Schizophrenia Spectrum and Other Psychotic Disorders (smartypance.com), Antipsychotics
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
Delusional disorder
Otherwise normally functioning person with a belief in something that does not exist but no other symptoms of schizophrenia.
Schizoaffective disorder
Psychotic disorder featuring symptoms of both schizophrenia and major mood disorder such as depression or bipolar disorder. Symptoms may occur at the same or different times
Schizophrenia
Psychotic disorder characterized by delusions, hallucinations, disorganized speech, and/or diminished, inappropriate emotional expression for greater than 6 months + difficulty functioning
Schizophreniform disorder
Major psychosis for > 1 week but < 6 months and no social or occupational impairment.
Delusional disorder
A 75-year old patient began thinking that her daughter was telling her caretakers to steal her money, although both her daughter and the caretakers deny this.
Schizoaffective disorder
A 45-year-old truck driver who c/o "hearing things that are not there" for two weeks. He reports that he was severely depressed five months ago and was placed on Prozac by his PCP. He recently started hearing voices.
Schizophreniform disorder
A 23-year-old male with c/o visual & auditory hallucinations that have been ongoing for two months. He is a graduate student at a local university, and he states that his hallucinations have been getting worse. He is still able to attend classes, but it is becoming more difficult to focus in class
Psychotherapy
What is the treatment of choice for delusional disorder?
Schizophrenia
Major psychosis for greater than 6 months difficulty functioning?
Delusional disorder
Otherwise normally functioning person with a belief in something that does not exist?
If the condition is less than six months it is schizophreniform, over six months it is schizophrenia
What differentiates schizophrenia from schizophreniform?
"True - Negative symptoms such as no facial expression
True or false: Patients with schizophrenia commonly have no facial expressions and poor hygiene.
Atypical antipsychotics such as olanzapine, risperidone or quetiapine
What is the treatment of choice for patients with schizophrenia?
True - Positive symptoms such as hallucinations and hearing voices are commonly associated with schizophrenia
True or false: Patients with schizophrenia hear voices?
Agranulocytosis; approximately 2% develop this side effect.
Clozapine is an atypical antipsychotic that is not considered first-line because of the propensity to cause what?
Typical neuroleptics - dopamine antagonists (haloperidol, chlorpromazine, thioridazine, loxapine, fluphenazine)
What medication are best for positive symptoms?
Patients with schizophrenia have an excess of xxx activity
dopamine
Blockage of the mesolimbic tract is crucial to the efficacy of antipsychotic therapy because excessive dopamine transmission here is believed to cause the positive symptoms of schizophrenia (hallucinations, delusions, agitation, and disorganized behavior/speech).
However, blockage of the other dopaminergic tracts can lead to unwanted side effects, including...
cognitive dysfunction (mesocortical tract)
hyperprolactinemia (tuberoinfundibular tract)
extrapyramidal symptoms (nigrostriatal tract).
D2 antagonists reduce positive symptoms (hallucinations, delusions, agitation, and disorganized behavior/speech).
Mesolimbic, Mesocortical, Nigrostriatal, Tuberfundibular
Mesolimbic pathway
Hypofunction of the mesocortical pathway may be related to cognitive and negative symptoms
Mesolimbic, Mesocortical, Nigrostriatal, Tuberfundibular
Mesocortical pathway
Stimulated purposeful movement; D2 antagonism induces extrapyramidal symptoms
Mesolimbic, Mesocortical, Nigrostriatal, Tuberfundibular
Nigrostriatal pathway
D2 antagonism increases prolactin levels (hyperprolactinemia)
Mesolimbic, Mesocortical, Nigrostriatal, Tuberfundibular
Tuberfundibular pathway
Increased risk for drug induced psychosis with drugs that increase synaptic xxx activity (eg, cocaine, amphetamines, levodopa)
dopamine
A limitation of the dopamine hypothesis is that it does not explain...
