General Anesthetics
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
What is general anesthesia?
Controlled, reversible state of loss of sensation and conciousess
What is analgesia
Decrease awareness of pain
Stages of general anesthesia
I. Analgesia
II. Disinhibition/Excitement
III. Surgical Anesthesia (GOAL)
IV. Medullary Depression: we do not want our patients to reach this stage
What is the goal in general anesthesia?
III. Surgical Anesthesia
Unconscious, no pain reflexes
Blood pressure and respiration are regular
Monitor: Reflexes, vital signs, EEG, respiratory and circulatory responses to surgical stimulation
Examples of inhaled anesthetics
Gas: Nitric Oxide
Volatile Liquids: Isoflurane, Desflurane, Sevoflurane, Enflurane, Methoxyflurane, Halothane
IV anesthetics examples
Barbiturates: Thiopental, Methohexital
Benzodiazepines: Diazepam, lorazepam, midazolam
Propofol, Etomidate, Ketamine ← different MOAs
Opioids: Morphine, fentanyl, sufentanil, alfentanil, remifentanil
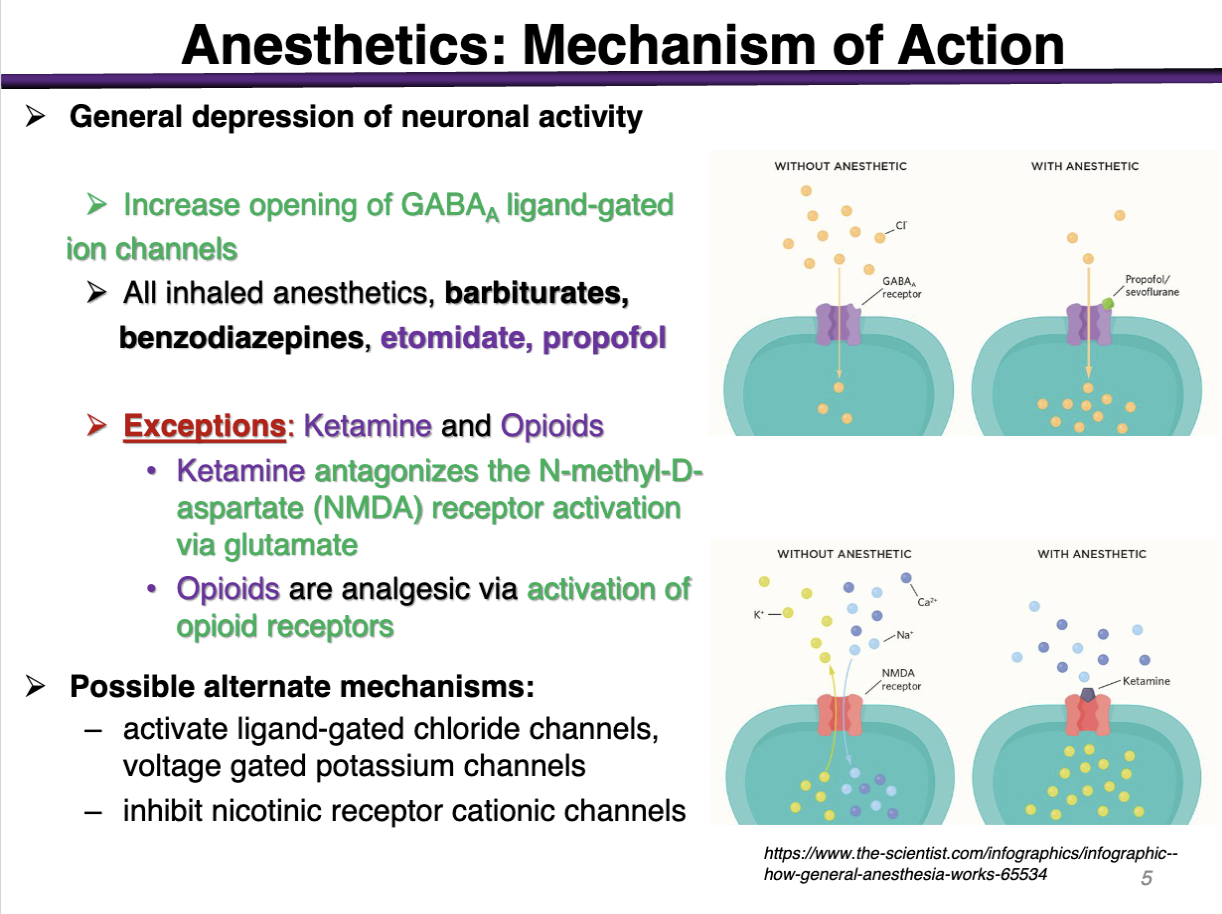
Anesthetics Goal
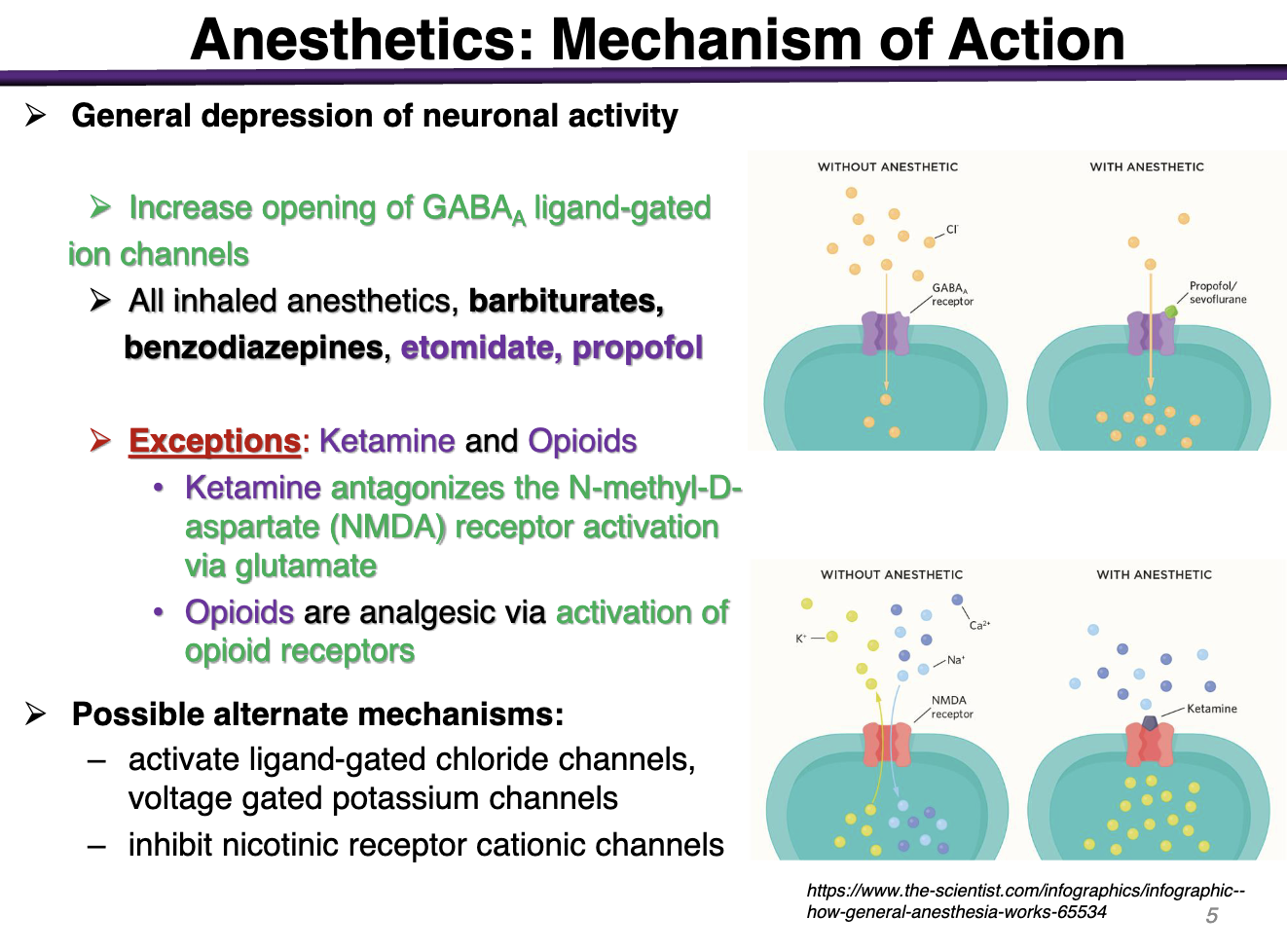
General depression of neuronal activity
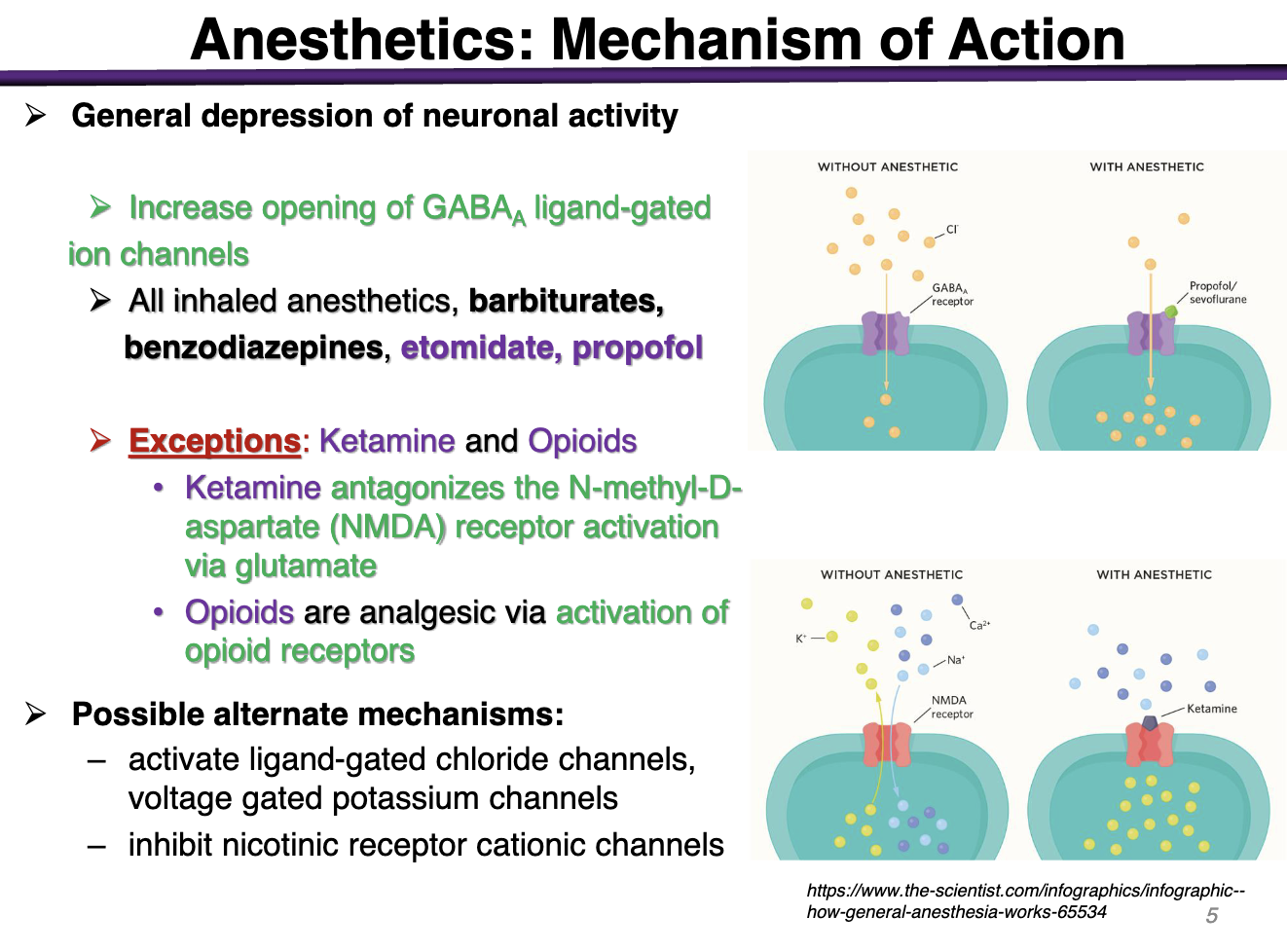
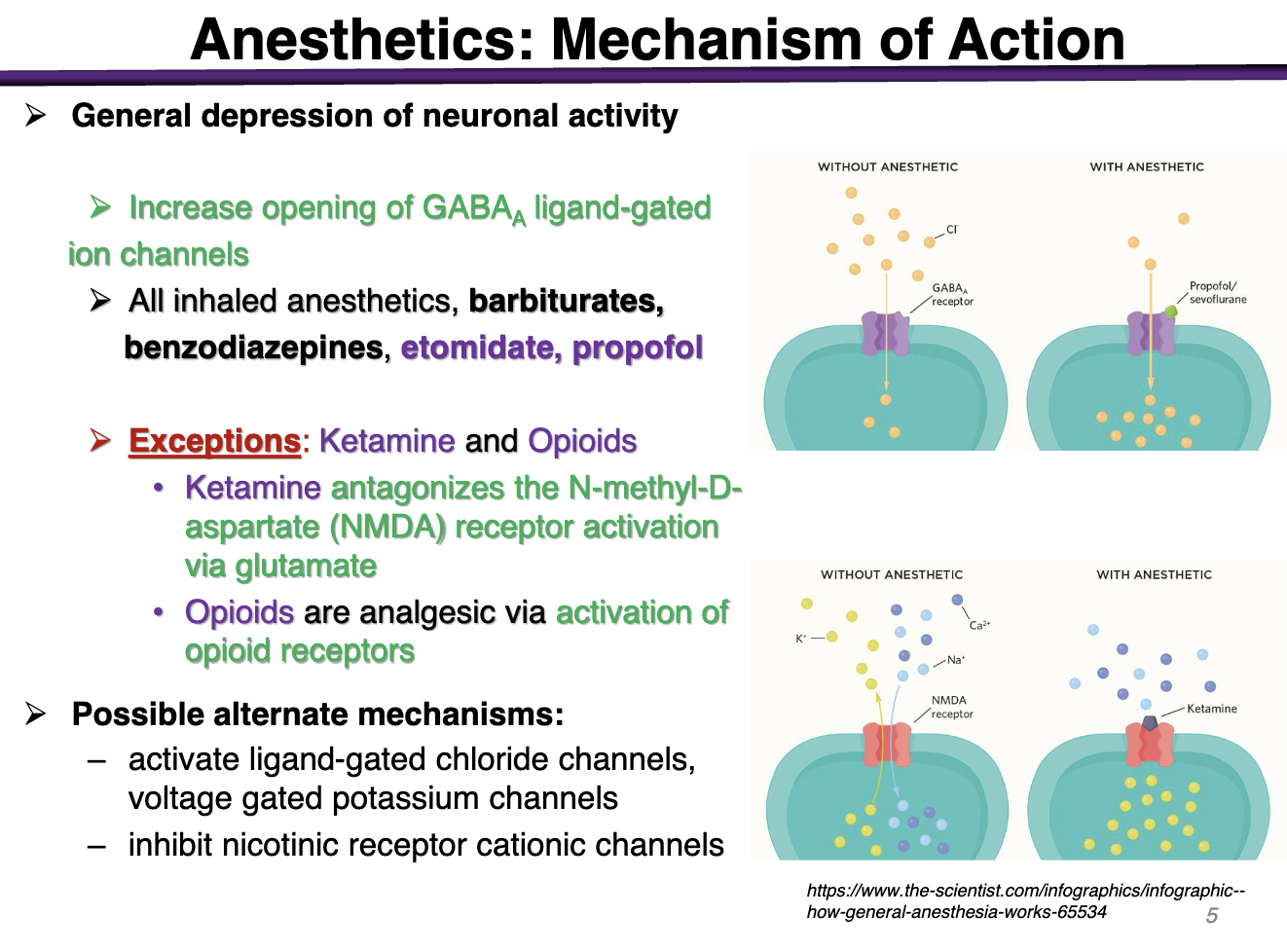
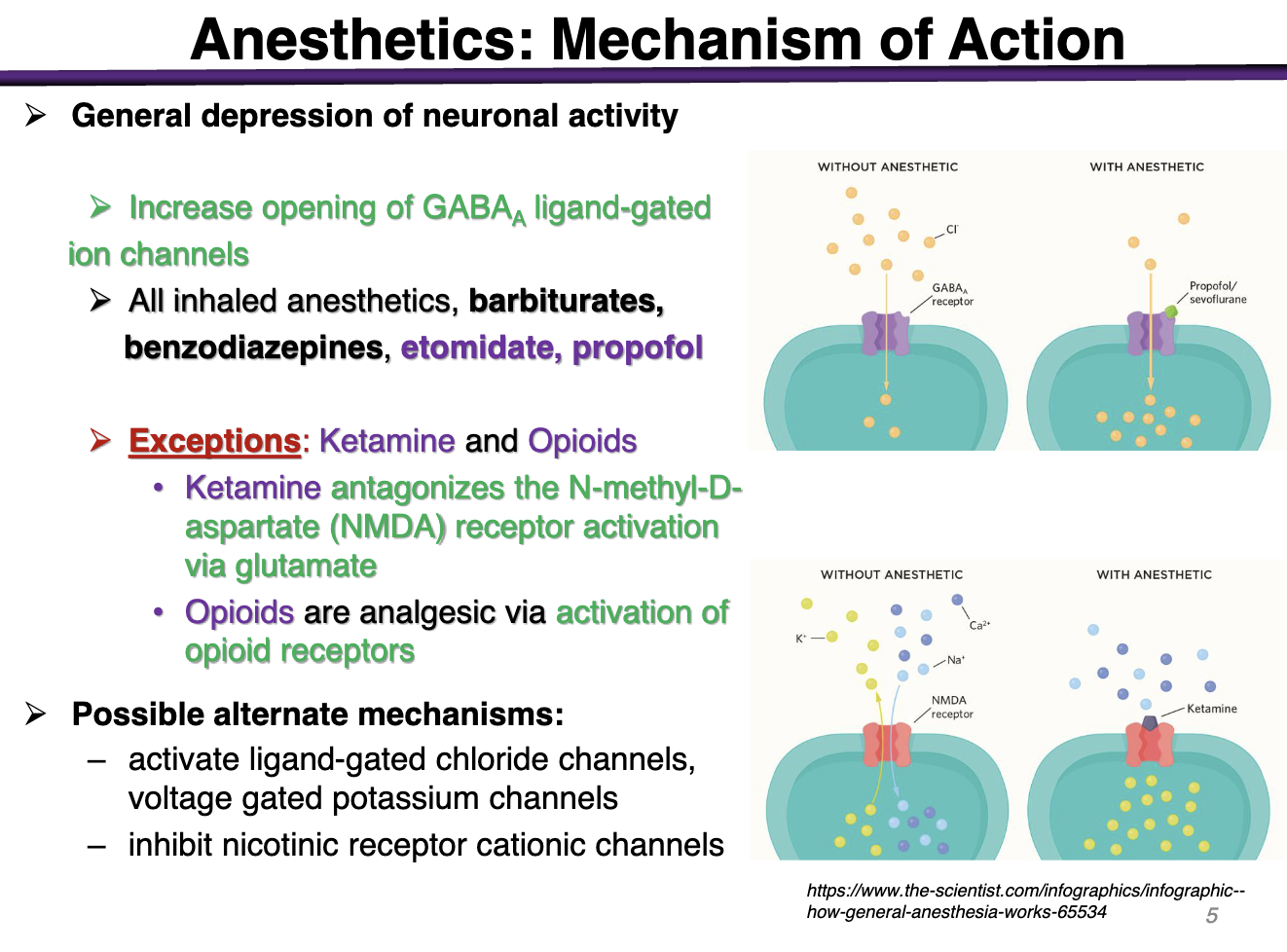
