NPB101: Digestive Tract
1/75
Earn XP
Description and Tags
Hamada lectures 42-45 SP2025
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
Where does the digestive tract begin and end
From the mouth to anus
Carbohydrate Digestion Order
Starts in the mouth, pauses in the stomach, and continues and finishes in the small intestine. Large intestine does not significantly digest carbs
What are the 4 major tissue layers of the digestive tract? (inner to outer)
Mucosa
Submucosa
Muscularis Externa (smooth muscle)
Serosa
Also includes lumen and enteric nervous system (not tissues)
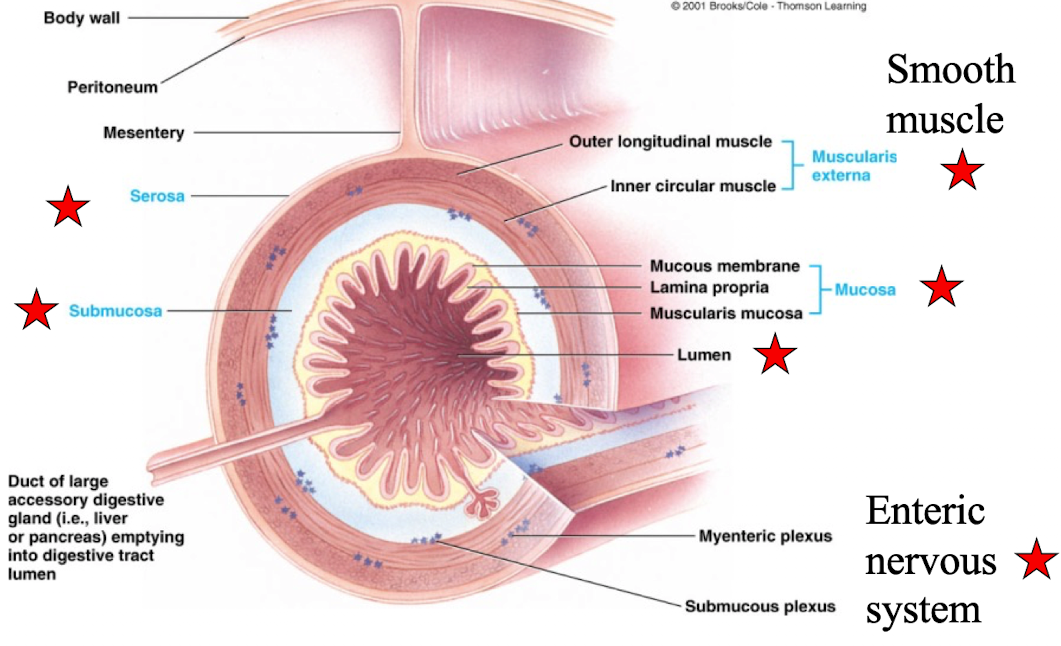
Mucosa
innermost layer of the GI tract; specialized for secretion and absorption and contains epithelial cells
Muscularis externa
Responsible for motility (peristalsis and segmentation)
Serosa
Outermost layer; primilary provides structural support and protection
What is significant about the digestive lumen’s relationship to the external environment?
It is continuous with the external environment.
It is exposed to:
pH changes
Harsh enzymes
Microorganisms
What are the 4 basic digestive processes?
Motility
Secretion
Digestion
Absorption
Motility
Propulsive:
Move contents forward through the digestive tract
Mixing movements:
aid digestion by mixing food with digestive juices
facilitate absorption by exposing food to absorbing surfaces
Secretion
Digestive juices into the lumen by exocrine glands
Digestion
biochemical breakdown of food
Absorption
Primarily in the small intestine; transfer of small absorbable units along water, vitamins, electrolytes from the digestive lumen into the blood or lymph
What anatomical structures are involved in the mouth and salivary gland function?
Lip & Tongue: contain food in mouth; guide food during chewing and swallowing
Teeth: begin mechanical breakdown by chewing of food
Palate: roof of oral cavity that separates oral cavity from nasal passage, allows chewing and breathing to occur simultaneously
Uvula: soft tissue that hands from the rear of the mouth and seals off nasal passage during swallowing
Cephalic Phase Response (CPR)
Important to prepare food digestion and nutrient absorption efficiently
Crucial for energy homeostasis and metabolism
What are the effects of no CPR?