cognitive effects or implications of other neurotransmitters
•Haloperidol (Haldol)
•Fluphenazine (Prolixin)
•Perphenazine (Trilafon)
•Thioridazine (Mellaril)
•Chlorpromazine (Thorazine)
•Thiothixene (Navane)
•Trifluoperazine (Stelazine)
•Loxapine (Loxitane)
First generation (typical) antipsychotics
MOA of FGAs
dopamine antagonists
•Clozapine (Clozaril)
•Olanzapine (Zyprexa)
•Risperidone (Risperdal)
•Paliperidone (Invega)
•Quetiapine (Seroquel)
•Ziprasidone (Geodon)
•Aripiprazole (Abilify)
•Iloeridone (Fanapt)
•Asenapine (Saphris)
•Lurasidone (Latuda)
•Pimavanserin (Nuplazid)
•Brexpiprazole (Rexulti)
•Cariprazine (Vraylar)
•Lumateperone (Caplyta)
Second generation (atypical) antipsychotics
First line agents in treatment of schizophrenia
SGAs - Risperidone
xxx should be considered after 2 failed antipsychotic trials
Clozapine
One of the most common agents prescribed for Schizophrenia
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Risperidone
Greater incidence of movement disorders
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Risperidone
Which 2nd generation antipsychotic has very high D2 antagonism, which can WORSEN negative symptoms?
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Risperidone
Increased risk of agranulocytosis, myocarditis, seizures, orthostatic hypertension
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Clozapine
Best drug for med refractory Schizophrenia
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Clozapine
Starting dose of Clozapine?
12.5-25mg
Higher risk of prolonged QT interval
Risperidone, Quetiapine, Olanzapine, Clozapine, Ziprasidone, Aripiprazole
Ziprasidone
MOA of SGAs
Four different mechanisms may contribute to "atypical" profile
•5-HT2A antagonism in the mesocorticial tract
•Serotonin-dopamine antagonism
•D2 antagonism with rapid dissociation
•D2 partial agonist
•Serotonin partial agonists at 5HT1A receptors
Antipsychotic effect - relief of positive symptoms, induction of EPS, increased prolactin levels
D2, serotonin, alpha1, H1, or M1 antagonism?
D2 antagonism
May attenuate EPS, improvement in negative symptoms and cognitive impairment
D2, serotonin, alpha1, H1, or M1 antagonism?
5HT2A-antagonism
Sedation, hypotension, reflex tachycardia
D2, serotonin, alpha1, H1, or M1 antagonism?
alpha1-antagonism
Sedation, contribution to weight gain
D2, serotonin, alpha1, H1, or M1 antagonism?
H1-antagonism
Anticholinergic effects (tachycardia, constipation, blurred vision, urinary retention, dry mouth, drowsiness)
D2, serotonin, alpha1, H1, or M1 antagonism?
M1 antagonism
Why would someone choose an SGA vs FGA?
Lower risk of EPS including tardive dyskinesia
Less prolactin elevation
Less neuroleptic malignant syndrome
Neutral effect (improvement on negative symptoms)
Main therapeutic effect of first generation antipsychotics
Relief of hallucinations, delusions, and disordered thought (positive symptoms)
Which FGAs are available as long acting injections?
Haloperidol (Haldol)
Fluphenazine (Prolixin)
Why are long acting FGA injections (Haloperidol, Fluphenazine) beneficial in treatment of schizophrenia?
Useful for non-compliant patients
When changing from an oral to intramuscular FGA (Haloperidol, Fluphenazine), sometimes need up to xxx injections to be given before discontinuing the oral dose
two
Which FGA has a higher risk of QTc prolongation?
IV Haloperidol
Which has a lower risk of EPS including tardive dyskinesia - FGAs or SGAs?
SGAs
Indicated for treatment resistant schizophrenia
Clozapine
Indicated for recurrent suicidal behavior associated with schizophrenia
Clozapine
Compared to other psychotropic agents, xxx has the most boxed warnings
Clozapine
Name 5 boxed warnings for Clozapine
1. Agranulocytosis
2. Seizure risk
3. Myocarditis
4. Orthostatic hypotension
5. Increased mortality in elderly with dementia related psychosis
What type of SGAs are Risperidone, Palperidone, Olanzapine, Aripriprazole?
Long acting
Metabolic side effects of SGAs include...
weight gain, dyslipidemia, impaired glucose tolerance/insulin resistance
Dopamine prevents the release of...
prolactin
Antipsychotics cause an increase in xxx via D2 inhibition
prolactin
Hyperprolactinemia is a side effect of what receptor antagonism?