Anesthetics MOA
Increase opening of GABAa ligand-gated ion channels
All inhaled anesthetics, barbiturates, benzodiazepines, etomidate, propofol
Exceptions: Ketamine and Opioids
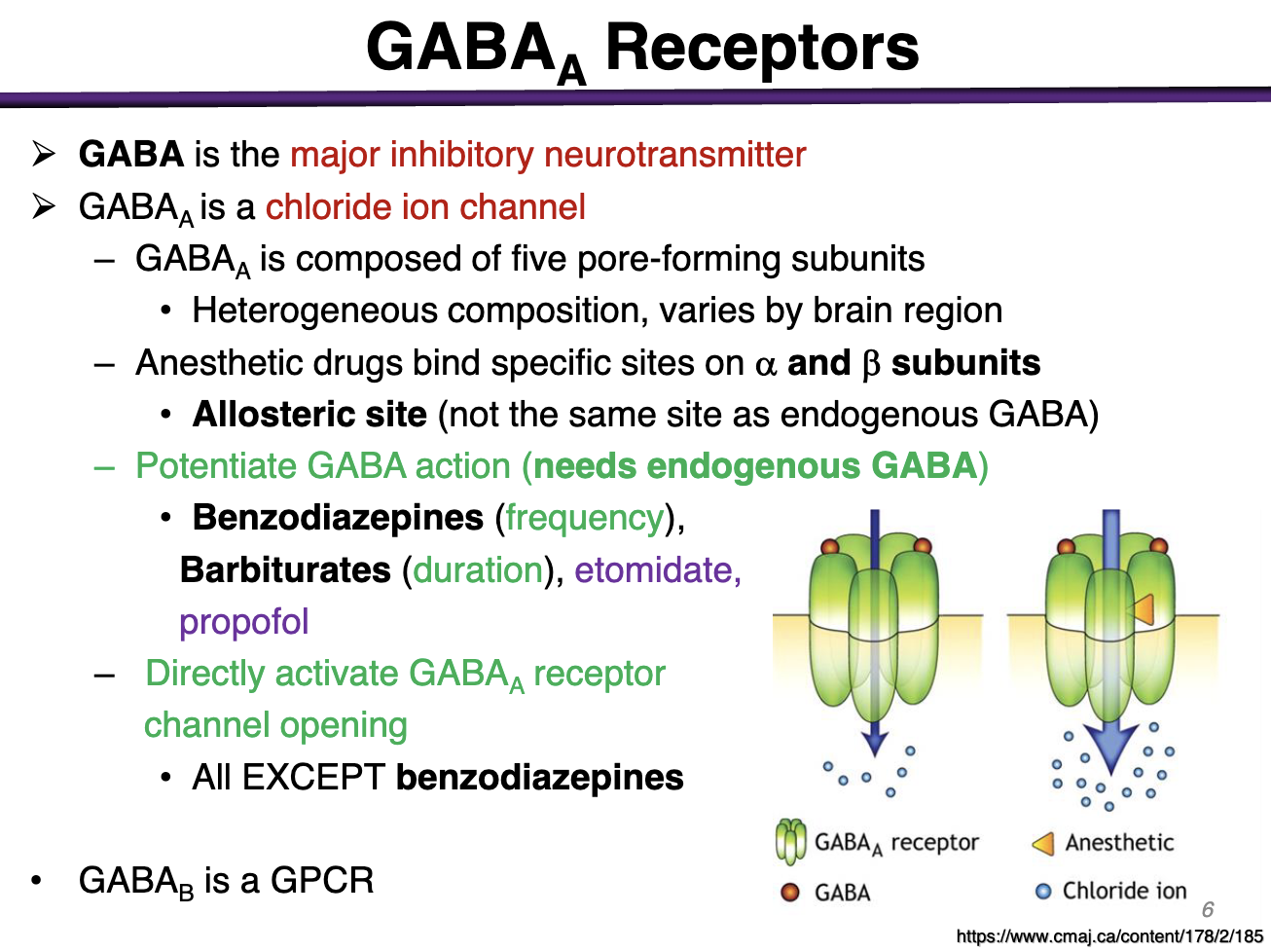
What type of channel is GABAa
Ligand-gated ion channel
Influx of Cl- causes hyperpolarization → Inhibatory
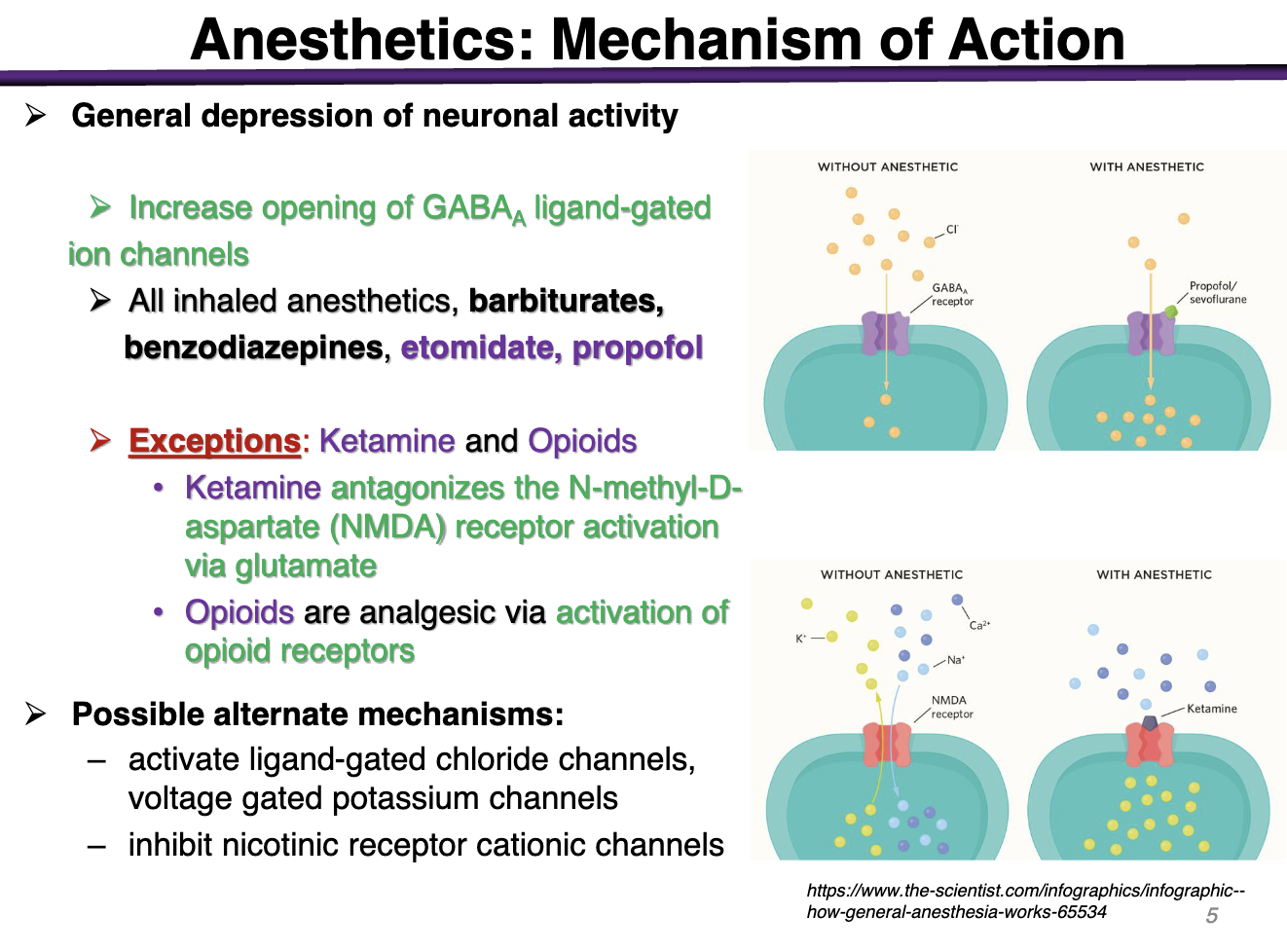
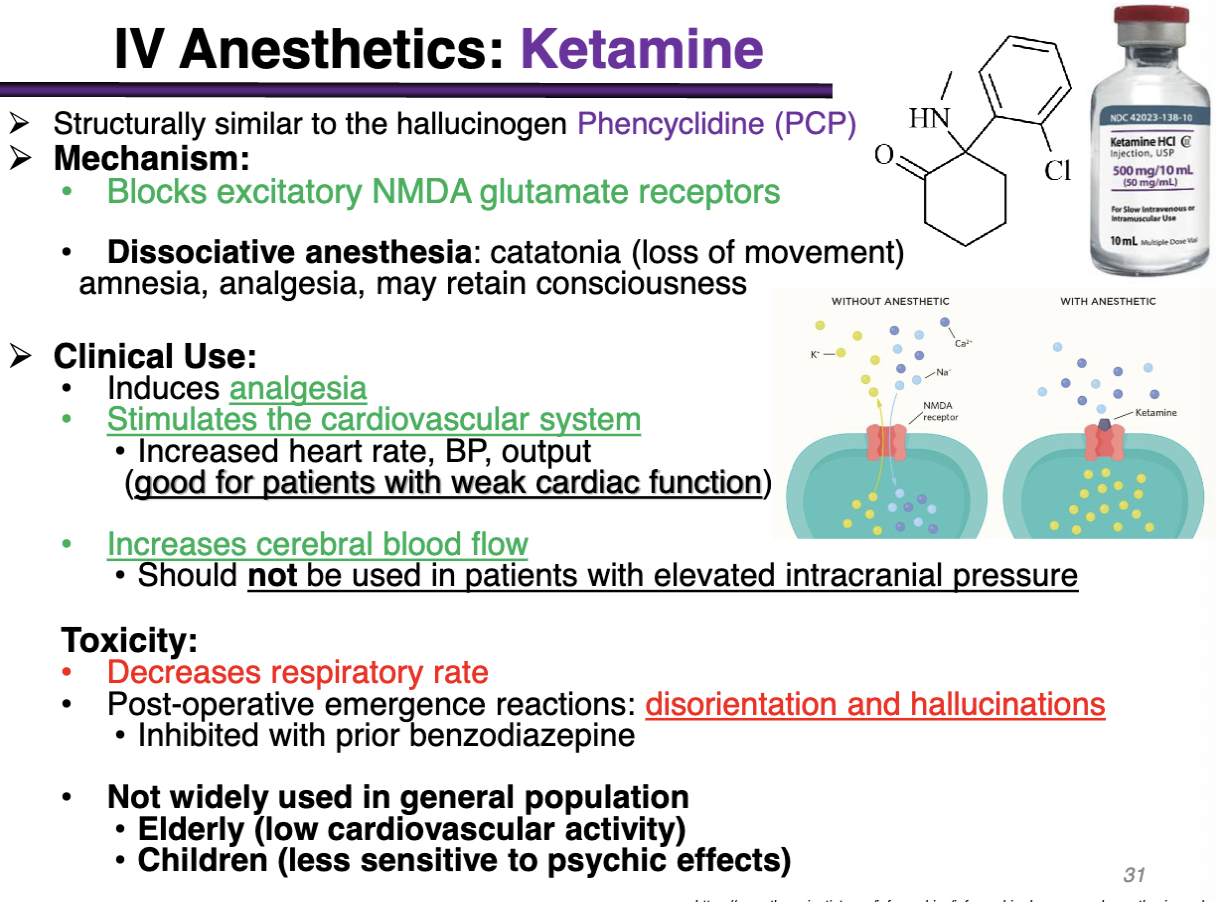
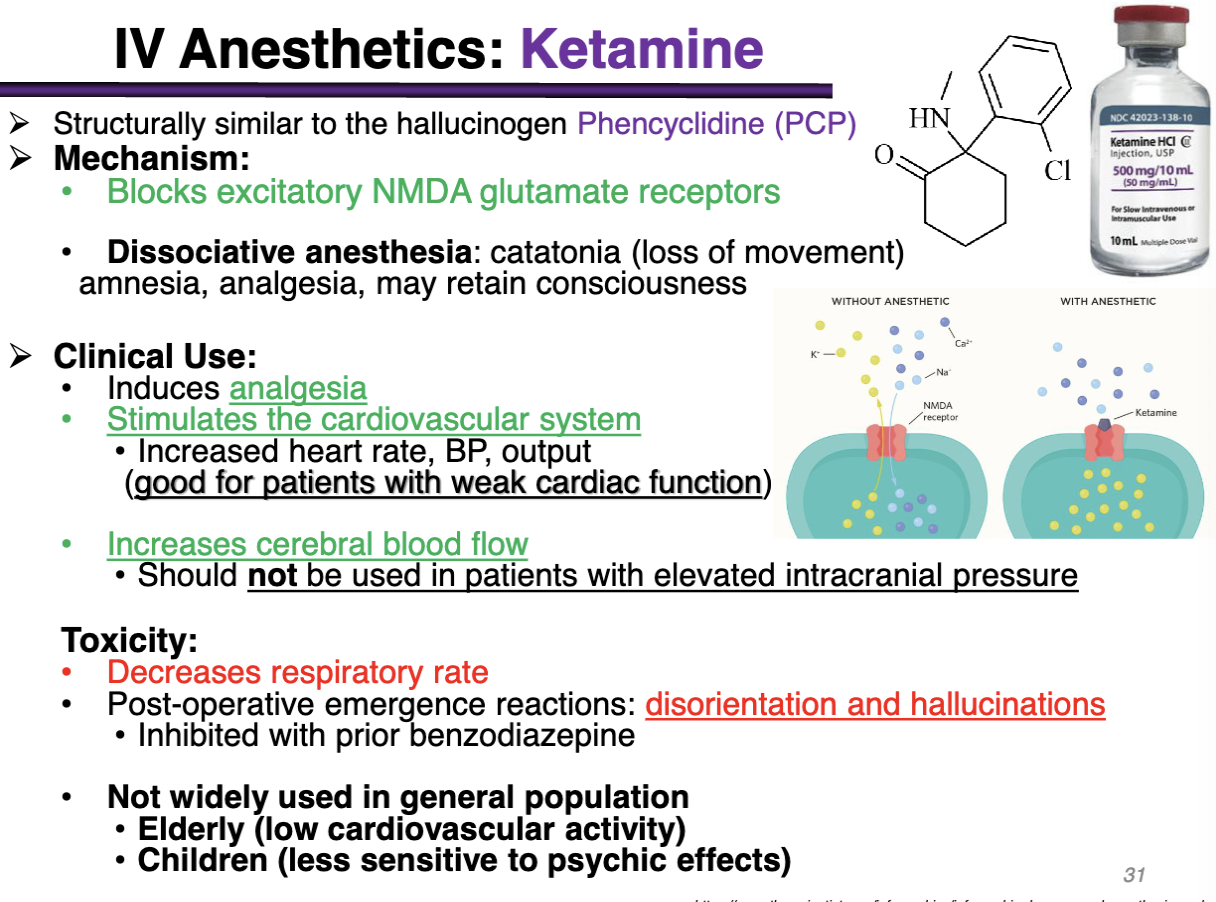
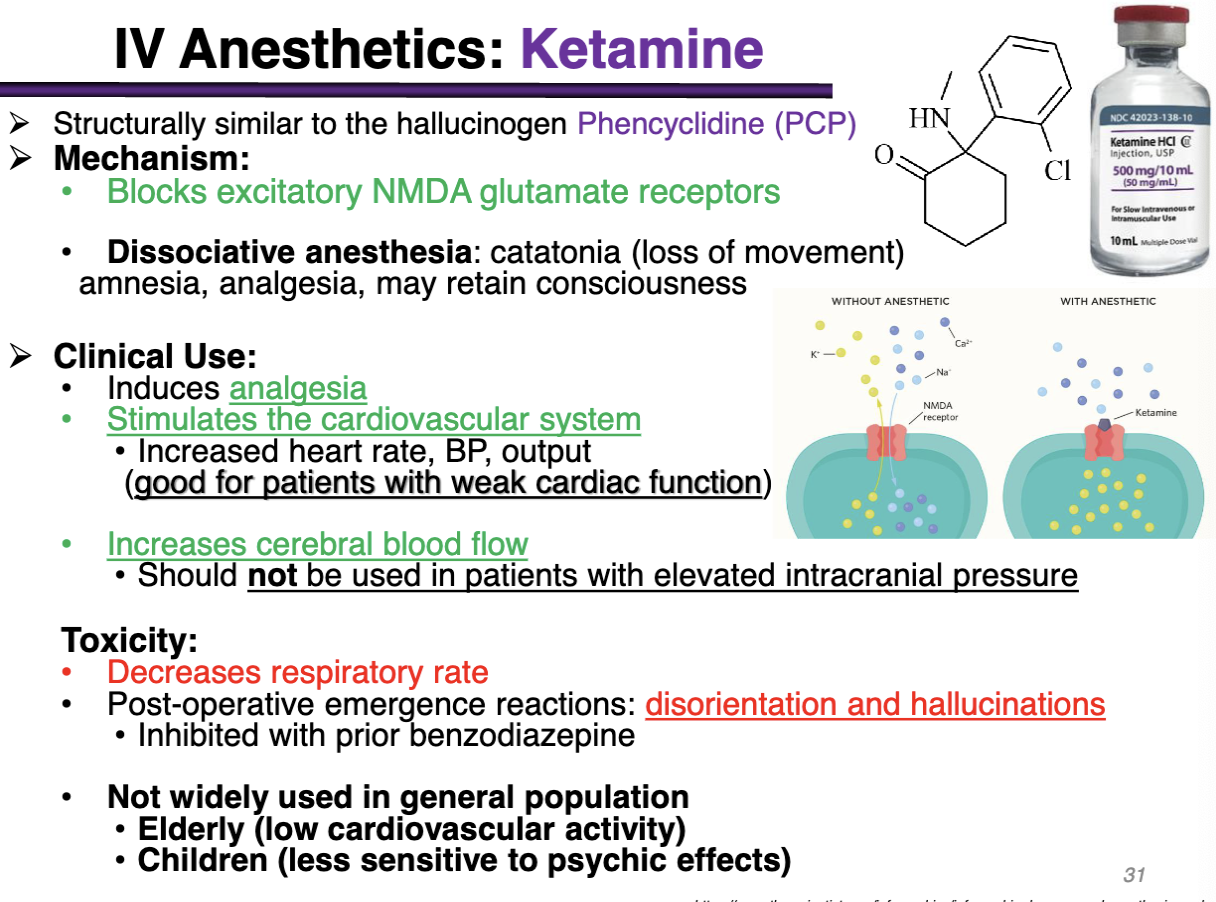
Ketamine MOA
Antagonizes the N-methyl-D-aspartate (NMDA) receptor activation of glutamate
Block receptor; Block Na from coming in, no depolarization occurs
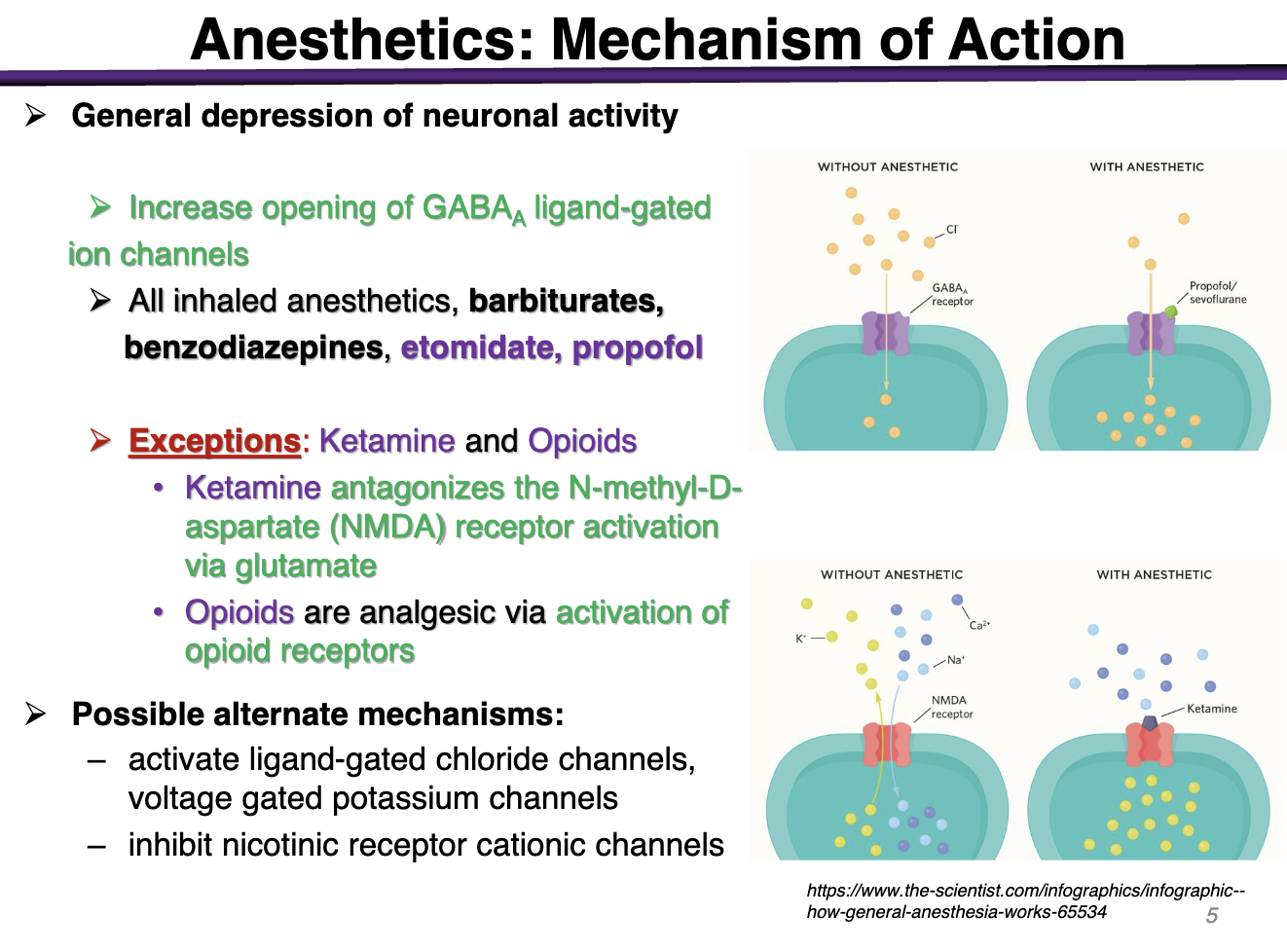
Opioids MOA
Activation of opioid g-protein receptors
Net effect is inhibitory
T/F Ketamine binds to GABA receptors to inhibit it
FALSE Ketamine antagonizes the N-methyl-D-aspartate NMDA receptor activation to inhibit glutamate
T/F GABA is the major excitatory NT in the brain
FALSE: GABA is a major inhibitory NT
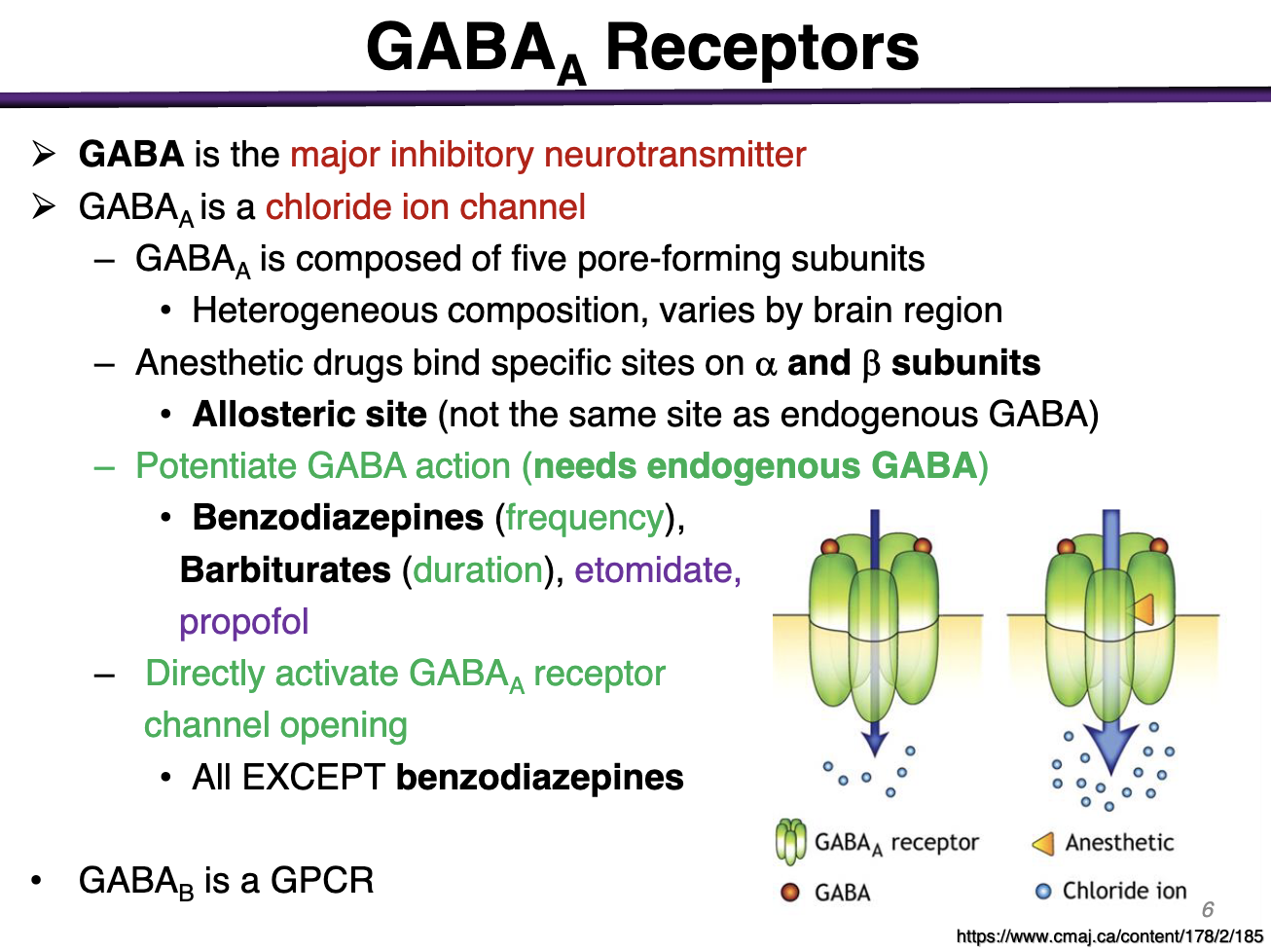
What kind of channel is GABAa
Chloride Ion Channel
Allows Cl to enter the cell and result in a hyperpolarization
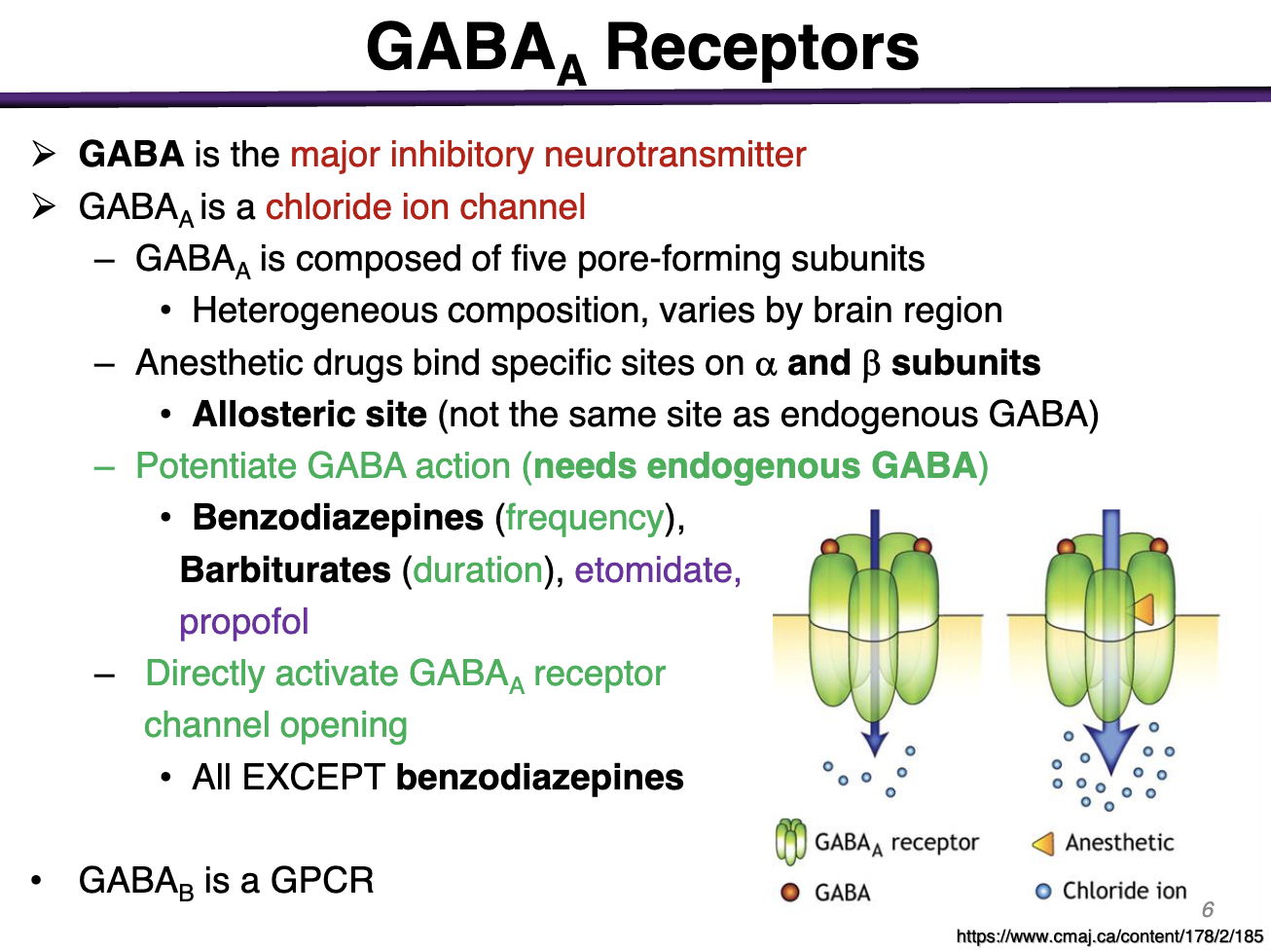
Where do anesthetic drugs bind to?
