Week 8: Complex Wounds
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
What are pressure ulcers?
Localized injury to the skin and/or underlying tissue, usually over a bony prominence
List the types of leg ulcers
-Arterial
-Venous
-Mixed
-Neuropathy (Diabetic)
List the possible pressure ulcer sites
-Ears
-Occiput
-Scapula
-Elbow
-Sacrum
-Greater trochanter
-Ischial Tuberosities
-Medial condyle
-Tibia
-Fibular head
-Lateral malleolus
-Medial malleolus
-Heels
How many pressure ulcer stages are there?
4 Stages
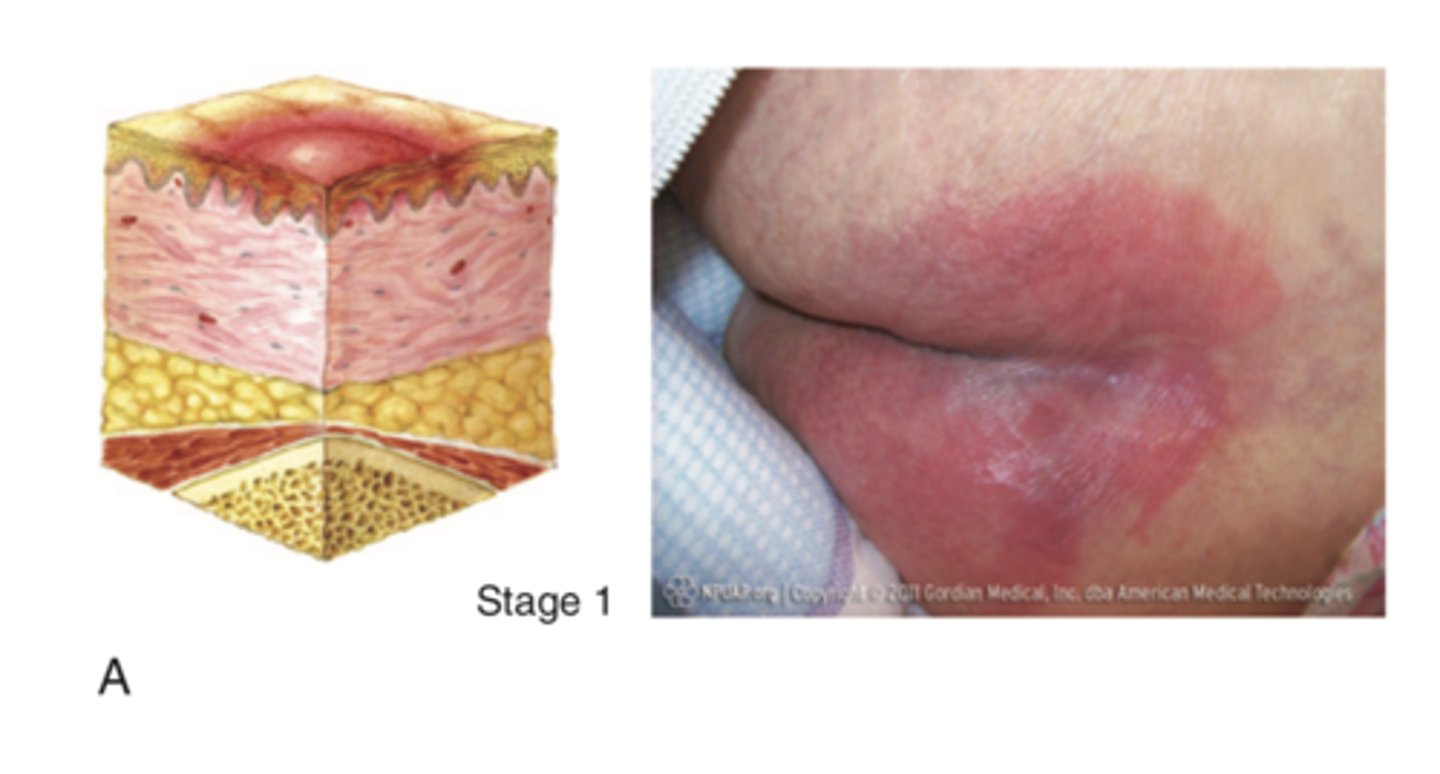
Outline stage 1 of pressure ulcers
-Intact skin
-Damage to skin but reversible
-Non-blanchable erythema that is red and doesn't lighten when pressed
-May be painful
-Patient may say: "I told the nurse my heel was sore"
-May be be warmer or cooler than surrounding skin
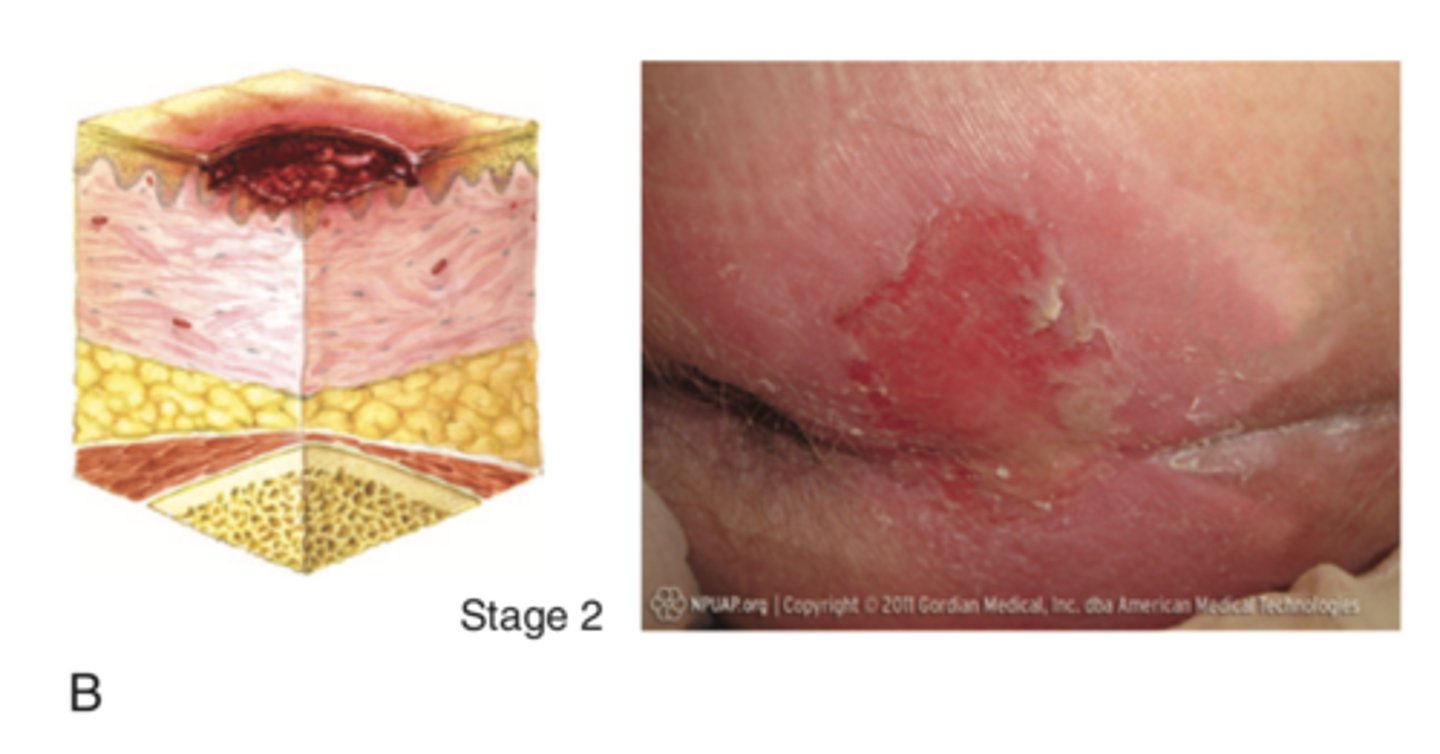
Outline stage 2 of pressure ulcers
-Partial-thickness skin loss (skin break down) involving epidermis, dermis, or both
-Pen wound
-Superficial
-Skin may be intact but appear as a fluid filled blister
-No slough or necrosis
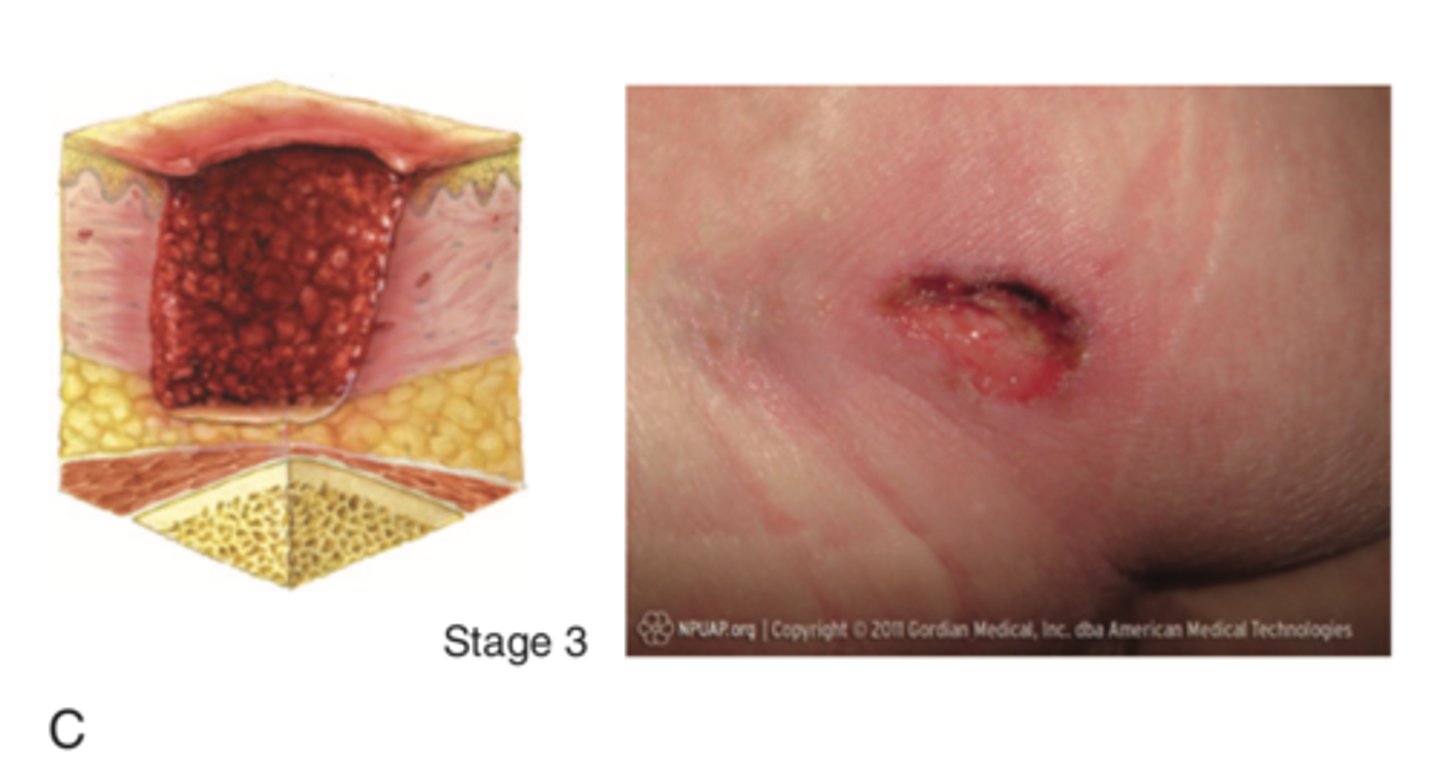
Outline stage 3 of pressure ulcers
-Full-thickness tissue loss with visible subcutaneous fat