Nutrient absorption delay
Slow-digesting speed
longer digestion period
Secrete saliva in response to ____ stimulation
autonomic
What does saliva contain?
mucus moisten food and lubricate
beings digestion of carbohydrate
lysozymes lyse bacteria (antibacterial effect/oral hygiene)
Bicarbonate buffer neutralize acids
Amylase (begins chemical digestion of carbohydrates)
Helps facilitate speech
What are the types of salivary secretion reflexes?
Simple reflex: Pressure receptors and chemoreceptors
Conditional reflex (cephalic phase response): Comes from cerebral reflex when thinking about food/eating food
What is the function of the pharynx in digestion?
Located at the rear of the mouth
A common passageway for both digestive and respiratory systems
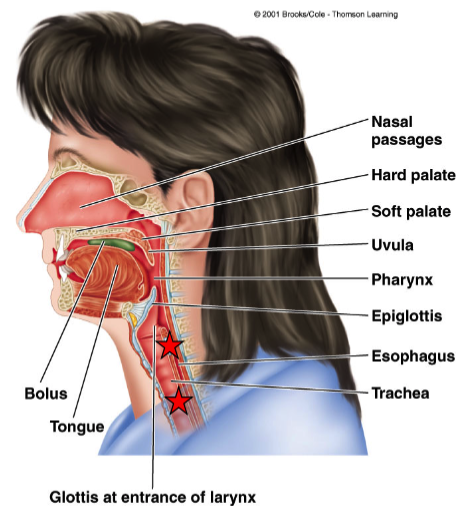
What is the esophagus and what does it connect?
A muscular tube connecting the pharynx and stomach
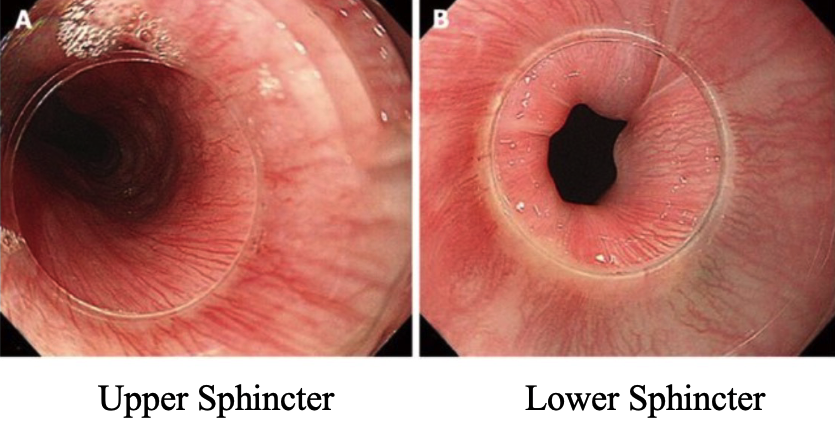
What are the two sphincters of the esophagus and their functions?
Upper sphincter (pharyngoesophageal): normally closed to prevent air entering the esophagus
Lower sphincter (gastroesophageal): normally closed to prevent acid reflux from the stomach
What is swallowing and how is it controlled?
An all-or-none reflex
Triggered by pressure of bolus in pharynx → activates pressure receptors → sends signal to swallowing center in the medulla (brain stem)
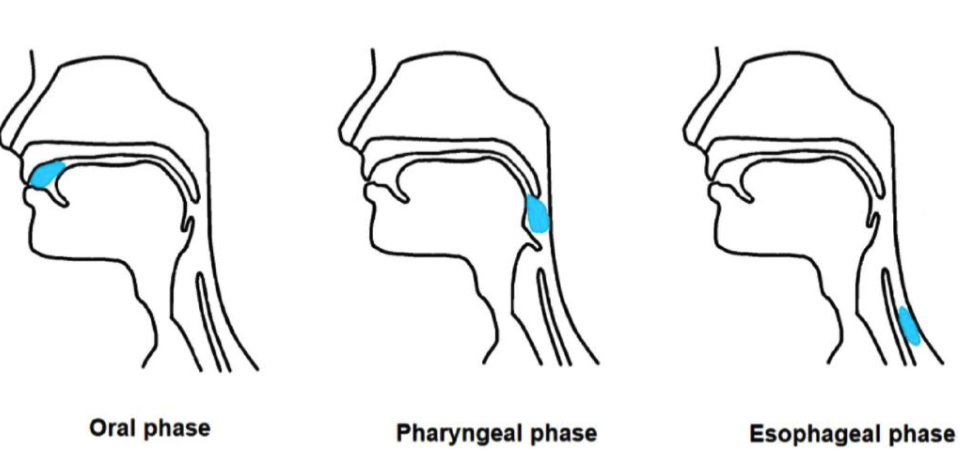
What are the stages of swallowing?
