David Morton
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
What is GORD?
ACID FLOWS FROM THE STOMACH THROUGH THE LOWER OESOPHAGEAL SPHINCTER INTO THE OESOPHAGUS WHERE IT THEN CAUSES SYMPTOMS
What type of epithelia lines the oesophagus/stomach
stratified squamous epithelial cells in the oesophagus and columnar in the stomach
Causes and Triggers of GORD:
Spicy Food-Capsaicin which makes food spicy can irritate the lining of the oesophagus, it can also slow down digestion so food sits in the stomach for longer
Coffee and Tea-relaxes low oesophageal sphincter and also increase the amount of acid the stomach secretes
Alcohol-relax sphincter, produce more stomach acid which can irritate stomach lining
Smoking-weakens sphincter (nicotine)
NSAIDs
Hiatus hernia-increase pressure on lower sphincter causing acid to be pushed into the oesophagus
Obesity-increase abdominal pressure, impair gastric emptying and decrease gut motility, overeating, unhealthy foods, higher levels of pancreatic enzymes and bile
Pregnancy-progesterone can relax the oesophageal sphincter and progesterone also slows digestion
Over 50-muscular fibres holding sphincter weaken
Stress-increases stomach acid production making it more likely to leak up, also relaxes sphincter
How do NSAIDs trigger GORD?
Damaging the digestive tract: NSAIDs can damage the mucus in the digestive tract, which can lead to GERD.
Increasing gastric acid secretion: NSAIDs can increase the amount of gastric acid secreted.
Reducing lower esophageal sphincter pressure: NSAIDs can reduce the pressure in the lower esophageal sphincter, which can lead to GERD.
Irritating the esophageal epithelium: NSAIDs can directly irritate the esophageal epithelium, which can lead to GERD.
Reducing stomach motility: NSAIDs can reduce the motility of the stomach, which can lead to GERD
Presentation of GORD:
DYSPEPSIA-indigestion
heartburn
acid regurgitation
retrosternal or epigastric pain
bloating
nocturnal cough (worse when lying down)
hoarse voice-acid causes laryngitis
Red Flags for GORD
Dysphagia-difficulty swallowing is the main one
Aged over 55
Weight loss
Pain and reflux-mass on palpation
Nausea and vomiting
low haemoglobin and raised platelet count
What is the rule of referral with red flag patients?
They will be referred for a direct access endoscopy
What type of endoscopy is an OGD
OESOPHAGO-GASTRO-DUODENOSCOPY (OGD) and it assesses for gastritis, ulcers, upper GI bleeding, Barretts oesophagus, oesophageal stricture, malignancy
Nb: patients with evidence of upper GI bleeding (malaena or ground coffee vomiting) need admission and urgent endoscopy
What is a hiatus hernia and what are the types of it?
herniation of the stomach through the diaphragm-when the opening in the diaphragm is wider, the stomach can enter through the diaphragm and the contents of the stomach refluxes into the oesophagus.
1: Sliding-stomach slides through the diaphragm
2: rolling-separate portion of the stomach folds up through the diaphragm
3: both
4: large opening and additional abdominal organs enter the thorax
Diagnostic process for a hiatus hernia:
Chest x-ray, CT Scan, endoscopy, Barium swallow test
Management of GORD:
Lifestyle changes e.g. lose weight, stop smoking, don’t eat acidic food, reduce tea, coffee, alcohol, smaller meals, stay upright after meals, eat 3hrs before lying down, stops NSAIDS
Ant-acids-Gaviscon, Pepto-Bismol
Proton pump inhibitors-omeprazole and lansoprole
Histamine H2 receptor antagonists e.g. famotidine
Surgery-laparoscopic fundoplication where the fundus is tied round the lower oesophagus to narrow the lower oesophageal sphincter
Normally H.Pylori is ruled out, 1 month trial of a PPI
Mechanism of action of PPIs:
bind and inhibit h/k+ ATPase irreversibly, in the parietal cells. The proton pump is the last stage in gastric acid secretion, and is responsible for secreting H+ ions into the gastric lumen. Because the H,K-ATPase is the final step of acid secretion, an inhibitor of this enzyme is more effective than receptor antagonists in suppressing gastric acid secretion. All of these drugs inhibit the gastric H,K-ATPase by covalent binding, so the duration of their effect is longer than expected from their levels in the blood
Mechanism of action of Histamine H2-receptor antagonists
Histamine H2 binds to Gs protein, increase adenylate cyclase, increase cAMP and increase the amount of gastric acid produced. antagonists bind reversibly to the histamine h2 receptors on gastric parietal cells, inhibiting their binding
What is helicobacter pylori?