D2 (dopamine) antagonism
Dystonia, Akathisia, Parkinsonism, Tardive Dyskinesia
Extrapyramidal symptoms
Antipsychotic exposure timeline of EPS symptoms (Dystonia, Akathisia, Parkinsonism, Tardive Dyskinesia)
Min-days: acute dystonia
Hours-days: acute akathisia
Days-weeks: Parkinsonism
> 3 months: Tardive dyskinesia
Antipsychotic exposure timeline of EPS symptoms
Dystonia --> Akathisia --> Parkinsonism --> Tardive dyskinesia
Spasms or sustained contractions of the neck or face (eg, trismus, protrusions of the tongue, facial grimacing, torticollis, and difficulty speaking).
Acute dystonia
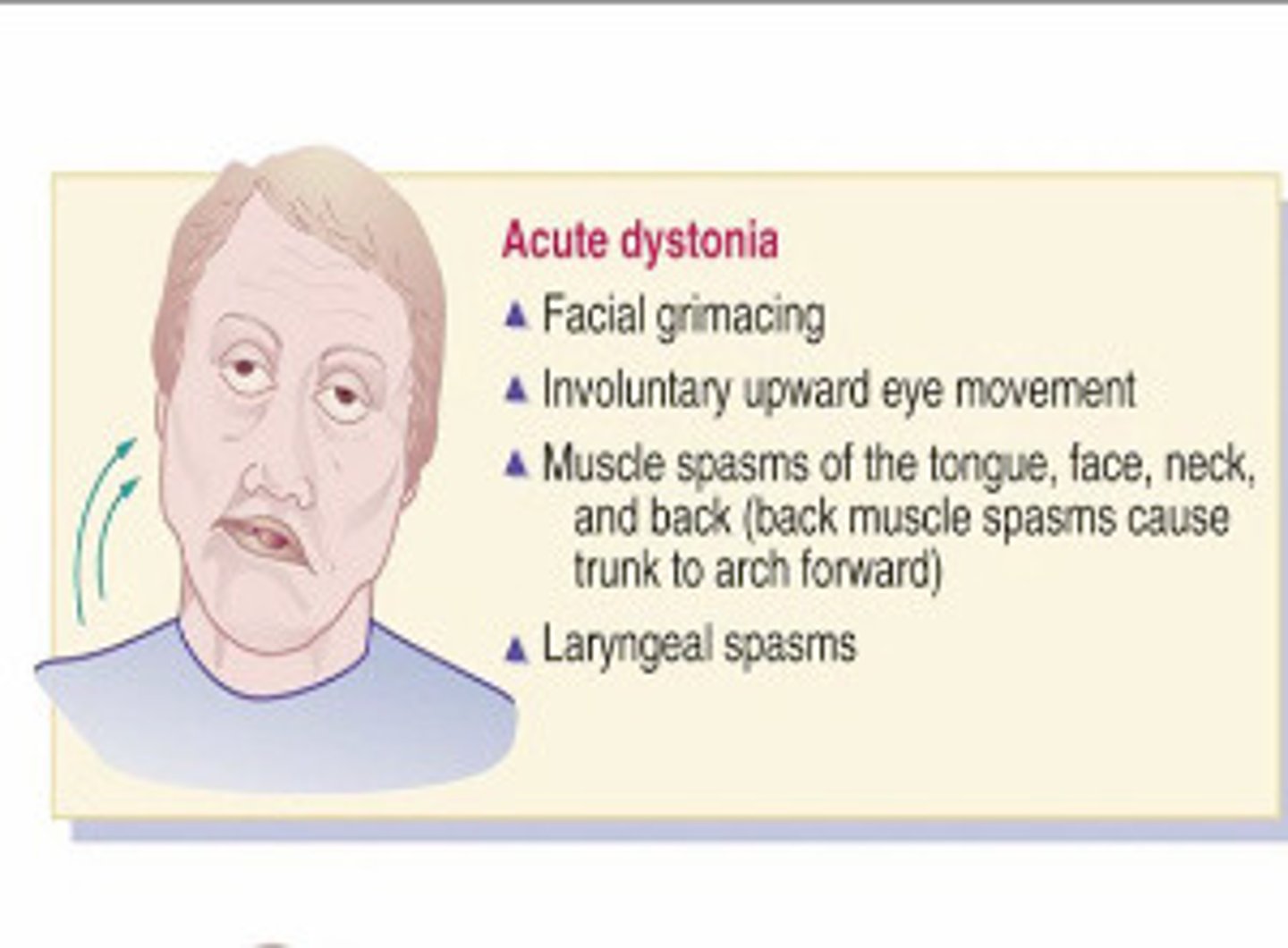
Management of acute dystonia
Anticholinergic agents (Diphenhydramine, Benztropine, Trihexyphenidyl)
Feeling of restlessness
Akathisia
