Female Reproductive System
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Organization of the female reproductive system
Primary sex organs: gonads
Ovaries
Production/storage of gametes (oocytes)
Hormone production
Secondary sex organs:
Internal genitalia
Uterine tubes
Uterus
Vagina
External genitalia
Vestibule
Labia minora
Labia majora
Mons pubis
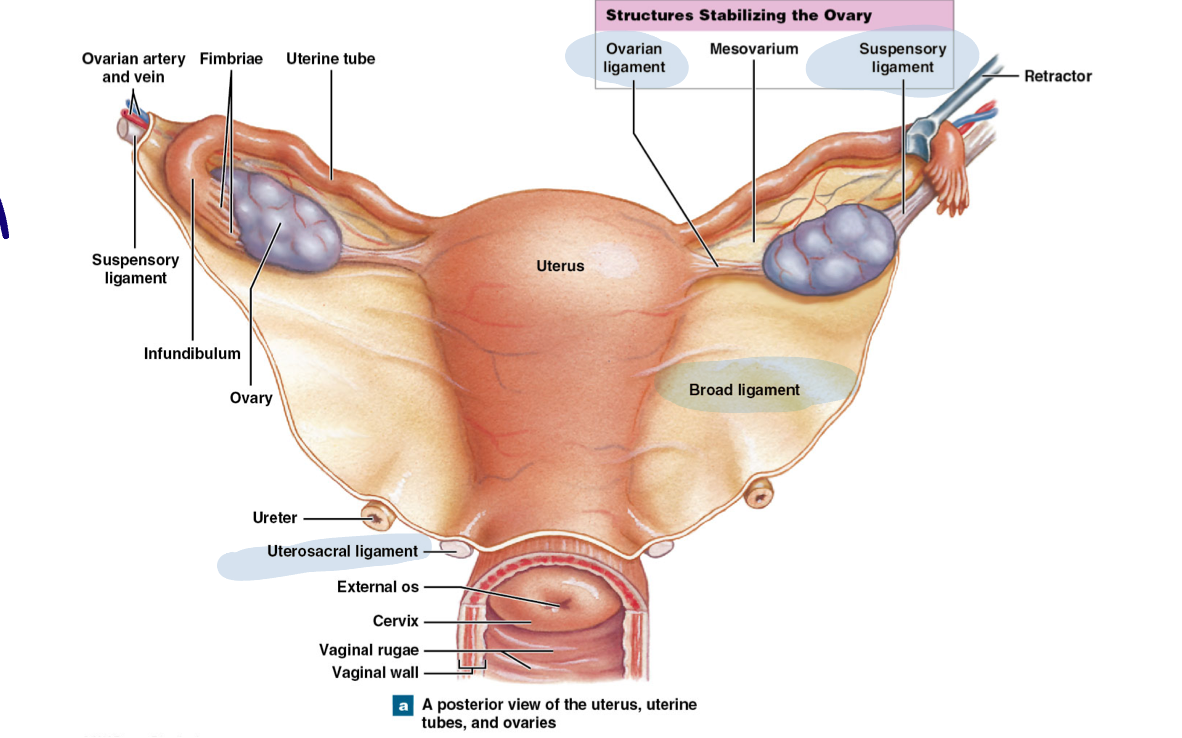
Supporting structures
Broad ligament: fold of peritoneum that covers the uterus and uterine tubes and attaches to walls of pelvic cavity
Ovarian ligament: attaches ovary to the uterus
Suspensory ligament: attaches ovaries laterally to pelvic wall
Uterosacral ligament: attaches uterus to sacrum
Uterine prolapse
The uterus slips into/protrudes out of vagina
Can occur as ligaments wear and stretch
Ovaries
Outer cortex and inner medulla
Medulla: blood/lymph vessels
Cortex contains:
Follicles: an oocyte with surrounding cells (granulosa and theca cells)
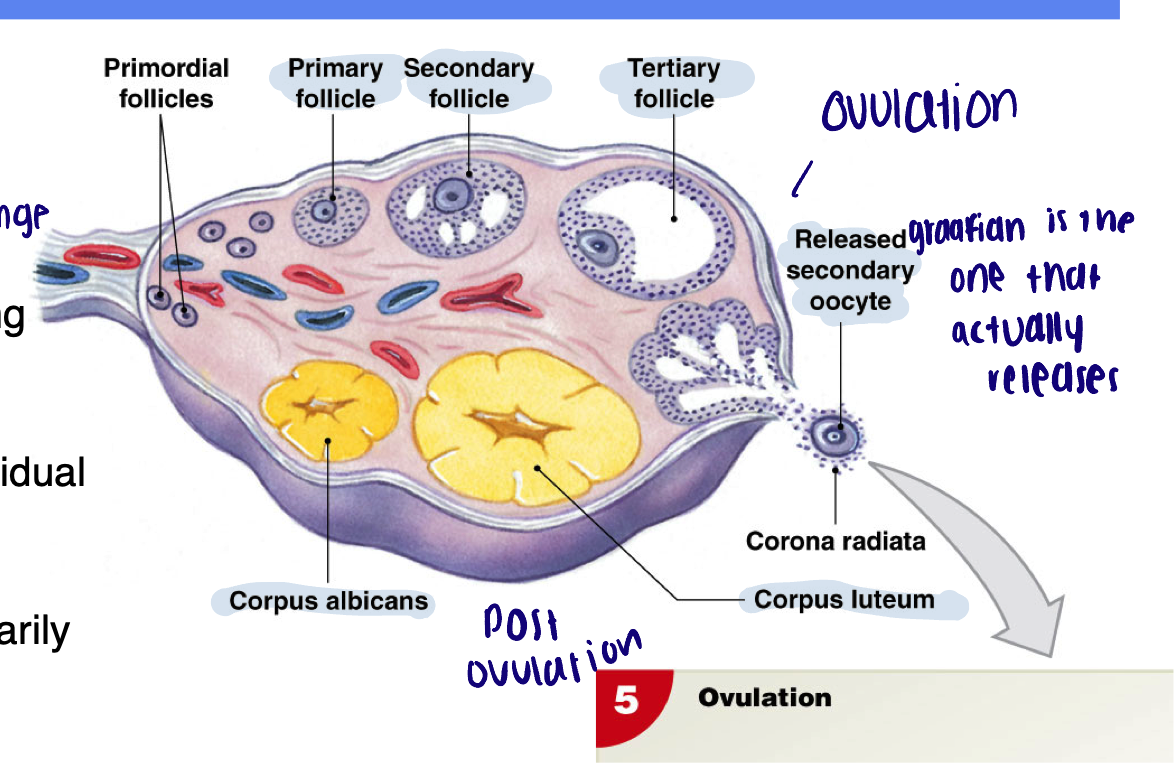
Corpus luteum “yellow body”: residual structure remaining after a follicle empties its oocytes during ovulation
Produces hormones (primarily progesterone)
Corpus albicans “white body”: residual structure formed when corpus luteum breaks down and is no longer functional
Follicles
Oocytes in different stages of development surrounded by specialized cells that produce hormones and support oogenesis
Overview of oogenesis
Primordial germ cells → oogonia → primary oocytes → secondary oocytes → ovum
In utero (oogenesis)
Germ cells develop into oogonia
Oogonia enter Meiosis I and freeze in prophase I (primary oocytes)
Puberty (oogenesis)
Menstrual cycle begins - once a month, select primary oocytes complete Meiosis I and generate 1st polar body