Oropharyngeal stage
Moving bolus from mouth through pharynx into esophagus
Esophageal stage
involves propulsive movements
peristaltic wave moves bolus through esophagus and into stomach
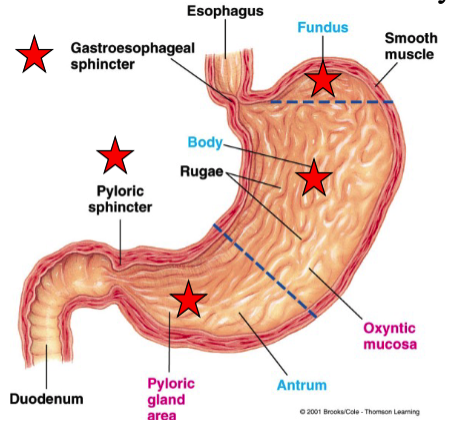
What are the main regions of the stomach and their features?
Fundus: above gastroesophageal sphincter
Body: middle portion
Antrum: bottom portion; thick smooth muscle; connects to small intestine via pyloric sphincter
What are the primary functions of the stomach?
Store ingested food and deliver it to small intestine at proper rate
Secrete HCl and enzymes to start protein digestion
Produce chyme: a thick liquid of food + gastric secretions
What region of the stomach contains oxyntic mucosa, and what structures does it include?
Lines the body and fundus
Located in gastric pits lining the mucosal wall
What are the functions of mucus in the stomach?
protect the stomach lining from acid and enzymes
lubricates food and protects mucosal surfaces
What are the 4 types of cells associated with gastric pits?
Mucous neck cells (secrete thin, watery mucus)
Chief cells (secrete pepsinogen - precursor of pepsin)
Parietal (oxyntic) cells (secrete HCl, intrinsic factor)
Surface epithelial cells (secrete thick, alkaline mucus)
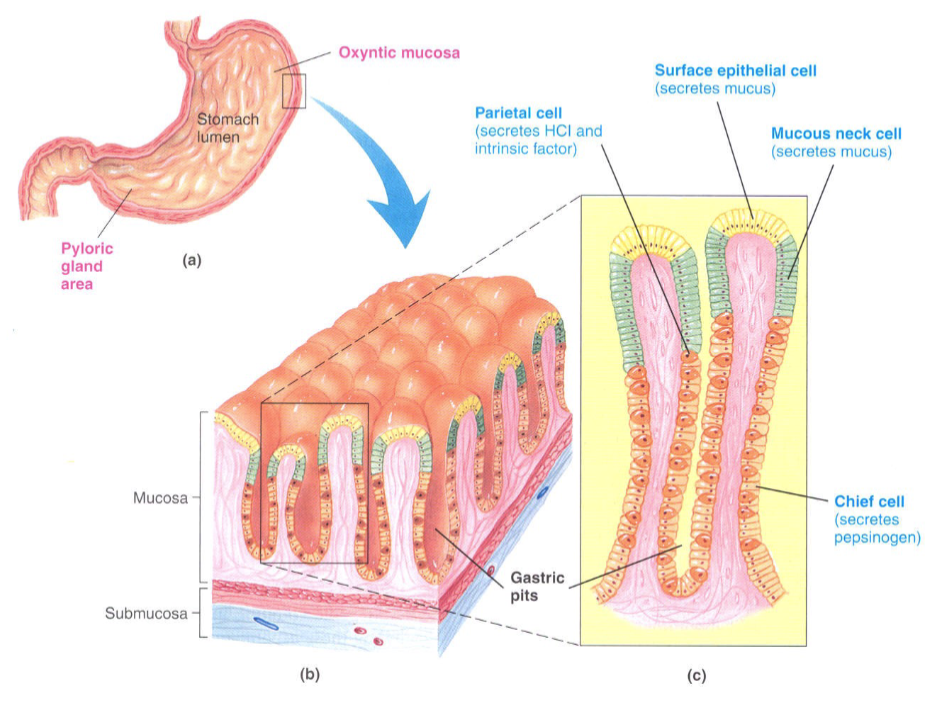
What do chief cells secrete, and what is the role of it?