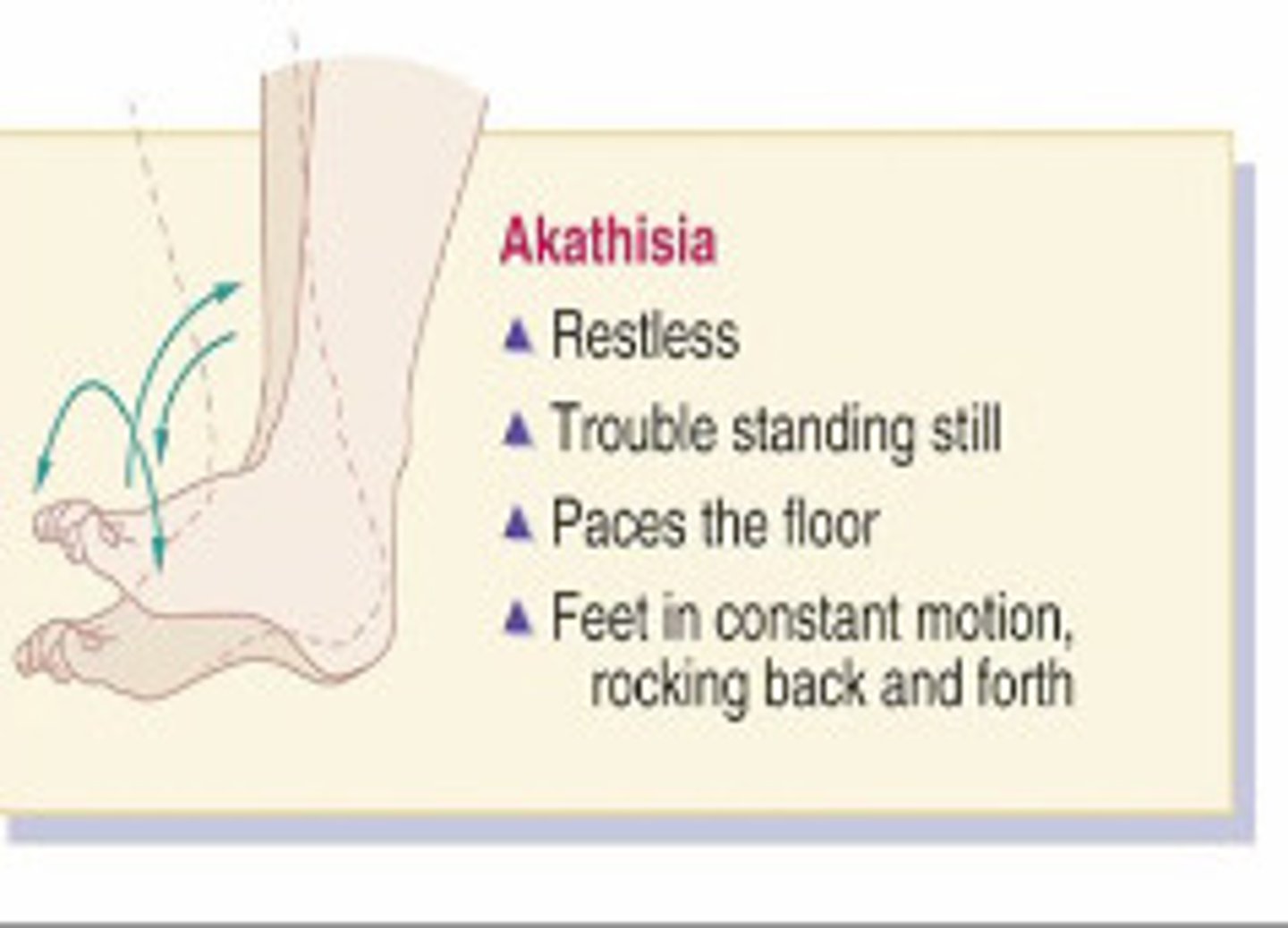
Management of akathisia
Decrease dose, slower dose escalation, change agents
Beta-blockers (eg, Propranolol) first line, Benzodiazepines, Anticholinergic agents
Bradykinesia, resting tremor, Cogwheel rigidity, postural abnormalities
Parkinsonism
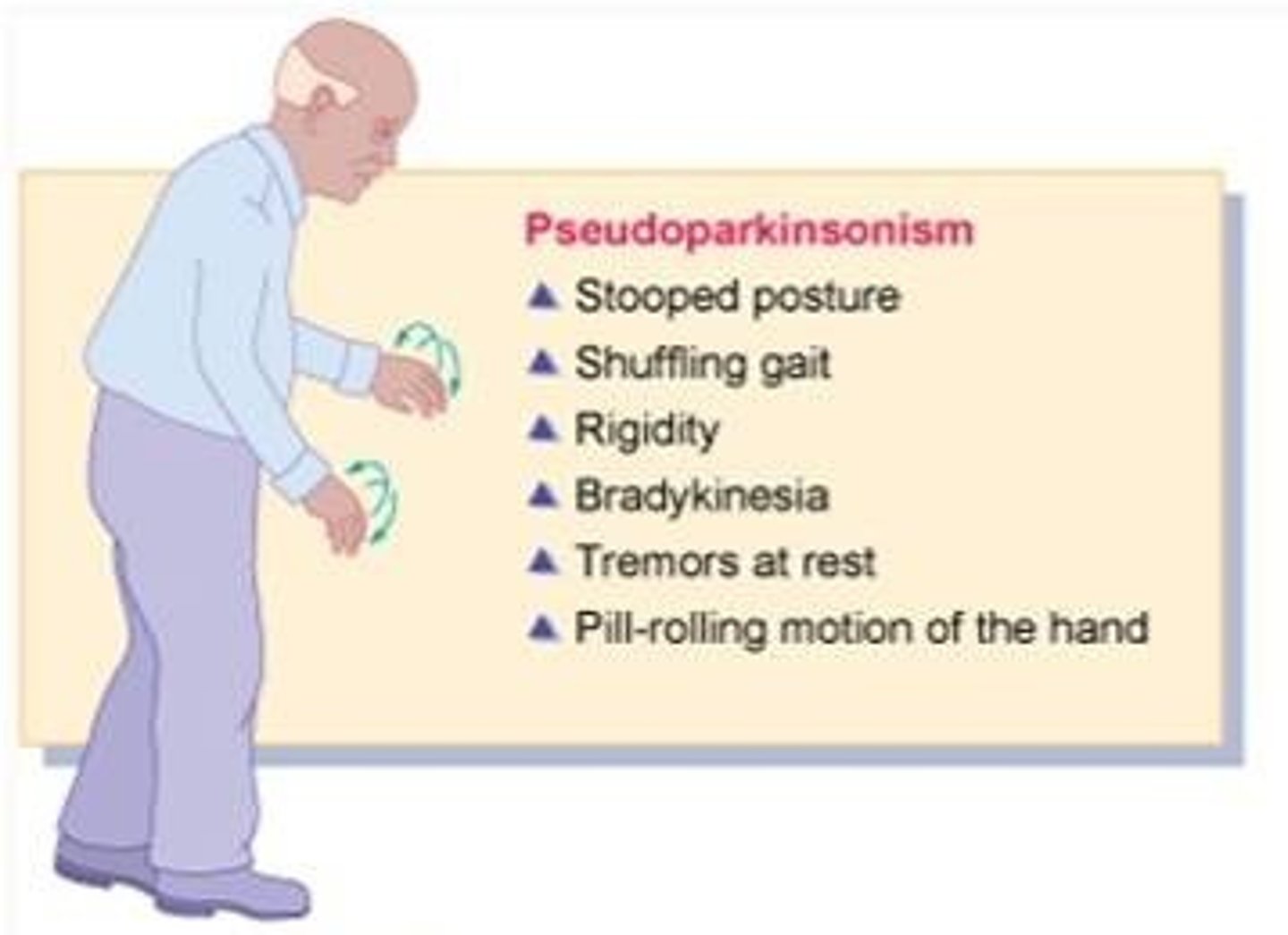
Management of Parkinsonism
Change to a different agent or decrease the dose.
