Pain Midterm
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
Pain definition
an aversive sensory and emotional experience, typically caused by, or resembling that caused by, actual or potential tissue damage
6 notes about pain
Pain is always subjective
Pain is different than nociception
Pain is learned through life experiences
A person’s report of pain should be accepted
Pain is usually protective, but experience of pain could harm function and/or social/psychological well-being.
Pain may be experienced by humans and non-human animals.
What things come together to give a person their pain experience in the biopsychosocial model?
Environment – stimulus
Emotions
Expectations
Genetics
Memories – can be protective or create threat in certain contexts/experiences
Sensory input: nociception!
Ask me 3 tool quiestions
What is my main problem?
What do I need to do?
Why is it important for me to do this?
^to figure out how much your pt knows about their overall health
red flags
Signs/symptoms that may indicate more serious/sinister pathology
orange flag
psychiatric symptoms
yellow flag
psychology, personality related
blue flag
work/job related
black flag
societal factors
depression screening tool
PHQ-2
PHQ-2 cutoff
yes on any question = significant
FABQ cutoff
FABQ-PA >15
FABQ-W >34 (poor prognosis of return to work)
PCS cutoff
>30/52
TSK cutoff
>37/68
GAD-2 cutoff
>3 pts
GAD-7 cut off
>10 pts
PSFS cutoff
MDC - 3 pt change
anxiety disorder screening tool
GAD-2
GAD-7
pain catastrophizing outcome measure
PCS
kinesiophobia outcome measure
TSK
what are the key pain science principles expressed in the NPQ-R
CANNOT have pain and not know it!
Pain is NOT a sensation, receptors detect chemical, temperature, and mechanical info (there are NO PAIN RECEPTORS). Pain is an alarm.
“Hurt does not equal harm” Pain does not only occur when you are injured or at risk of being injured.
When body is injured, receptors convey ‘danger’ messages to your SC. Nociceptors transmit “danger” messages to SC.
Special nerves in your SC convey “danger” messages to your brain.
Nerves adapt by increasing their resting level of excitement. Nerves/nociceptors can become sensitized or can wake up. Can wake up their neighbors so the alarm system becomes more sensitive.
Chronic pain does NOT mean that an injury hasn’t healed properly. Hurt does not equal harm.
Worse injuries do NOT always result in worse pain. Pain relies on context. Ex: red light – patients felt more pain.
CNS can INHIBIT or FACILITATE.
Pain does not always mean you are injured. Or you can be injured and not have pain.
Pain depends on the environment/context.
The pain decides when you will experience pain. “Pain is in the brain.”
what is Pain neuroscience education (PNE)
Use of stories and metaphors to teach about pain
“Pain treatment” > move towards living without pain.
Based on the biopsychosocial model of pain
Depends on the skill of the clinician teaching it.
PNE is NOT
Not just advise movement despite pain
Not cognitive behavioral therapy.
Not cognitive/behavioral advice
Not a denial that nociceptive input can contribute to pain as an output.
PNE metaphors
“Alarm system”
Pain vs function
Envelope of function (avoiding boom/bust)
Can you describe the narrative review findings from Bunzli et al., 2023 regarding patient beliefs/narratives and pain and function for individuals with knee OA?
Broken machines narrative is impairment focused while an active bodies narrative is participatory focused.
placebo definition
I shall please
Causes positive effects
Images of STRENGTH
Body FUNCTION
Focus on ABILITY
Nocebo definition
I shall harm
Causes negative effects.
Images of WEAKNESS, PAIN
Body ILLNESS
Focus on DISABILITY
Why does AAOMPT oppose the use of the term degenerative disc disease
Recent evidence highlights the potential negative impact these diagnostic labels can have on patient outcomes. Relying on diagnostic anatomical labels to describe natural age-related changes, to guide interventions, and to inform activity recommendations can adversely affect patient outcomes”
lateral spinothalamocortical pathway
transmits sensory/discriminative aspects of pain
where
what
how strong
medial spinothalamocortical pathway
transmits emotional/affective aspects of pain
affect
memories
emotions
wide dynamic range neurons
register reponses that are noxious and non-noxious
1. Majority of lateral system neurons
2. Respond to noxious and non noxious stimuli
3. Increased spontaneous firing rates in elevated pain states/processing models
acute pain
1. Known MOI <3 months duration
2. Proportional to tissue load/stage of healing
3. Primarily “nociceptive” mechanism
4. Protective/adaptive
5. Have central INHIBITION
Periaqueductal gray
Rostroventromedial medulla
Parabrachial nucleus
Dorsal reticular nucleus
chronic pain
1. MOI variable >3 months duration
2. Disproportionate to tissue load/stage of healing
3. Primarily “nociplastic” mechanism
4. “disease state”/maladaptive
5. Increased WDF firing
6. Loss of inhibitory interneurons
7. Reduced central inhibition – so central FACILITATION
Amplified response to peripheral input
Longer response duration
“hyperexcitability”
8. Cortical reorganization
What factors may predict the transition from acute to chronic pain? Why might these be important to identify (and HOW might you identify them in your PT evaluation)?
