LO5
1/80
Earn XP
Description and Tags
Identify the Supporting Structures of the Teeth
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
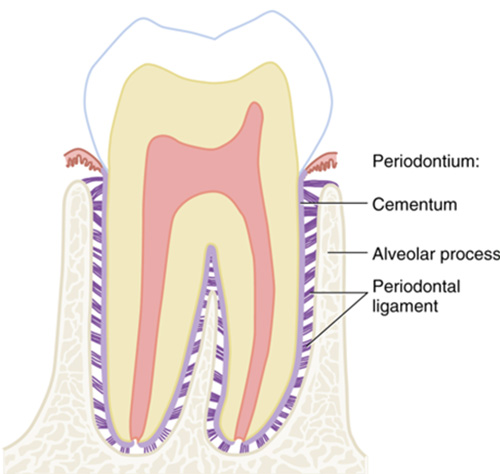
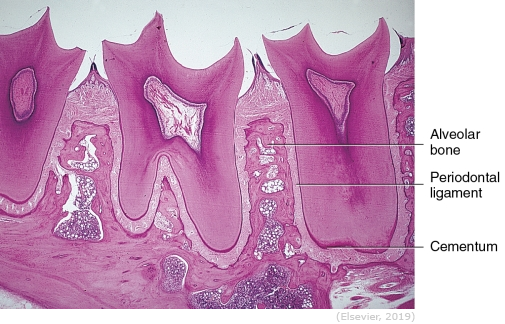
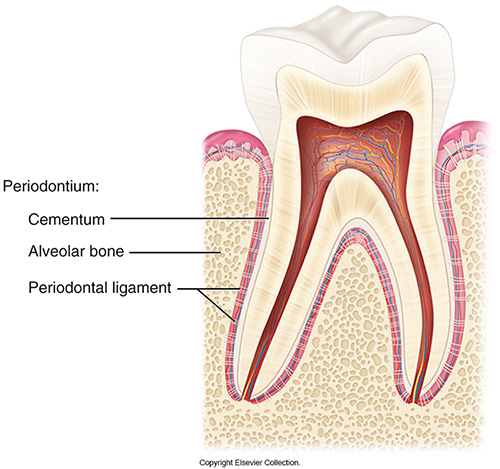
The attachment apparatus
Cementum
Alveolar process
Periodontal ligament
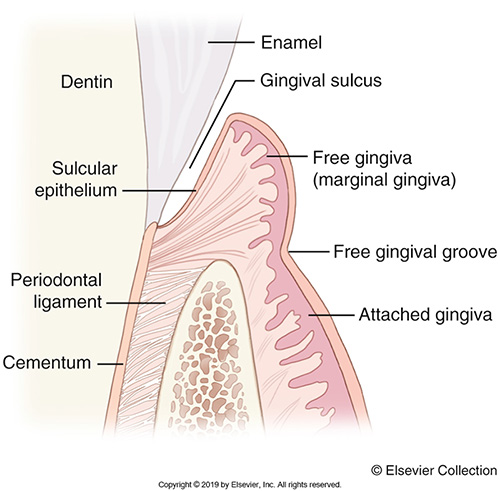
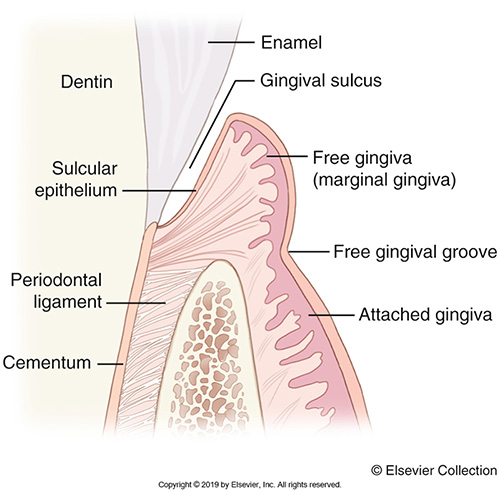
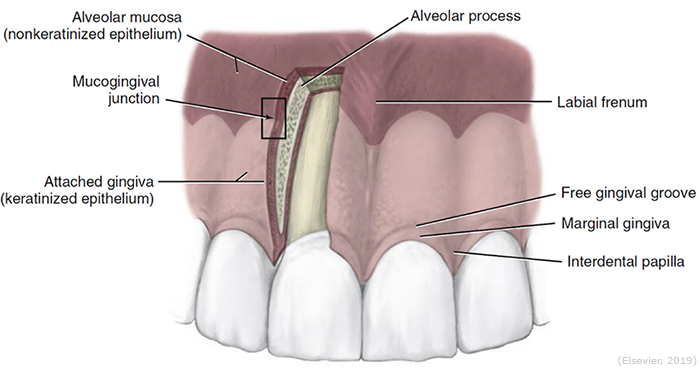
Th gingival unit
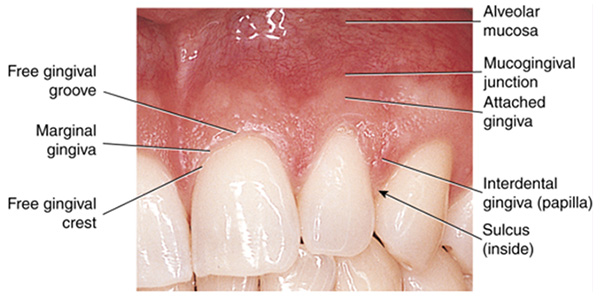
Free gingiva
Attached gingiva
Alveolar mucosa
Cementum
The outermost layer of the root of the tooth
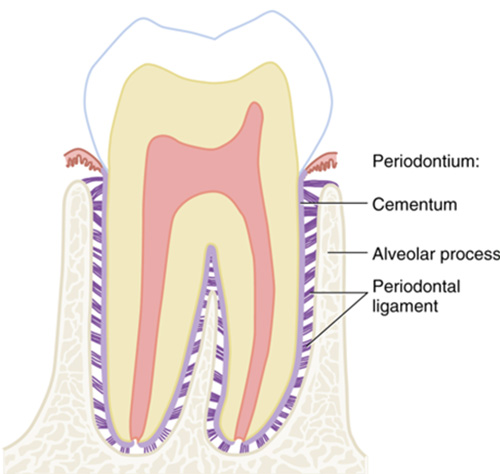
Periodontal ligament
The ligament surrounding the teeth that supports and attaches them to the alveoli bony surface.
