Chapter 22: The Respiratory System
1/108
Earn XP
Description and Tags
Merged flashcards from Chapter 22, McGraw Hill Anatomy and Physiology Tenth Edition, by Kenneth S. Saladin.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
109 Terms
Respiratory system
Organ system that takes in and expels air from the body
Respiration (breathing)
Ventilation of the lungs
Respiratory system functions
Gas exchange (O2 and CO2)
Acid-base balance (CO2 pH regulation)
Blood and lymph flow and filtration (pressure)
Platelet production (transfer to blood)
Blood pressure regulation
Abdominal content expulsion
Olfaction (smell)
Communication (speech)
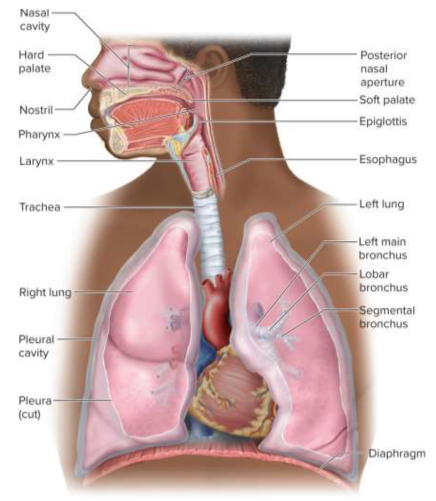
Respiratory system organs
Nose
Pharynx
Larynx
Trachea
Bronchi
Lungs
Respiratory system zones
Conducting zone (airflow)
Respiratory zone (gas exchange)
Upper respiratory tract (nose to larynx)
Lower respiratory tract (trachea to lungs)
Conducting zone
Area of the respiratory system that serves only for airflow, no gas exchange (nostrils)
Respiratory zone
Areas of the respiratory system that participate in gas exchange (alveoli, other structures)
Upper respiratory tract
Area of the respiratory system from the nose to the larynx
Lower respiratory tract
Area of the respiratory system from the trachea to the lungs
Nose
Part of the respiratory system made of cartilage that warms, cleanses, and humidifies air while detecting odors and amplifying voice through chambers
Ala nasi
Flared portion at the lower end of the nose made of specialized cartilage
Nasal septum
Structure that divides the nasal cavity into the left and right nasal fossae; made of cartilage
Vestibule
Small chamber inside the nostrils with guard hairs that block insects and debris from entering the nose
Nasal conchae (turbinates)
Tissue that vibrates the vestibule from behind to move mucus

Goblet cells
Mucus-producing cells

Ciliated cells
Cells with motile cilia that move mucus
Olfactory epithelium
Tissue within the nose involved in smell through chemical detection
Erectile tissue (swell body)
Tissue that restricts airflow to each nostril 30 to 60 minutes at a time by swelling with blood to allow recovery from drying
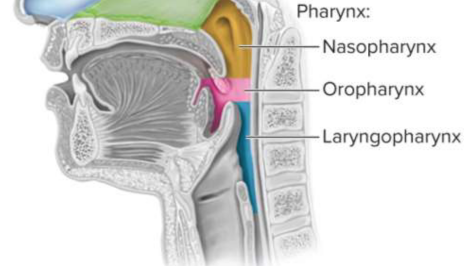
Pharynx
Muscular funnel extending about 13 cm that is divided into three regions:
Nasopharynx
Oropharynx
Laryngopharynx

Nasopharynx
Part of pharynx that receives the auditory tubes and contains the pharyngeal tonsil