Anesthetic drugs bind to specific sites on a and b subunits on the allosteric site (NOT the same as endogenous GABA)
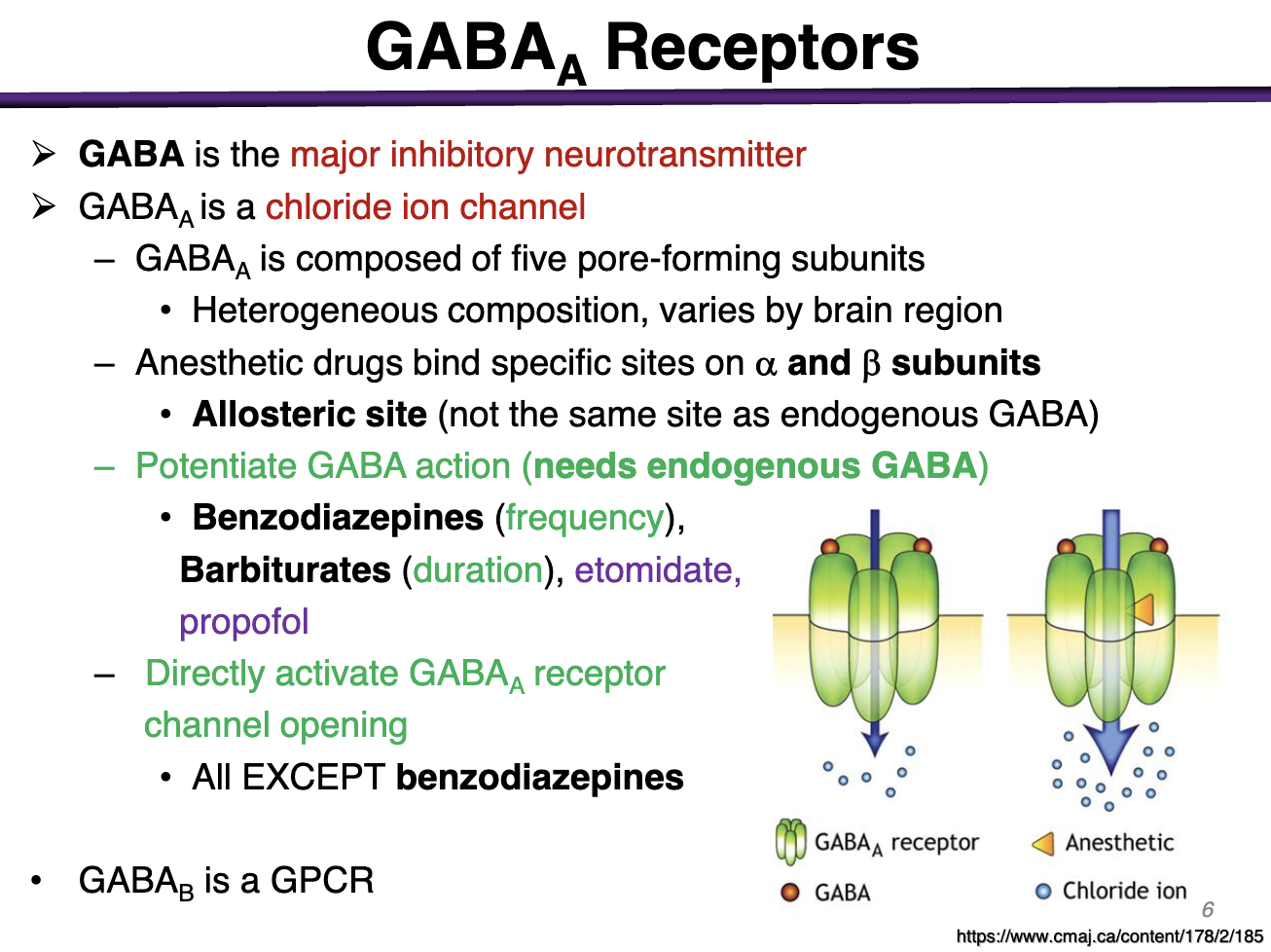
What drugs potentiate GABA action
These needs endogenous GABA
Benzodiazepines (increase frequency of channel opening) REQUIRE GABA regardless of concentrations
Barbiturates do not require at high doses (Duration; they make the channel open for longer) - etomidate, propofol
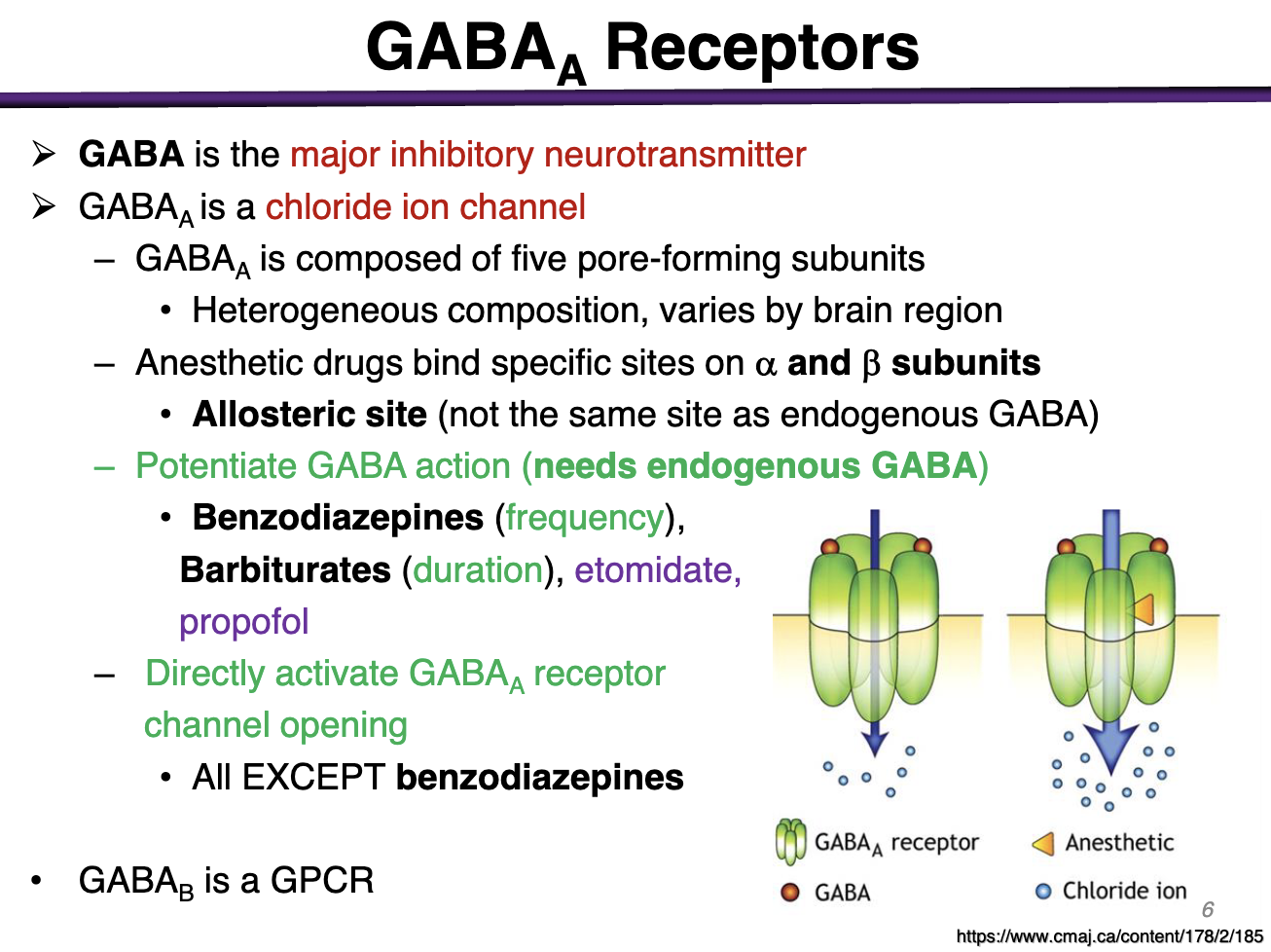
Major difference between benzodiazepines and barbiturates MOA
Benzodiazepines increase frequency via allosteric site
Barbiturates increase the duration. Examples include etomidate,propofol
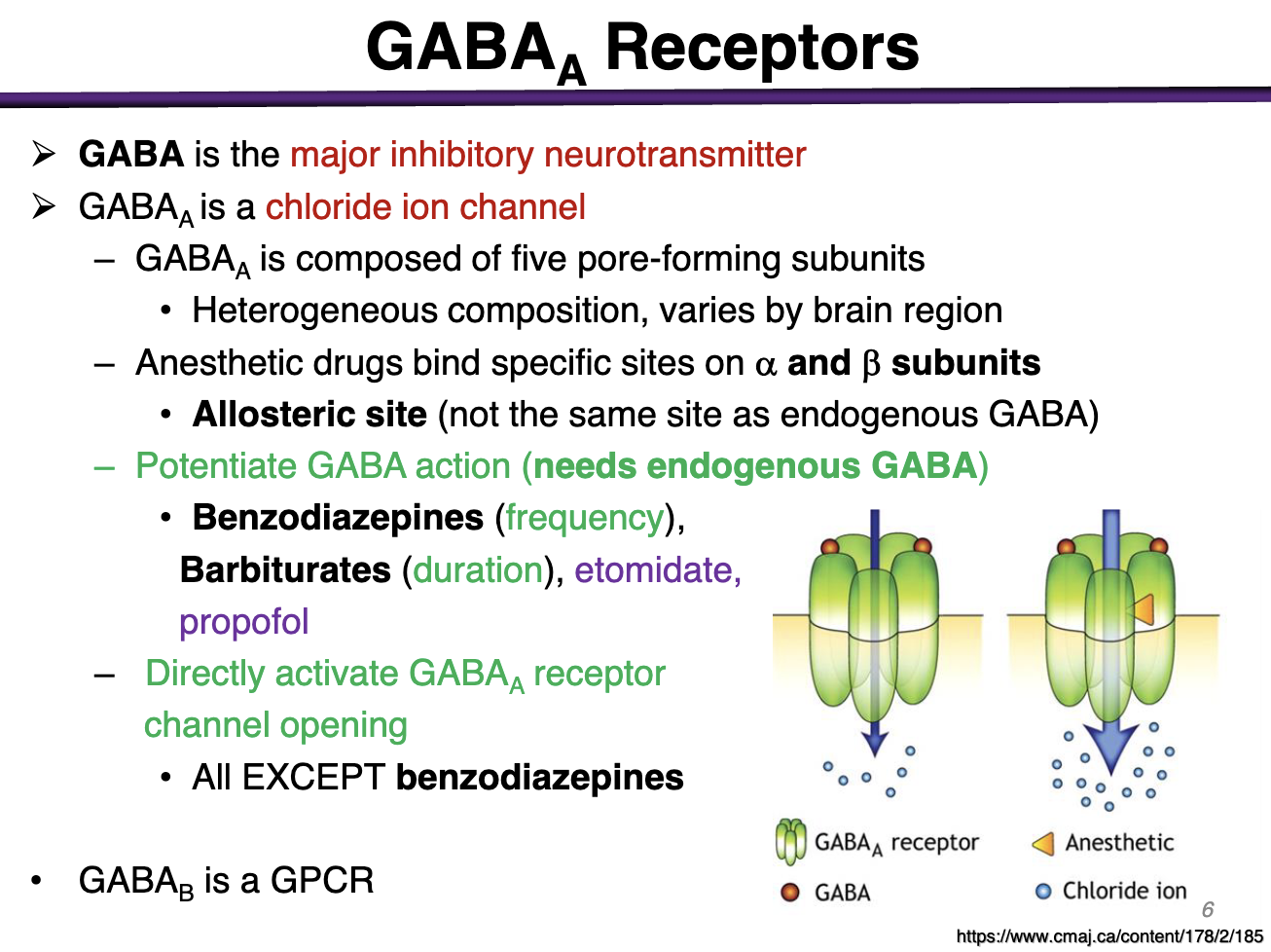
T/F All anesthetics directly activate GABAa receptor channel opening at high concentrations
All EXCEPT benzodiazepines
Benzodiazepines NEED GABA to work to bind to the allosteric site
For all others, at high concentrations, you may not need GABA to act at the allosteric site. Benzodiazepines cannot directly activate GABA at high concentrations
However regardless, all prefer to have GABA present at normal concentrations
How can we induce selective effects with anesthetics?
Neuronal pathways are differentially sensitive to anesthetics
Example: The dorsal horn neurons (pain) are the most sensitive
What are the first neurons that respond to anesthetic doses?
Dorsal horn neurons (pain) most sensitive
Stage I analgesia and conscious sedation
What is the least sensitive neuronal pathway?
Respiratory and vasomotor centers of medulla neurons: Least sensitive
Stage IV cardio-respiratory collapse
What explains the excitatory phase in Stage II
Small inhibitory neurons are inhibited
Thus these result in effects in Stage II:
II.Disinhibition/Excitement
• Delirious, amnesia, enhanced reflexes
• Irregular respiration
• Vomiting, incontinence
What neuronal pathways explain step III?
We want to quickly achieve stage 3 while also keeping them at stage 3
Ascending pathways of reticular activating system: mediate sleep/awake cycle, spinal reflex activity
Stage III: Loss of consciousness and muscle relaxation
Surgical Anesthesia
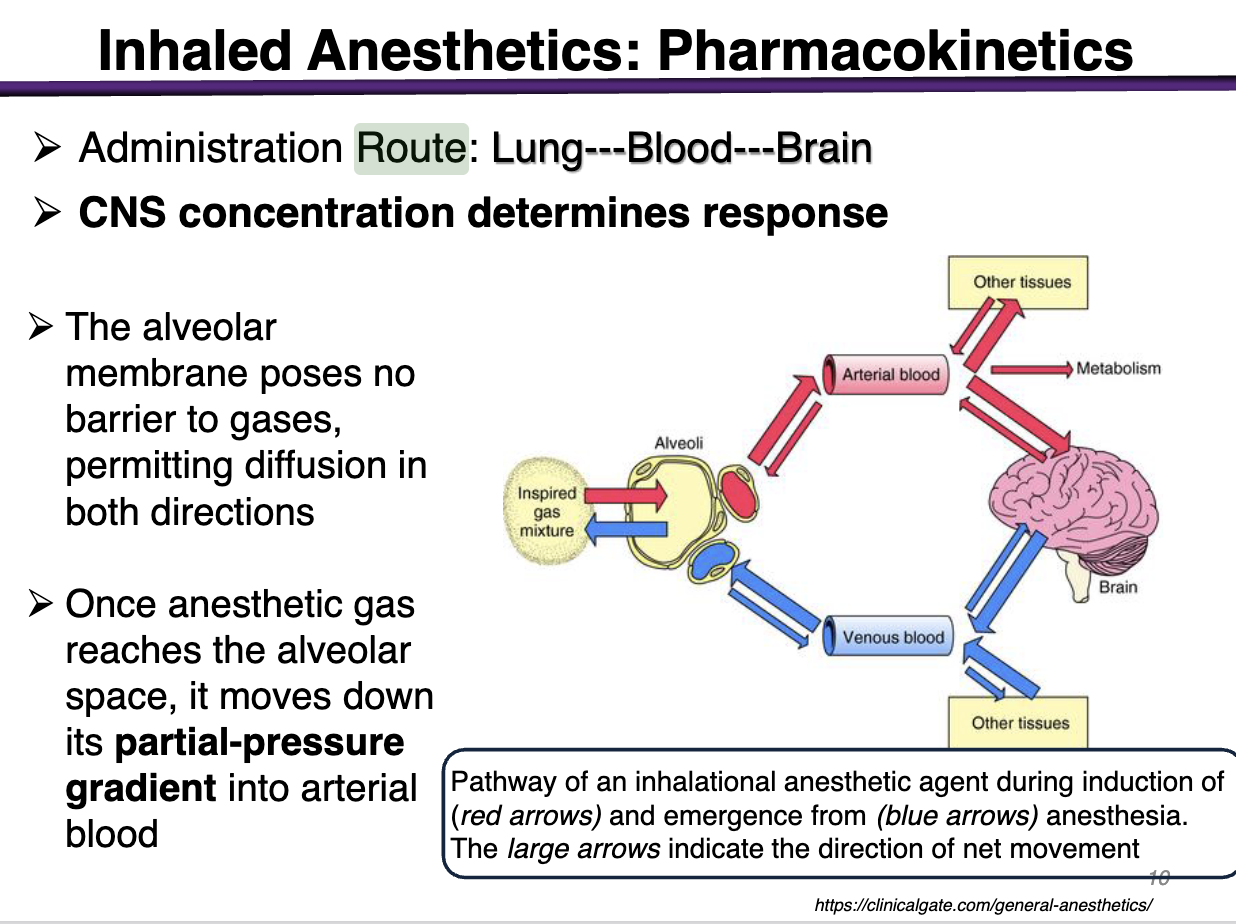
Administration Route
lungs — blood — brain
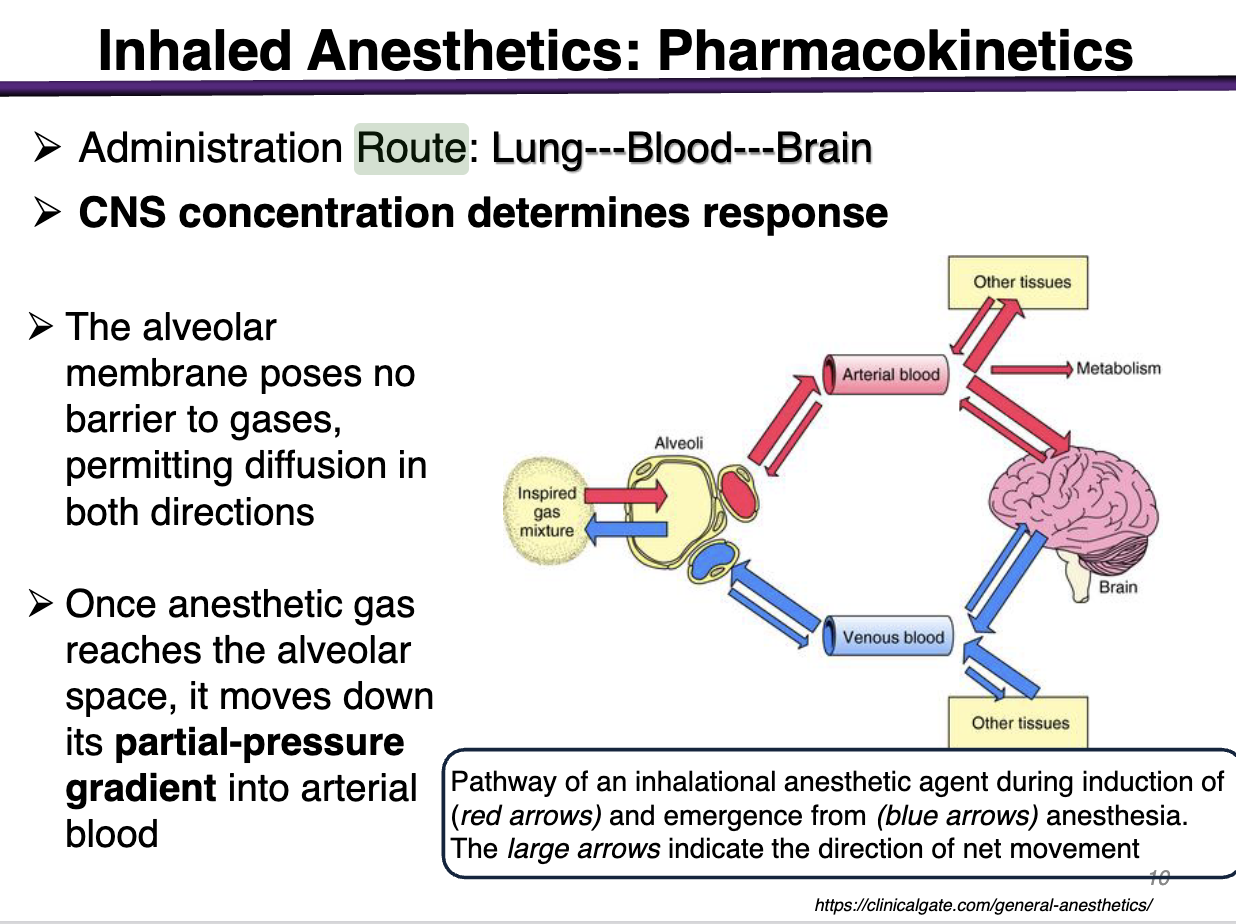
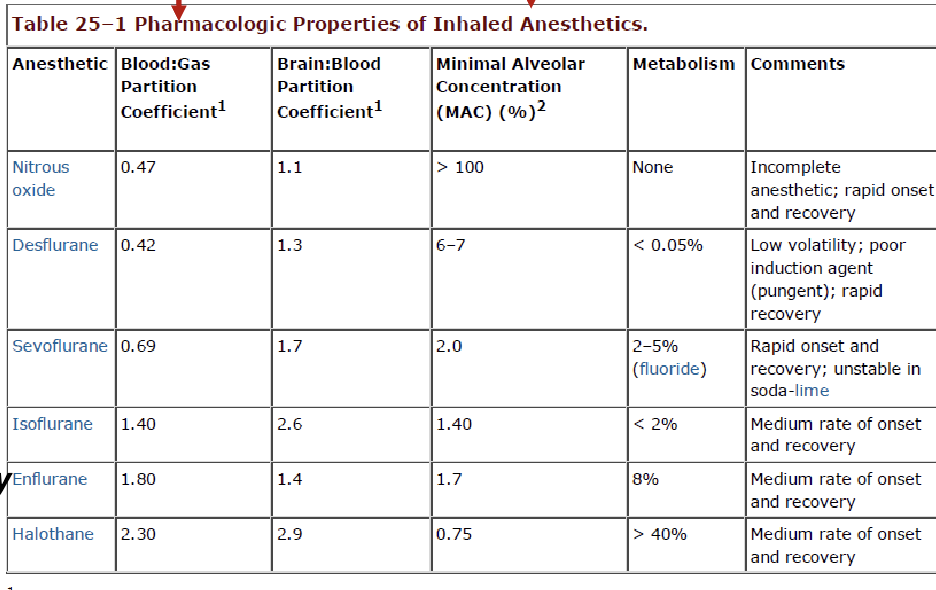
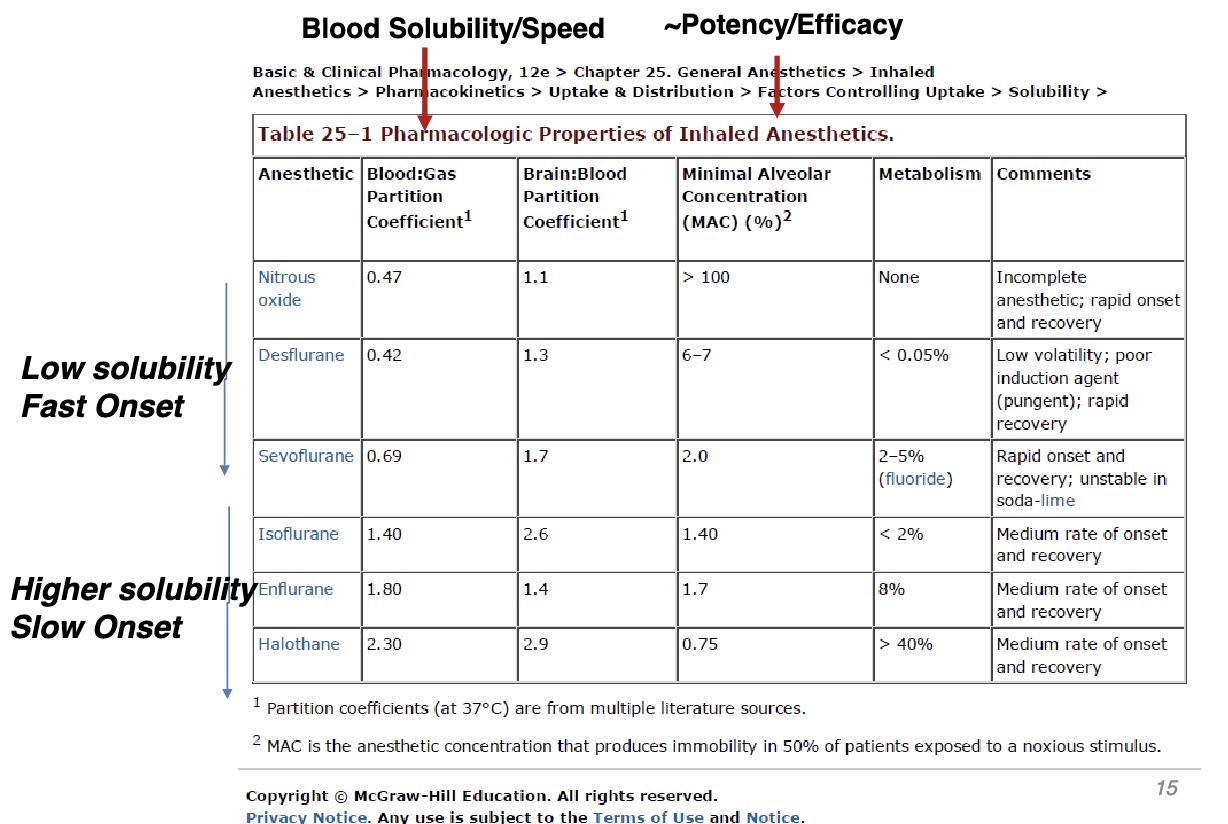
What determines response for inhaled anesthetics?
