Public health in neurology and mental health
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
34 Terms
What is public health?
All organized measures to prevent disease, promote health, and prolong life among the population as a whole.
What is health?
A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
What is a disability adjusted life year (DALY)?
One DALY represents the loss of the equivalent of one year of full health
Equation for disease adjusted life years (DALY)
Years of life lost (YLL) + years lived with a disability (YLD).
What are years of life lost (YLL)?
A measure of premature mortality
Equation for years of life lost (YLL)
Number of deaths x standard life expectancy at the age of death
What are years lived with a disability (YLD)?
One YLD represents one full year of healthy life lost due to disability or ill-health
Equation for years lived with a disability
Prevalence of a condition x the condition's disability weight
What is the prevalence of neurological conditions globally?
- 3.4 billion people (42% of the global population) were affected by neurological conditions in 2021
What is the prevalence of neurological conditions in the UK?
Mental health and neurological conditions are the 2nd and 3rd biggest contributors to years lived with disability in the UK
What are the most prevalent neurological conditions globally?
1. Stroke
2. Neonatal encephalopathy
3. Migraine
4. Alzheimer disease and other dementia
5. Diabetic neuropathy
6. Meningitis
7. Epilepsy (idiopathic)
8. Preterm births
9. Autism spectrum disorder
10. Nervous system cancers
How many adults in the UK have a mental health condition?
- 1 in 6 adults have experienced a common mental health disorder in the past week (public health England)
- Severe mental illness e.g. schizophrenia or bipolar affects ½ a million adults in England.
In the UK, what conditions have the highest years lived with disability score (YLD)?
Musculoskeletal disorders and mental and behavioural disorders.
These are most common in the 15-49 year old age group
Who is most affected by suicide in the UK?
- Men < 50 years old and women <35 years old.
- Highest rate of suicide is people aged 50-54 years old
- Men are 3 times more likely to die by suicide than women
What is the life expectancy of someone with a common mental health disorder compared to someone without one?
Mental health disorder e.g. depression and anxiety, people have a 70% higher mortality rate.
Life expectancy of someone with a severe mental illness is 15-20 years less than the general population.
- These can be checked and prevented through annual health checks
How common is it to have a physical co-morbidity with a mental health condition?
- 30% of people with a long term physical condition also have a mental health problem.
- If have mental health disorder, less likely to have treatment of physical health so likely to die from physical health. If have physical health condition, then likely to have a mental health condition due to physical condition.
- 100,000 people die of a physical health condition which is preventable, 1 in 3 have a mental health condition
Describe health inequalities in the UK
- Area: people in the poorest 5th of the population are twice as likely to be at risk of developing a mental health problem than those on an average income
- People with black ethnicity were 3.5 times likely to be sectioned in a mental health facility (under Mental Health Act) compared to their white counterparts.
What are some of the wider determinants of health?
Social economic factors such as:
- loneliness
- employment
- benefits
- housing
What are health inequalities?
Systematic, avoidable and unjust differences in health and wellbeing between different groups of people
How can we prevent health inequalities?
If we can prevent the disease earlier in someone's life, we should.
This can include vaccinating children or addressing mother's post-natal depression.
- We want to intervene at key points in life e.g. as a baby, adolescence, adult, eldery
- We want to target different generations
How do health inequalities relate to pharmacy?
The RPS (Royal Pharmaceutical Society) say that as pharmacists we should ensure that patients' mental healthcare is as good as out physical health care and that patients with mental health conditions get adequate physical health treatment too.
What are the three domains of public health?
1. Health promotion - improving health and wellbeing
2. Healthcare and public health - improving the quality of health services
3. Health protection - preventing harm
How can we prevent harm (health protection)?
1. Vaccination
- For example, meningitis to prevent deaths from meningitis.
- Need people to trust vaccination system
- One thing which affects it is recommendation from a public health professional e.g. pharmacist recommending a vaccine makes people more likely to use it .
2. Preventing falls
This prevents head injuries in the elderly; reduces chance of seizures.
3. Preventing suicide
Pharmacists see patients 31 times more than GP. The increased frequency of contact means we have more chances to intervene in poor mental health.
We can ask someone: are you thinking about killing yourself or suicide? Through this we can check if someone is suicidal and can refer them.
What is mental wellbeing?
Feeling good in yourself and being able to function. This represents the positive side of mental health, not the absence of mental illness.
How do we promote health (health promotion)?
1. We can signpost patients to different resources and services e.g. Make Every Contact Count, Mental health first aid, Every Mind Matters, 5 ways to wellbeing.
5 ways to achieve wellbeing
- Connect
- Notice
- Be active
- Keep learning
- Give
2. Proportional universalism
3. Annual physical health check for people with severe mental illness
- Invite people
- Screen AND intervene
- It is good to get health variables measured but we need to also intervene through either advice, sign posting etc.
What are the determinants of brain health?
1. Physical health
e.g. improve by: stop smoking, improving cardiovascular health, exercise
2. Health environment
3. Safety and security
4. Learning and social connection
5. Access to quality services
e.g. improve by: social prescribing
What is social prescribing?
Connecting patients to local non-clinical services to improve physical and mental wellbeing.
Give some examples of social prescribing
- Community gardening initiatives
- Exercise classes
- Mental health support sessions
- Social activities combating loneliness
- Support with financial stress, housing or employability
What is proportionate universalism?
When we deliver a service to everyone and provide the universal services at a scale and intensity proportionate to the degree of need - for example, more deprived areas will get more of the service as they need it.