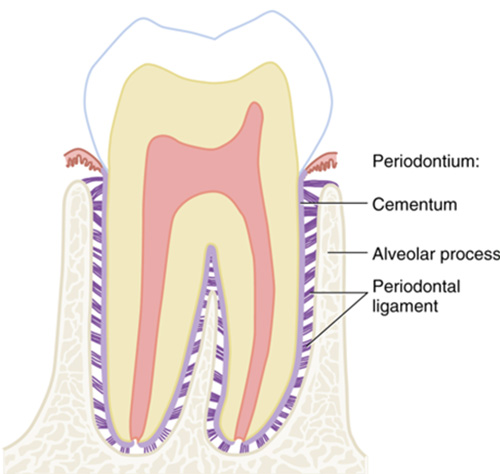
Alveolar process
The dental arch or tooth bearing part of each jaw that contains alveoli.
Free gingiva
The tissue that forms a collar around the tooth
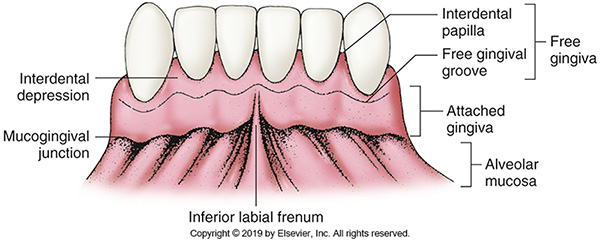
Attached gingiva
Gingiva that adheres tightly to the alveolar process around the roots of the teeth.
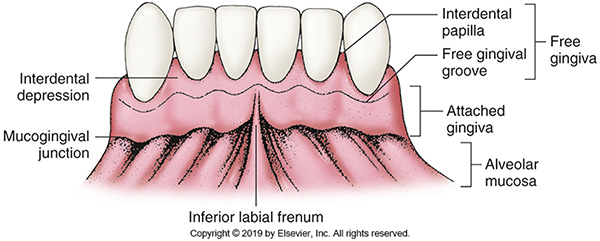
Alveolar mucosa
The oral mucosa immediately apical to the mucogingival junction.

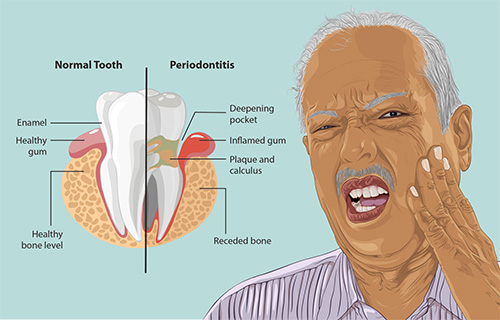
Periodontitis
Is inflammation of the supporting tissues of the teeth. This inflammatory process starts in the gingiva or gums and can spread to the alveolar bone supporting teeth.
Periodontal disease
Is an infectious disease with systemic connections in individuals and several causes.
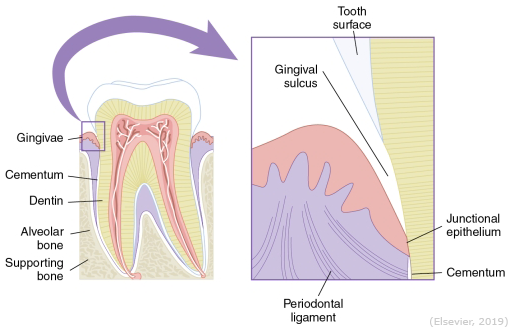
Healthy periodontium
Consists of healthy supporting tissues that include the alveolar bone, cementum, periodontal ligaments, and the gingiva. Healthy gingiva is usually pink or coral pink but may have a brown pigment in individuals with darker skin.
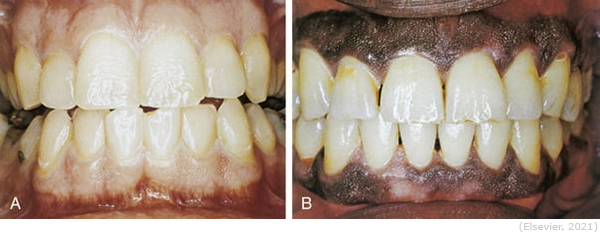
Healthy gingiva
Does not bleed when probed and has surface stippling (looks like an orange peel). The stippling is caused by the connective tissue fibers attaching the epithelium to the underlying bone. The interdental papilla (IP) fills in the area between the teeth up to their contact areas and prevents food from becoming lodged or impacted between teeth.
Unhealthy periodontium
It becomes swollen and blunted. As this happens, the original shape is lost, and it tends to get more irritated when eating, causing more problems. Shows a breakdown of the supporting structures that hold teeth in place. The images below show extensive disease in the supporting tissues as well as bone loss.

First signs of gingival problems in periodontal diseases
A loss of stippling. This is initially caused by swelling or edema of the gingival tissues. In a diseased state, the gingiva may become red-whitish or have ulcerations or outgrowths of the mucosa.

Factors that lead to the breakdown of periodontal tissues and bone
Bacteria
Plaque
Decay
Rough surfaces on teeth
Restorations with overhanging margins
Build-up of calculus

Occlusal trauma
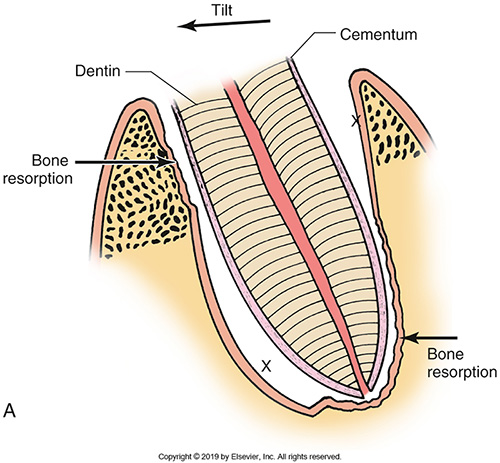
Occurs when specific teeth prematurely contact one another when a person bites together. This is not an ideal situation, as it puts more force on the specific tooth (teeth), leading to tooth fracturing and injury to the periodontal tissues. Maintaining a proper bite after receiving a dental restoration should be done, to ensure that no part of the restoration is hitting prematurely.
Tooth Migration
Occurs when a specific tooth does not have an antagonist tooth to occlude against in the arch. When this occurs, the tooth begins to super-erupt, trying to meet an occluding force. Because of this, supporting tissues will collapse, resulting in bone loss. Replacing missing teeth is important to maintain an ideal occlusal bite. There are several options to do this; partial dentures, fixed bridges and implants are prime examples of tooth replacement.