Secrete pepsinogen (inactive)
inactivated form prevents damage to stomach lining
Pepsinogen is cleaved by HCl to form pepsin
Pepsin:
Activates more pepsinogen (autocatalytic)
Begins protein digestion by splitting amino acid linkages
Works best in acidic environment
What do parietal (oxyntic) cells of the gastric mucosa secrete?
H+ and Cl- (intrinsic factors) are actively secreted by separate pumps HCl-:
Activates pepsinogen
Aids breakdown of connective tissue
Kills ingested microorganisms
What are parietal (oxyntic) cells of the gastric mucosa intrinsic factor?
Needed for vitamin B12 absorption
B12 is essential for normal RBC function
What do mucous neck cells and surface epithelial cells secrete?
Mucous neck cells: secrete thin, watery mucus
Surface epithelial cells: secrete thick, alkaline mucus
What do mucous neck cells and surface epithelial cells do?
Protects against mechanical injury
Prevents self-digestion
Shields against acid injury
What secretions are produced in the pyloric gland area (antrum)?
Mucus
Pepsinogen
Gastrin (hormone)
Describe how gastric mixing and emptying works
Strong antral peristaltic contractions
mix food with gastric secretions to produce chyme
propel chyme towards pyloric sphincter where small amount is pushed into the duodenum
upon reaching the pyloric sphincter, cause the sphincter to close and the remaining chyme is tumbled back into the antrum
strength can vary depending on a number of factors
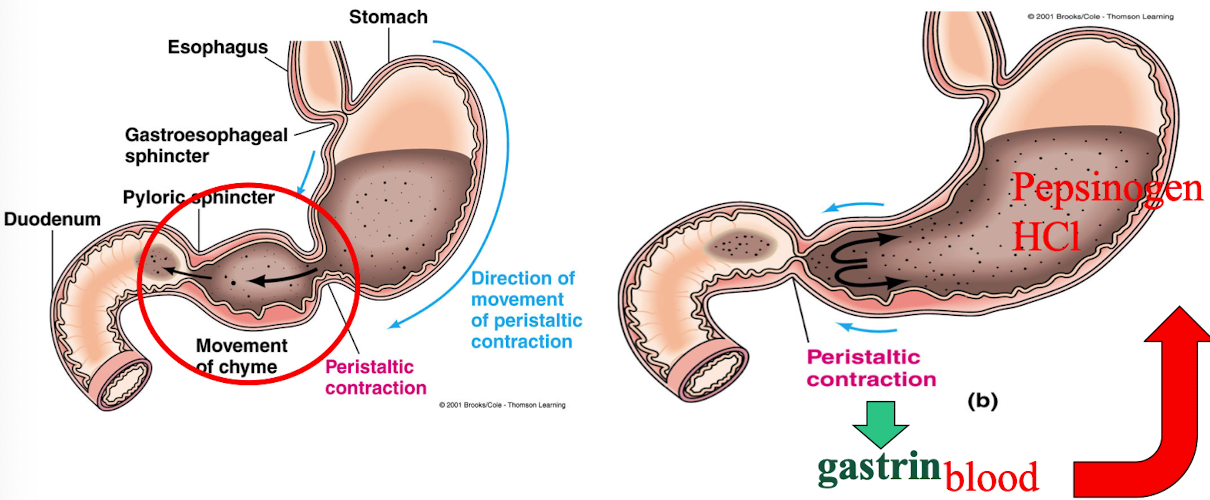
What hormone stimulates gastric mixing and secretions?
Gastrin → stimulates parietal and chief cells to produce HCl and pepsinogen
What factors control gastric mixing and emptying? Stomach
Volume of chyme
Fluidity of chyme
What factors control gastric mixing and emptying? Duodenum
The presence of any of these would inhibit It until the duodenum has coped with factors already present. Chyme inhibits. Gastrin promotes
Fat
Acid
Hypertonicity
Distention
What is the primary site of digestion and absorption?