Secondary oocyte is formed (haploid with duplicated chromosomes)
Meiosis II begins - freeze in metaphase II
Secondary oocyte is ovulated
Fertilization (oogenesis)
Meiosis II completes
Formation of second polar body
Folliculogenesis
Follicular maturation → begins in… and completes during…
Development of follicles
Follicular maturation: begins in utero and completes during menstrual cycle
Primordial follicles
Primary follicles
Secondary follicles
Tertiary follicles
Graafian follicle
Primordial follicles
Form in utero
Single layer of cells surround the primary oocyte → granulosa cells (majority of follicles at any one point)
Primary follicles
Sporadically form from primordial follicles
Granulosa cells enlarge
Secondary follicles - requires what and when
Requires gonadotropins (therefore onset of puberty and onward)
Granulosa layer thickens
Outer layer of cells develop → theca cells
Tertiary follicles
Ongoing stimulation by gonadotropins
Thecal and granulosal layers continues to develop
A fluid filled antrum forms
Graafian follicle
The follicle that will ovulate during the menstrual cycle
Oocyte now connected to the rest of the follicle by a stalk
Uterine tubes (oviducts)
Around 5 inches in length, smooth muscular tubes lined with ciliated epithelium
Infundibulum: funnel shaped segment adjacent to ovary, has finger like projections called fimbriae. Ovulated oocyte enters uterine tube at the infundibulum
Ampulla: mid portion of the tube, the ampulla is the usual site of fertilization of oocyte
Isthmus: segment that connects to the uterus
An early embryo travels down the uterine tube and implants in the uterus approximately 5-9 days post fertilization