PDL function
Prevent teeth from being pushed into the bone and minimize the trauma of teeth being pushed together; the adaptability and versatility makes orthodontic treatment possible!
PDL sensory function
The fibers also act as receptors necessary for the proper positioning of the jaws during normal functioning. The fibers allow you to feel light touch and pressure, as well as hot and cold.
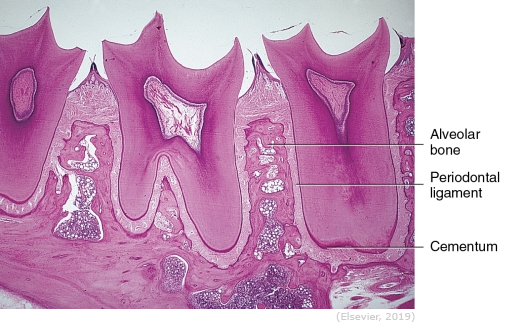
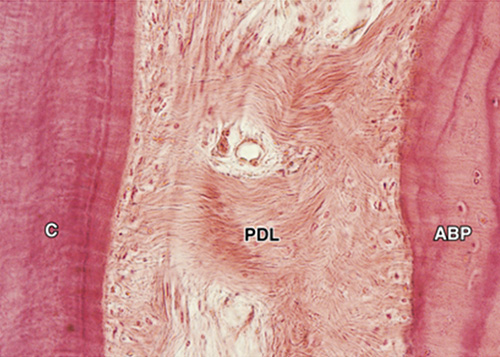
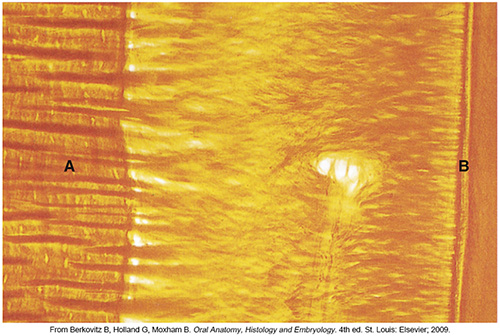
PDL characteristics
Is a component of the periodontium; it is a layer of connective tissue between the bone and the cementum. It is less than 0.25mm in width (averaging 0.12-0.33 mm). It is hourglass in shape – widest at the coronal portion, narrowest in the middle and slightly wider at the apex.
PDL development
Develops from the cells of the middle layer (mesodermal cells) of the dental sac. This occurs after the cementum has begun forming. The dental sac begins to change, and the cells become fibroblasts that form collagen fibers. The fibers are initially parallel with the root surface. Later, they will arrange into fiber groups.
Cells in the PDL
Fibroblasts
Small group of epithelial cells
Cementoblasts
Osteoclasts
Undifferentiated mesenchymal cells
Macrophages
Other cellular components of blood
Fibroblasts
Produce collagen fibers
Small group of epithelial cells
Epithelial rests of Malassez
Cementoblasts
Produce cementum
Osteoclasts
Resorb bone
Undifferentiated mesenchymal cells
Can become other cells of the PDL when needed.
Macrophages
Defensive cells
Other cellular components of blood
Mast cells, eosinophils, and other blood cells
Intracellular substance
A ground substance (proteoglycans and mucopolysaccharides).
Fibers (60% of the PDL).
Makes up the fibers of the PDL, collagen fibers physically constructed to withstand heavy forces.
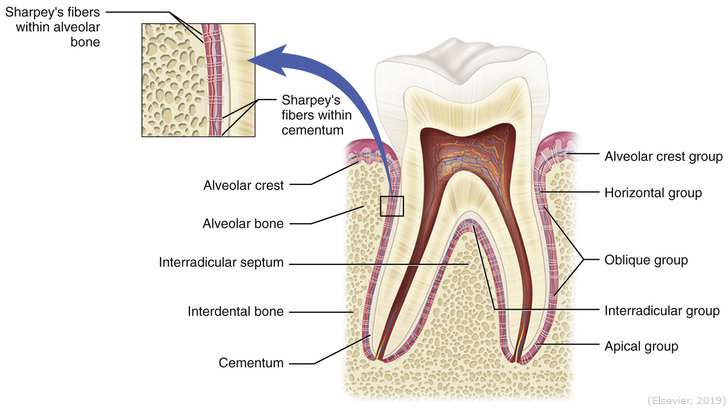
Sharpey’s fibers
Entrapped collagen fiber bundles in cementum or bone. The fibers of the PDL are embedded in the cementum on one end and the alveolar bone on the other end. These embedded potions become mineralized and are called ______.
Other components of the PDL
Blood vessels, lymphatic vessels and cementicles also make up the structure of the PDL. The cementicles are minute calcified bodies that may or may not be attached to the cementum.
Three groups of PDL fiber groups
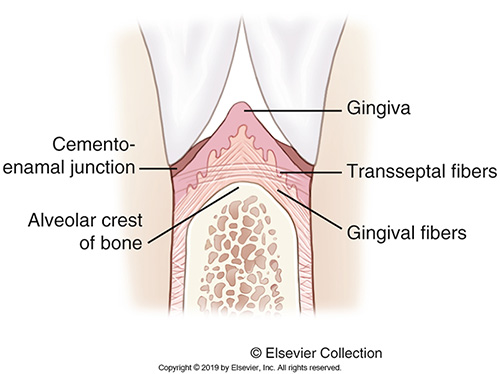
Gingival fibers
Transseptal fibers
Alveolodental fibers
Gingival fiber groups
Support the gingiva that surrounds the tooth.
Contain the following fiber sub-groupings:
Gingival fibers
Circular fibers
Gingival fibers
Run from the cementum to the free gingiva and attached gingiva.
Circular fibers
Run in the free gingiva and hold the gingiva against the tooth by forming a band around the tooth. These are not attached to the bone of the alveolar process.
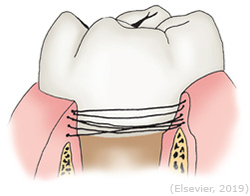
Transseptal or Interdental Fiber Groups
Support the tooth in relation to the adjacent teeth.
Run from the cementum of the interproximal portion of one tooth across alveolar bone to the cementum of the interproximal of the adjacent tooth.
Supports the interproximal gingiva and the position of the adjacent teeth.