Small intestine
No digestion occurs after the small intestine
What is segmentation in the small intestine?
Type of oscillating, ringlike contraction (not peristaltic wave)
Mixes and propels chyme
absent btwn meals but vigorous during and after a meal
Chyme moves forward because contraction frequency gradient gradually decreases along the intestine
What enzymes aid digestion in the small intestine?
lumen is accomplished by pancreatic enzymes
Bile secretions enhance fat digestion
Pancreas and Liver Secretions
Provide secretions that mix with the contents of the duodenal lumen
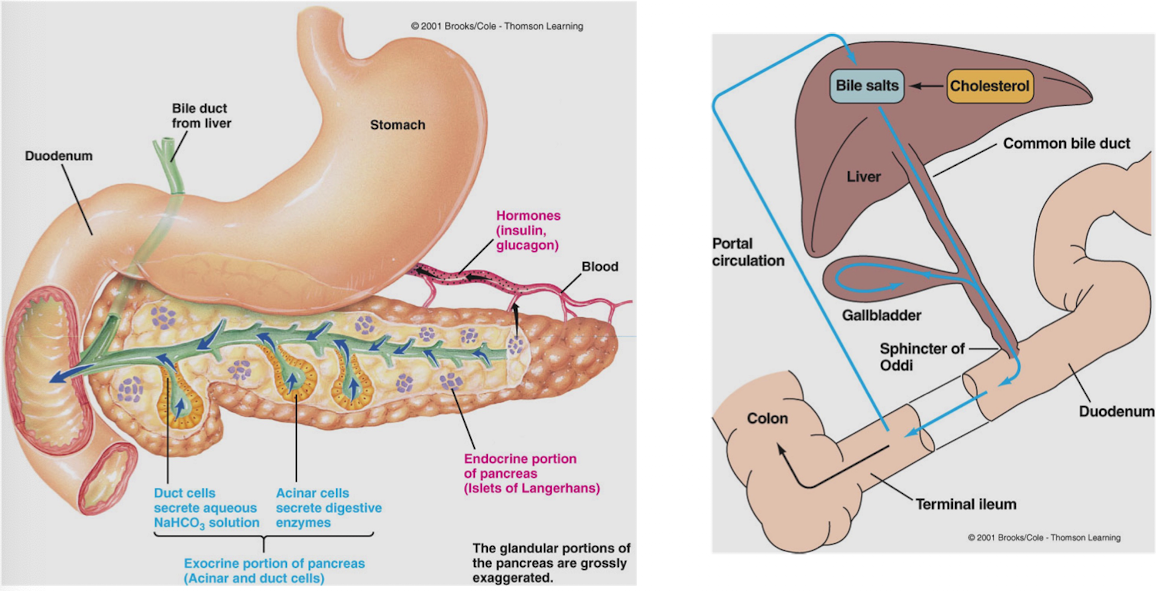
What does the exocrine pancreas secrete and which cells are involved? Duodenum
Acinar cells: release 3 types of enzymes
Proteolytic enzymes (trypsinogen)
Activated by enterokinase in the duodenum → becomes trypsin (active form)
Trypsin autocatalyzes more trypsinogen
Trypsin inhibitor prevents premature activation
Pancreatic amylase (carbohydrate digestion)
Pancreatic lipase (fats) → only fat-digesting enzyme in GI tract
Duct cells: release sodium bicarbonate (NaHCO₃) to create alkaline environment
Chyme in the duodenum triggers the release of what 2 major enterogastrones?
Secretin: released in response to acidic chyme
Cholecystokinin (CCK): triggered by fat and protein in chyme
All 3 enzymes (proteolytic, amylase, lipase) are packaged into common vesicles → fat/protein triggers release of all 3
Carbohydrates do not trigger enzyme release
What are the major components and functions associated with bile?
Bile salts: aid digestion and absorption of fats in the duodenum
Gallbladder: stores bile
Sphincter of Oddi: controls bile entry into duodenum
Bile salts are recycled
What anatomical regions are bypassed in Roux-en-Y gastric bypass surgery?
Antrum
Duodenum
Reduces absorption of nutrients and caloric intake that is mostly done within small stomach (esp within duodenem)
What does bile act on?