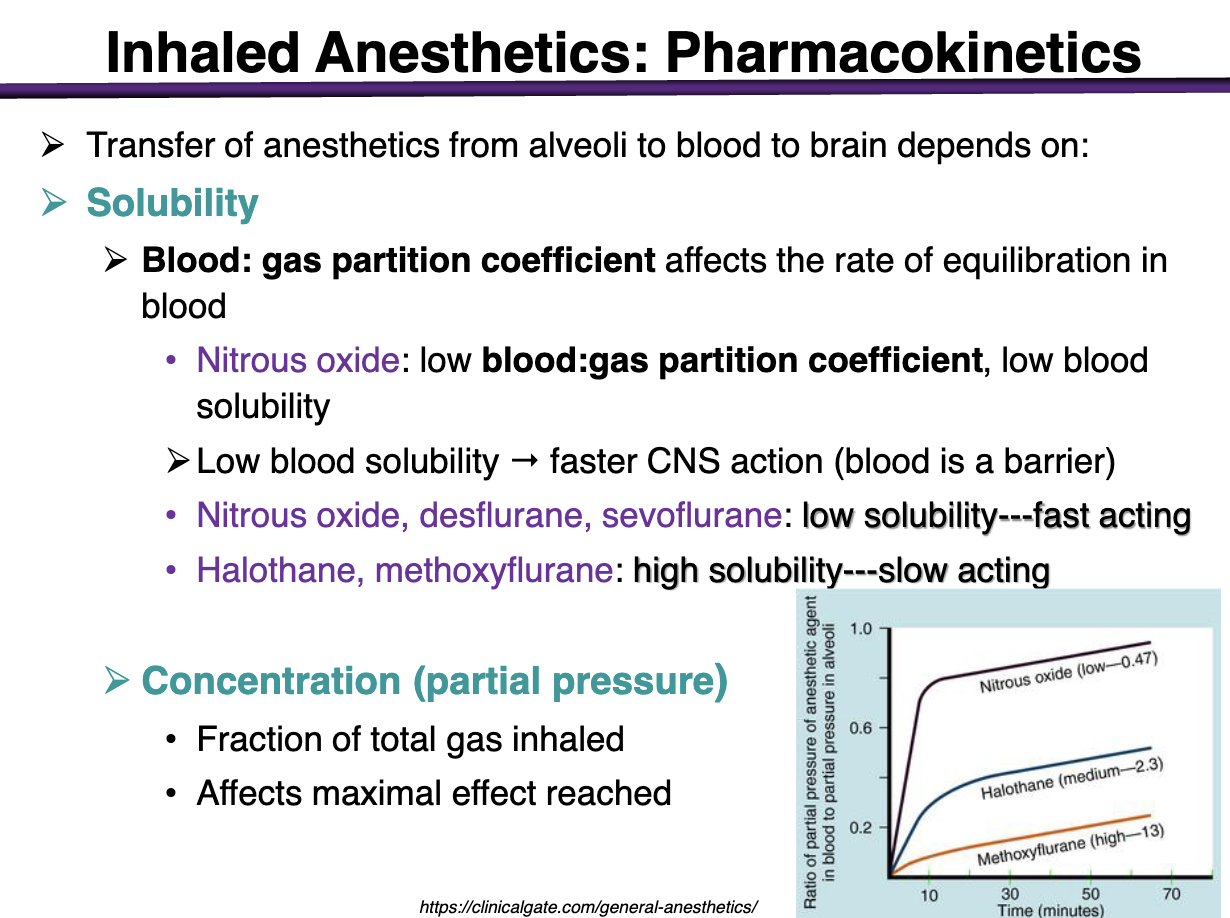
CNS Concentration determines response
low gas partition coefficient
Affects the rate of equilibration in blood
low:gas partition coefficient = low solubility in the blood
this means that a drug with a low blood:gas partition coefficient leads to FASTER CNS action (prefers the gaseous form; blood is a barrier)
If it is not soluble (low) it wants to get our of the blood into the brain for more CNS effect
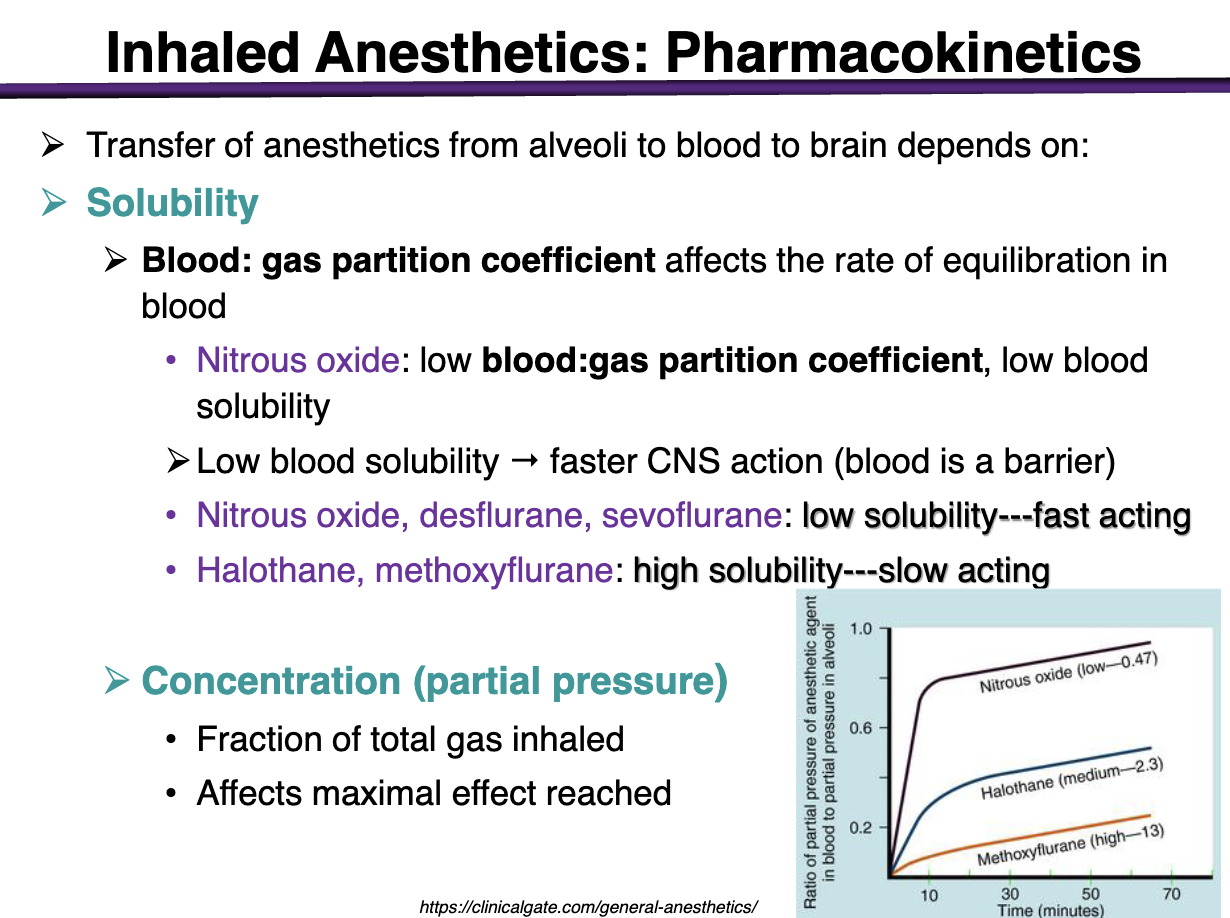
onet of action for nitrous oxide
Low blood:gas partition coefficient
Low blood solubility
*remember, low blood solubility → faster CNS action
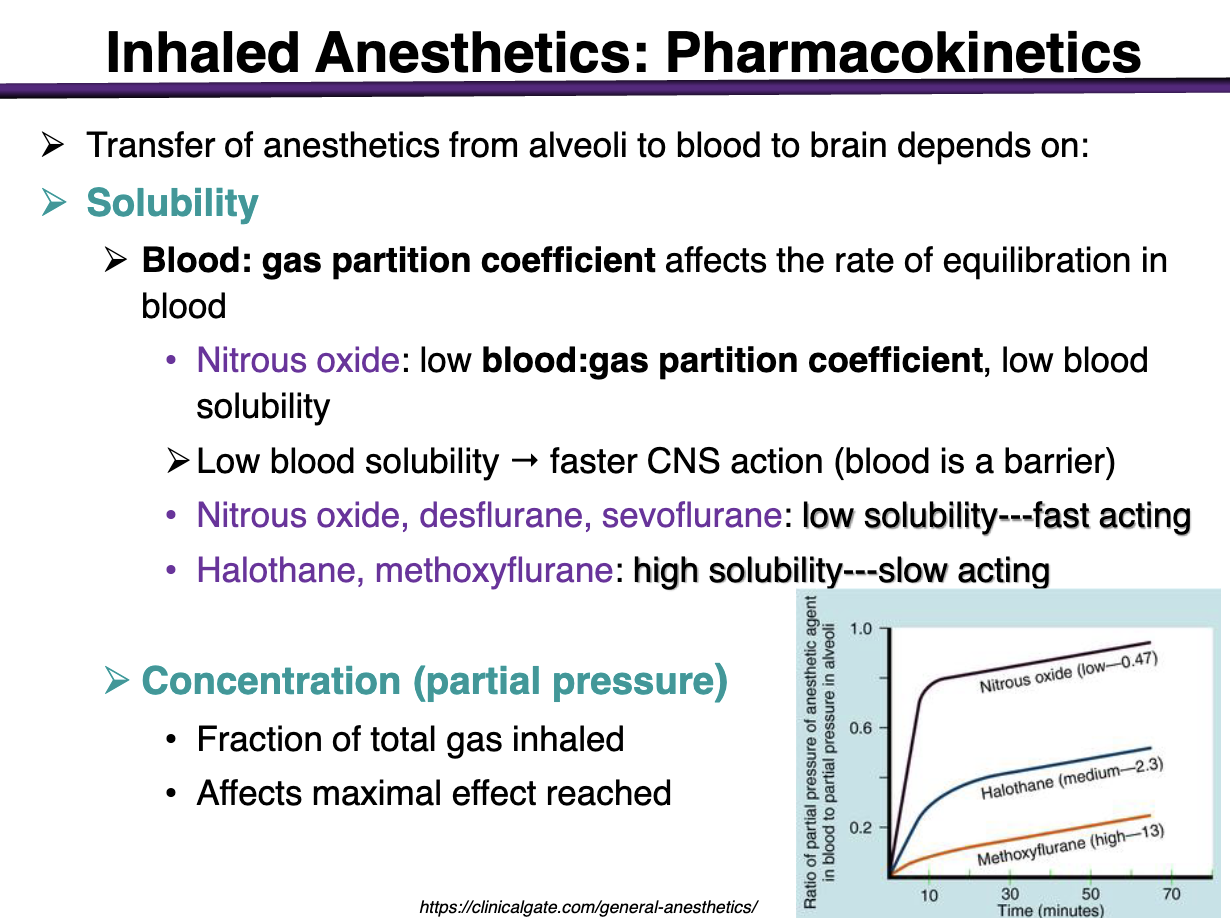
characteristics of nitrous oxide, desflurane, sevoflurane: blood solubility
Low solubility → fast acting
Low blood = hate blood = more gas = more action in the brain
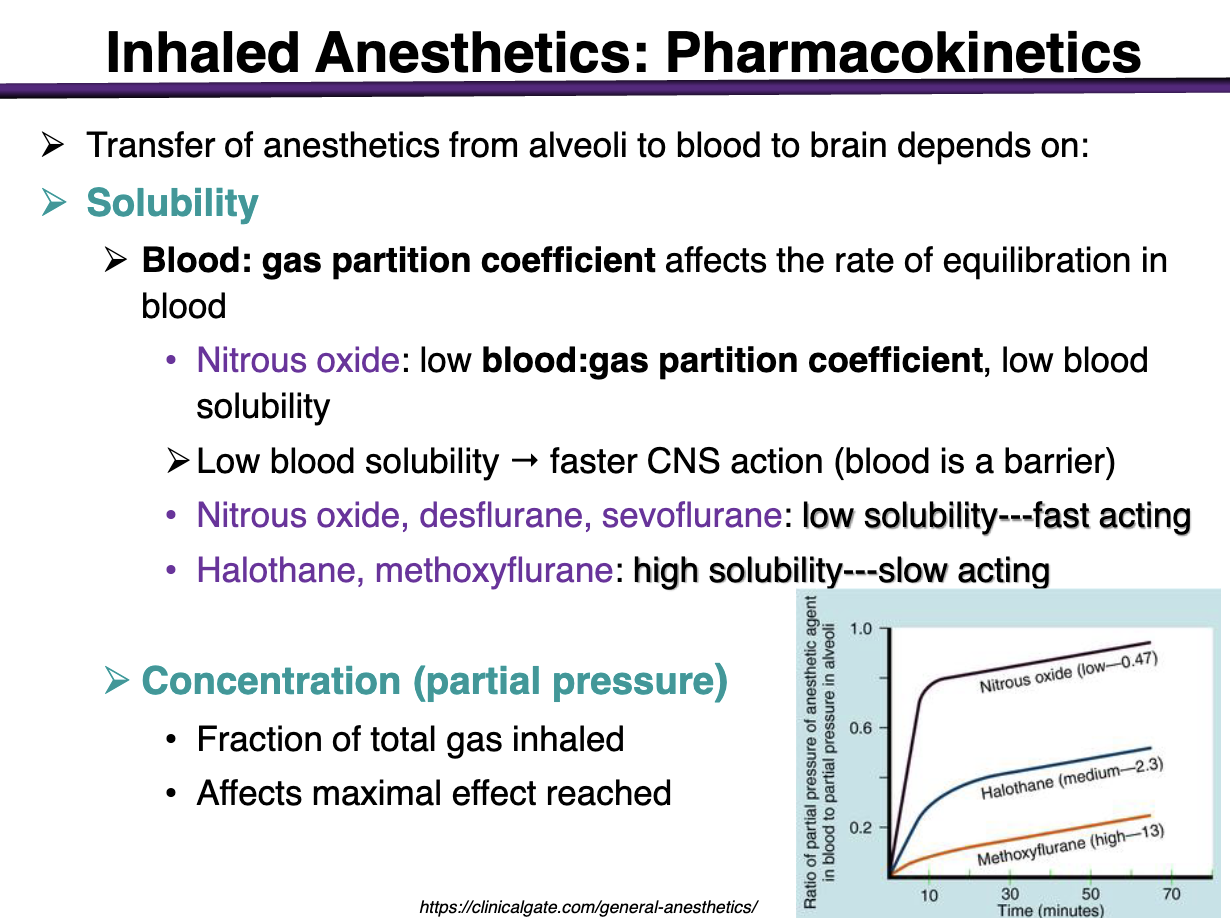
characteristics of halothane, methoxyflurane: blood solubility
High solubility → slow acting
Wants to stay in the blood → not gas → little CNS crossing
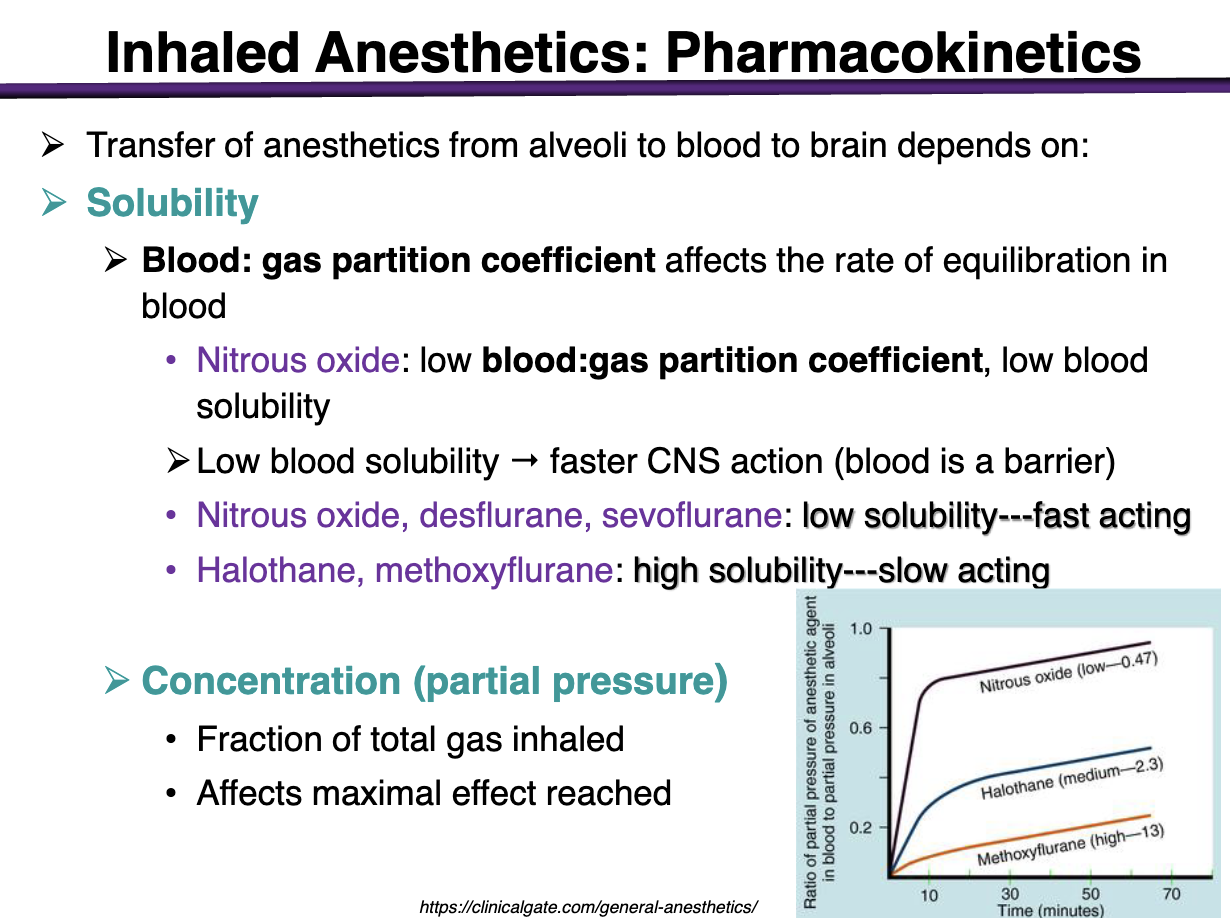
What is partial pressure
Fraction of total gas inhaled
Affects maximal effect reached
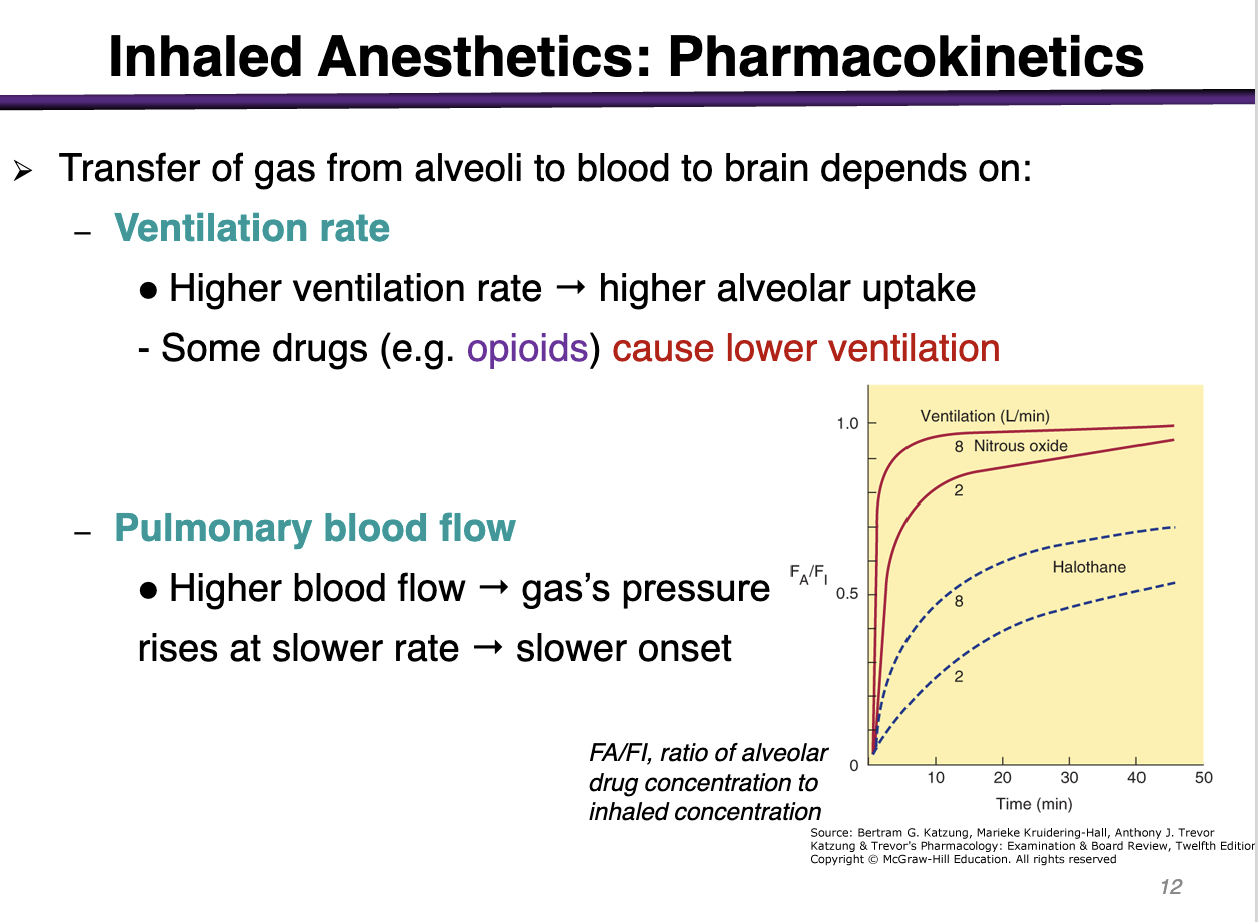
what does a higher ventilation rate translate to
higher alveolar uptake
Opioids cause lower ventilation
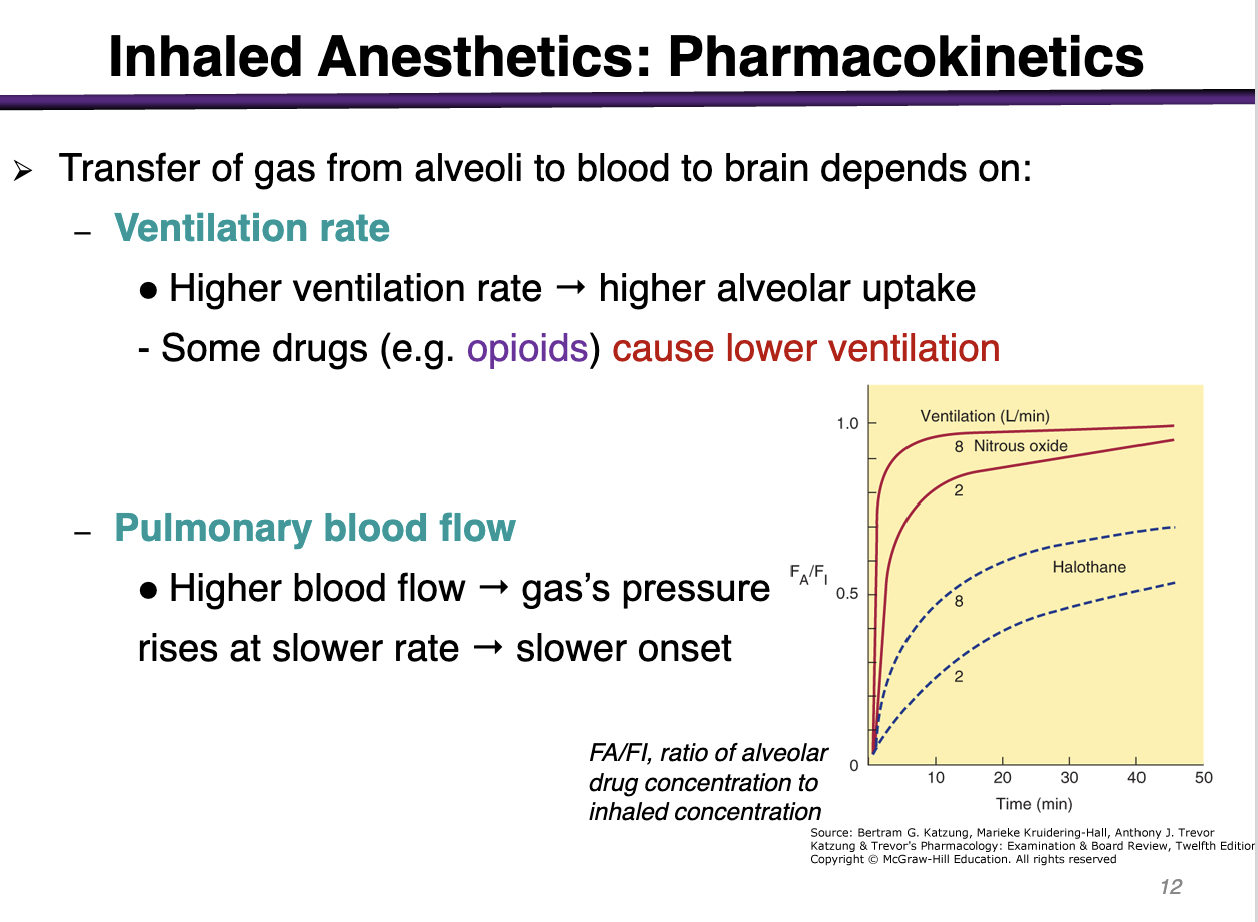
what does a higher pulmonary blood flow translate to
Higher blood flow → gas’s pressure rises at a slower rate → slower onset
the partial pressure of gas concentration (amount per volume) would take longer to increase and this can slow down the transfer of the anesthetic drug from the lungs into the blood → can slow the onset of action
how are halothane and methoxyflurane metabolized?
metabolized by the liver and produces hepato-toxic metabolites
how are isoflurane and desflurane metabolized?