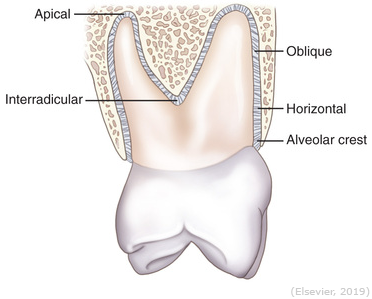
Alveolodental Fiber Groups
Support the tooth in its socket. They run from the cementum to the alveolar bone and contain the following five subgroupings:
Alveolar crest fibers
Horizontal fibers
Oblique fibers
Apical fibers
Interradicular fibers
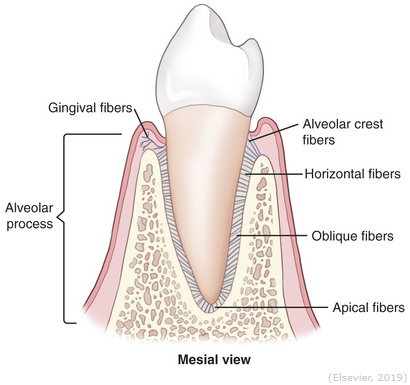
Alveolar crest fibers
Runs from the crest of the alveolar bone to the cementum in the CEJ region.
Retains tooth in the socket and helps resist horizontal movements of teeth.
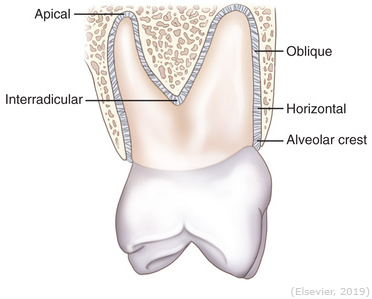
Horizontal fibers
Runs horizontally from cementum to alveolar bone (right angles to the long axis of the tooth).
Restrains lateral tooth movement and helps resist horizontal movement.
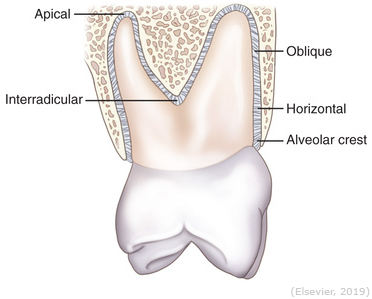
Oblique fibers
Runs upward or coronally from the cementum to bone.
Most numerous fibers and constitute the main attachment to the tooth.
Resists forces placed on the long axis of the tooth and occlusal stresses.
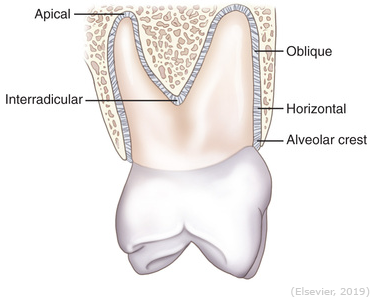
Apical fibers
Radiates outward from the apical cementum to the bone.
Prevents tooth from tipping and twisting or being pulled from its socket.
Protects blood, nerve, and lymph supplies.
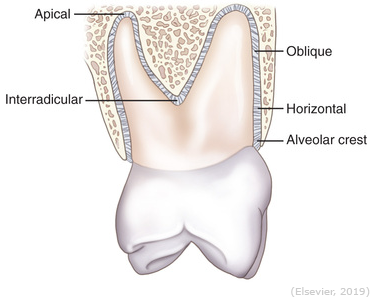
Interradicular fibers
Found only on multirooted teeth running from cementum to interradicular septum.
Enhances resistance to tipping and twisting or forces that may try and remove the tooth.
Five main functions of the PDL
Mechanical/supportive
Formative
Sensory
Nutritive
Resorptive
Mechanical/Supportive Function
Provides tooth anchorage and a cushion to absorb forces.
Transmits tension forces to bone which helps maintain bone formation.
Allows the tooth to withstand the pressures and forces of mastication.
Formative function
Tissue development – cells continuously form collagen, cementum, and bone
Sensory function
Nerve fibers in the surrounding bone provide the tooth with the protective “sense of touch,” pressure, pain and proprioception (sensation of contact when teeth are occluding).
Nutritive function
Ligaments receive their nutrition from the blood vessels that also supply the tooth and its alveolar bone.
Resorptive function
Fibroblasts of the periodontal ligament permit the continuous and rapid remodeling that is required for these fiber groups.
Can remodel the alveolar bone in response to pressure (i.e., orthodontic treatment, occlusal changes).
Periodontal Attachment Apparatus
Connects the gingiva and the PDL to the tooth. Its components include the epithelial cells of the junctional epithelium (JE) which attach via the hemidesmosomes and the connective tissue fibers that insert into the root. The normal location for this is at or around the CEJ. With periodontitis, the attachment is apical to the CEJ.
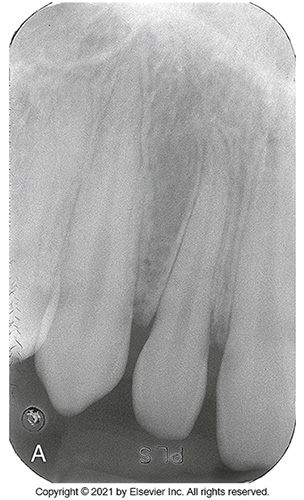
PDL radiograph
Is seen as a thin, radiolucent area adjacent to the root and the lamina dura of the bone.