Fat in the duodenum
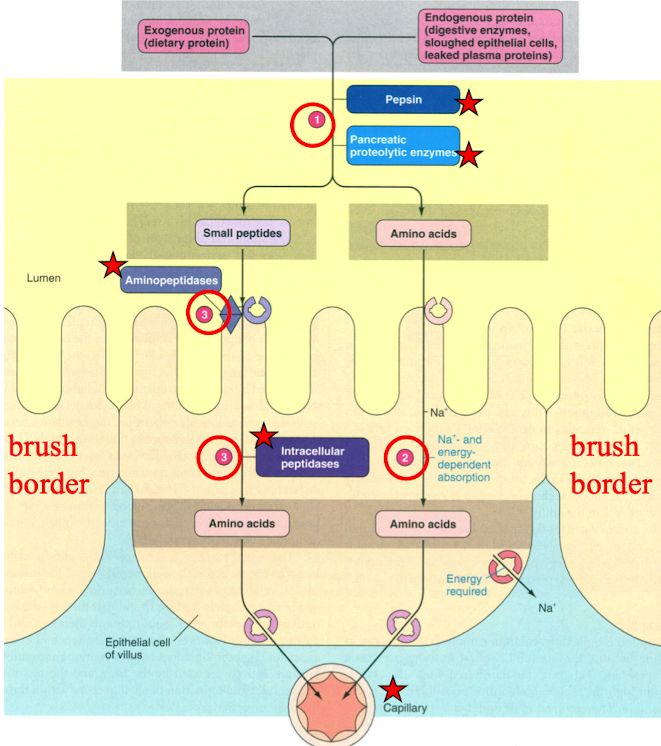
What is the brush border and what enzymes does it contain?
microvilli on intestinal epithelial cells
Contains 3 enzymes:
Enterokinase
Disaccharidases
Aminopeptidases
Brush Border: Enterokinase
activates pancreatic enzyme trypsinogen
Brush Border: Disaccharides
maltase, sucrase, lactase
complete digestion of carbohydrates
Brush Border: Aminopeptidases
Complete digestion of proteins by hydrolyzing most of the small peptide fragments into their amino acid components
Where is digestion of different macromolecules completed?
Fat digestion: completed extracellularly
Protein and carbohydrate digestion: completed intracellularly
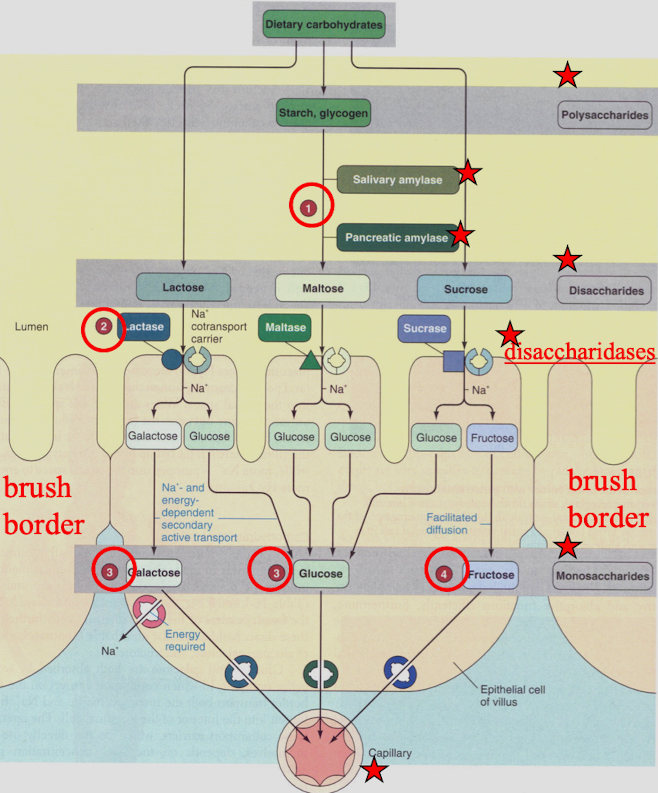
How are carbohydrates digested and absorbed?