liver enzymes
what is a major route of elimination for inhaled anesthetics?
clearance by lungs is the major route of elimination
the rate of recovery from anesthesia using agents with a ___ blood solubility is faster than that of anesthetics with a ___ blood solubility
The rate of recovery from anesthesia using agents with low blood solubility is faster than that of anesthetics with high blood solubility
Drugs with a low solubility are eliminated at a ___ rate
Drugs with a low solubility are eliminated at a fast rate
desflurane and sevoflurane have a shorter recovery time
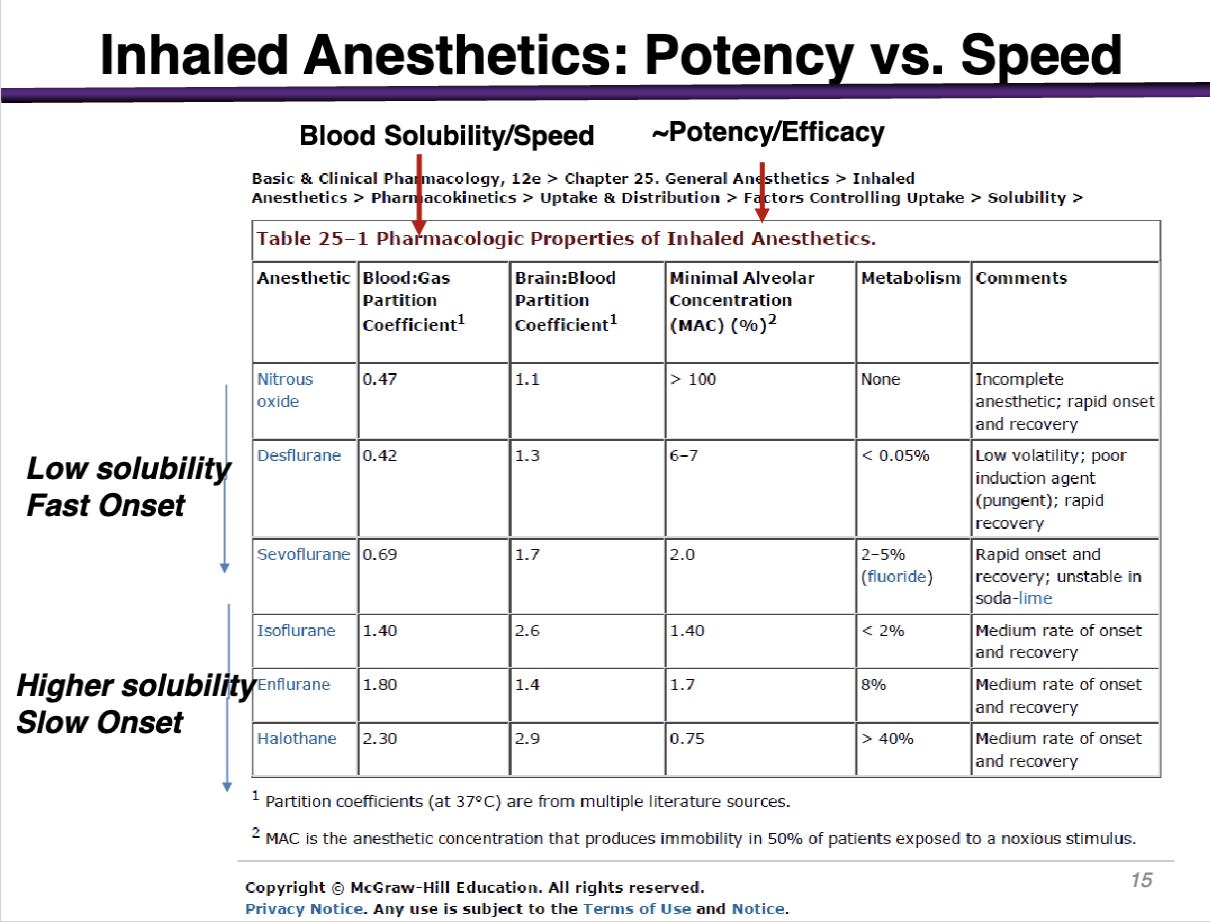
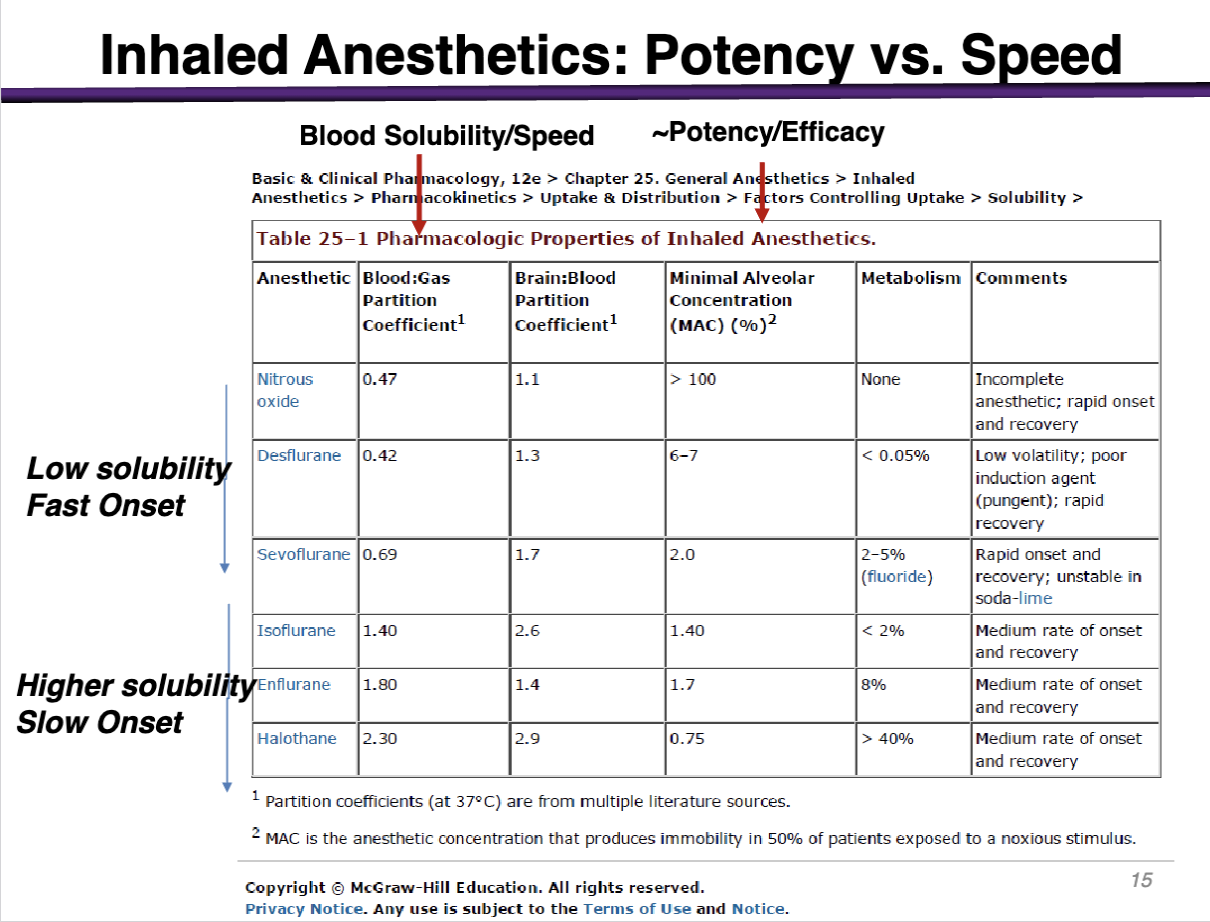
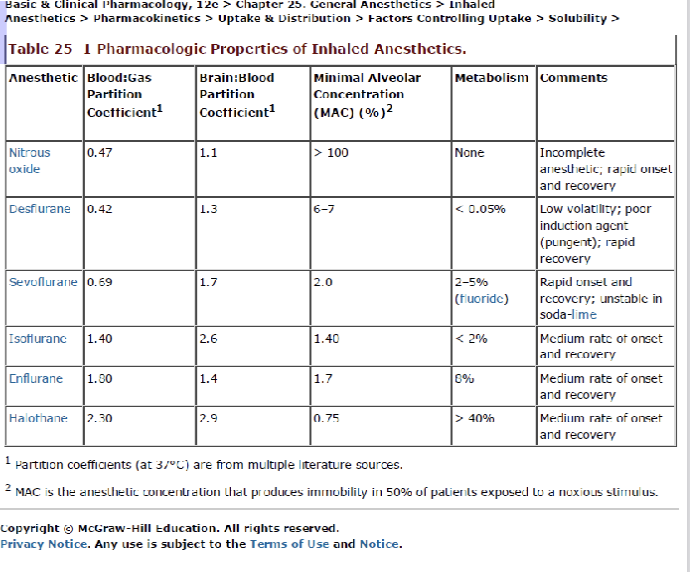
What is potency of inhaled anesthetics measured by?
Minimum alveolar anesthetic concentration (MAC) at which 50% of patients do not move in response to a standardized painful stimulus unit of anesthetic dose
50% of pts will not feel the pain
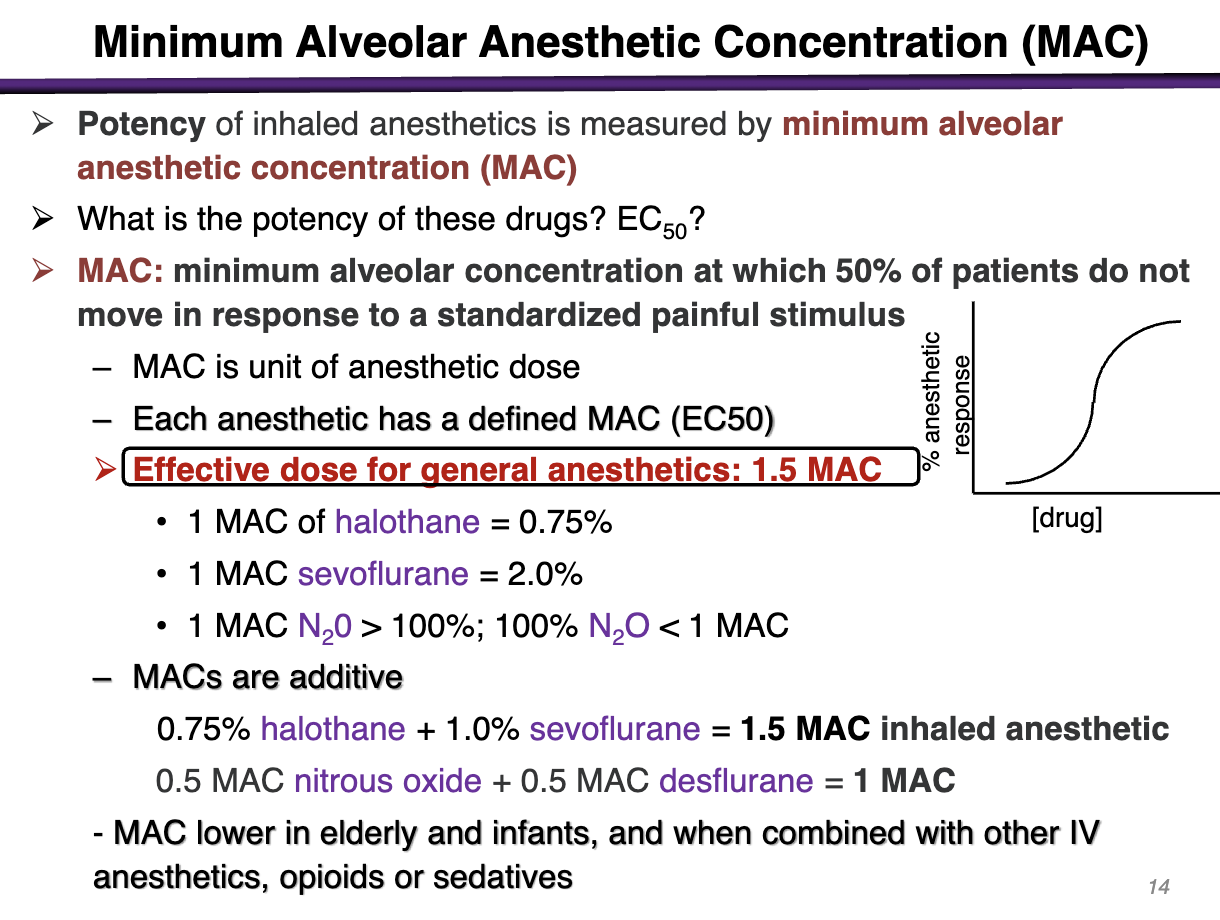
The lower the EC50; the ____ potency
The higher the potency (EC50 is the amount needed to yield the desired effect)
Effective dose for general anesthetics is
1.5 MAC
I will have an effect combination if I have at least 1.5 MAC to be efficacious
The lower MAC; what is potency
Higher potency
What groups have a lower MAC?
Lower in elderly and infants and when combined with other IV anesthetics, opioids or sedatives
Why isnt N2O efficacious
1 MAC of N2O > 100% ; BUT 100% N2O < 1MAC
Even if you give 100% of N2O you will never reach the 1.5 efficacious MAC
T/F MACs are a unit specific to drugs and cannot be readily added together
FALSE
MACs are additive;
You can add
0.75% of halothane + 1.0% sevoflurane (0.5 MAC sevoflurane) = 1.5 MAC Inhaled anesthetic
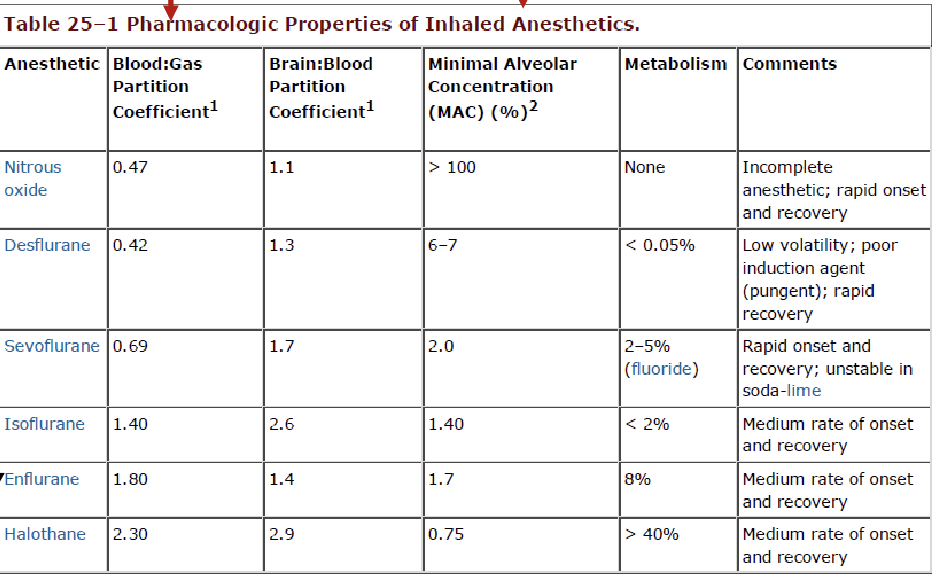
What aspect of the chart deals with potency and efficacy?