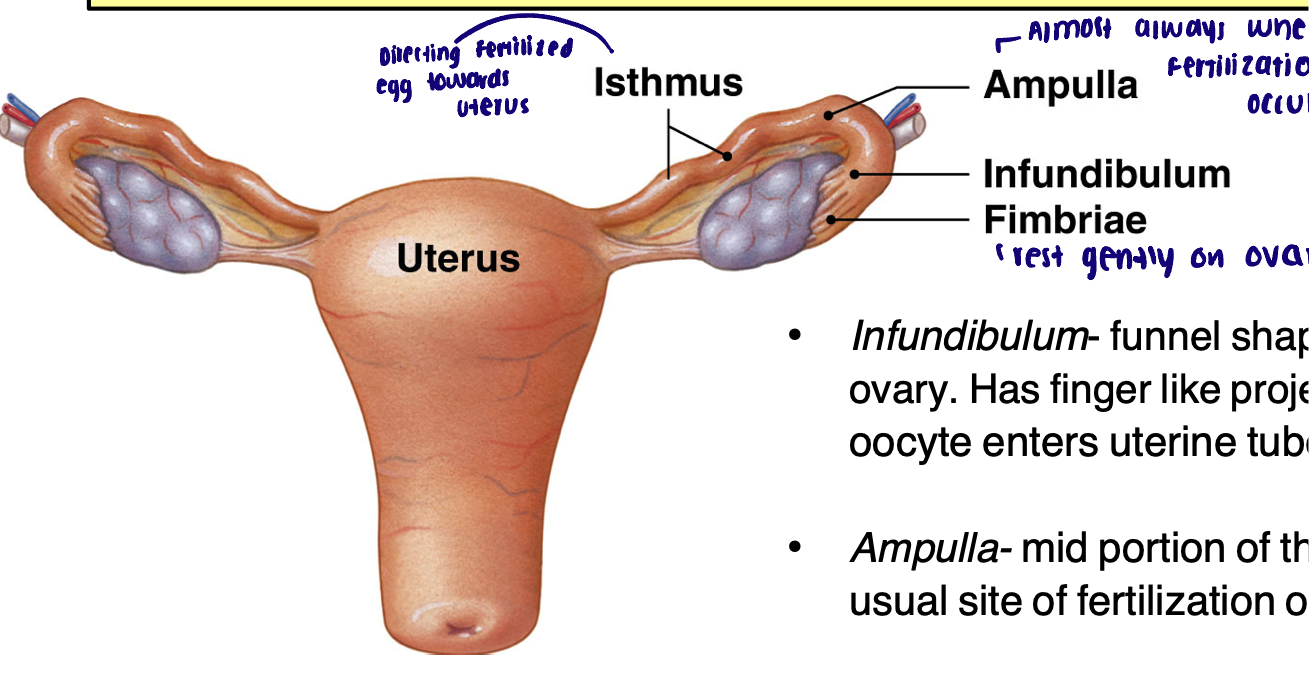
Ectopic pregnancy
Pregnancy outside the uterus, a common site for ectopic pregnancies is the uterine tube, a life threatening condition
Anatomy of the uterus
Three regions
Three layers of uterine wall
Three regions
Fundus: rounded portion above entrance of uterine tubes
Body: largest region of uterus
Cervix: most inferior, narrowed region of the uterus
Internal os: opening to the uterine body
External os: opening to vagina
Three layers of uterine wall
Endometrium: inner layer of epithelial cells, uterine glands, underlying stroma
Myometrium: smooth muscle layers - (longitudinal, circular, and oblique)
Perimetrium: serosa layer of outer surface
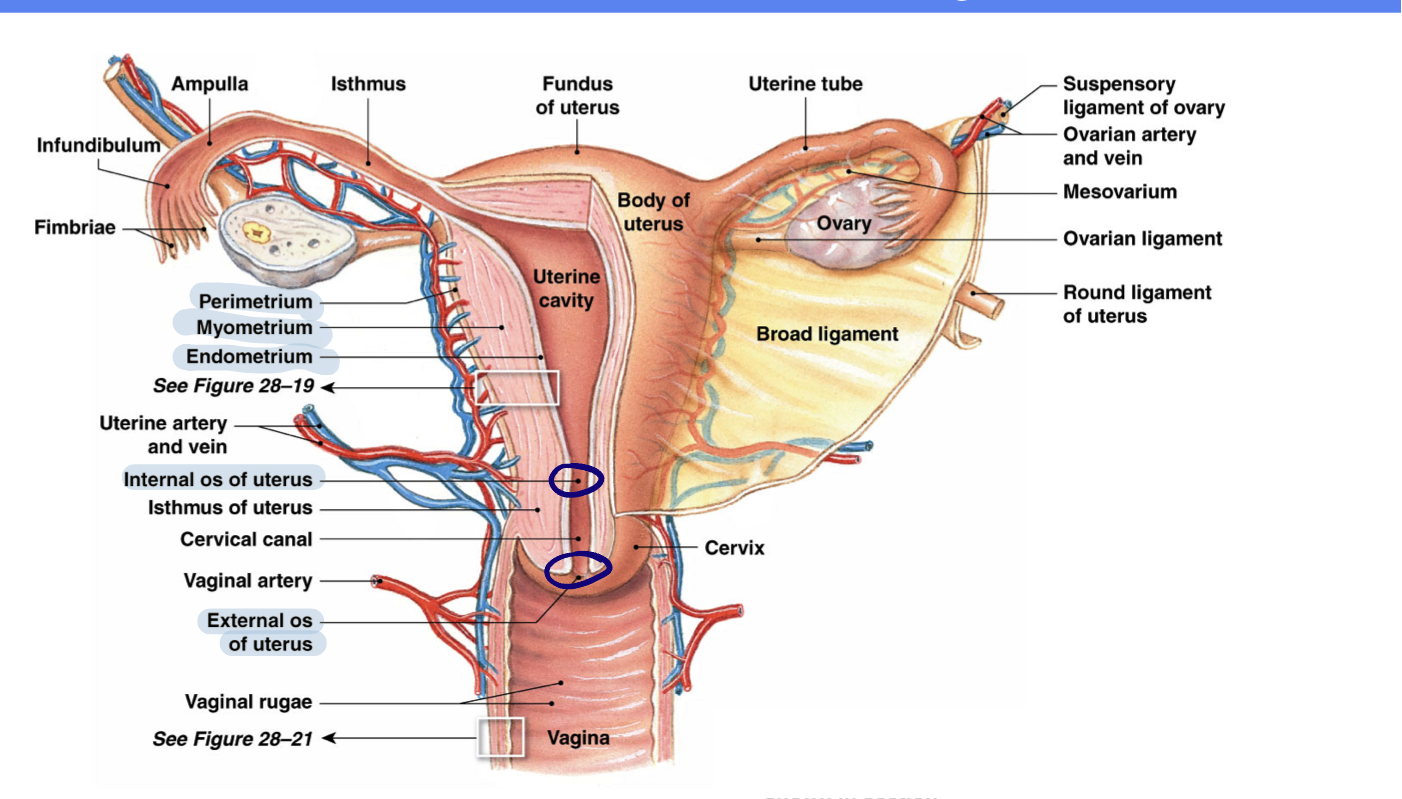
Blood flow of the uterus
Uterine arteries (L and R) → Branches of uterine arteries → Arcuate arteries → Radial arteries → → Straight (feeding basilar) and Spiral arteries (feeding functional)
What is the endometrium divided into
Basilar zone (stable)
Functional zone (variable)
What is the vagina and what does it consist of
Hollow, distensible muscular tube around 3-5 inches in length, walls are arranged into rugae
Vaginal mucosa: stratified, squamous epithelium and underlying lamina propria
Vaginal muscularis: smooth muscle layer, loosely arranged in circular and longitudinal layers
Vaginal adventitia: outer layers of dense and connective tissue and elastic fibers
Vestibular glands: near the vestibular opening, produce and secrete lubricating mucous particularly during sexual arousal
Hymen: elastic epithelial fold that partially covers the vaginal opening
External genitalia
Vulva: term that refers to external genitalia collectively
