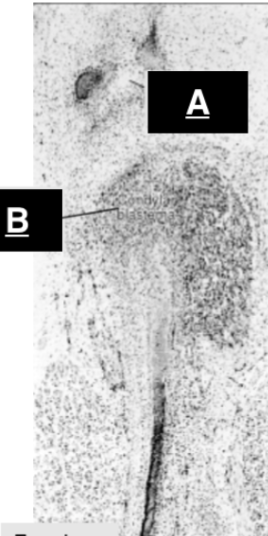
condylar blastema
what is B
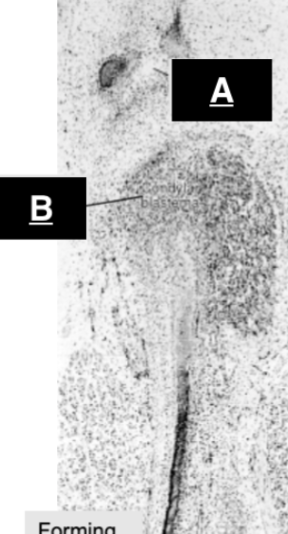
cavitation stage
stage of TMJ formation where clefts form in the condylar and temporal blastema, leading to the development of joint spaces.
inferior joint cavity
forms from cleft ABOVE condylar blastema
superior joint cavity
forms from cleft BELOW temporal blastema
TMJ disc
what does the tissue between the two clefts in the cavitation stage form?
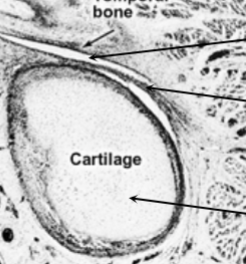
cavitation stage
when does the condylar blastema become cartilage
condensation
what stage is this?
cavitation
what stage is this?
maturation stage
what stage is this?
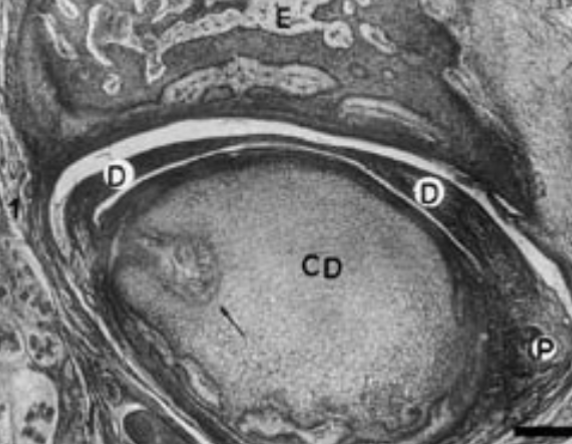
maturation stage
stage of TMJ formation where tissues attain mature morphology
temporal condensation
forms in optic capsule of cranial base
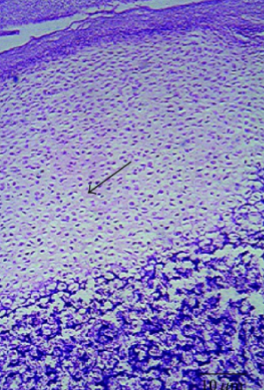
fibrous tissue
what covers the joint surface of the TMJ?
multidirectional
what is the directional growth potential of the TMJ
mandibular condyle
major site of mandibular growth
long bone (unidirectional growth)
where can this type of bone be found?

cartilage decreases in thickness
what happens to the condylar surface as we age?
condyle (multidirectional growth)
where can this type of bone be found
colateral ligaments
what binds the disc to the condyle
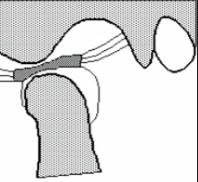
rotation
what type of movement occurs between the DISC and the CONDYLE (inferior cavity)
sliding/translation
what type of rotation occurs between the DISC and MANDIBULAR FOSSA
posterior
which way does the disc move during opening ROTATION
passive opening
what position is this TMJ in
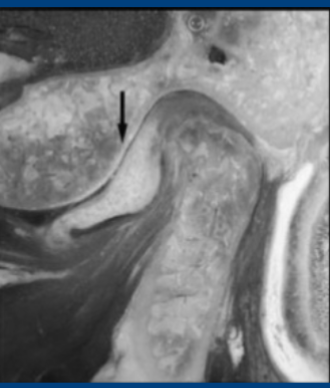
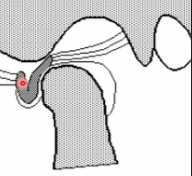
anterior disc displacement
what is the ISSUE indicatacted by the arrow
temporal blastema
where does structure A come from
fibrocartilage
what is the fibrous material on the surface of the TMJ
meckels cartilage, articular cartilage, condylar condensation, condylar cartilage
what is the series of cartilage formation for condylar cartilage
meckels cartilage
stimulates condylar condensation
condylar cartilage
which secondary cartilage is incorporated into the mandible
A
which direction (A or B) is anterior
down and anterior
which DIRECTION will the mandibular CONDYLE move as the jaw OPENS
down and anterior
which DIRECTION will articular DISC move as the jaw OPENS
clicking
what happens if the disc moves more than condyle during opening
type I collagen
helps disc resist tensile loading
nothing, forms primitive jaw
what does meckels cartilage contribute to OSSEOUS development of TMJ
posterior temporalis and deep masseter
which muscles RETRACT/RETRUDE the condyle during jaw closing
motor end plate
Each muscle FIBER has ONLY ONE of these neuromuscular junctions that transmit signals from motor neurons to muscle fibers.