Oral anticholinergic agents
Repetitive involuntary movements mostly involving the face (eg, lip smacking, teeth grinding, and rolling of the tongue). Seen with long term use (especially first generation)
Tardive dyskinesia
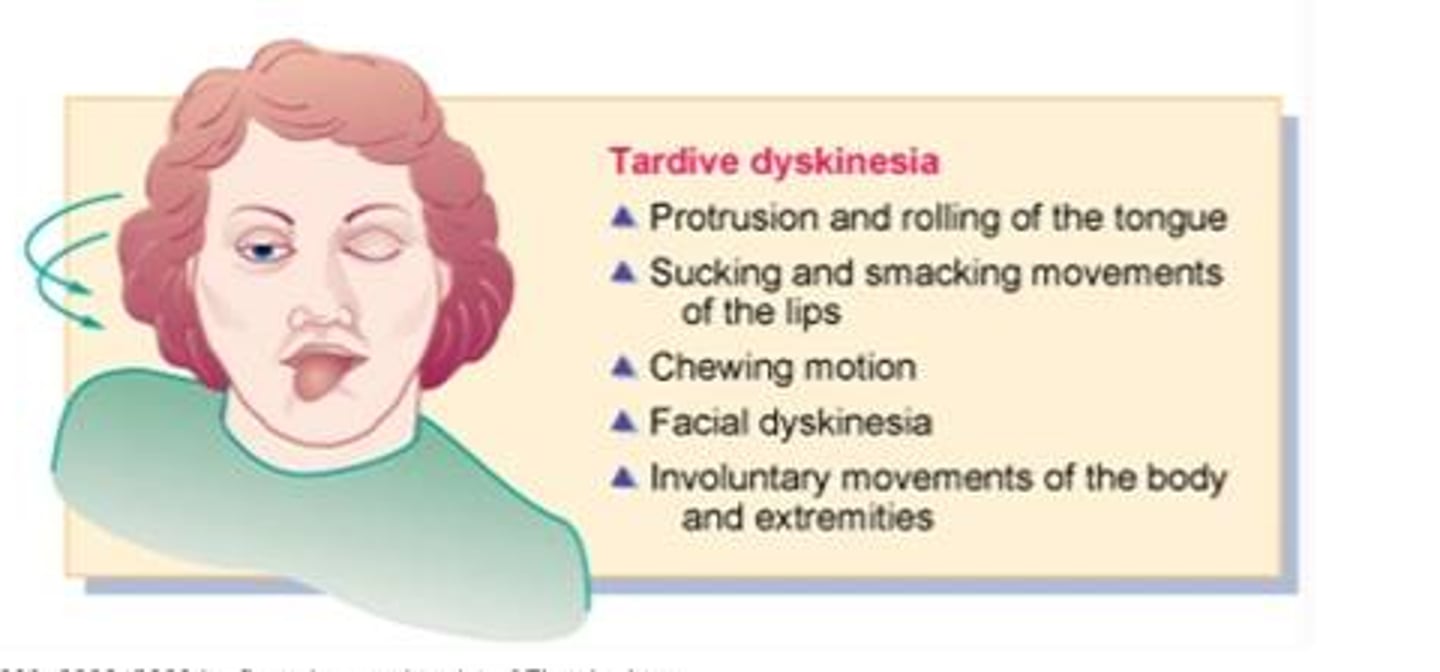
How do you prevent Tardive dyskinesia?