-Some slough and necrosis may be present and may include tunneling under neighbouring tissue
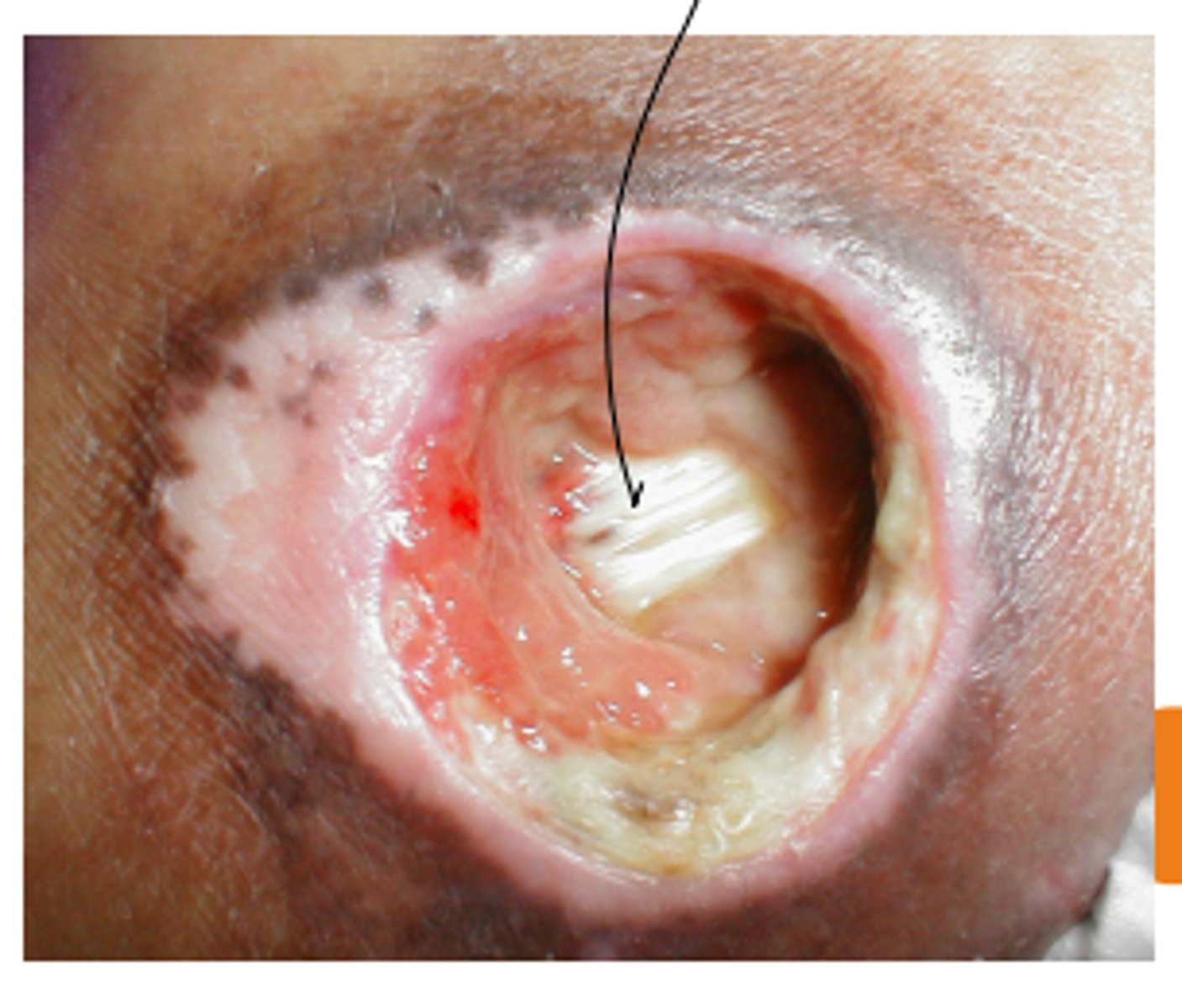
Outline stage 4 of pressure ulcers
-Full thickness
-Depth varies based on location
-Extends through muscle down to bone and tendon
-Slough and eschar may be present
-Undermining and tunneling may occur
Define the unstageable stage of pressure ulcers
-Can not confirm full extent of tissue loss
-Obscured by slough or necrosis (black tissue)
-Stable eschar should NOT be removed

List the factors involved in ulcer prevention
-Assess risk factors
-Assess for tissue integrity and perfusion
-Relieve pressure/ Pressure redistribution
-Address patient factors
-Use proper dressings
What is the braden scale?
A clinical tool used to assess a patient's risk of developing pressure ulcers
Outline the six categories of the braden scale
-Sensory perception
-Moisture
-Activity
-Mobility
-Nutrition
-Friction and shear
Outline the four categories of the braden scale
1: Completely limited
2: Very Limited
3: Slightly Limited
4: No Impairment
List the principles of asepsis
-All objects on a sterile field must be sterile
-A sterile object remains sterile only when touched by another sterile object