a gram-negative aerobic bacteria that can live in the stomach. It causes damage to the epithelial lining, resulting in gastritis, ulcers and an increased risk of stomach cancer. It avoids the acidic environment by forcing its way into the gastric mucosa, using flagella to propel itself. It creates gaps in the mucosa, exposing the epithelial cells underneath to damage from stomach acid.
H. pylori produces ammonium hydroxide, which neutralises the acid surrounding the bacteria. It also produces several toxins. The ammonia and toxins lead to gastric mucosal damage.
We offer a test for H. pylori to anyone with dyspepsia. They need 2 weeks without using a PPI before testing for H. pylori for an accurate result.
What are the investigations for H.Pylori?
Stool antigen test
Urea breath test using radiolabelled carbon 13
H. pylori antibody test (blood)
Rapid urease test performed during endoscopy (also known as the CLO test). This is when a small sample of stomach mucosa which is added to urea, and H.Pylori converts urea to ammonia which is more alkaline, so it can be pH tested.
How is H.Pylori treated?
triple therapy with a PPI, two antibiotics (amoxicillen and clarithromycin) for 7 days.
What is Barretts Oesophagus?
lower oesophageal mucosa changes from squamous to columnar cells-makes it more likely to turn into adenocarcinoma as this is a metaplasia condition. It is a step wise condition ranging from low grade to high grade dysphagia, and it is a premalignant condition. Patients may actually notice an improvement in reflux symptoms when they develop barretts oesophagus
Treatment of Barretts oesophagus:
endoscopic monitoring of progression of adenocarcinoma
PPiS
Endoscopic ablation-destroys columnar epithelial cells and these are then replaced with squamous epithelial cells
Dysplasia:
Metaplasia:
presence of abnormal cells
change in the type of cells
What is Zollinger-Ellison Syndrome
this is when a duodenal or pancreatic tumour secretes excessive quantities of gastrin, a hormone that stimulates acid secretion in the stomach, causing dyspepsia, diarrhoea and peptic ulcers.
Gastrin-secreting tumours (gastrinomas) may be associated with multiple endocrine neoplasia type 1 (MEN1), an autosomal dominant genetic condition, which can also cause hormone-secreting tumours of the parathyroid and pituitary glands.
do side effects of h2 antagonists and ppis
What is the set point theory?
the idea that the human body has a pre-determined weight or fat mass range that it tries to maintain. The body tries to regulate energy intake e.g. increased or decreased appetite or energy expenditure (metabolism decreases or feelings of lethargy)-explains why dieters to maintain weight loss over a longer period of time as caloric restriction may become less effective and harder to obtain
passive set point compensation and leptin and ghrelin:
passive-burn less calories as carrying less weight around all the time and also if you increase muscle mass, you burn more calories. There is an increase in leptin which is a hormone that indicates fullness in obese individuals and low leptin levels in anorexia sufferers, however it’s weakness doesn’t really explain why people’s set points can change throughout their life e.g. as you get older
Ghrelin is a hormone which is produced in hunger, high levels in anorexia patient, low levels in obese individuals (increase during dieting)
Evidence underlying the set point:
Animal studies-overfed/underfed rats and they returned to their pre-weight
Human-Minnesota starvation experiment-gained back the 66% of fat that they’d lost
Identical twins: similar weight
set point tends to range from 5-10% of the body weight of the individual
Against-western diets are obesogenic-camouflages the set point, rich in fat and sugar as these foods can modify the metabolism and shift the set point upwards
Function of the upper oesophageal sphincter:
block food from regurgitating into the airways and prevents air entering GI tract
What makes up the upper oesophageal sphincter?