Dyesthesia
An unpleasant abnormal sensation, whether spontaneous or evoked (ex: allodynia and hyperalgesia are dysesthesias)
paresthesia
An abnormal sensation, whether spontaneous or evoked
anesthesia
absence of sensation
hypoaesthesia
decreased sensitivity to stimulation
hyperaesthesia
increased sensitivity to stimulation
allodynia
pain caused by a stimulus that does not normally provoke pain
hyperalgesia
increased pain from a stimulus that normally provokes pain
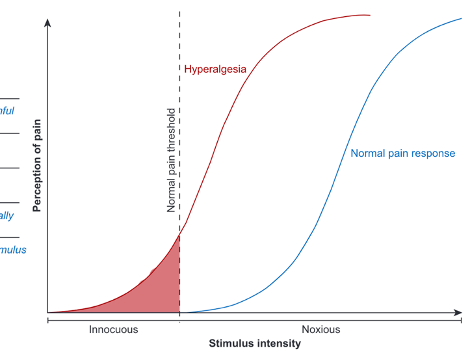
peripheral sensitization
Increased responsiveness and reduced threshold of nociceptive neurons in the periphery to the stimulation of their receptive fields
central sensitization
Increased responsiveness of dorsal horn (spinal cord) neurons (e.g., “wind up” or temporal summation).
conditioned pain modulation
The ability of descending pain inhibitory mechanisms (central) to effectively inhibit pain following a painful stimulus
temporal summation
Increased pain response to repetitive noxious stimuli
primary hyperalgesia
1. Increased responsiveness of primary afferent nociceptive neurons following tissue injury and related persisting pain (happens as early as a few days)
2. Due to PERIPHERAL sensitization
3. Protective/adaptive response from nervous system to prevent further damage/use of area of tissue injury
Secondary hyperalgesia
1. Increased responsiveness of dorsal horn neurons localized in the spinal segments of the primary source of nociception
2. Due to CENTRAL sensitization
3. Could help explain spreading pain
homosynaptic facilitation
1. Repeated peripheral input sensitizes dorsal horn projection neurons in nociceptive pathway
2. Process proprosed to contribute to PRIMARY HYPERALGESIA
heterosynaptic facilitation
1. Intraneuronal facilitation of adjacent spinal projection pathways
2. May explain expansion of pain beyond the area of insult/injury
3. Process proposed to contribute to SECONDARY HYPERALGESIA
Nosy neighbors
nociceptive pain definition
Pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors. Aka “tissue damage”
nociceptive description
1. Proportional
2. Provokable
3. Periodic
4. Predictable
nociceptive patient outcome measures
1. VAS (MCID:20)
2. NPRS – numeric pain rating scale (MCID: 2)
neuropathic pain definition
Pain caused by a lesion or disease of the somatosensory nervous system. Can be to PNS or CNS but must be part of somatosensory system (cerebellum lesion would not qualify). aka “nerve injury”
neuropathic pain description
1. Subjective/history (of nerve injury)
2. Sensory deficits (dermatomal pattern)
Stretching the nerves (provokes symptoms
neuropathic patient outcome measures
1. S-LANSS - self-reported leeds assessment of neuropathic symptoms (> 12 – likely neuropathic component)
2. Pain DETECT (>19 – likely neuropathic component)
nociplastic pain definition
Pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain. Aka “sensitization”
nociplastic pain description
1. Disproportionate pain
2. Disproportionate agg/ease factors
3. Diffuse pain (or palpation tenderness)
4. Distress (psychosocial issues)