Mons pubis: fatty region that overlies pubic symphysis
Labia majora: outer protective folds (develop from same embryonic tissue as the scrotum in males)
Labia minora: inner protective folds; mucous membrane and richly supplied with glands and blood vessels
Vestibule: area enclosed by labia minora
Vaginal orifice: opening of vagina
Urethral orifice: opening of urethra
Clitoris: erectile tissue, rich in nerves; glans (visible) and body (deep)
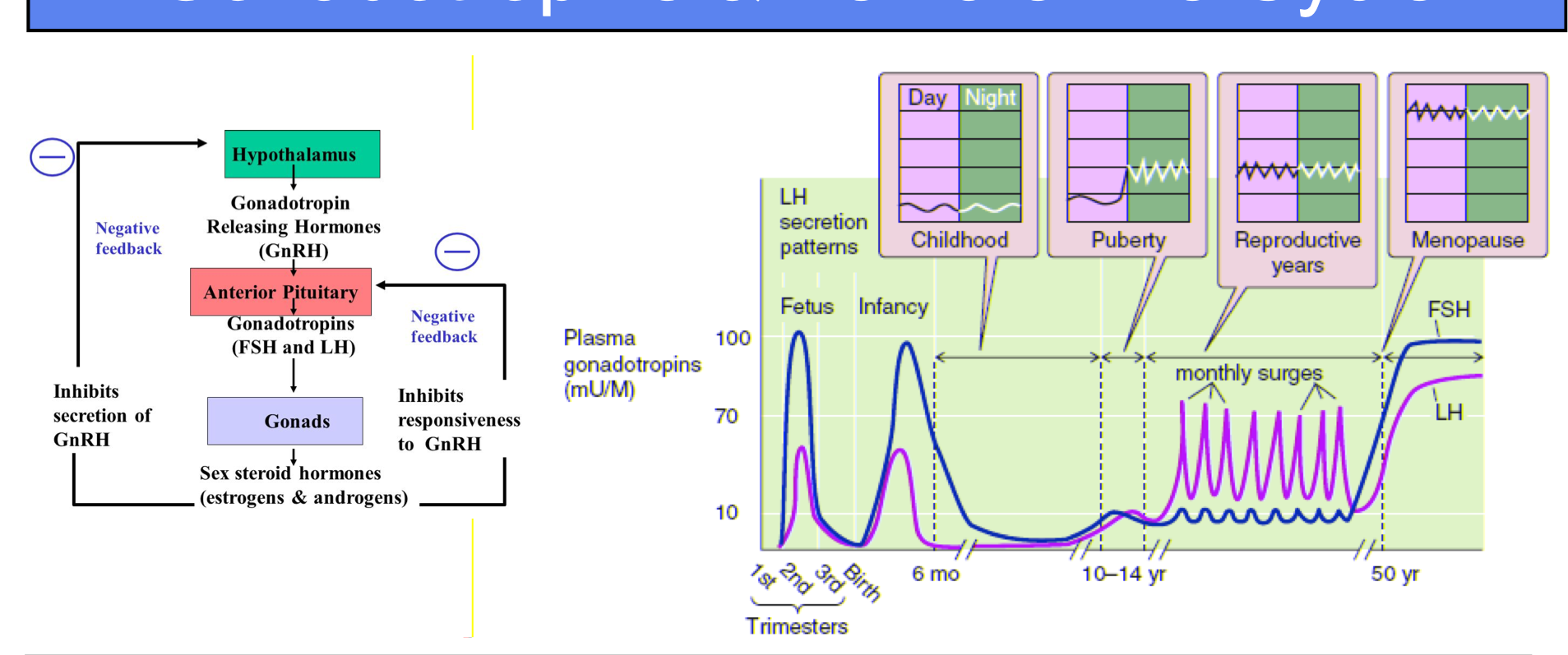
Gonadotropins and female life cycle → in utero/early infancy
In utero/early infancy: peak in gonadotropin release - second trimester and early infancy
Gonadotropins and female life cycle → in childhood
In childhood: low levels of gonadotropin release
Gonadotropins and female life cycle → Puberty
Puberty: nighttime pulsatility of GnRH release
Menarche: first menstruation around 13 years of age
Gonadotropins and female life cycle → In reproductive years
Reproductive years: ongoing pulsatility of GnRH release, monthly surges of gonadotropins and cyclic pattern of estrogen and progesterone release
Gonadotropins and female life cycle → Menopause
Menopause: decrease in estrogen and progesterone levels due to exhaustion of follicular pool, loss of negative feedback, higher levels of gonadotropins, no monthly surges
Images of gonadotropins and female life cycle
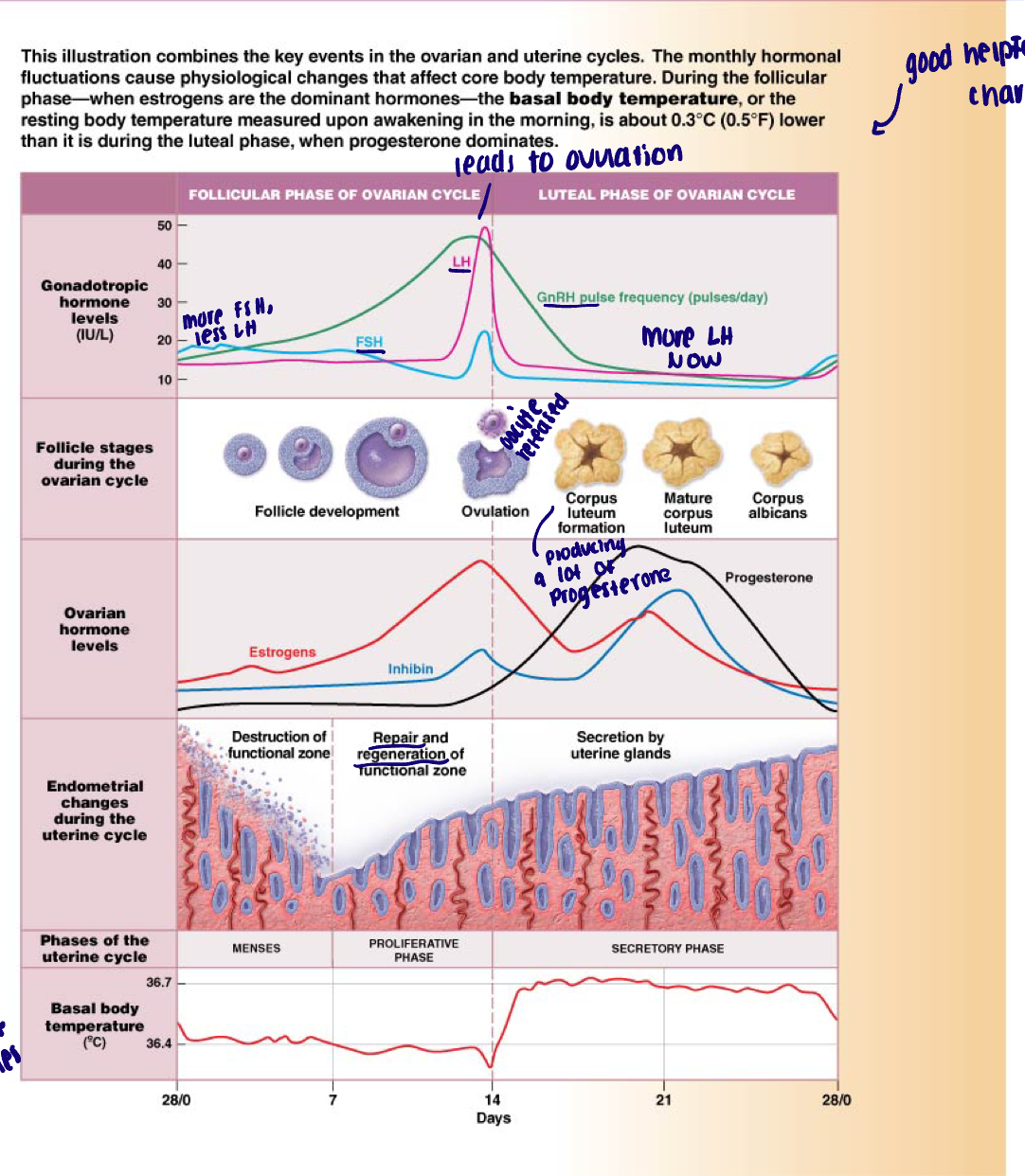
What is the menstrual cycle
Cyclic changes in ovarian hormone production and uterine morphology over around a 28 day period in women of reproductive years
Described according to ovarian changes (ovarian cycle) and uterine changes (uterine cycle)
Uterine changes are a result of changes in production of ovarian hormones