The cricoid cartilage and the arytenoid and inter arytenoid muscles make up the anterior parts of the sphincter. The thyropharyngeus and the cricopharyngeus muscles form the majority of the sphincter's posterior and lateral walls, with the former accounting for the upper two-thirds of the sphincter and the latter occupying the lower one-third.
How does the UES open?
Contraction of the hyoid muscle that pulls the larynx forwards, combined with the relaxation of the cricopharyngeus and the thyropharyngeus, causes the sphincter to open wide
What to do when a patient presents with pain in the stomach?
SOCRATES
Test and treat for helicobacter-amoxicillen
blood tests-LFTs, amylase-butary colic
radiological investigations (CXR, US, CT (obstruction/perforation), MRI-inflammation)
Upper GI endoscopy-look for pathology
Manometry and oesophageal pH study-heightened pressure/acid reflux
Causes of upper abdominal pain:
oesophageal/gastric/duodenal ulcer
GORD
Oesophagitis
cancer
Cholelithiasis-gall stones
oesophageal spasm
acute/chronic pancreatitis
Non-visceral/GI pain e.g. musculoskeletal, cardiac
Visceral and non-visceral pain
non-visceral: pain usually well localised, exacerbated by movement, pain, coughing etc. e.g. spinal/painful rib, last for seconds or constant
visceral may be more widespread
Exacerbations dyspepsia:
peptic ulcer-diurnal variation, oral intake, specific foods
GORD-oral intake, lying down, bending over
Oesophagitis-swallowing, extreme temperatures, spices, alcohol
Associated symptoms dyspepsia:
heartburn, odynophagia(pain on swallowing), dysphagia, regurgitation, nausea, vomiting, GI bleeding, early satiety, anaemia, jaundice
What is dyspepsia?
a group of symptoms that alert doctors to consider disease of the upper GI tract, and states that dyspepsia itself is not a diagnosis. Typically present for 4 weeks or more and include upper abdominal pain, gastric reflux, heartburn, nausea and vomiting.
Epidemiology:
40% h.pylori in uk
4% of adult consultations
David Morton plan of action:
Differential Diagnosis
FBC
Medication review e.g. nitrates, NSAIDs, corticosteroids
Urgent referral if over 55 for GI endoscopy in 4-6 weeks for unexplained persistent dyspepsia
one month PPI trail and lifestyle advice
Test and treat for H.Pylori if above doesn't help
Drugs which can lower tone of oesophageal sphincter:
calcium antagonists, nitrates, theophyllines (asthma/COPD)
Bisphosphonates-taken for osteoporosis
Red Flag Symptoms:
Anorexia
Weight loss
Persistent vomiting
Anaemia
Haematemesis/melaena
abdominal mass
People who you would refer for upper GI endoscopy:
dysphagia
abdominal mass
GI bleeding (same day referral)
aged 55 over with upper abdominal pain, reflux and dyspepsia.