-A sterile object or field out of the range of vision or an object held below a person's waist is considered to be contaminated
-A sterile object or field becomes contaminated by prolonged exposure to air
-When a sterile surface comes in contact with a wet, contaminated surface, the sterile object or field becomes contaminated by capillary action.
-Any puncture or tear that passes through the sterile barrier results in a non-sterile area
-Fluid flows in the direction of gravity
If in doubt about the sterility of the object, consider it unsterile
-The edges of a sterile field or container are considered to be contaminated
List the wound care goals and nursing Responsibilities surrounding wounds
-Assessment of the wound and of peri-wound skin (skin around the wound)
-Dressing change
-Provide a wound environment that supports healing with an appropriate topical dressing
-Choose a wound dressing that meets the characteristics of the wound bed
MOA of gauze dressing
Most utilized. Can be used to dress, dry, or pack a wound
MOA of Non Adherent contact layer dressing
Can be applied to a wound bed (open area) to prevent disruption of the healing process by protecting newly healed epithelial tissue from being removed by gauze
MOA of Mepilex dressing
5 layer dressing designed to channel and trap exudate away from the wound bed as well provides a barrier that prevents exudate from re-entering the wound even under compression
MOA of Hydrogel (intra-site) dressing
Preforms autolytic debridement to a necrosed tissue , by helping the body promote its own autolytic debridement process
MOA of Transparent film dressing
Often placed over IV's, but can be placed over areas of friction. They are also selective filters that are occlusive to liquids, bacteria, and viruses, but water vapor, oxygen, ad carbon dioxide can easily be exchanged (semi-permeable)
Foam (Lyofoam and Biatain) dressing
Non-adherent absorption of exudate and other fluid discharge, but will need to be secured with tape as it does not have an adherent border. It also does NOT provide any sort of cushion
Alginate dressing
Forms a gel when in contact with wound fluid, absorbing up to 20 times their weight in fluid, and can be used on infected and non-infected wounds
MOA strip packing and antimicrobials dressing
Comes in many forms:
Plain packing: Should be used with saline and soaked with saline then placed into the wound.