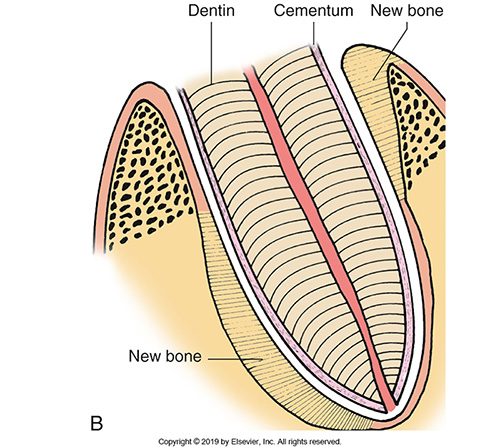
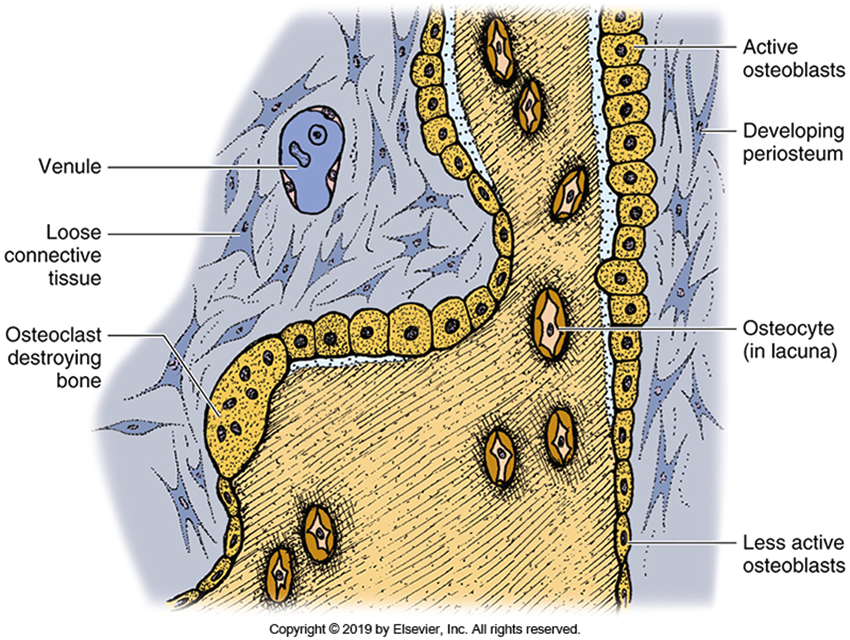
Alveolar bone development
This bone is a type of connective tissue that originates from the mesoderm. It forms through intramembranous bone formation where primitive mesenchymal cells become osteoblasts and form periosteum and then secrets hydroxyapatite to form bone.
Alveolar bone composition
A mature adult one will be composed of 65% inorganic crystals and the remaining 35% will be organic (mostly collagen).
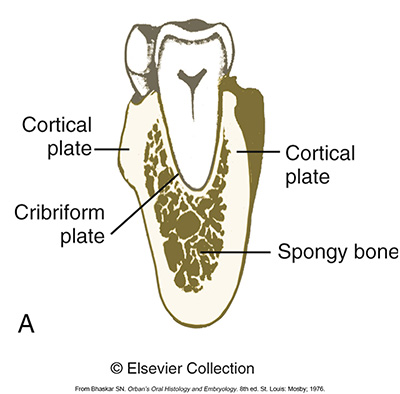
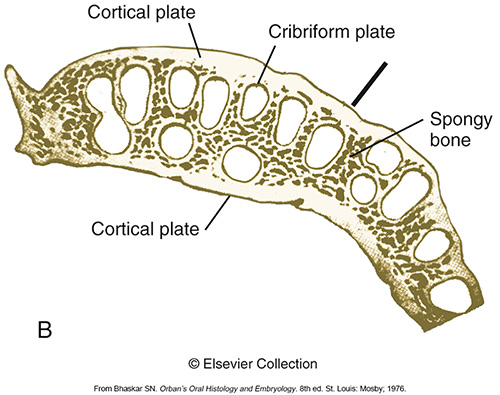
Spongy bone
Is found in the middle (bone marrow). It is small bridges of bone that have space in between and these spaces function as either blood producing or fat storing tissue.
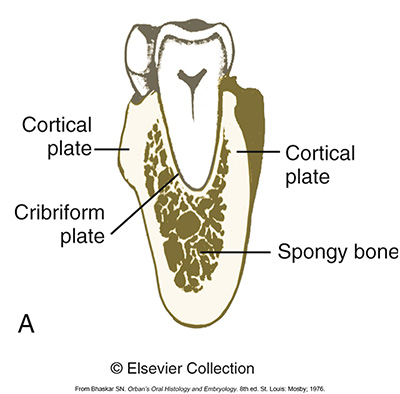
Compact or dense bone
is the hard outer layer of bone. It is bone that is made up of osteoblasts, osteocytes, collagen fibers and ground substance. It also has microscopic crystals of a substance called hydroxyapatite.
These crystals of calcium and phosphates are found packed into the ground substance and fibers between cells, giving bone its hardness.
Compact bone that is on the buccal and lingual surface is called cortical bone. The cribriform plate is also compact bone. It forms the tooth socket and contains holes for the passage of blood vessels.
Intramembranous bone formation
Is formation within tissue. Bone forms in regular connective tissue when the primitive mesenchymal cells become osteoblast cells. These osteoblasts are soon surrounded by a double layered structure called the periosteum.
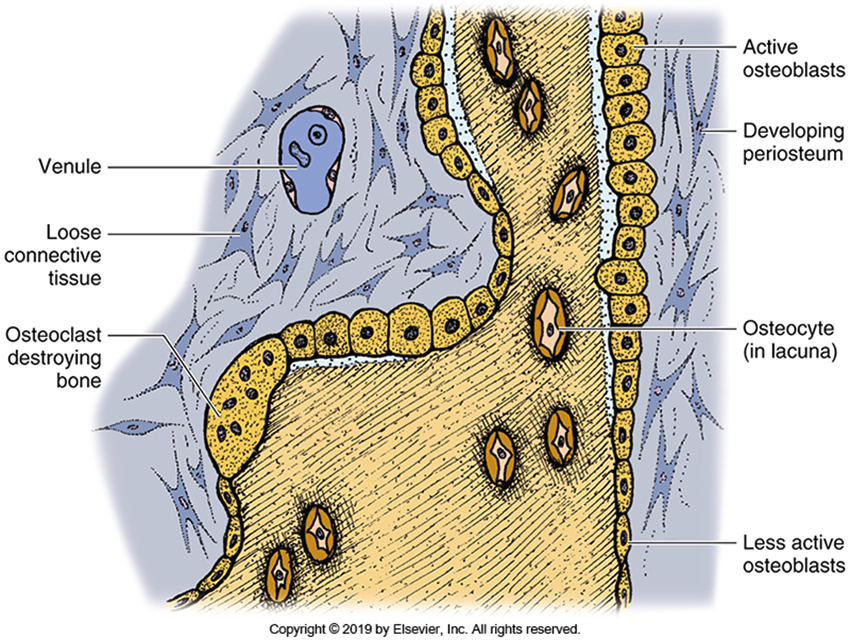
Periosteum
The outer layer of this structure is collagen, and the inner layer is osteogenic cells that become osteoblasts that secrete bone. These osteoblasts secrete ground substance, collagen fibers and then hydroxyapatite crystals. The crystals grow and are tightly packed together, and the bone hardens.