In lumen:
Polysaccharides → disaccharides (via salivary and pancreatic amylase)
At brush border:
Disaccharides → monosaccharides
Absorption: Monosaccharides → capillaries (blood)
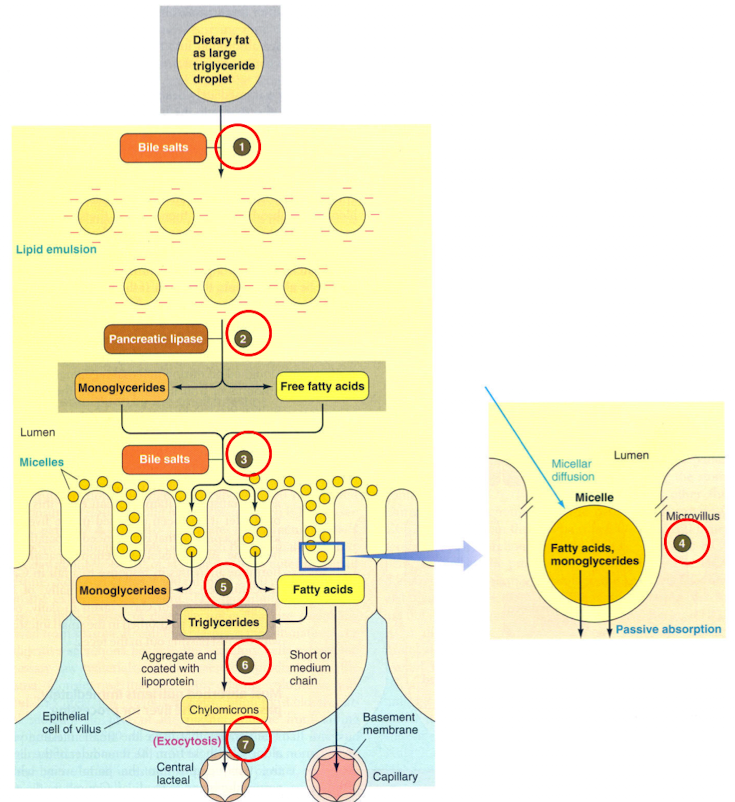
Function of Bile Salts
Aid fat digestion by acting as a detergent (emulsifying fat)
Facilitate fat absorption by forming fat micelles
How do bile salts aid fat digestion by acting as a detergent (emulsifying fat)?
Convert large fat globules → lipid emulsion of small droplets
Increases surface area for pancreatic lipase
How do bile salts help form micelles for absorption?
Micelles = tiny structures (smaller than fat droplet)
Composed of: bile salts, cholesterol (hydrophobic), and lecithin
Micelles have hydrophobic core and hydrophilic shell
How is fat digested and absorbed?
Fat is emulsified by the detergent action of bile salts
Lipases hydrolyze triglycerides into monoglycerides and free fatty acids
water insoluble products move in the interior of micelles to cell surface
Monoglycerides and free fatty acids diffuse into cell
Monoglycerides and free fatty acids resynthesizes into triglycerides
Triglycerides Coates with lipoprotein and form chylomicrons that are exocytosed from cell
Chylomicrons enter lymphatic vessels
How does content flow from the small to large intestine?
One-way flow from ileum → cecum
Prevents colonic bacteria from entering small intestine
What structures regulate this one-way flow?
Ileocecal valve
Ileocecal sphincter
What effects does gastrin have on intestinal flow?
Enhances gastric motility
Stimulates ileal motility
Relaxes ileocecal sphincter
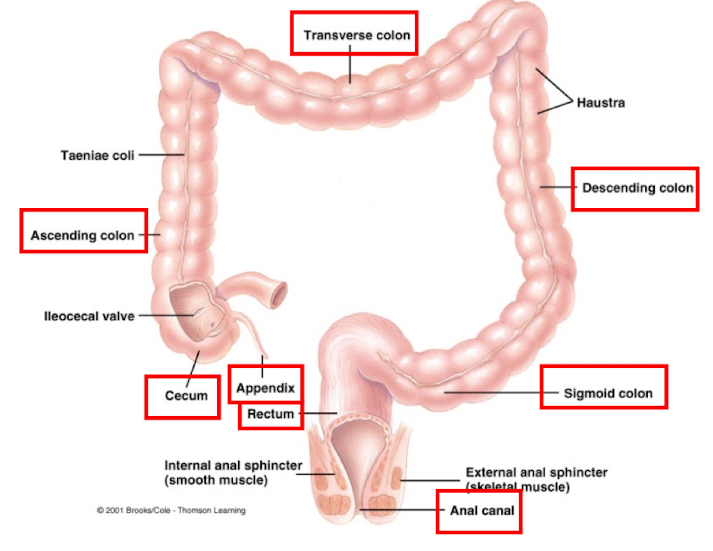
What are the two types of movements in the large intestine?