2 phases:
Before ovulation
Ovarian: follicular phase
Uterine: menses and proliferative phase
After ovulation
Ovarian: luteal phase
Uterine: secretory phase
Summary of sex steroids
In the non-pregnant female of reproductive years, the most abundant progestin is progesterone
These hormones primarily originate from the ovary
Androgens:
Biologically active: testosterone
Dihydrotestosterone (DHT)
Estrogens:
Biologically active: estradiol
Progestins:
Biologically active: progesterone
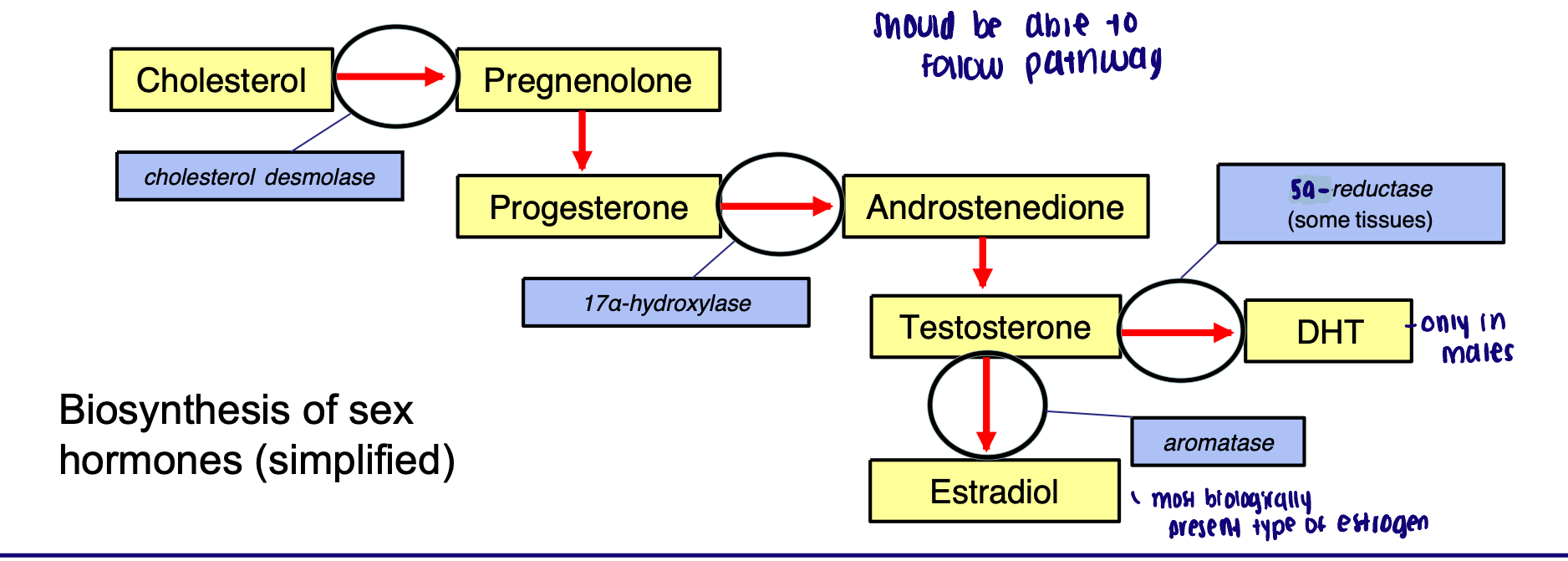
Estradiol synthesis requires…
Two cells (theca and granulosa) and two gonadotropins (LH and FSH)
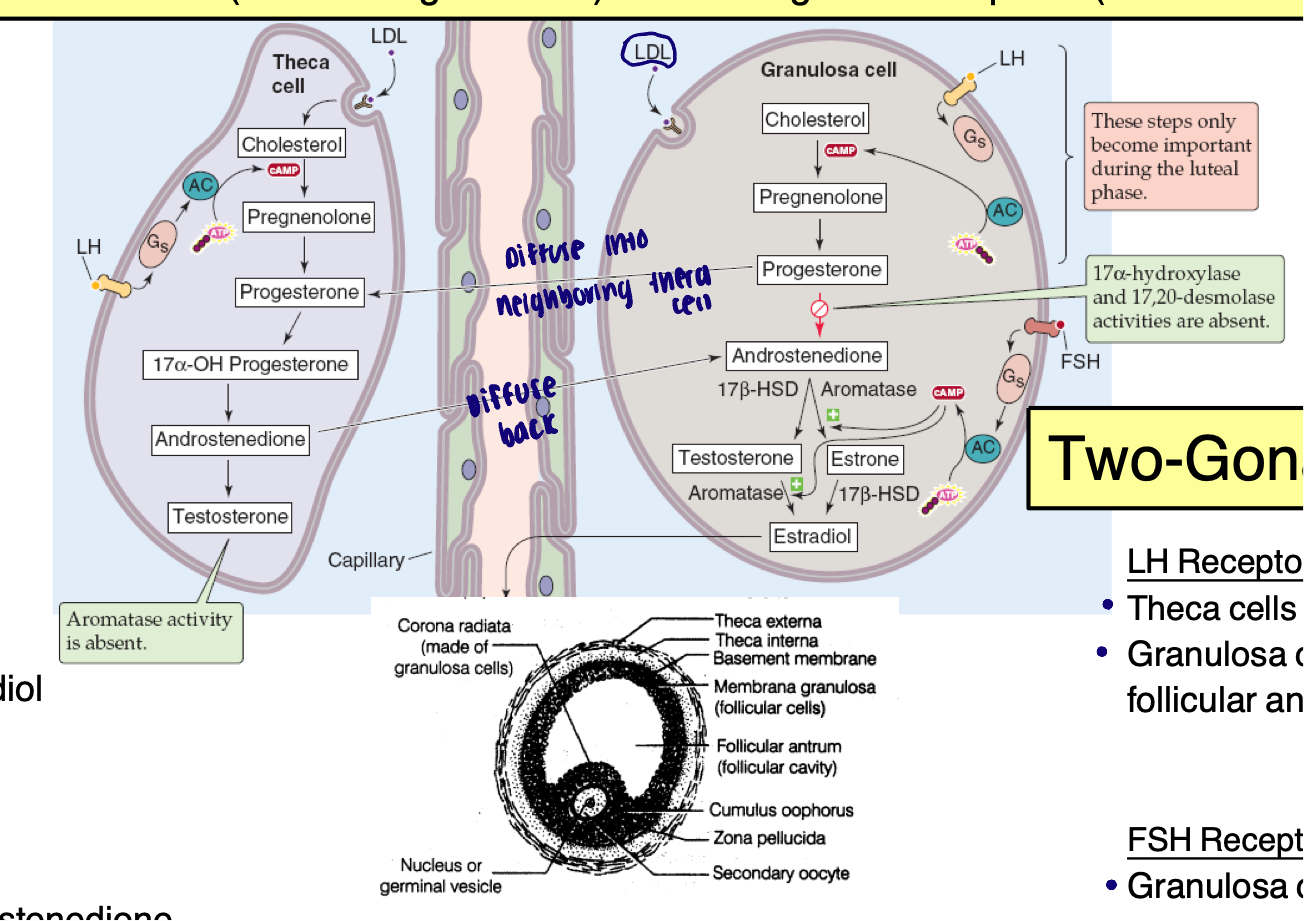
Two cell
Theca cell:
Lacks aromatase
Cannot convert testosterone → estradiol
Granulosa cell:
Lacks 17alpha hydroxylase
Cannot convert progesterone → androstenedione
Theca cell: androstenedione synthesis, diffuses to nearby granulosa cell
Granulosa cell: utilizes androstenedione as a precursor for estradiol synthesis
Two-gonadotropin
LH receptors:
Theca cells (always)
Granulosa cells (late follicular and luteal phases)
FSH receptors
Granulosa cells only
LH: induces cholesterol desmolase enzyme activity (generate progesterone from cholesterol) and LDL receptor expression
FSH: induces aromatase activity
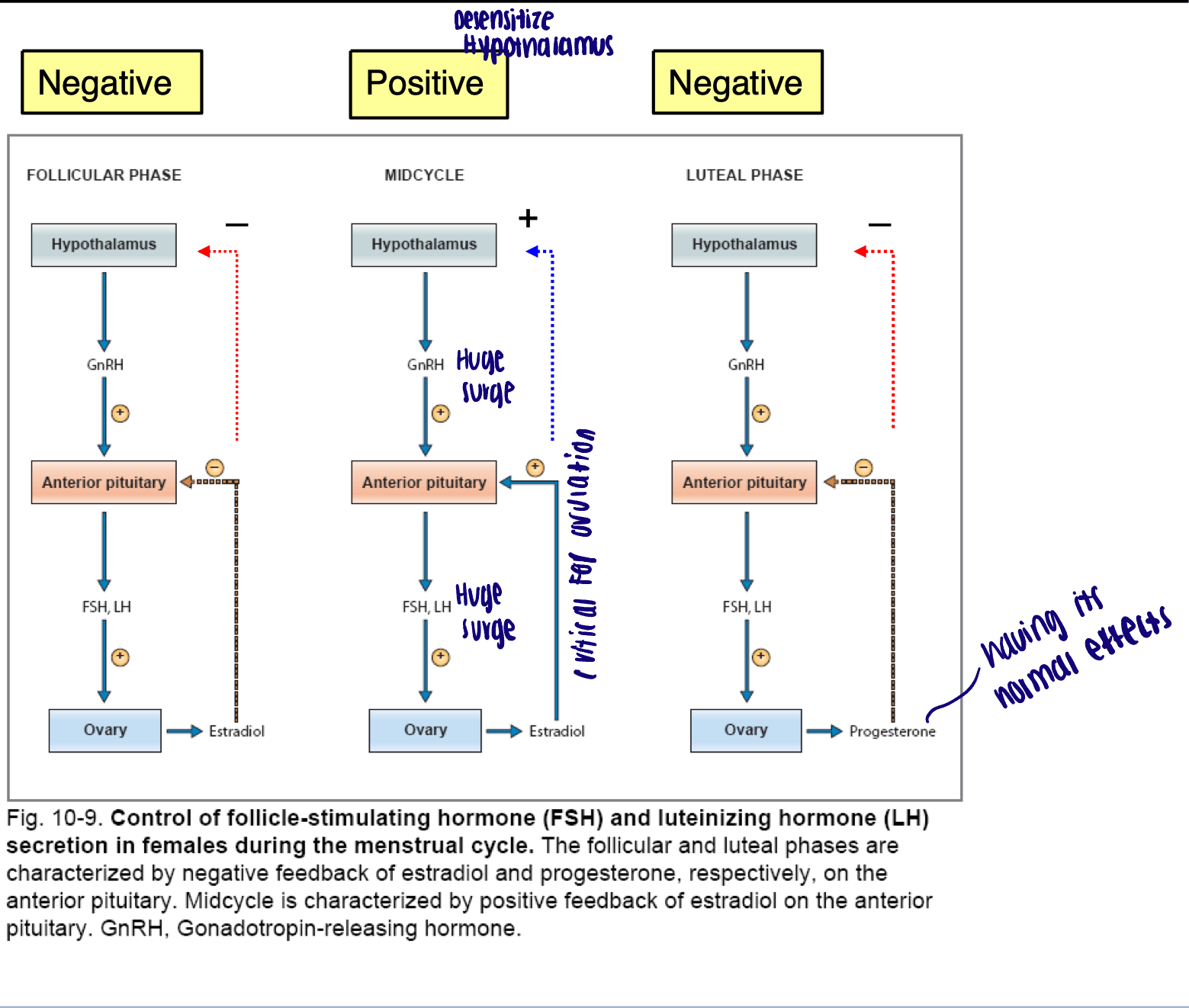
Feedback control of ovarian hormones
What are the main big picture segments of the menstrual cycle
Ovarian Cycle
Uterine Cycle
Broadly → Ovarian cycle
Day 1-14: Follicular phase: FSH
Follicular development of a cohort of follicles (around 7-12) under the influence of FSH
Only one will grow into a Graafian follicle to be ovulated
Rising estrogen production by follicles