Oropharynx
Part of the pharynx that contains the palatine tonsils

Laryngopharynx
Part of the pharynx that is posterior to the larynx and begins the esophagus
Larynx
A cartilaginous chamber to keep food and drink out of the airway and produce sound
Epiglottis
Flap of tissue over the top of the larynx that prevents airway occlusion
Thyroid cartilage
Shield-shaped and largest laryngeal cartilage; contains the laryngeal prominence (Adam’s apple) which is larger in males due to testosterone
Vestibular folds
Folds of the larynx that play no role in speech but close the larynx during swallowing; supported by vestibular ligaments
Vocal cords (vocal folds)
Folds of the larynx that produce sound when air passes between them, contains vocal ligaments to endure vibration and contact alongside muscles to create sound
Gender vocal cord differences
Males have longer and thicker vocal cords that vibrate slower and produce lower-pitched sounds
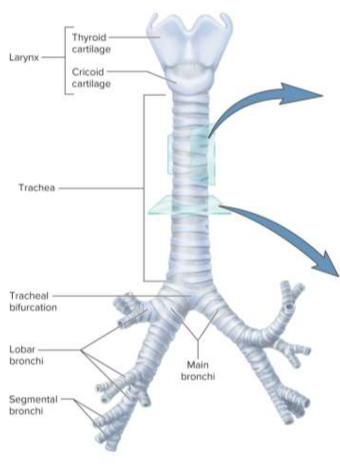
Trachea (windpipe)
Rigid tube that connects the larynx to the bronchi; is anterior to the esophagus and supported by cartilage rings
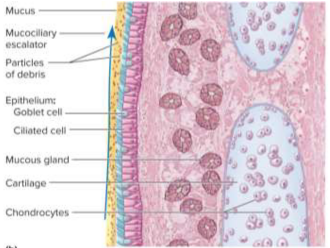
Mucociliary escalator
Mechanism for debris removal to move particle-trapping mucus upwards towards pharynx to be swallowed
Tracheotomy
A temporary opening in the trachea with a tube to allow airflow, preventing asphyxiation, but can dry out mucous membranes and increase infection risk by bypassing the nasal cavity
Intubation
Directly introducing air into the trachea with a ventilator; air is filtered and humidified
Base
The broad, concave portion of the lung resting on the diaphragm
Apex
Tip of the lung that projects above the clavicle
Costal surface
Part of the lung pressed against the ribcage (costals)
Mediastinal surface
Part of the lung that faces medially toward the heart
Hilum
Slit through the lung recieving the main bronchus, blood vessels, lymphatics, and nerves
Lobe diffferences
Right lung has three lobes (superior, middle, and inferior) while left lung has two (superior and inferior)
Cardiac impression
The left lung’s indentation to accomodate the heart
Bronchial tree
A branching system of air tubes in each lung
Main bronchi (primary bronchi)
Bronchi that arises from the fork of the trachea; right is wider and more vertical than left leading to higher aspiration rates
Lobar bronchi (secondary bronchi)
Bronchi branhcing off into each lobe of the lung into to superior, middle, and inferior lobar bronchi (superior and inferior in the left lung)
Segmental bronchi (tertiary bronchi)
Bronchi that branch off the lobar bronchi into smaller segments
Bronchioles
Continuations of the bronchi without supportive cartilage, <1 mm in diameter
Terninal bronchioles
The final branches of the conducting zone and bronchi before the alveoli; no mucous glands or goblet cells (instead moving on mucociliary escalator)
Respiratory bronchioles
Bronchioles that branch off terminal bronchioles with alveoli budding from the walls for gas exchange; considered part of the respiratory zone
Alveolar sacs
Clusters of alveoli around a central space
Alveoli
Microscopic air patches in the lungs about 0.2 to 0.5 mm in diameter for gas exchange
Alveolar macrophages (dust cells)
One of the most numerous cells in the lung, they wander the alveoli and connective tissue by phagocytizing (“eating”) dust particles then go up the mucociliar escalator
Respiratory membrane
The thin barrier between the alveolar air and blood where gases are exchanged across
Pulmonary circuit pathway
After passing through pulmonary valve:
Pulmonary trunk
Pulmonary arteries
Lobar arteries
Capillaries around alveoli
Pulmonary veins
Then to left atrium
RIght-to-left shunt
Blood flow pattern in the heart where some deoxygenated blood passes to the oxygenated left ventricle, diluting oxygen content
Alveolar pressure
Lower to prevent accumulation and increase aeration
Pleura
Serous membrane that lines the thoracic wall and forms the surface of the lung, split into the visceral (surface) and parietal (medastinal) pleura
Visceral pleura
Pleura that forms the surface of the lung
Parietal pleura
Pleura that adheres to the mediastinum and inner surface of the rib cage
Pleural cavity
The potential space between the pleurae for friction reduction and pressure maintenance
Inspiration
The act of inhalation
Expiration
The act of exhalation
Respiratory cycle
One complete breath measuring the cycle of inhalation and expiration; relies on pressure differences
Quiet respiration
Effortless and automatic breathing while at rest