Primary Approach to Dyspepsia if no alarm symptoms:
reduce tea, coffee, spicy foods, stop smoking, stop NSAIDs
Ant-acids/acid suppressants-omeprazole/h2 antagonists
sulcrafate/bismuth
Duration of PPI treatment
levels off round 4 weeks for treatment, 6 weeks recommended for healing. take 30 mins before food and with famotidine best taken late at night on an empty stomach-dual therapy can be used
Side effects of PPI:
diarrhoea, headaches, dizziness, tiredness
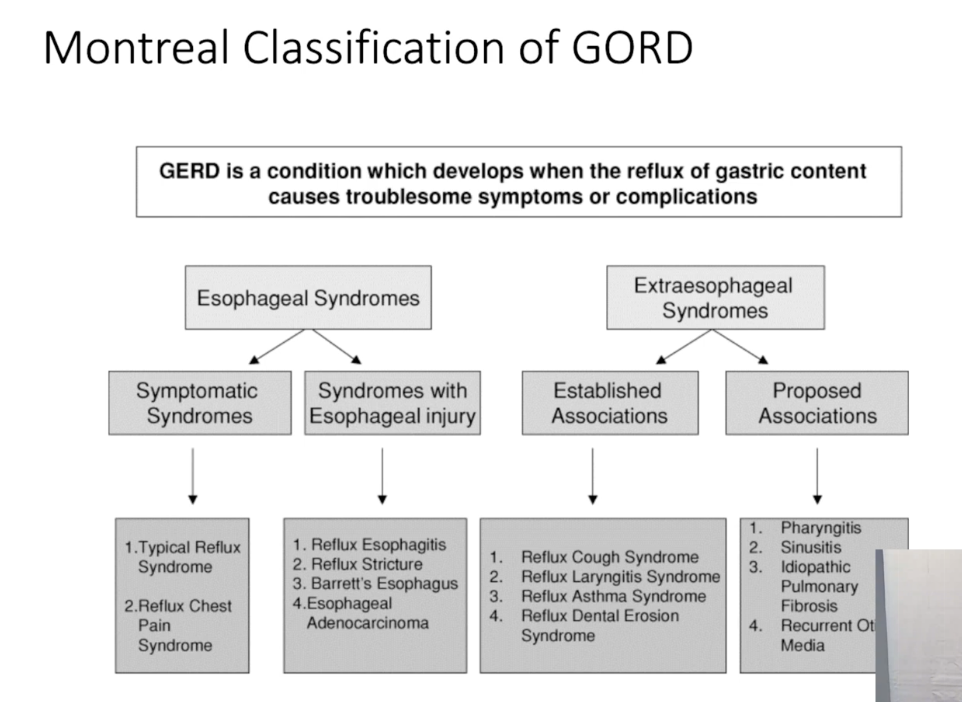
Classifications of GORD:
Treatment of GORD:
weight loss, smoking, sleep with head high, mealtimes smaller and closer together.
medical-antacids, alginates, H2RA, PPI, prokinetics-medications which help empty acid from the stomach but not longterm
surgical-fundoplication-dysphagia, belching, bloating, flatulence as symptoms
LINX and Stretta procedures
Follow up of GORD:
non-erosive A and B-Treat symptomatically
C and 😩 -may need long term treatment
Barrett’s oesophagus: 0.5% chance of oesophageal carcinoma
Peptic ulcers:
oesophageal, gastric and duodenal: gastric and duodenal due to h. pylori or aspirin/nsaid use.
gastric and oesophageal may be malignant
aim to reduce gastric acid secretion
Treatment of peptic ulcer:
Treat underlying cause: h pylori infection/nsaids/aspirin
PPI
oesophageal/gastric ulcer to be followed up
check for helicobacter eradication
bleeding ulcer-maintain haemodynamic instability, endoscopic treatment, perforated ulcer-surgery
H.Pylori infection and disease:
associated with ulcers and can cause gastritis, 95% MALToma cancer cleared with h pylori clearance
use antibiotics and PPI to clear it but there is increasing antibiotic resistance
Barrett’s oesophagus risk factors:
males
obesity
aged 50+
caucasian
family history
smoking
can take more than 10 years to develop
anthropomorphises-change in lining of the intestine, likely will require lifelong PPI therapy
Achalasia:
Achalasia is a swallowing condition that affects the tube connecting the mouth and the stomach, called the esophagus. Damaged nerves make it hard for the muscles of the esophagus to squeeze food and liquid into the stomach. Food then collects in the esophagus, sometimes fermenting and washing back up into the mouth
treated by Heller's cardiomyotomy is the name of the surgical procedure used in achalasia. Surgery is indicated for: young patients (<40 years) who will require lifelong dilations or botulinum toxin injections; patients with recurrent or persistent symptoms after multiple nonsurgical treatments; patients who choose surgery initially; patients who are at high risk for perforation with pneumatic dilation
H2RA:
can cause breast enlargement