Mid-cycle: LH surge due to positive feedback of estrogen
Ovulation and conversion of a Graafian follicle into the corpus luteum
Day 14-28: Luteal phase: LH
Rising progesterone production by corpus luteum
Finite life span of corpus luteum
Uterine Broadly → Uterine cycle
Day 1-7: Menses (days 1-7 of follicular phase)
Triggered by the dramatic decrease of estrogen and progesterone production of ovary
Shedding of endometrial layer
Day 7-14: Proliferative Phase (days 7-14 of follicular phase)
Growth of endometrial layer under the influence of progressively rising estrogen
Day 14-28: secretory phase (overlaps with luteal phase)
Conversion of built up endometrial layer into a secretory structure by the actions of progesterone
What does the ovarian follicular phase consist of
Early follicular phase
Late follicular phase
Early follicular phase
FSH stimulates follicular growth in follicular cohort (7-12 follicles)
Increases aromatase activity (increased estradiol synthesis)
By day 5 one dominant follicle outcompetes others for FSH ultimately becoming Graafian follicle
Rapidly grows and produces increasing higher levels of estradiol
Ovarian follicular phase → effects of circulating estradiol
Increases FSH receptor expression of granulosa cells (leading to further production of estradiol)
Estradiol increases estrogen and progesterone receptor expression in the uterus (estrogen priming)
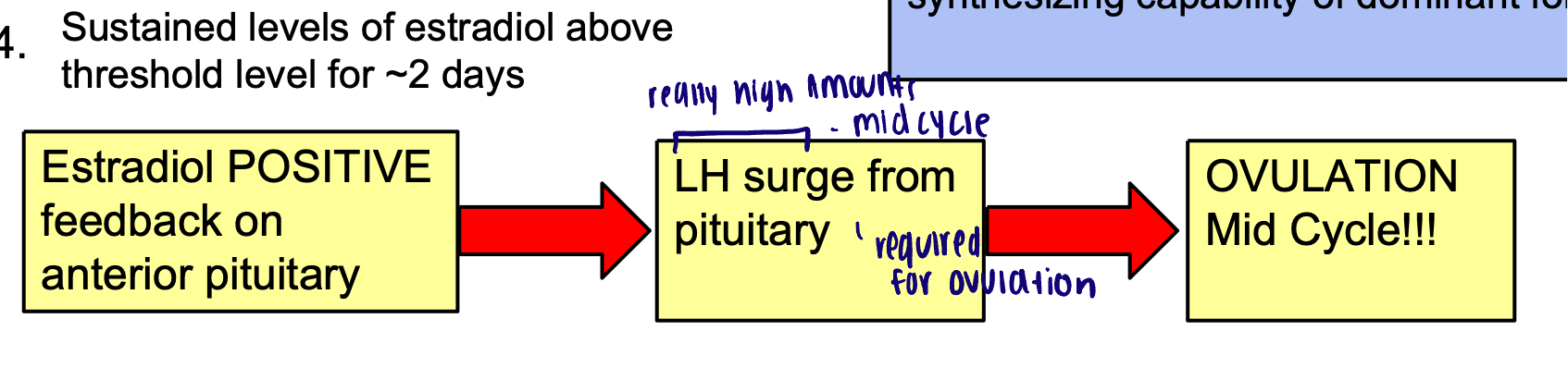
Late follicular phase
FSH induces LH receptor expression on granulosa cells of dominant follicle now responsive to LH
(also increases theca cell expression of LH receptor)
Sustained levels of estradiol above threshold level for around 2 days