Minimal Alveolar Concentration (MAC)
Shows the percentage required to reach 1 MAC
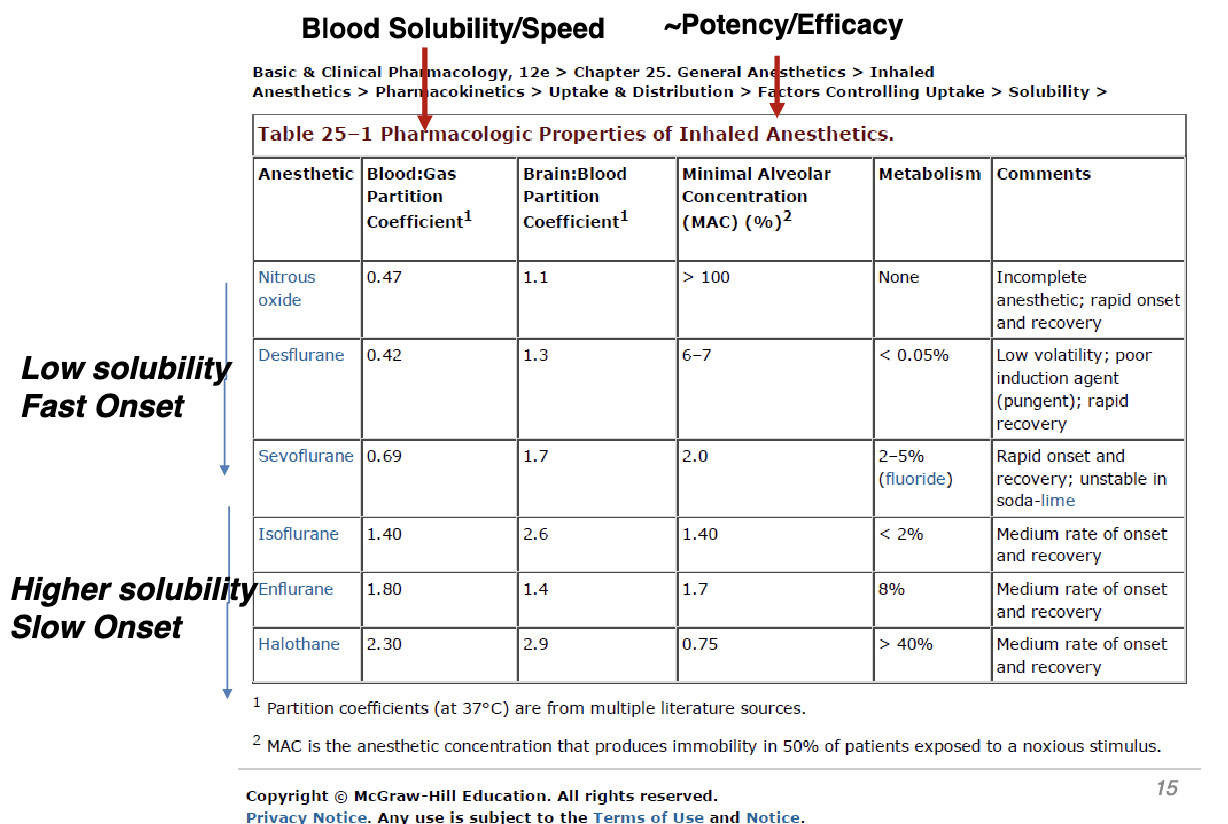
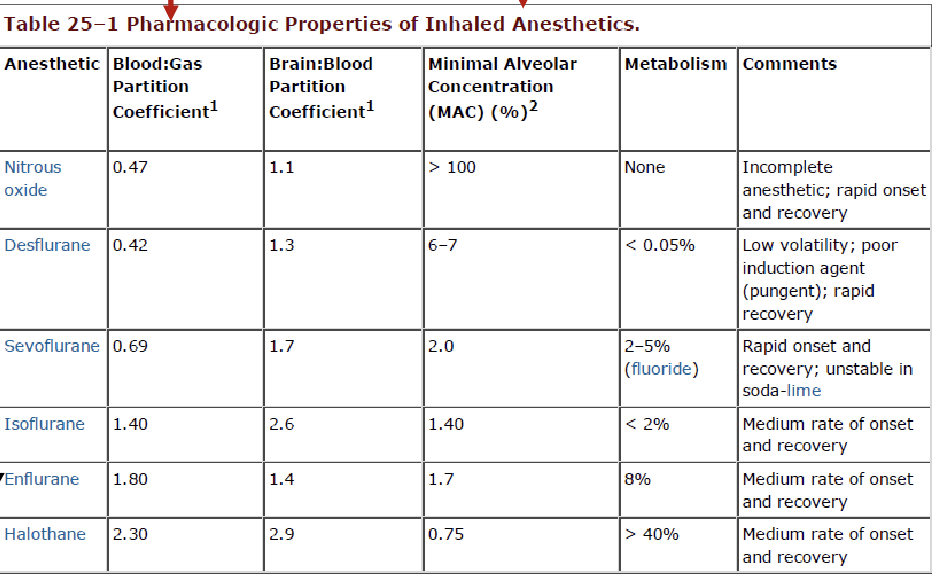
What aspect of the chart shows speed and onset of action?
Blood:Gas Partition Coefficient
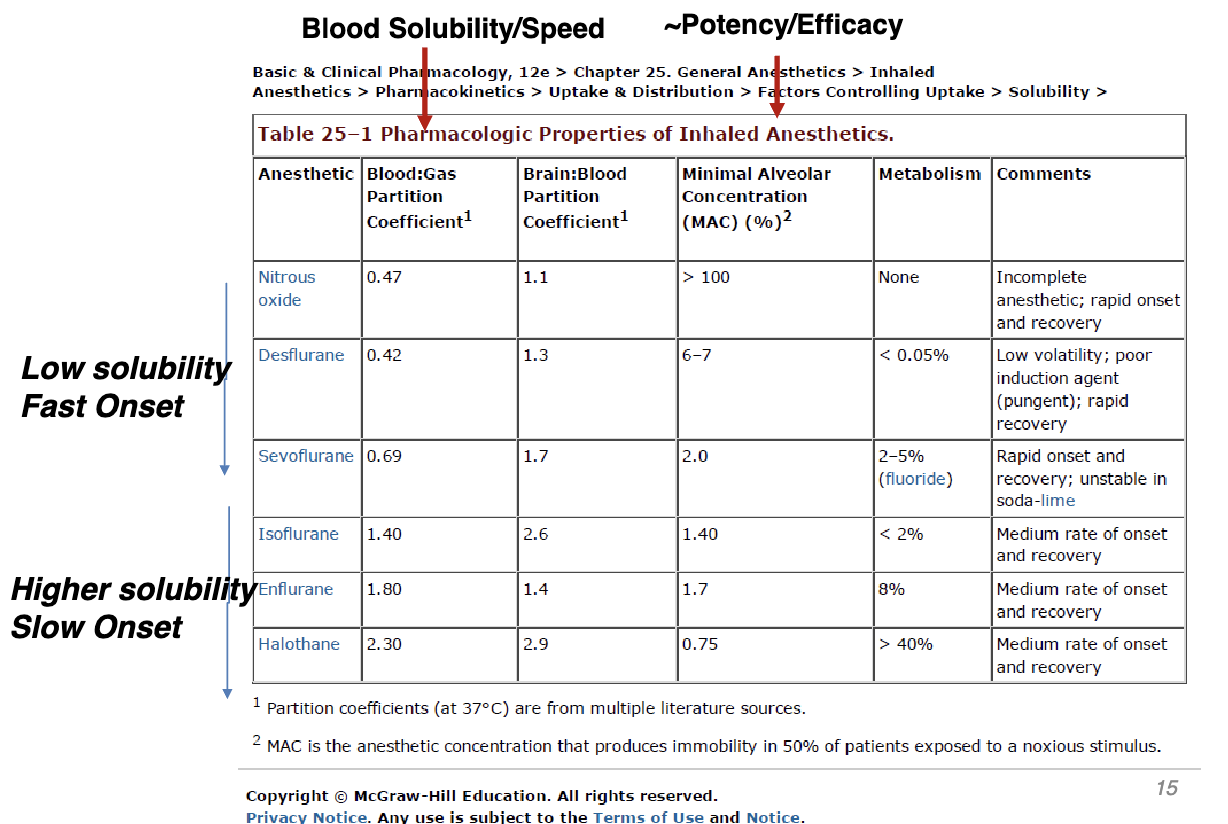
The lower solubility = WHAT? speed
The higher solubility = WHAT speed?
Low solubility = fast onset (hates the blood; wants to be gas = go into brain)
Higher solubility = slow onset (stays in the blood)
what effect do anesthetic drugs have on the braim?
Can increase cerebral blood flow via decreasing vascular resistance
Can lead to an increase in intracranial pressure
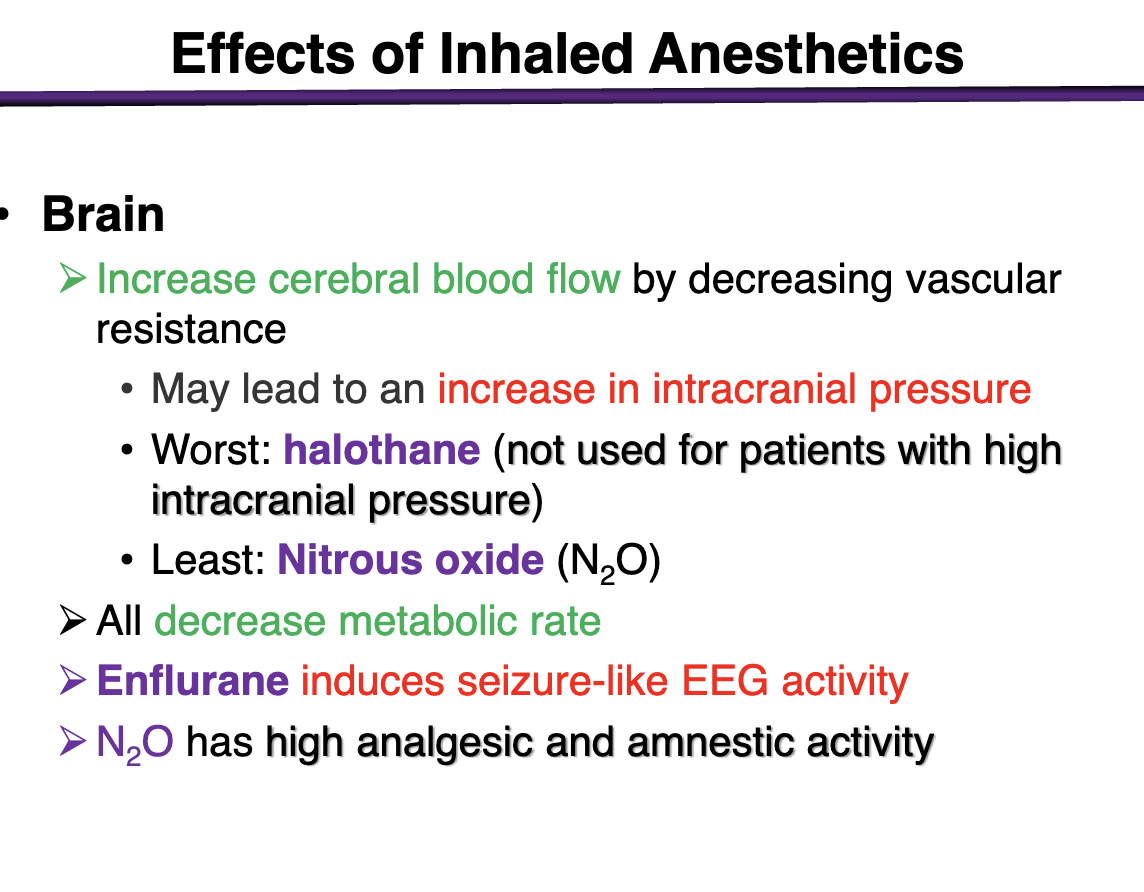
What is the worse anesthetic for increasing intracranial pressure?
Halothane should NOT BE USED in Pts with High Intracranial Pressure
Least with nitrous oxide (N2O)
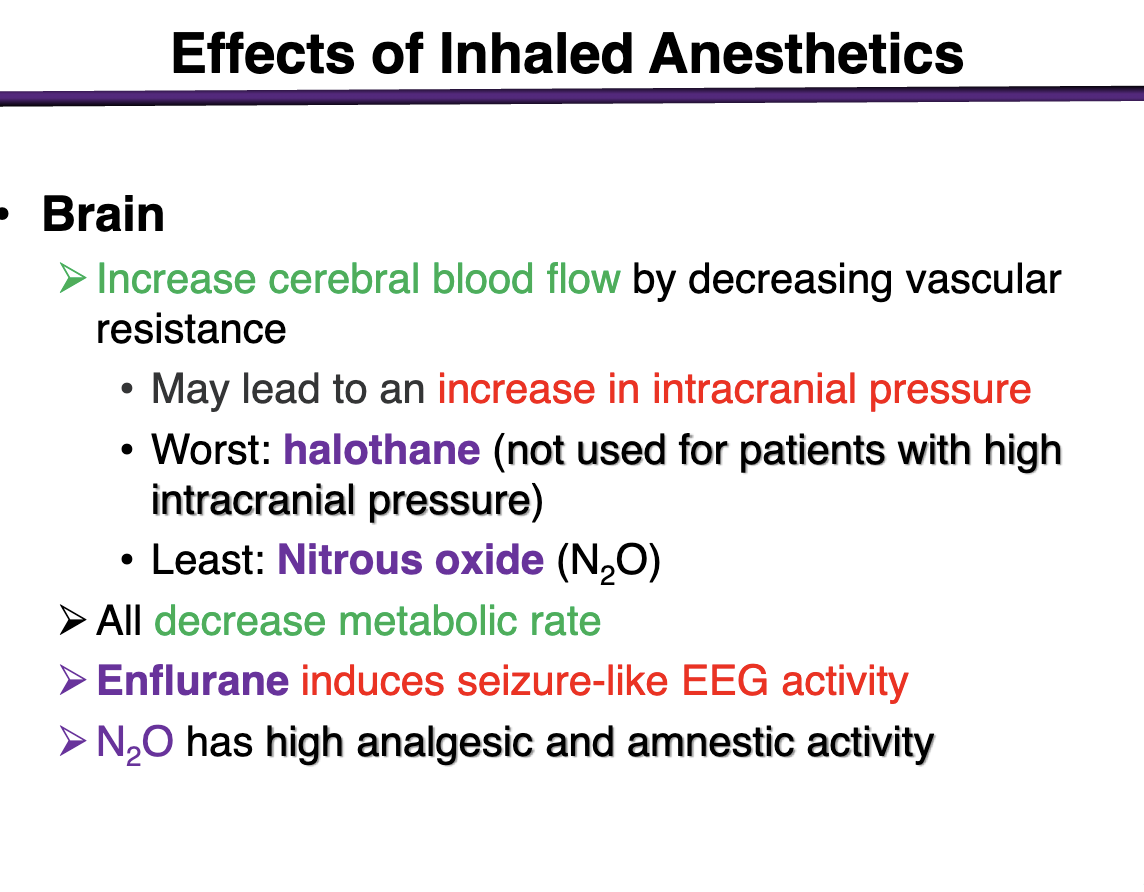
Effects of inhaled anesthetics on metabolic rate
Decrease metabolic rate in the brain
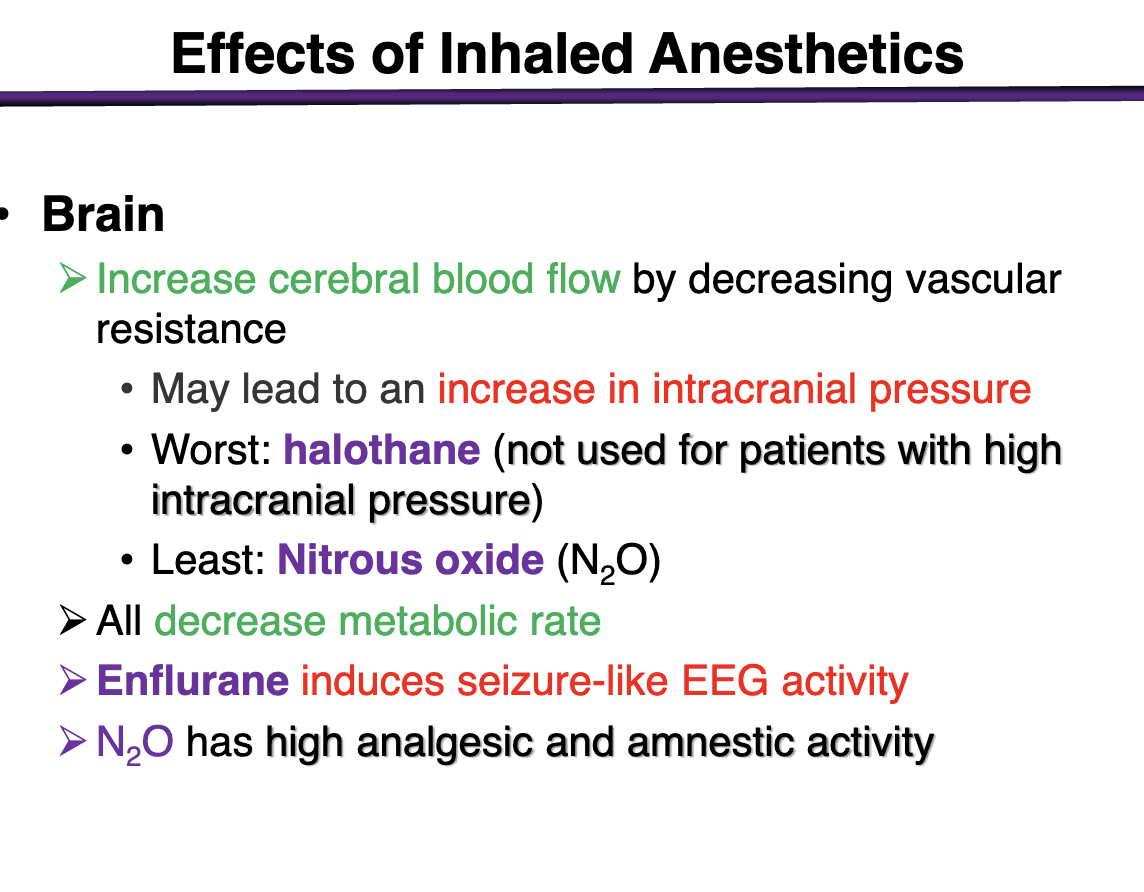
what does enflurane do to the brain
induces seizure-like EEG activity; contraindicated in pts with history of seizure
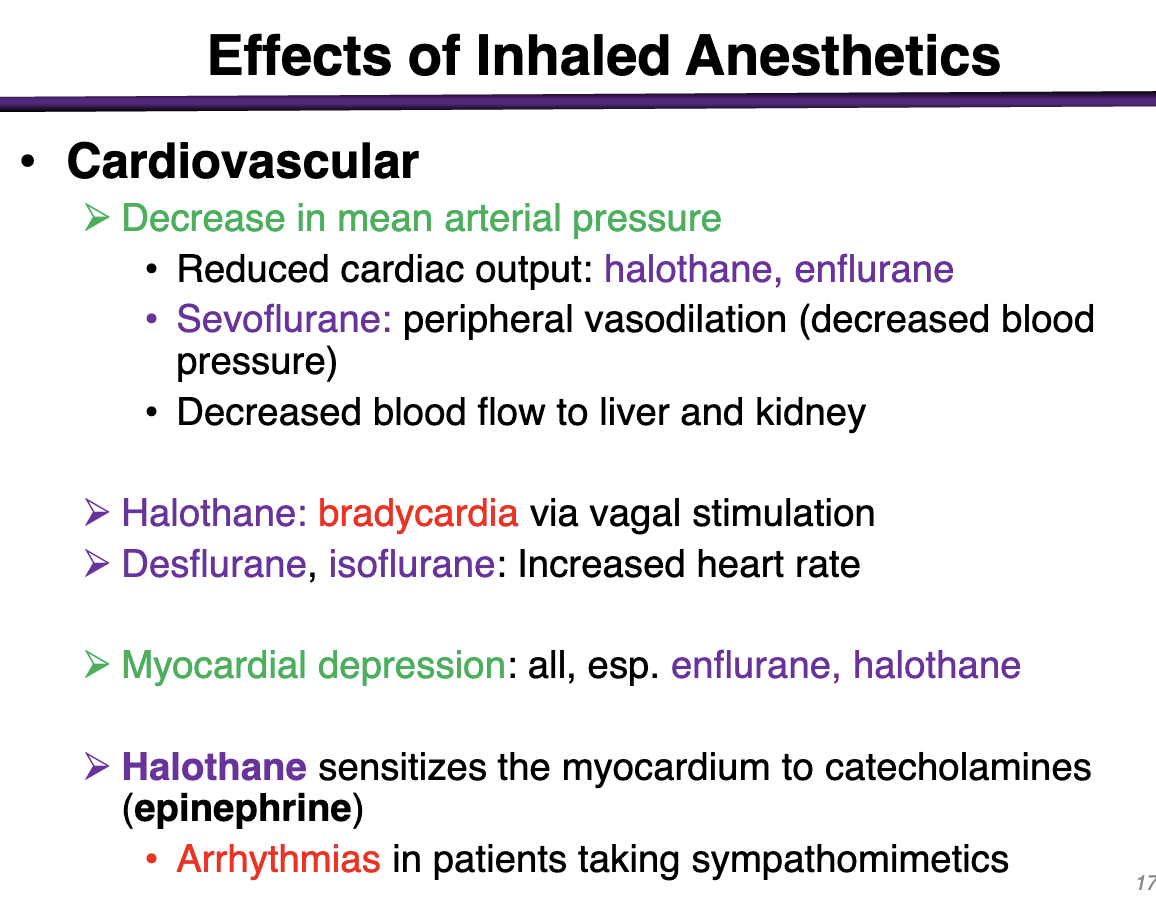
what effect do anesthetics have on the cardiovascular system?