auriculotemporal
provides SENSORY information from area of mandibular condyle
large variety of motor tasks
why are muscles of mastication so different from skeletal muscles
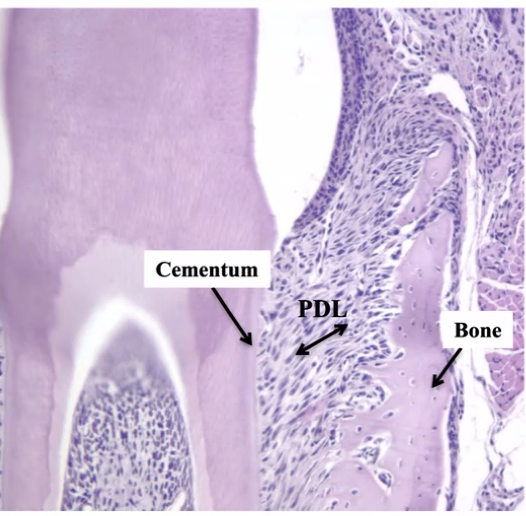
PDL
collagen fibers. between TOOTH ROOT and ALVEOLAR bone
sharpey’s fibers
PDL collagen fibers embedded in ROOT CEMENTUM and ALVEOLAR BONE
coronal 2/3
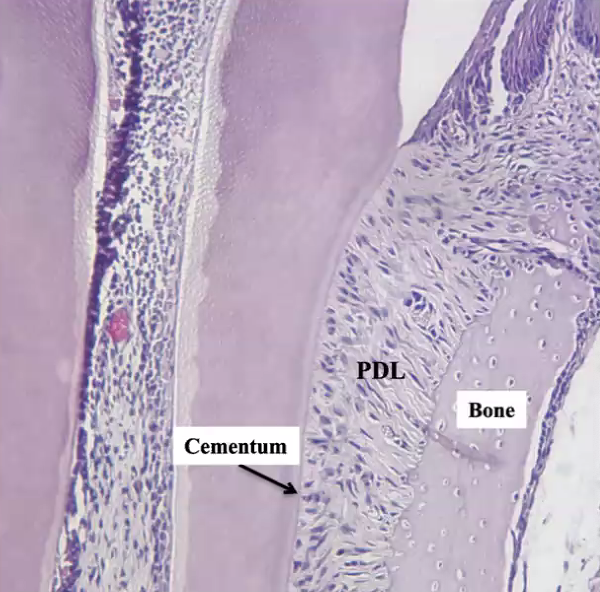
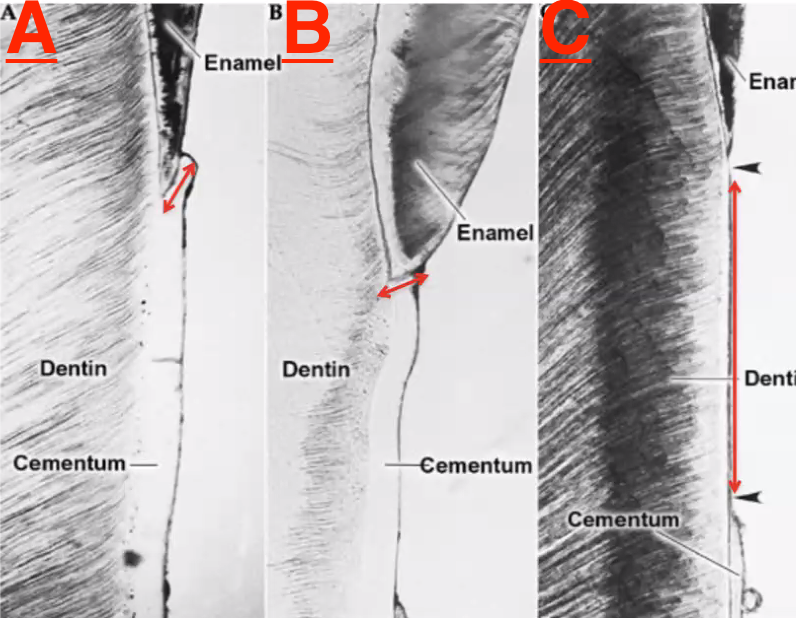
where does ACELLULAR cementum occur
apical 1/3
where does CELLULAR cementum occur
cementum(cementoblasts), PDL (fibroblasts), and alveolar bone (osteoblasts)
what does the dental follicle gives rise to
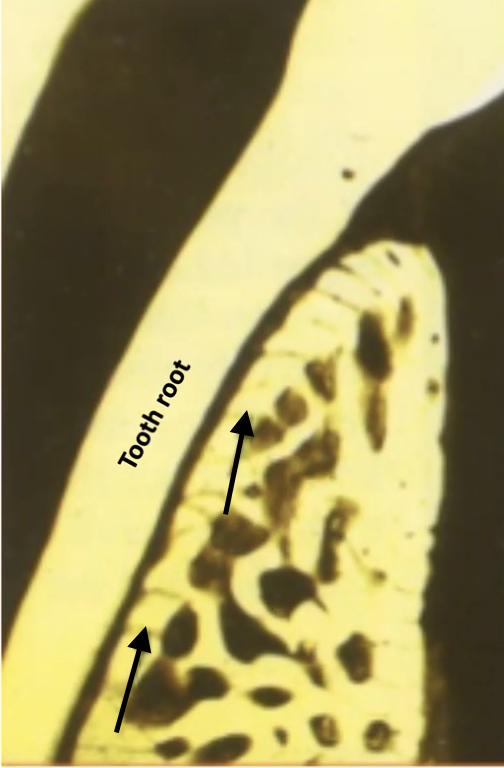
oblique
how would you categorize thee PDL fiber indicated by the double headed arrow?
acellular
what kind of cementum would be in the area indicated
cribriform plate/alveolar bone proper
what bone is indicated by the arrows
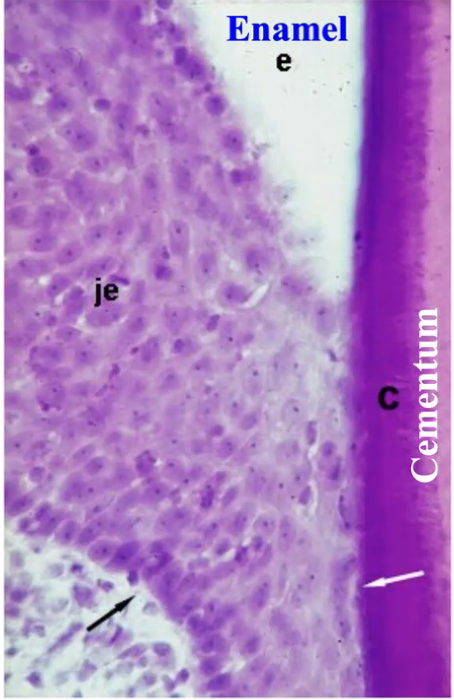
acellular afibrillar
which kind of cementum forms at the CEJ
A (overlap)
which of these conditions is the most common form of acellular afribrillar cementum
acellular cementum
which cementum occurs FIRST (primary)
reduced enamel epithelium
forms junctional epithelium
acellular afibrillar
what type of cementum is here
cellular
which cementum forms in POST-FUNCTIONAL stage of tooth eruption
cellular cementum
thicker cementum with CEMENTOCYTES embedded
acellular
which cementum has mostly EXTRINSIC FIBERS
cellular
which cementum has mostly INTRINSIC FIBERS
acellular (primary)
which cementum functions in ATTACHMENT
cellular
which cementum functions in MAITAINING TOOTH POSITION
anterior displacement with reduction
disc displaced and RETURNS to normal position when jaw opens
anterior displacement without reduction
disc is displaced and STAYS displaced
lateral pterygoid
muscle that functions in PROTRUSION
masseter, temporalis, medial pterygoid
muscles that function in ELEVATION/CLOSING
suprahyoid, infrahyoid, lateral pterygoid
muscles that function in DEPRESSION/OPENING
muscle fascicle
individually wrapped in PERIMYSIUM, vessels and nerves travel in between
muscle fiber
long thin multinucleated post-mitotic cells individually wrapped in ENDOMYSIUM
sarcomere
contractile unit of muscle