Late follicular phase → effects of LH on granulosa and theca cells
Increased LDL receptor expression and cholesterol desmolase activity
Increased available pregnenolone available as precursor for estradiol synthesis
Combined greatly increased estradiol synthesizing capability of dominant follicle
Ovarian luteal phase
LH surge: luteinization
Conversion of emptied follicle into a fluid filled corpus luteum
Abundant cholesterol available to granulosa luteal cells for progesterone synthesis (yellow color)
Granulosa cells now have abundant LH receptors
Granulosa cells of luteum - increased capability of synthesizing progesterone
10 fold increase in progesterone levels during the luteal phase
Progesterone transform uterus into organ capable of supporting developing embryo
Ovarian luteal phase → if no pregnancy occurs
If no pregnancy occurs, there is a finite life span of corpus luteum (14 days)
After the corpus luteum breaks down (corpus albicans):
Progesterone and estrogen levels begin to drop
Decrease negative feedback
FSH levels begin to rise at the end of the luteal phase → recruitment of new cohort of follicles
Uterine cycle: Menses
Menses: loss of hormonal support
Early follicular phase
Shedding of outer endometrial layer (functional zone) accompanied with blood loss due to a decrease in hormonal support
Prostaglandins released by ruptured cells leads to smooth muscle contractions
Onset → 14 days after ovulation, average length: 4-6 days
Uterine cycle: Proliferative phase
Proliferative phase: increasing estradiol
Late follicular phase: increased estradiol
Thickening of endometrial layer:
Proliferation of epithelial cells of the endometrial layer (functional zone)
Increase estrogen receptor expression