Haustral contractions: slow shuffling contents of large intestine to aid absorption (mainly water and salts)
colon’s main motility
Mass movements: large, strong contractions in ascending and transverse colon
Occur 3–4 times/day
Triggered by gastrin (after meals) and extrinsic autonomic nerves
What initiates the defecation reflex?
Mass movement pushes feces into rectum
Rectal wall distension activates stretch receptors → initiate reflex
Reflex:
Internal anal sphincter (smooth muscle) → relaxes
Rectum and sigmoid colon → contract
External anal sphincter (skeletal muscle) must also relax for defecation under voluntary control
What is constipation (large intestine) and what causes it?
Occurs when defecation is delayed
Too much water is reabsorbed → feces become dry and hard
What is appendicitis (large intestine) and how can it occur?
Caused by hardened feces lodged in appendix
Blocks normal circulation and mucus secretion
What are the 4 main mechanisms that regulate digestive function?
Autonomous smooth muscle (e.g., Interstitial Cells of Cajal)
Intrinsic nerve plexuses (Enteric Nervous System)
Extrinsic nerves (Autonomic Nervous System: Sympathetic & Parasympathetic)
Gastrointestinal hormones (e.g., Sympathetic Nervous System → Gastrin, Secretin, CCK)
What are Interstitial Cells of Cajal and what do they do?
Non-contractile autonomous smooth muscle cells
Act as pacesetters with slow-wave potentials that spread through gap junctions
Self-induced electrical activity referred to as:
slow wave potential
basic electrical rhythm (BER)
pacesetter potential
Regulate:
Rate of contraction
Intensity of contraction
Intrinsic Nerve Plexuses
functions to coordinate local activity within the digestive tract
contains both sensory neurons and neurons that innervate smooth muscle, exocrine, and endocrine cells
output cells can be excitatory or inhibitory
Extrinsic Nerves
Originate outside the digestive tract
Come from both sympathetic and parasympathetic nervous system
influence motility and secretion by
modifying ongoing activity in the internal nerve plexuses,
altering the level of gastrointestinal hormone secretion,
acting directly on smooth muscle and glands
Sympathetic Nervous system in digestive function Extrinsic Nerves
dominates in fight or flight situations
inhibits motility and secretion
Parasympathetic Nervous System in Digestive Function Extrinsic Nerves
dominates during rest
stimulates motility and secretion
acts primarily via vagus nerve
Gastrointestinal Hormones - Endocrine gland cells
located within the mucosa of certain regions of digestive tract
release gastrointestinal hormones into the blood
Gastrointestinal Hormones
released primarily in response to specific changes in the luminal contents (fats, proteins, acid)
carried by the blood to other areas of the digestive tract where they can exert either excitatory or inhibitory influences
Ex: Gastrin, Secretin, CCK
Which section of the stomach has the thickest musculature?
antrum
Large intestine is primarily a drying and storage organ that consists of:
Cecum (blind-ended pouch below illeocecal valve)
Appendix (finger-like projection of lymphoid tissue)
Colon (ascending, transverse, descending, and sigmoid)
Rectum (“straight”, connected to anal canal)
Carbohydrate Digestion and Absorption
Dietary polysaccharides starch and glycogen converted to disaccharide maltose
maltose, lactose, and sucrose converted to their respective monosaccharides (glucose, lactose, and fructose) by lactase, maltase, and sucrase. Molecules enter cell by Na+ and energy dependent secondary active transport
Glucose and galactose enter the blood down their concentration gradients by passive carriers
Fructose enters blood by facilitated diffusion
Protein Digestion and Absorption
Proteins hydrolyzed into peptide fragments and individual amino acids by pepsin and pancreatic proteolytic enzymes
Amino acids absorbed into cell via Na+ and energy-dependent active transport
Small peptides are broken down into amino acids by intracellular peptidases and aminopeptidases.
Amino acids then enter blood down their concentration gradients