Lowest effective dose
Change from FGA to SGA
Minimize anticholinergic agents
Get a baseline Abnormal Movement Scale (AIMS) and on-going
Management of Tardive dyskinesia
Deutetrabenazpine, Valbenazine, Tetrabenazine (these are VMAT2 inhibitors and deplete monoamines, including dopamine to reduce hyperkinetic movements)
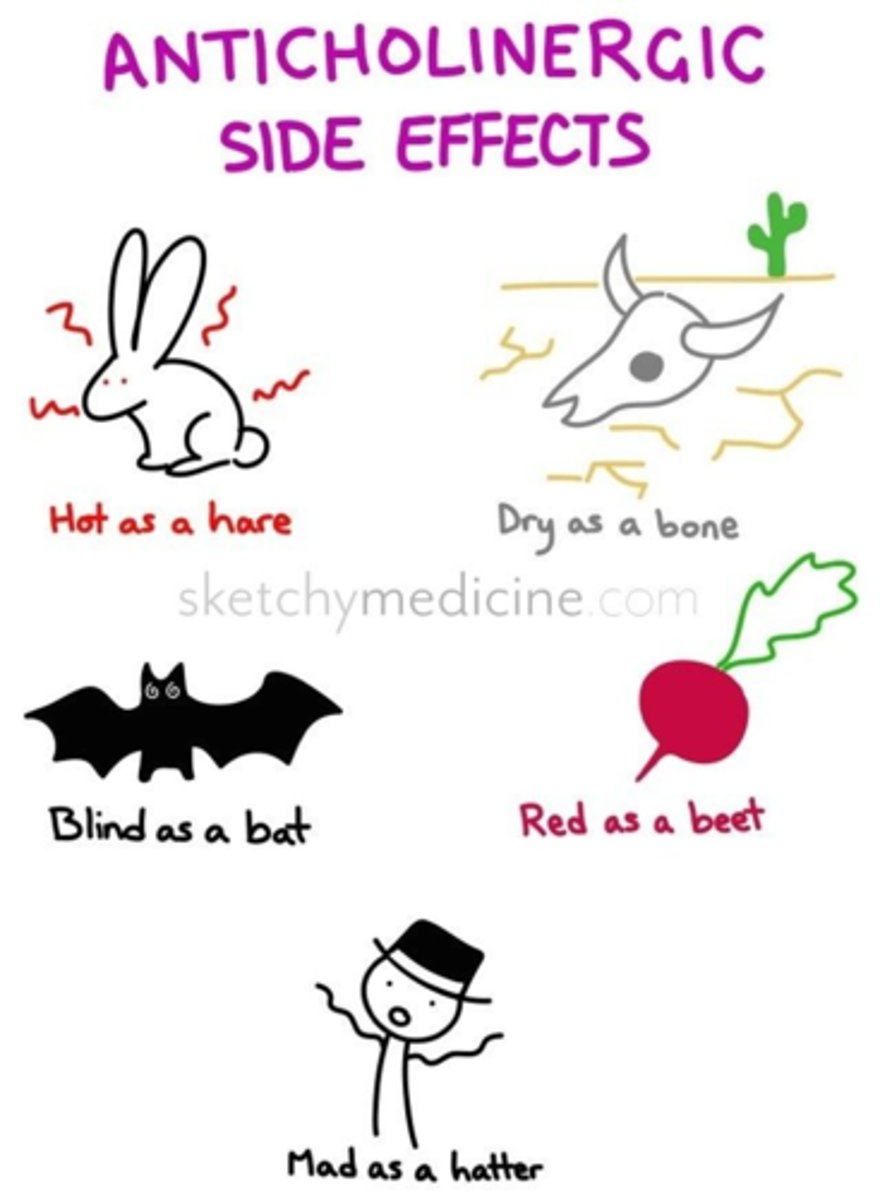
Anticholinergic side effects
Dry mouth, dry eyes, blurred vision, urinary retention, constipation, and hyperthermia
Antihistaminic side effects
sedation, weight gain
Alpha1-antagonism side effects
Sedation, hypotension, reflex tachycardia
When do we initiate clozapine in clinical practice?
ANC > 1500/μL
Why do we monitor a patient on Clozapine?
Risk of agranulocytosis (neutropenia)
When initiating Clozapine, make sure to get a baseline...
CBC w/ diff
When initiating Clozapine, how often should you get a CBC w/ diff?
Baseline
First 6 months of therapy = weekly
6-12 months = every 2 weeks
> 12 months = every 4 weeks
xxx patients with dementia-related psychosis treated with ANY antipsychotic drug are at an increased risk of death compared to placebo.
Elderly
Altered mental status, "lead-pipe" muscle rigidity, autonomic instability (tachycardia, tachypnea, hyperthermia, fever, bp changes, hypersalivation, and diaphoresis), incontinence, leukocytosis, rhabdomyolysis (increased CPK, LDH, and LFTs)
Neuroleptic malignant syndrome
Management of Neuroleptic malignant syndrome
Stop causative agent. Supportive care, Dopamine agonists (eg, Bromocriptine, Amantadine, Lorazepam, Dantrolene)
After treating Neuroleptic malignant syndrome, can you rechallenge antipsychotics?