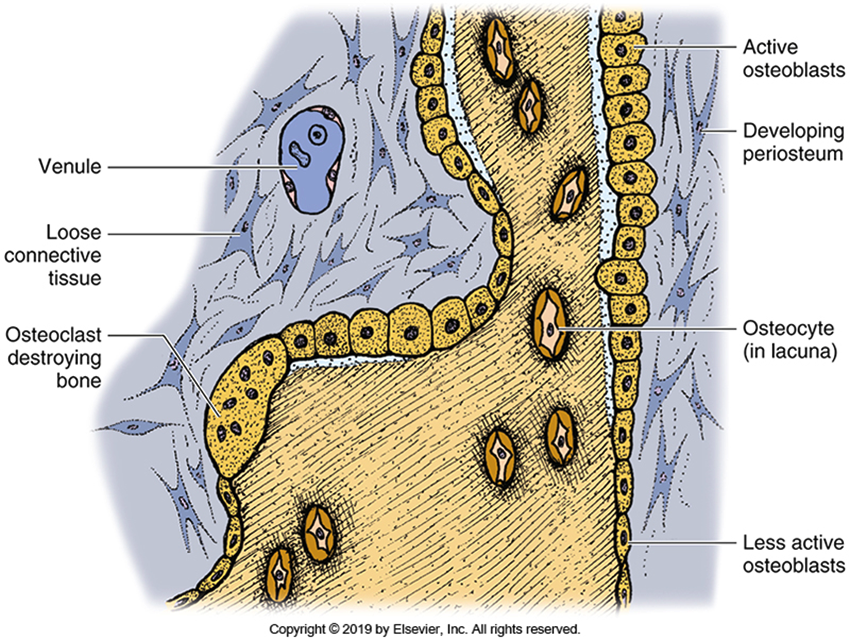
Osteocytes
The osteoblasts that get trapped in their own matric are called ____ which play a role in the nutrition of the bone.
Where does intramembranous bone formation occur
Bone growth in the head
Endochondral bone formation
With this type of bone formation, cartilage is formed first. The cartilage is covered by perichondrium.
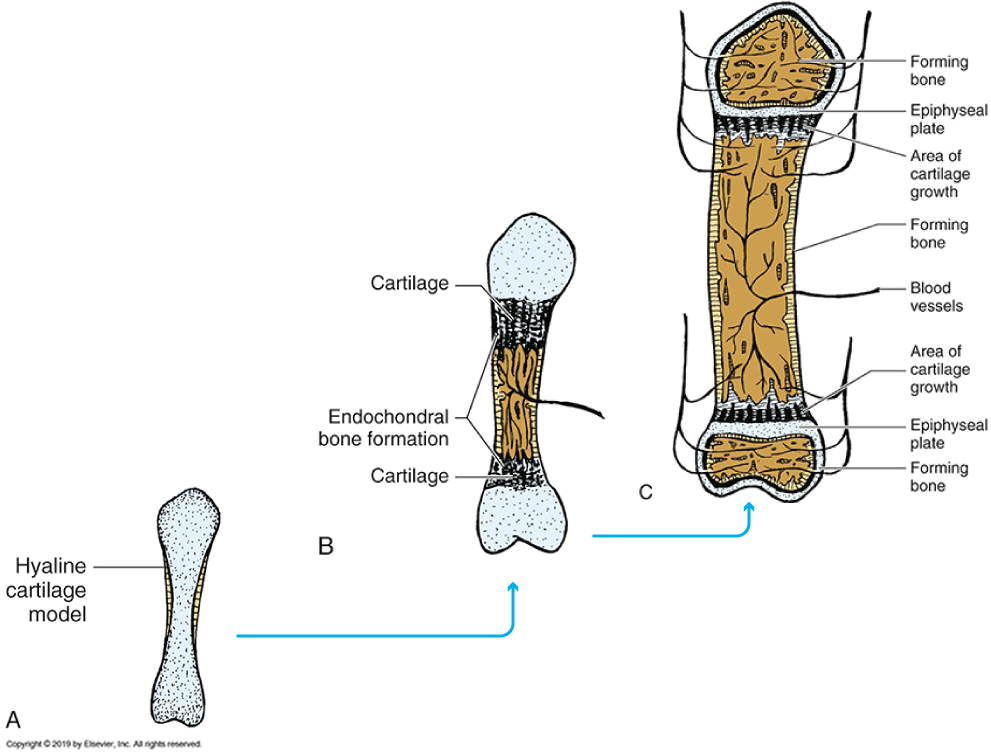
Inner layer of perichondrium
Contains cells that become chondroblasts, which produce a cartilage model of the future bone shape. The cartilage is then invaded by bone cells, which replace the cartilage with bone. As the bone replaces cartilage, it does so in two end sections called epiphyses and a center section called the diaphysis.
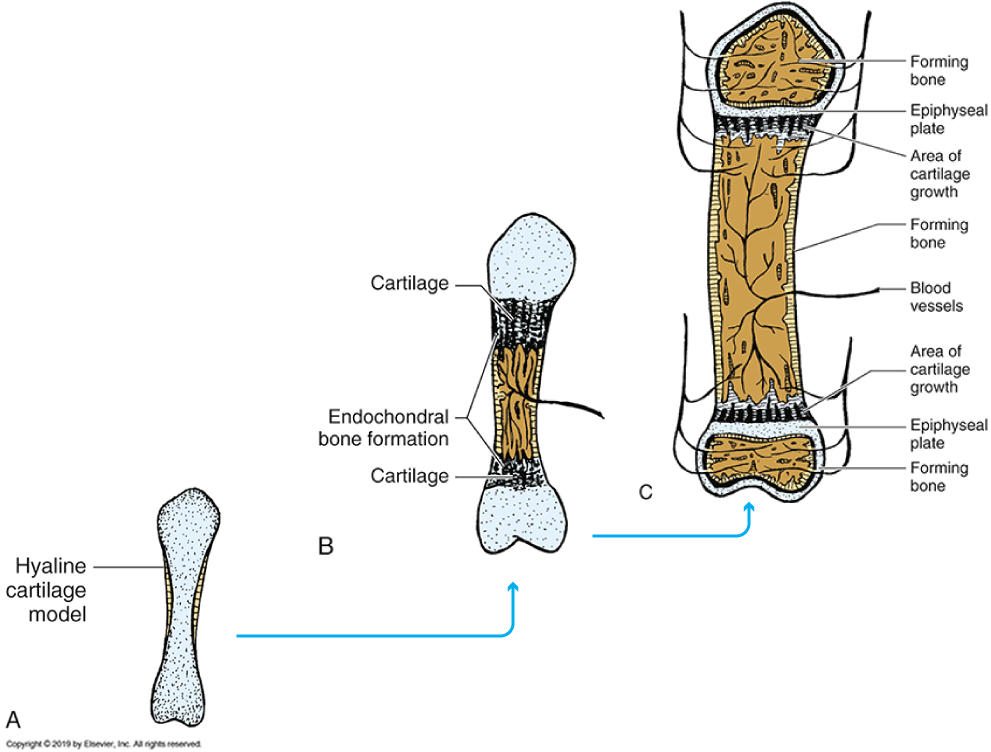
Epiphyseal plate
Between the two sections (epiphyses and diaphysis) is a block of cartilage known as this. Within this plate is the interstitial growth of cartilage that causes the plate to lengthen. The cartilage allows for directional growth.