Decrease in mean arterial pressure + General depression of cardiac function
Reduce cardiac output: halothane, enflurane
Sevoflurane: peripheral vasodilation (decrease blood pressure)
Decreased blood flow to liver and kidney
Halothane: bradycardia via vagal stimulation
Desflurane, isoflurane: decreased heart rate
Myocardial depression: all, esp. enflurane and halothane
Halothane sensitizes the myocardium to catecholamines (epinephrine)
Arrhythmias in pts taking sympathomimetics
These make sense; we don’t want these to be SUPER active but we have to make sure we don’t make any existing comorbidities worse
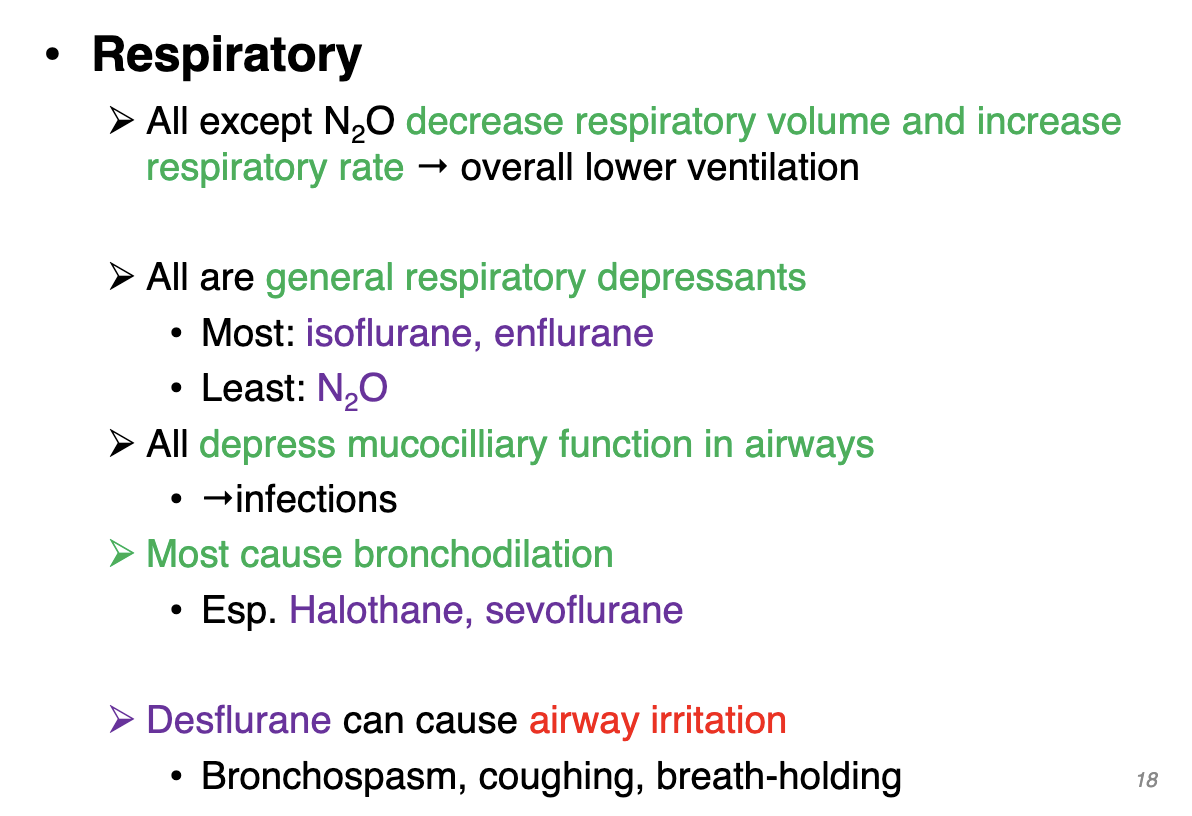
what effects do inhaled anesthetics have on respiratory system?
All except N2O → decrease respiratory volume and increase respiratory rate → overall lower ventilation
All are general respiratory depressants
Most: isoflurane, enflurane
Least: N2O
All depress mucociliary function in airways
Increase infections
Most cause bronchodilation
Esp. Halothane, sevoflurane
Desflurane can cause airway irritation
Bronchospasm, coughing, breath-holding
Effects of inhaled anesthetics on the kidney
decrease GFR and renal blood flow
effects of inhaled anesthetics in the liver
decrease hepatic blood flow
effect of inhaled anesthetics on uterus
potentially relax uterine smooth muscle
malignant hyperthermia
rare genetic disorder, sensitivity to inhaled anesthetics
Mutations in ryanodine receptors; responsible for the release of calcium from intracellular organelles
caused by increase in free calcium concentration in skeletal muscle cells
Severe muscle rigidity, hyperthermia, tachycardia, hypertension
Treated with dantrolene to decrease Ca, stabilize temperature and electrolytes
examples of barbiturates
thiopental, methohexital
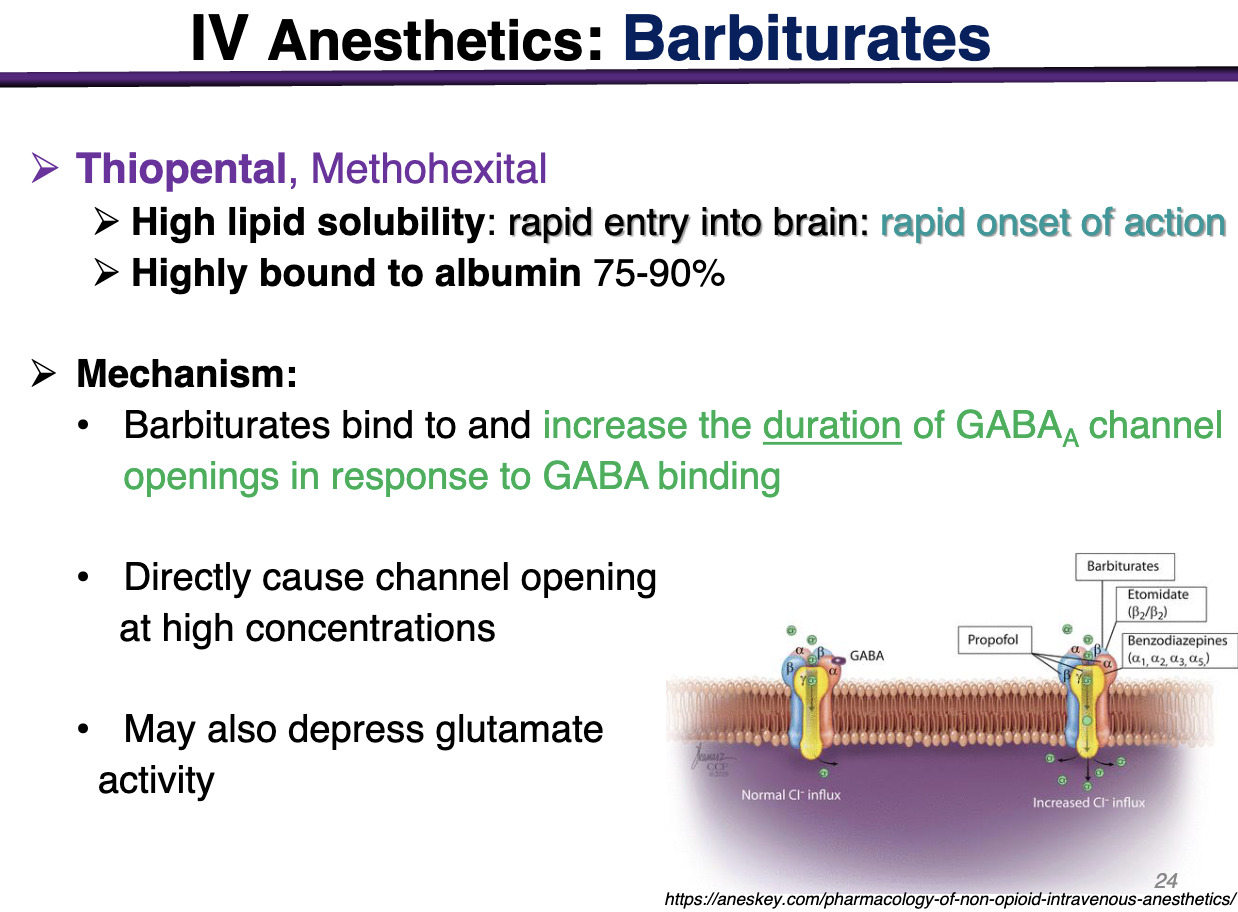
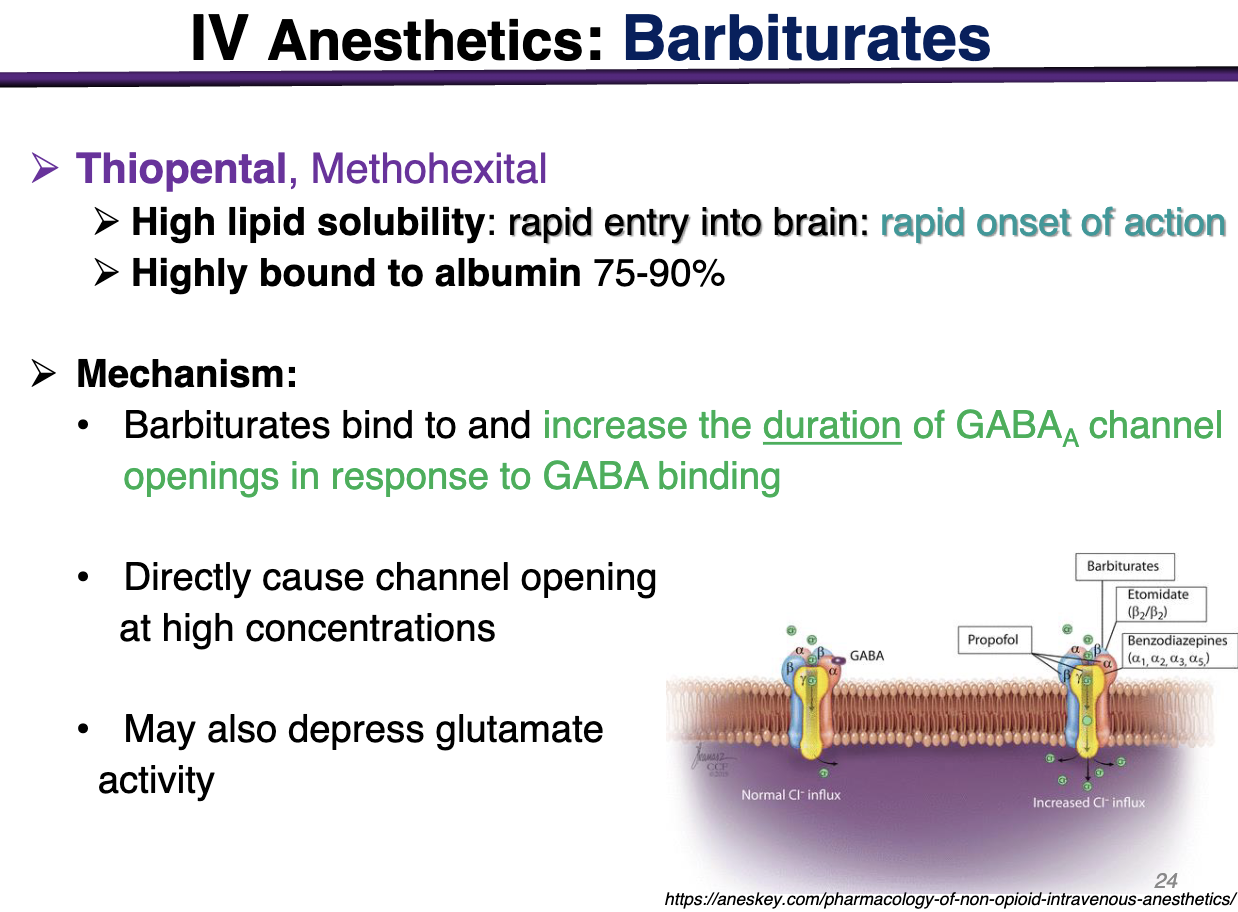
barbiturates moa
barbiturates bind and increase the duration of GABAa channel openings in reponse to GABA binding
HIGH lipid solubility → low blood gas coefficient (want to leave when they get to the blood) —> cross BBB
Directly cause channel opening at high concentrations
Barbiturates would prefer GABA to be present in the channel, BUT at a high concentration; they could activate the receptor on their own
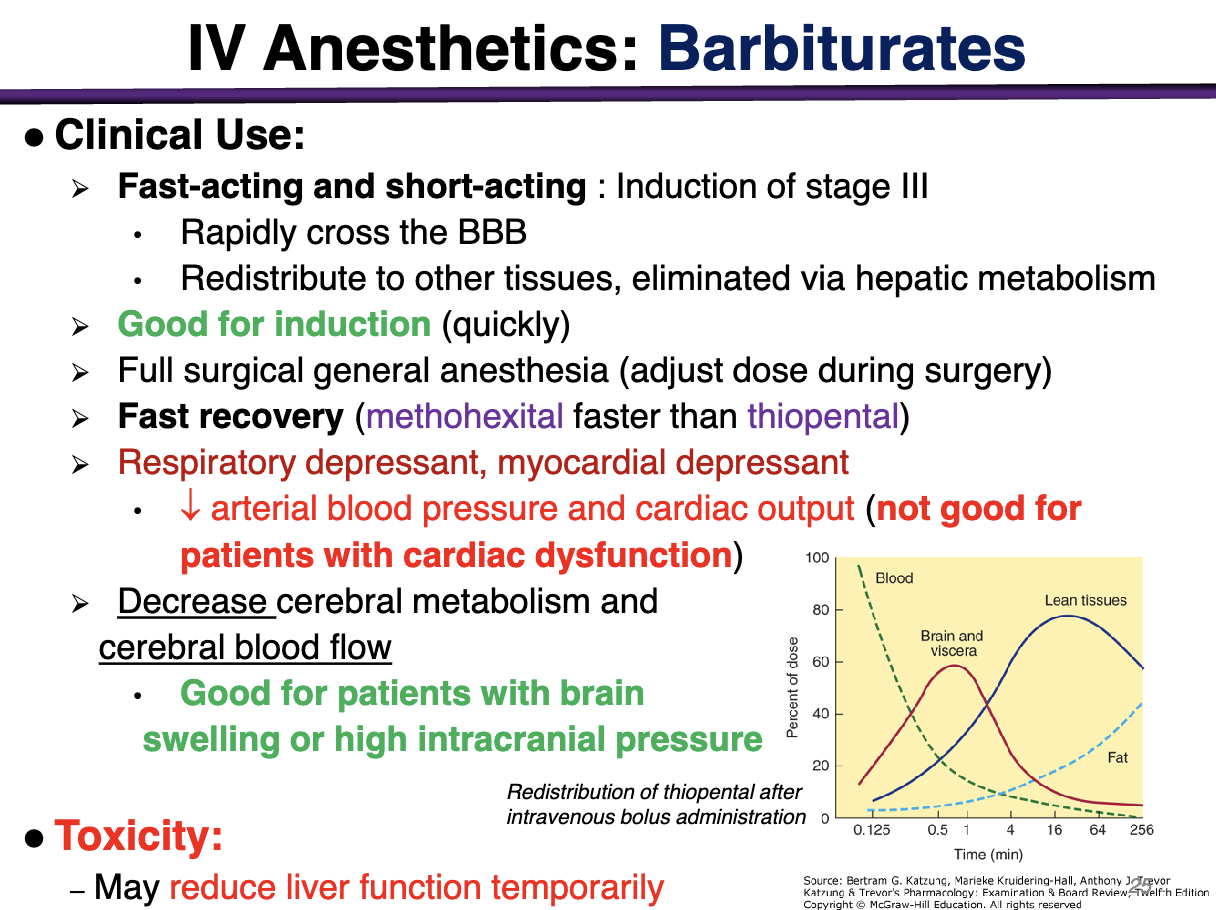
Clinical use for barbiturates
Fast acting and short acting: Induction of stage III
Rapidly cross BBB
Redistribute to other tissues, eliminated via hepatic metabolism
Good for induction (quickly)
Fast recovery (methohexital > thiopental)
Respiratory depressant, myocardial depressant
leads to a decrease in arterial blood pressure and cardiac output (not good for pts with cardiac dysfunction)
Decrease cerebral metabolism and cerebral blood flow
Good for patients with brain swelling or high intracranial pressure
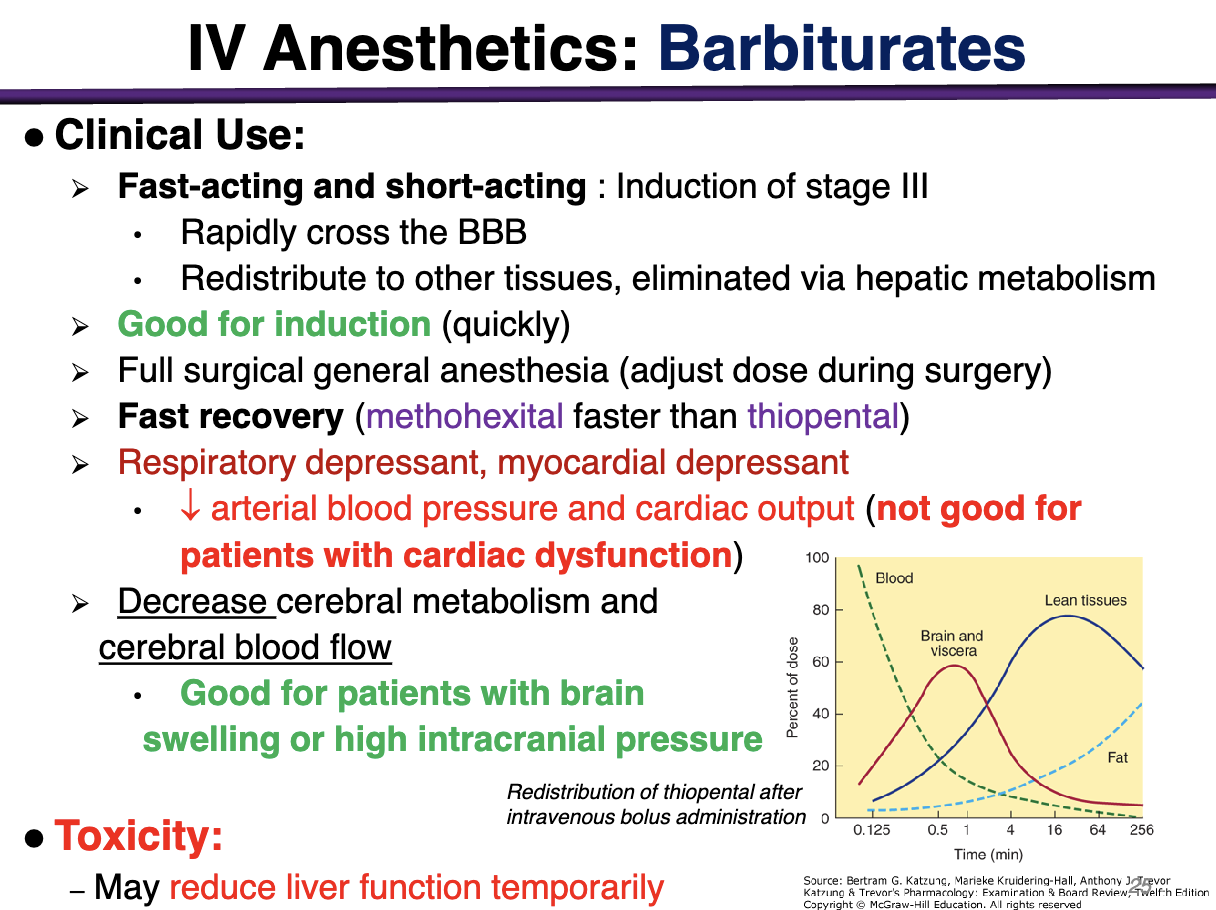
What is an clinical advantage and disadvantage for IV barbiturates
Advantage: decrease cerebral metabolism and cerebral blood flow; good for patients with brain swelling or high intracranial pressure
Disadvantage: Respiratory depressant, myocardial depressant, decrease arterial blood pressure and cardiac output (not good for patients with cardiac dysfunction)
can also reduce liver function temporarily
examples of benzodiazepines
lorazepam, diazepam, midazolam
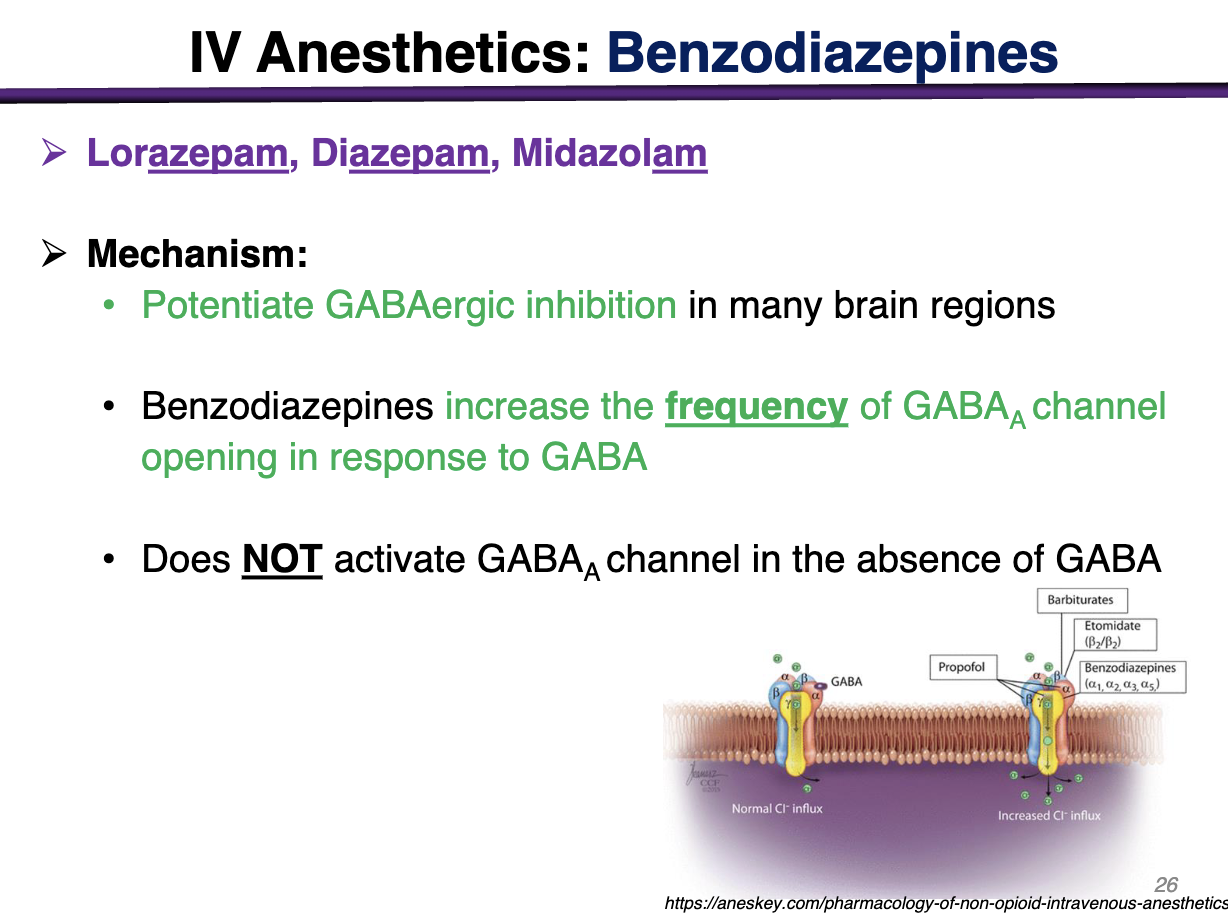
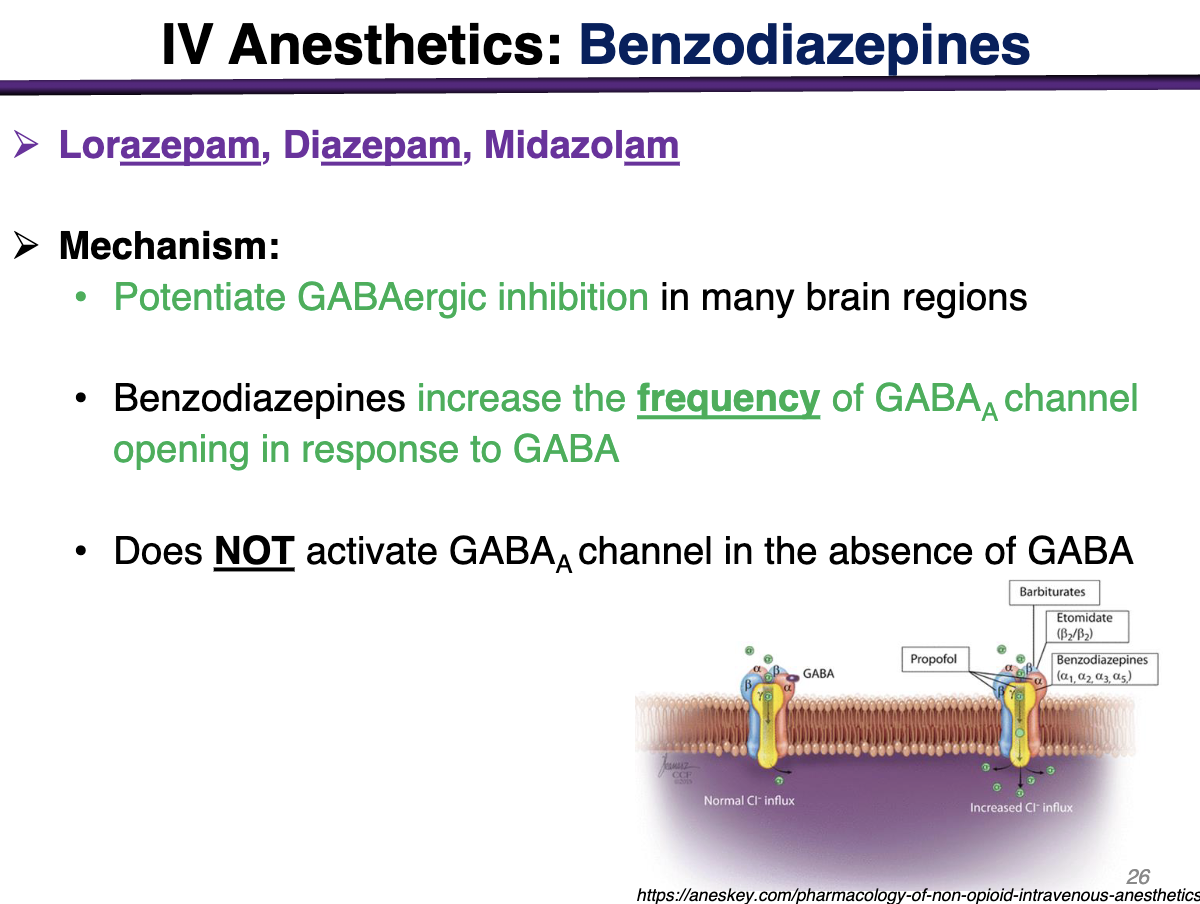
Benzodiazepines MOA
Potentiate GABAergic inhibition in brain regions
increase the frequency of GABAa channel opening in response to GABA
DOES NOT ACTIVATE GABAa CHANNEL IN THE ABSENCE OF GABA
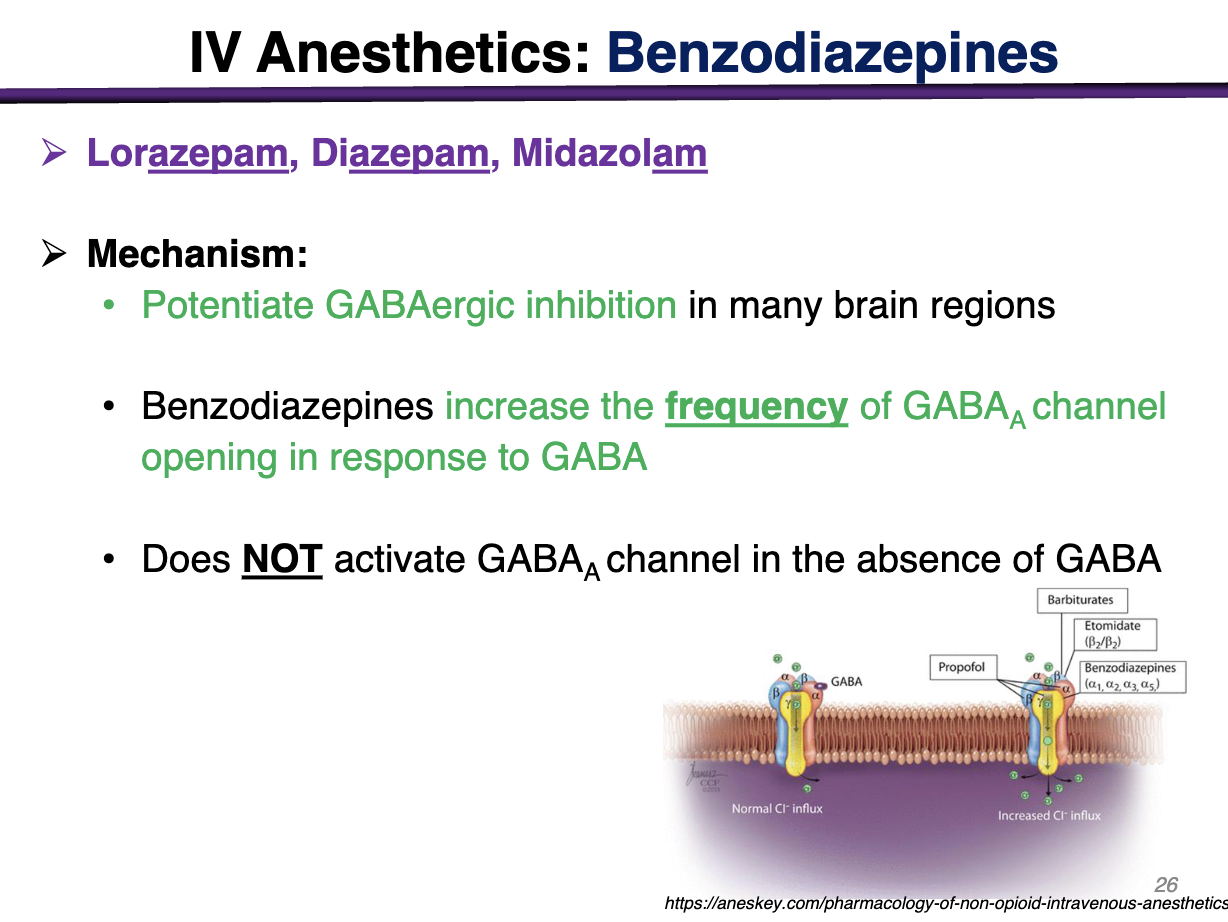
difference between barbiturates vs benzodiazepines MOA
Barbiturates increase the duration of GABAa channel
Benzodiazepines increase the frequency of GABAa channel (allosteric site)
does NOT activate GABAa channel in the absence of GABA
T/F at high concentrations, benzodiazepines can directly activate GABAa receptors
FALSE; benzodiazepines require the prior binding of GABA to GABAa receptors
onset of action of benzodiazepines vs barbiturates
Benzodiazepines have a slower onset of action than barbiturates
Characteristics of benzodiazepines in clinical use
Slower onset than barbiturates: Midazolam effects are slower than thiopental but has a longer duration of action.
Midazolam > diazepam > lorazepam
Does NOT reach surgical levels of anesthesia alone
significant sedation and amnesia
High doses may result in very long recovery from anesthesia, post operative respiratory depression
what can be used to accelerate recovery from sedative effects of benzodiazepines?
flumazenil (antagonist)