lodoForm packing: Used for packing small areas or tracks if tunneling is present. Comes with pretreatment of antimicrobial properties, thus it should NOT be soaked in saline and should be placed on the wound as it
How should you prepare for a complex dressing change?
-Prepare Patient: Explain the process/what to expect, and pretreat with analgesia (30 minutes - 1 hour in advance)
-Dressing tray
-Syringe and angiocath
-Sterile gloves
-Dressing material
-Tape/other securing device (E.g. Tape)
What does a complex dressing entail?
-Sterile procedure
-Wound is typically open
-Requires assessment of wound base
-May change dressing product depending on assessment
Should you clean from least to most contaminated or most contaminated to least contaminated?
Least to most contaminated (clean to dirty)
1 multiple choice option
True or False: Irrigation and packing of the wound is common?
True
1 multiple choice option
What does a simple dressing entail?
-Aseptic (no touch) procedure
-Wound is closed
-Requires assessment of incision
-Clean least to most contaminated
-Mainly use gauze and non adherent contact layer
MOA wound Irrigation
Cleanses and irrigates surgical or chronic wounds by introducing a cleansing solution directly into the wound
What kind of pressure does wound irrigation utilize?
Perform a high-pressure and pulsatile high-pressure lavage (aka irrigating/washing)
What do you want to avoid in wound irrigation?
Fluid retention in the wound
What does wound irrigation promote?
Wound healing
What should you use and assess for when packing a wound?
-Assess size, depth, shape of wound base
-Assess for tunnelling and undermining (can use a sterile Q-tip to assess)
What should you pack a wound with?
Normal saline (NS) soaked gauze (unless otherwise indicated)
List the types of wound debridement
-Autolytic
-Enzymatic
-Mechanical
-Biological
-Sharp
MOA of autolytic wound debridement
The body's natural processes of breaking down and removing necrotic tissue in a moist wound environment. And with some with some modern dressing (E.g. Intrasite) to facilitate the removal of devitalized tissue while minimizing trauma to healthy tissue
MOA of enzymatic (collagenase) wound debridement
Enzymes solutions are applied to the wound in an effort to remove devitalized tissue. However, enzymes non-selectively remove both healthy and devitalized tissue (which can be problematic)
MOA of biological wound debridement
The use of maggots to remove necrotic tissue
MOA of mechanical wound debridement
Accomplished by irrigating the wound, to help remove necrotic or slough tissue and will not be damaging to healthy tissue
MOA of sharp wound debridement
Surgical, a sharp object is used to cut away the necrosed tissue
What is DIMES?
A wound bed treatment strategies chart, acting as a framework to assess and guide the management of wounds
What does DIMES stand for?
D-Debridement
I-Infection or Inflammation Control
M-Moisture Balance
E-Edge of the Wound
S-Supportive Care
MOA of negative pressure wound therapy (Wound VAC)
The application of negative pressure to a wound through suction. The entire system needs to be enclosed and airtight in order to:
-Accelerate wound healing
-Optimize blood flow
-Remove wound fluid
-Maintain a moist environment
Outline the steps for collecting a wound culture
1. Clean wound using sterile normal saline
2. Moisten a sterile swab from a culturette tube with sterile normal saline to more readily absorb organisms
3. Press swab to the wound in the area closest to the wound bed to ensure wound flora rather than skin contaminants are captured.
4. May press around the wound and gently turn the swab to collect as much tissue or fluid as possible.
5. Placed swab into either an aerobic or anaerobic culture tube or both, depending on the type of organism suspected,
6. Send to the laboratory for culture
What should be included in the documentation of the wound?
-Location of wound
-What dressings and packing did you remove
-Length width and depth of wound
-Appearance of wound edges
-Amount and type of exudate
-Irrigation fluid used (irrigated until clear)
-Any cultures taken (E.g. Swabs)
-Presence of signs of healing (granulation tissue)
-What the wound was packed with (E.g. NS soaked gauze)
-External dressing used
-Patients tolerance of the dressing change