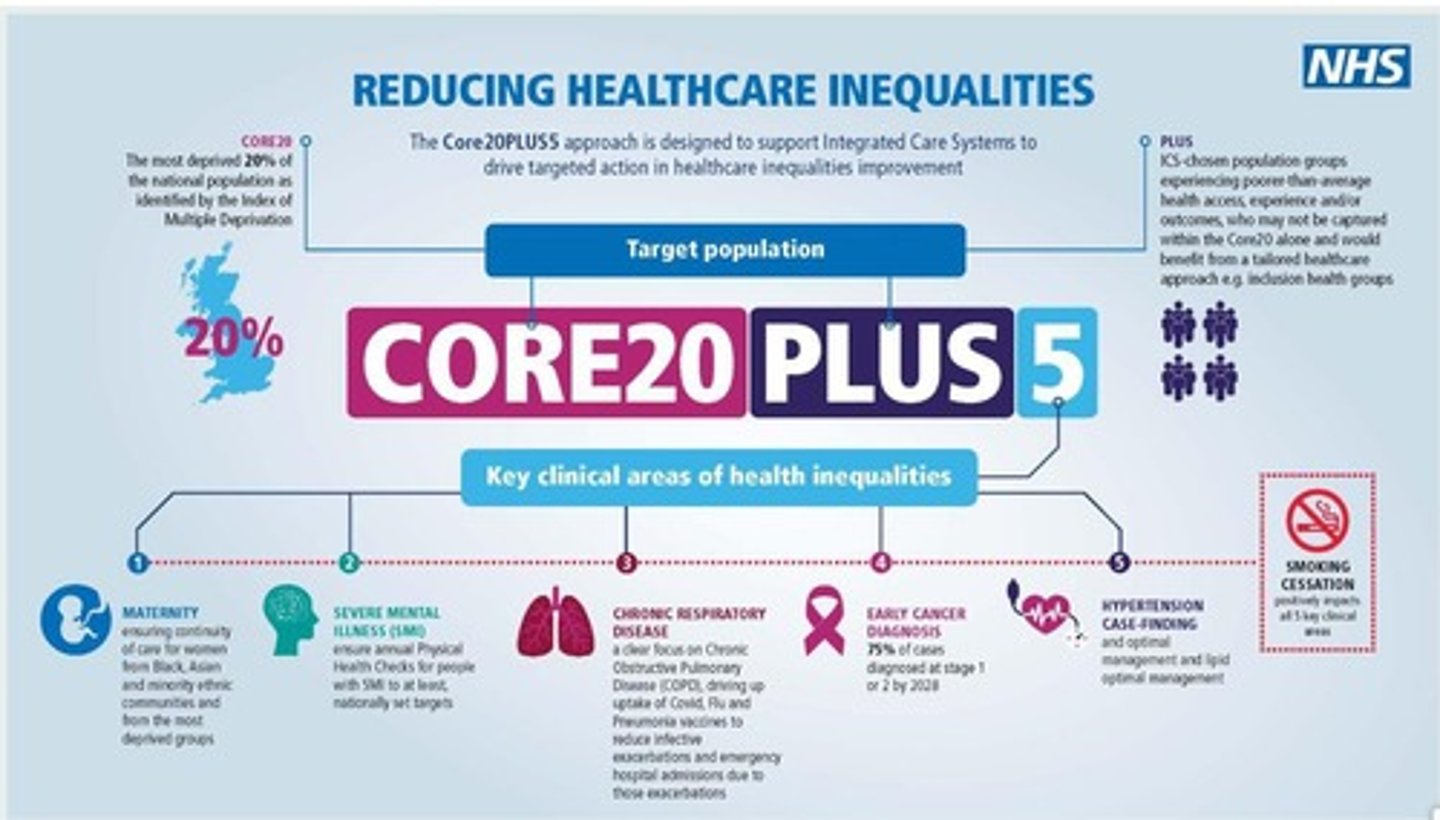
What is the CORE20PLUS5?
1. A new NHS plan to tackle inequalities. Data used from local areas will identify the most deprived 20% households who will be targeted to improve their health.
2. 5 key areas of focus: pregnancy, mental health, cancer diagnosis rate, hypertension and chronic respiratory disease.
How do we improve the quality of health services (healthcare and public health)?
1. Inclusive services
For example, dementia friends initiative.
This is training from the Alzheimer's association . - There is a dementia friendly pharmacy tool kit e.g. environment, training systems, lifestyle advice, prescription support, medicines adherence, signposting to support.
- Can make environment more inclusive for patients with different conditions
2. Screening, when it is evidence-based and done correctly, can save lives.
Why may screening not be the best way to improve health services?
1. False positives may present
- may cause worry in people by saying they are at risk of something, when they are not.
2. False negative may present
- may miss/ not count people who are at risk of the disease
- gives patient false assurance
What role can pharmacists have in global health inequalities?
1. Promotion of essential medicines
- essential medicines e.g. paracetamol, ibuprofen, propranolol, valproic acid and sumatriptan are in varying availability across the globe.
- pharmacists can provide information as to why it is vital that these essential medicines are accessible globally; they could do this through making and changing health policies.
2. Improving local area
- For example, changing the flooring in their pharmacy to make it accessible to patients with Parkinson's disease e.g. making sure it is one continuous colour/ pattern.
What percentage of pharmacists are trained in neurological conditions?
Only 28% of pharmacists are trained in neurological conditions