Forced respiration
Deep or rapid breathing during an activity
Diaphragm
The prime mover of respiration; contraction flattens this muscle to enlarge the thoracic cavity and pull air in
Intercostal muscles
Muscles located between the ribs (costals) that contribute to thoracic contraction and enlargement
Accessory muscles
Muscle like the erector spinae, sternocleidomastoid, scalenes, pectoralis, and serratus that act during forced respiration, deep inspiration
Valsava maneuver
Breathing technique used to help expel contents of the abdomen
Central chemoreceptors
Brainstem neurons that respond to cerebrospinal fluid pH changes which reflect CO2 levels for respiration stability
Peripheral chemoreceptors
Receptors in the carotid and aortic bodies that respond to pH, gas content of blood
Stretch receptors
Receptors in the bronchi, bronchioles, and visceral pleura that regulate and respond to inflation
Inflation reflex (Hering-Breuer reflex)
Reflex triggered by excessive inflation that inhibits inspiratory neurons and stops inspiration
Irritant receptors
Nerves that respond to external irritants such as smoke or dust to cause reflexes like bronchoconstriction, shallow berathing, apnea, or coughing
Atmospheric pressure
The weight of the air on Earth; lower at higher elevations
Intrapulmonary pressure
Air pressure within the lungs
Boyle’s law
At a constant temperature, the pressure of a gas is inversely proportional to volume
More lung volume results in lower pressure; less lung volume results in higher pressure
Intrapleural pressure
The slightly negative pressure between the two pleural layers to allow for expansion
Charles’s law
At a constant pressure, the volume of a gas is directly proportional to temperature
Higher air temperatures expand the lungs further as it is warmed
Pneumothorax
The presence of air in the pleural cavity where the thoracic wall is punctured and negative intrapleural pressure is loss, allowing lung collapse
Atelectasis
The collapse of part or all of a lung that can also result from airway obstruction or clots
Bronchodilation
The increase in diameter of a bronchus or bronchiole for increased airflow; can be caused by epinephrine or sympathetic stimulation
Bronchoconstriction
The decrease in diameter of a bronchus or bronchiole for decreased airflow; caused by histamine, cold air, chemicals, or parasympathetic nerves
Pulmonary compliance
The ease with which the lungs can expand given a change in pressure for lung volume
Alveolar ventilation rate
The amount of air ventilating alveoli per minute
Spirometry
Measuing pulmonary ventilation to assess disease severity
Spirometer
Device used to make spirometry measurements to recapture breath and record breathing variables
Tidal volume (TV)
The volume of air inhaled and exhaled in one cycle of breathing
Inspiratory reserve volume (IRV)
Air in excess of tidal volume that can be inhaled with maximum effort
Expiratory reserve volume (ERV)
Air in excess of tidal volume that can be exhaled with maximum effort
Residual volume
Air remaining in lungs that cannot be exhaled even with maximum effort; allows some gas exchange before next breath of fresh air arrives
Vital capacity
Total amount of air that can be inhaled then exhaled with maximum effort
Inspiratory capacity
Maximum amount of air that can be inhaled after a normal tidal expiration
Functional residual capacity
Amount of air remaining in lungs after a normal tidal expiration
Total lung capacity
Maximum amount of air the lungs can contain
Restrictive disorders
Disorders that result in a reduction in pulmonary compliance (inflation); includes black lung disease and tuberculosis
Obstructive disorders
Disorders that interfere with airflow through airway obstruction; makes inhalation or exhalation more difficult and includes asthma and chronic bronchitis
Emphysema
Disorder commonly caused by smoking that combines elements of restrictive and obstructive disorders
Air composition
78.6% N
20.9% O2
0.04% CO2
trace amounts of Ar, Ne, He, CH4, O3
Dalton’s law
The total atmospheric pressure is the sum of the contributions of the individual gases
Partial pressure
The separate contribution of each gas to pressure in a mixture
Alveolar gas exchange
The movement of O2 and CO2 across the respiratory membrane, using a film of water to cover the epithelium to dissolve oxygen and diffuse carbon dioxide
Hyperbaric oxygen therapy
Treatment with oxygen at greater than 1 atmosphere of pressure to allow more diffusion into the blood; used to treat gangrene and CO poisoning