Increase progesterone receptor expression: “estrogen priming:
Progressive increase in amount of cervical mucus, mucus thins: spinnbarkeit
Uterine cycle: Secretory phase
Secretory phase: increased progesterone
Luteal phase: increased progesterone
Differentiation of endometrial layer into a glandular epithelium with increased (secretions rich in glycogen and lipids)
Progesterone inhibits contraction of the myometrium
Cervical mucus production decreases, mucus thickens
Late secretory phase: if there is not a fertilized embryo in the uterus, the corpus luteum breaks down → loss of hormonal support: spasm of blood vessels: ischemic phase
Life span of ovulated (non-fertilized) oocyte
24 hours
Life span of spermatozoa within female reproductive tract
3-5 days
Fertilization occurs
Within the uterine tubule (ampulla)
Window of fertility
5 days before ovulation and also the day of ovulation
Fertilization during the cycle
Ovulation occurs → day 14 and fertilization must happen within 24 hours (typically in ampulla)
Zygote reaches the uterus approximately 5-9 days later (around day 19- day 21) → uterus is in secretory phase
Cells of the early embryo produce a hormone called human chorionic gonadotropin (hCG)
Once embryo implants in the uterine wall, this hormone enters the maternal circulation
hCG rescuers the corpus luteum and prevents it from breaking down
The corpus luteum maintains high levels of progesterone to maintain the uterus in a pregnancy friendly state during the first 2-3 months of the pregnancy until the placenta fully forms
Once the placenta fully forms, it takes over the production of maternal hormones needed to maintain pregnancy
CORPUS LUTEUM → PLACENTAL SHIFT