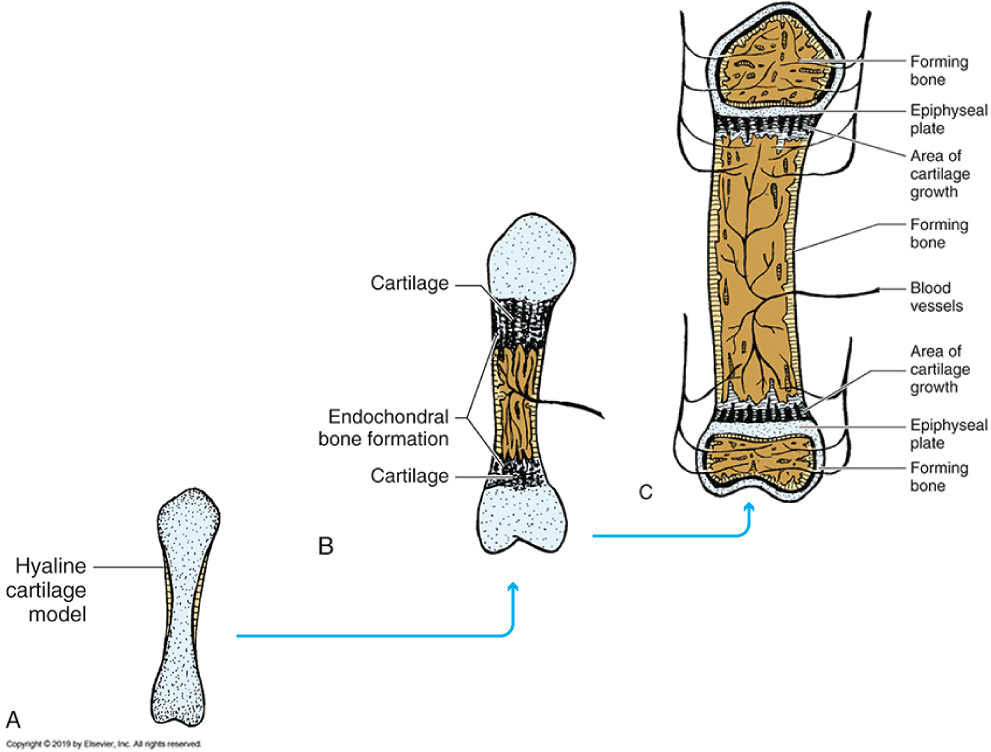
What happens when the pituitary gland stops producing growth hormones?
The epiphyseal plate disappears, and the bone is no longer in three sections – it unites as one. This type of bone growth can be seen in the growth of long bones and vertebrae and certain areas at the bottom of the skull.
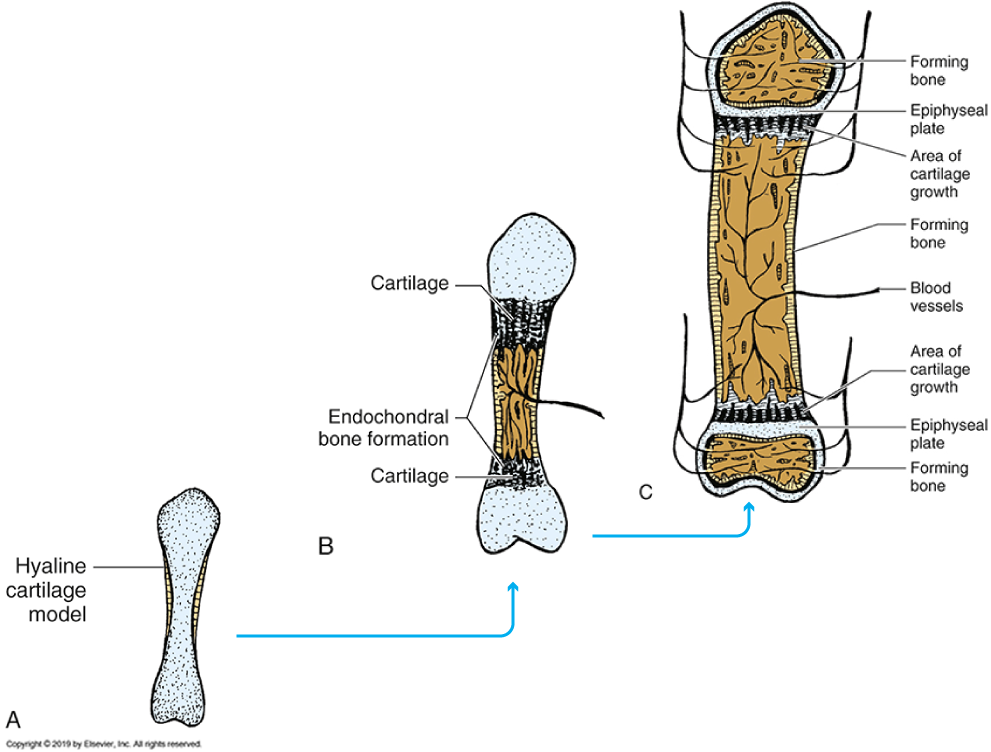
Endochondral formed bone composition
The bone is about 50% hydroxyapatite crystals, and the rest is made up of collagen, ground substance and water. It is covered on the outside with a thin connective tissue covering called the periosteum.
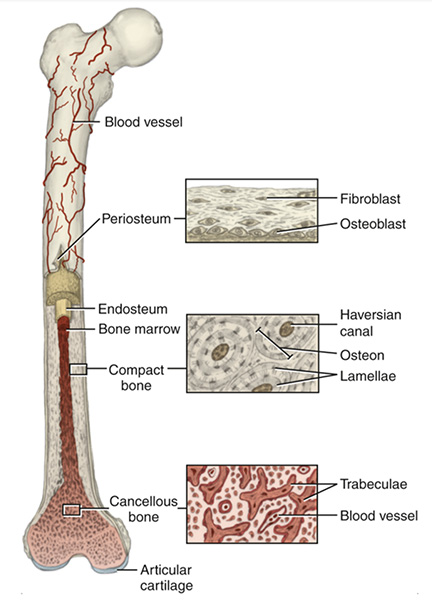
Center of long bones
Contains a marrow cavity and is the site of blood cell production. The inner wall of this marrow cavity is lined by an endosteum, which forms modified bone on the inside during remodeling of bone in bone growth.