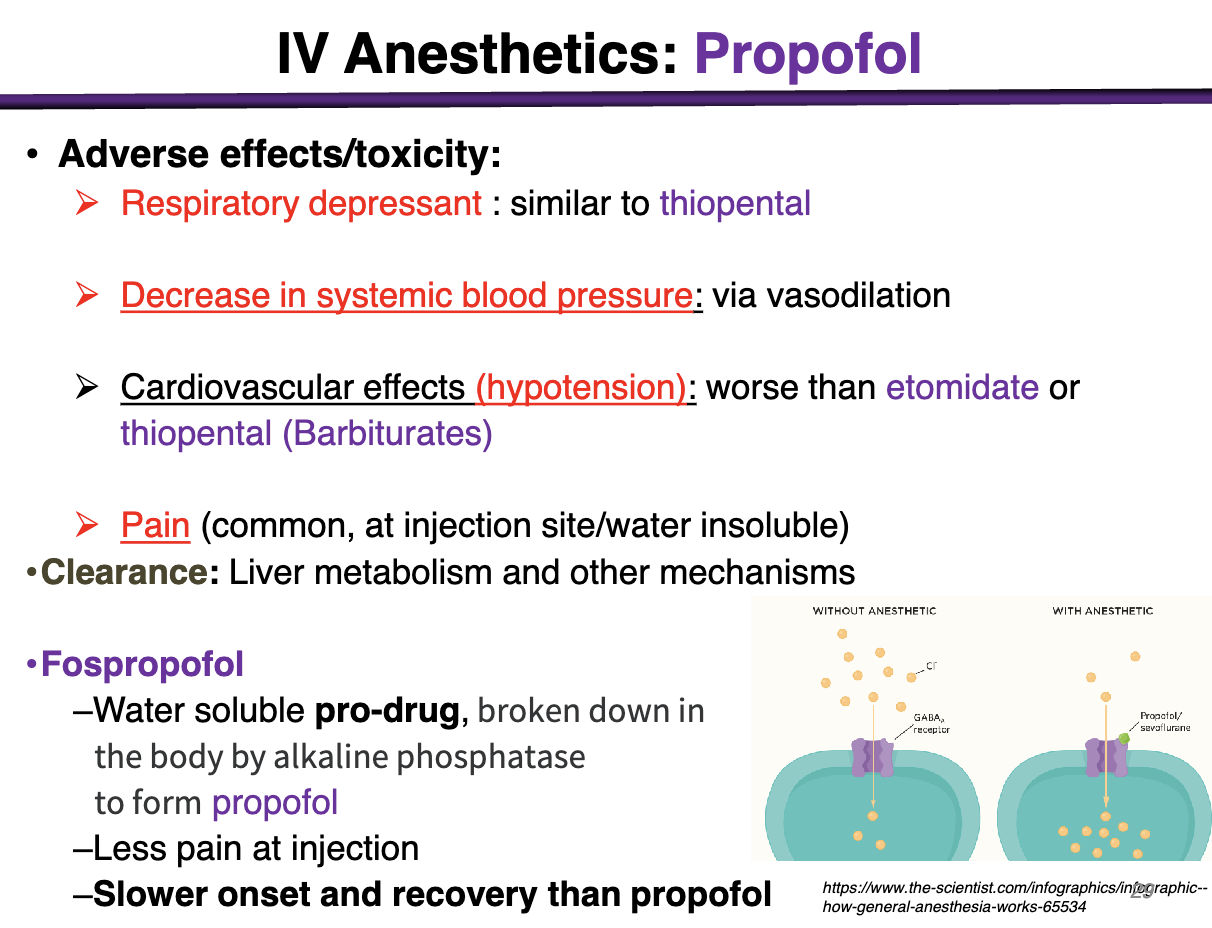
Propofol MOA
Potentiate GABA action, directly activate GABAa receptor channel opening
Propofol clinical use
Popular, replacing barbiturates as induction agents
Rapid onset of action: similar barbiturates
Rapid recovery: faster than barbiturates
Comfortable recovery: better than barbiturates (anti-emetic)
Commonly used for For surgery, part of a cocktail induction and maintenance
Used alone for outpatient surgery procedures
ADR: prolonged sedation in critical care patients
ADR for propofol
Respiratory depressant: similar to thiopental
Decrease in systemic blood pressure: via vasodilation
Cardiovascular effects (hypotension): worse than etomidate or thiopental (barbiturates)
Pain (common, at injection site/water insoluble)
CLEARANCE: Liver and other mechanisms
Etomidate MOA
potential GABA action, directly activate GABAa receptor channel opening
imidazole derivative
Etomidate clinical use
Used for induction: rapid onset, rapid recovery
No analgesic effects: given with opioids to block intubation response
Causes minimal cardiovascular and respiratory depression
no change in HR, little hypotensive effect
Toxicity: Pain on injection, post-operative N&V
Prolonged infusion can cause hypotension and electrolyte imbalance
No analgesic effect
MOA of ketamine
Blocks excitatory NMDA glutamate receptors
Can cause dissociative anesthesia: catatonia (loss of movement), amnesia, analgesia, may retain consciousness
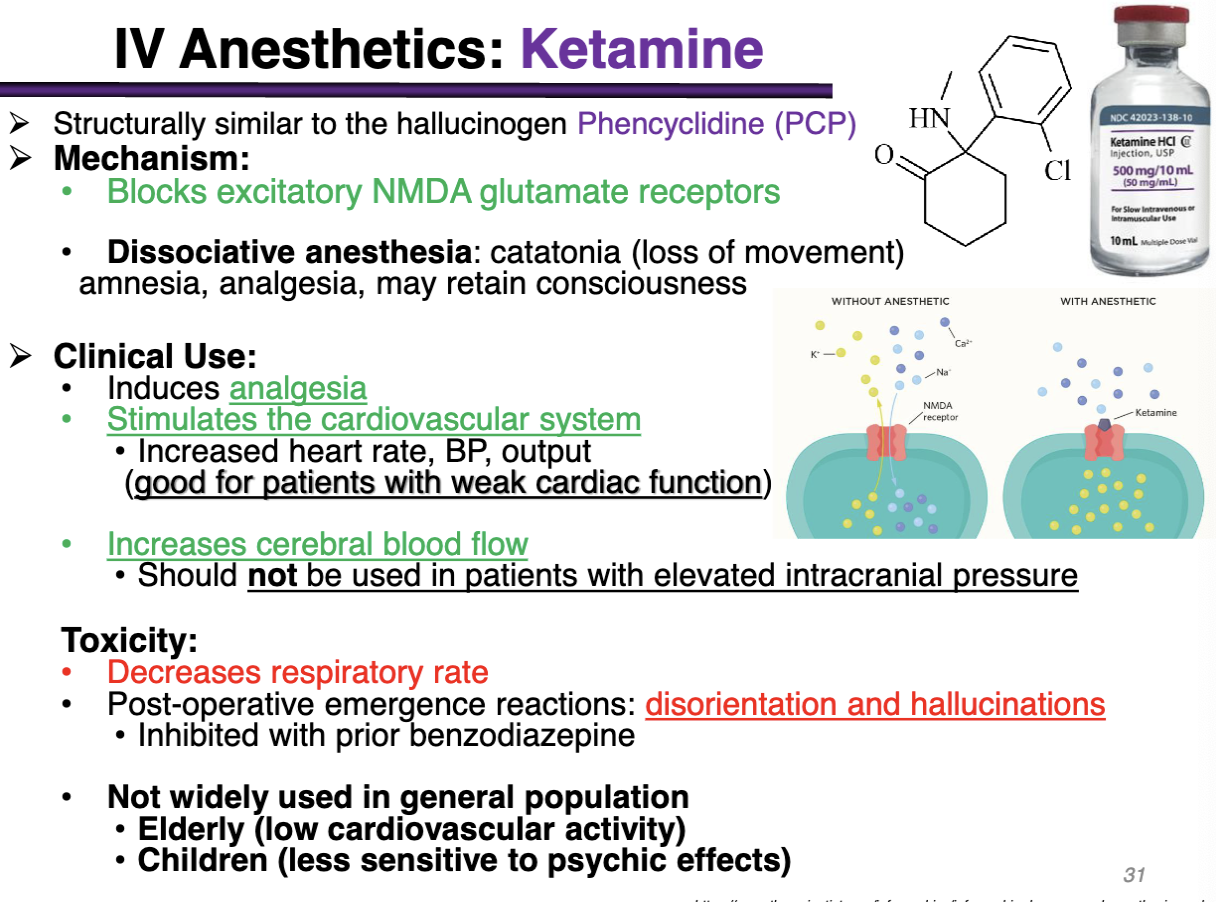
what is ketamine used for
analgesia
stimulated the cardiovascular system
increase HR, BP, output (good for pts with weak cardiac function)
Increases cerebral blood flow
should not be used in patients with elevated intracranial pressure
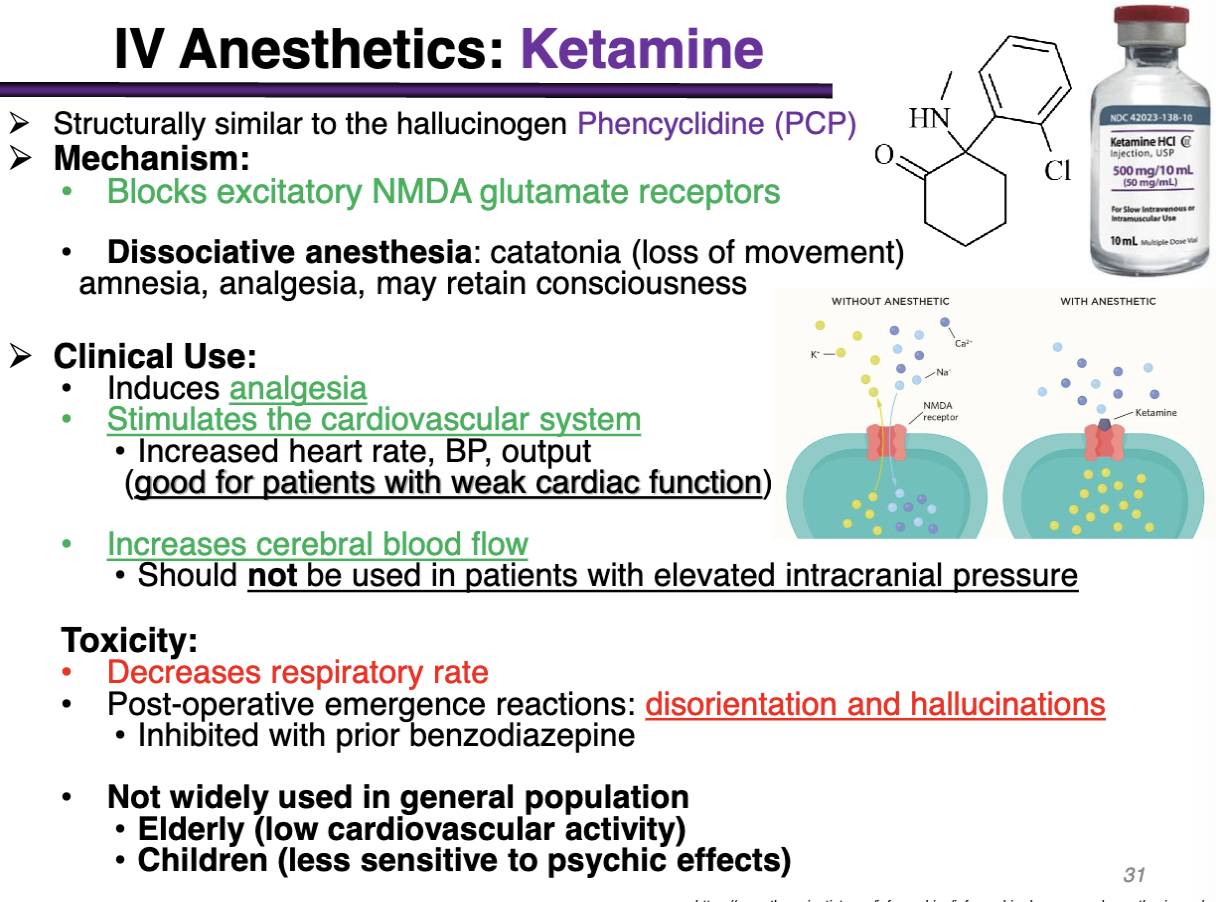
ketamine toxicity
decreases respiratory rate
post-operative emergence reactions: disorientation and hallucinations
inhibited with prior benzodiazepine (etomidate)
NOT USED in the elderly (low cardiovascular activity)
Children (less sensitive psychic effects)
Opiates MOA
full agonists at the u opioid GPCRs
opiates clinical use
moderate general anesthesia
Morphine/Fentanyl combined with N2O benzodiazepines
Pts with low circulatory reserve
Premedication and induction agents or as an adjunct for other anesthetics
alfentanil and remifentanil: short duration of action
Remifentanil has fastest metabolism; fastest recovery
ambulatory procedures
Opioids useful for spinal and epidural applications: post-operative analgesia
Outpatient procedures as fast recovery and short acting
Cocktail of balanced anesthesia
Conscious sedation: minor procedures
opioids ADR
impaired ventilation due to rigidity of the chest wall
prolonged postoperative respiratory depression —> reversed with naloxone
The primary mechanism for most general anesthetics is to:
A. Activate GABA_A
B. Inhibit GABA_A
C. Activate GABA_B
D. Inhibit GABA_B
A) Activate GABA_A receptors
downstream effect is inhibition bc GABA is inhibitory
In inhaled anesthetics, faster onset of action is predicted by
A. High blood solubility
B. Low blood solubility
C. High MAC
D. Low MAC
B) Low blood solubility
Low blood solubility = more for the gas = easier to get to the brain OR low blood solubility = hates water = lipophilic
Onset deals with Solubility and Speed and path to the brain
MAC deals with efficacy and potency (similar to EC50)
In inhaled anesthetics, maximal efficacy is predicted by_________.
A. High blood solubility
B. Low blood solubility
C. High MAC
D. Low MAC
D) low MAC
MAC deals with efficacy and potency (similar to EC50) → Minimum alveolar anesthetic concentration; low possible dose for same efficacy
Low blood solubility = more for the gas = easier to get to the brain OR low blood solubility = hates water = lipophilic
Onset deals with Solubility and Speed
Which of the following would be a reasonable level of inhaled anesthesia for major surgery?
A. Pure nitrous oxide
B. Pure halothane
C. 10% isoflurane
D. 2% sevoflurane + 3% desflurane
E. 3% halothane + 1% sevoflurane
D. 2% sevoflurane + 3% desflurane
This would give 2% Sevoflurane = 1 MAC (2.0% is needed for 1 MAC) and 3% desflurane = 0.5 MAC (6-7% is needed for 1 MAC)
The MAC in percent is the percent need to achieve 1 MAC
Which drug causes the least effect on blood pressure and respiration?
A. Halothane
B. Enflurane
C. Sevoflurane
D. Desflurane
E. Nitrous oxide
E. Nitrous Oxide
Safest overall with the lowest MAC
What kind of receptors are glutamate receptors?
Major excitatory NT in the CNS; when glutamate binds to its receptors? The sodium channels open up; Ligand gated CATION channels