Yes. May rechallenge antipsychotics after 2 weeks of complete resolution of symptoms.
Smoking causes induction of...
CYP450 1A2
Initiation of smoking (eg, after discharge from hospital) can cause emergence of xxx symptoms in patients with schizophrenia
psychiatric
HT is a 23 y/o man with a history of schizophrenia presenting to the ED with disorganized behaviors and increasing agitation. He is given 5 mg of intramuscular haloperidol. Approximately 15 minutes later he is found to have severe contraction of muscles in his neck. What is the most appropriate course of action:
a.
The patient's agitation is not resolved thus administer additional intramuscular haloperidol
b.
The patient is likely experiencing akathisia and propranolol would be the treatment of choice
c.
The patient is likely experiencing an acute dystonia, administer parenteral diphenhydramine
d.
The patient is having a parkinsonian reaction, levodopa-carbidopa should be administered
The patient is likely experiencing an acute dystonia, administer parenteral diphenhydramine
SK is a 38 year old man with a history of schizophrenia who has failed 3 adequate trials of different antipsychotic medications (olanzapine, aripiprazole, risperidone). He has a past medical history of hyperlipidemia and hypertension. The most appropriate medication regimen for SK would be:
a.
A trial of clozapine, due to his multiple treatment failures his schizophrenia can be considered treatment resistant
b.
The patient should have a retrial of risperidone because it is available in a long acting injectable
c.
A combination of ziprasidone and quetiapine should be given, because he has not had a trial of 2 coadministered second generation antipsychotics yet
d.
A trial with the first generation agent chlorpromazine should be considered due to its superiority over clozapine
A trial of clozapine, due to his multiple treatment failures his schizophrenia can be considered treatment resistant
YP is a 53 year old female with a history of schizophrenia who was newly started on clozapine during a 19 day inpatient hospitalization. After discharge YP begins smoking 2 packs per day (she did not smoke during her hospitalization). What is a potential consequence of YP beginning to smoke after discharge:
a.
Serum level of clozapine may increase resulting in the risk of seizure
b.
Serum level of clozapine may increase resulting in the risk of agranulocytosis
c.
Serum level of clozapine may decrease resulting in the risk of relapse and rehospitalization
d.
Serum levels of clozapine will not change, but she should be counseled on the benefits of smoking cessation
Serum level of clozapine may decrease resulting in the risk of relapse and rehospitalization
SC is a 24-year-old male who was admitted to an inpatient hospital service for 3 weeks for auditory hallucinations, persecutory delusions, and bizarre behavior and speech including attempting to walk home in cold weather from a city 45 miles away. He had been having delusions and unusual behaviors for much of the past 6 months. His symptoms improved significantly with his hospital care including treatment with risperidone. Collateral information from his family indicated during his second year of college, around age 21, he had a personality change, he withdrew from his college courses, and stopped communicating with friends and family. Medical work-up upon admission, including routine labs, head imaging, and urine drug and alcohol screening were all negative.
The patient and his parents present to an outpatient follow-up appointment 1 month after the hospital discharge. The patient and his parents all insist that th
Recommend changing risperidone to fluoxetine for improved side effect profile and targeting the depressed phase of his illness
JL is a 27-year-old women who present to the outpatient clinic with her mother. JL's father is estranged but is known to suffer from schizophrenia and poor medication adherence and severe psychosocial problems. JL's mother wants to know what can be done to better understand or reduce JL's risk of also developing schizophrenia. JL has not developed positive or negative symptoms of schizophrenia, but has difficulty keeping jobs due to anxiety and does "self-medicate" with cannabis two to three times per for anxiety and being easily overwhelmed by day-day stressors.
a.
Recommended chemical dependency evaluation/treatment and cognitive behavioral therapy for her anxiety
b.
Recommend prophylactic treatment with an antipsychotic medication as her family history places her at moderately high risk of schizophrenia
c.
Recommend a PET scan of brain to evaluate the mesolimbic and mesocortical pathways
d.
Order polygenic risk s
Recommended chemical dependency evaluation/treatment and cognitive behavioral therapy for her anxiety