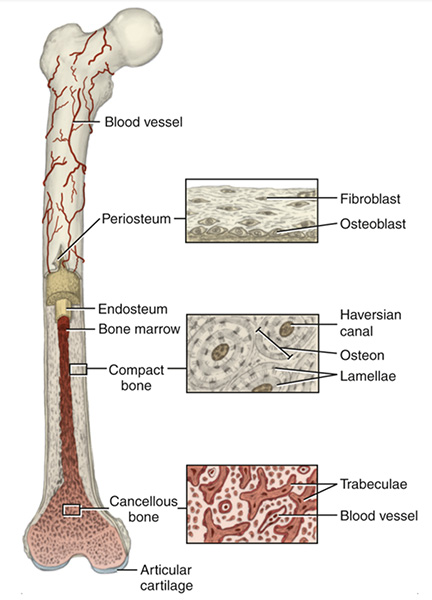
Haversian System
The hard structure between the periosteum and the marrow cavity is known as the cortical bone or plate (compact bone) and has numerous blood vessels running through it to keep it vital. Around the blood vessels, there are many trapped bone cells which are called osteocytes. The arrangement of these blood vessels and osteocytes is called a __________, a series of blood vessels running parallel to one another along the length of the bone.
Volkmann’s canals
Running perpendicular to the Haversian lamellae, there are this. These canals are also known as nutrient arteries, and they bring blood to the inside of the bone.
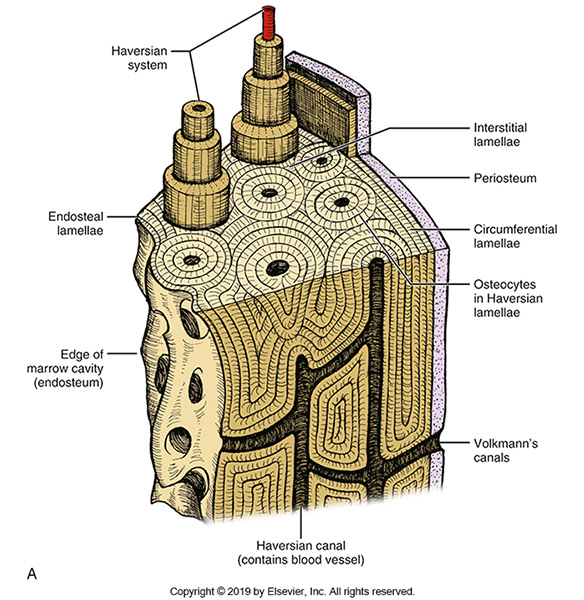
Venules
Within the Haversian System, nutrients are passed on to the entrapped osteocytes closest to the blood vessel and they pass nutrients on to the cells farther from the blood vessels. Blood is also carried into the marrow spaces where more blood cells are produced and passed out of the bone. Before the arteries reach the marrow cavity, they go through capillary beds and enter the marrow cavity as this. The veins carry the blood and new cells produced by the marrow cavity back out of the bone and into the venous circulation of the body and back to the heart.
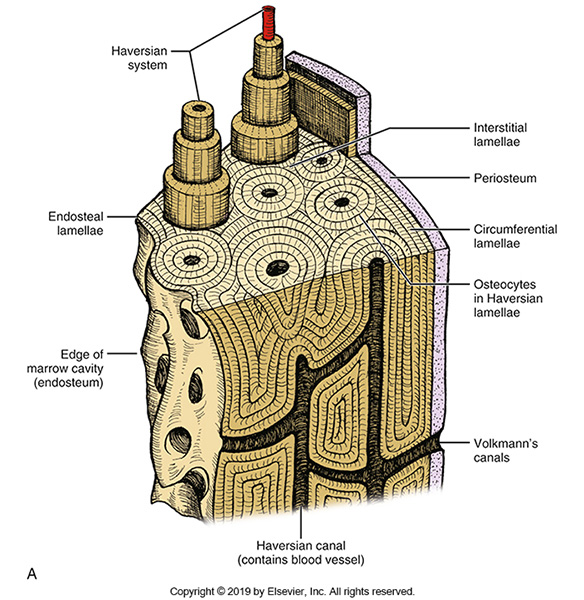
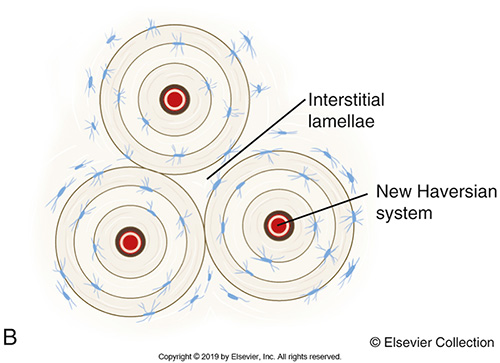
Interstitial Lamellae
The area between the Haversian Systems is known as the Interstitial Lamellae. It also has entrapped bone cells and layers. The Interstitial lamellae are old Haversian System parts that were destroyed and replaced with new systems.
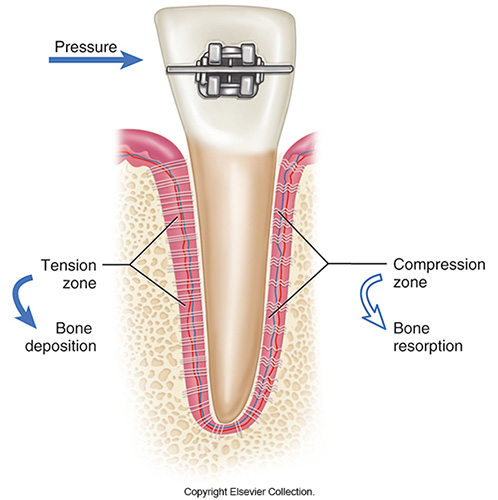
Bone remodeling
When the bone resorbs and reforms, it's called this. It is because of this that tooth movement is possible. Orthodontic treatment is a great example of this. Teeth can move because the bone is able to change and remodel.
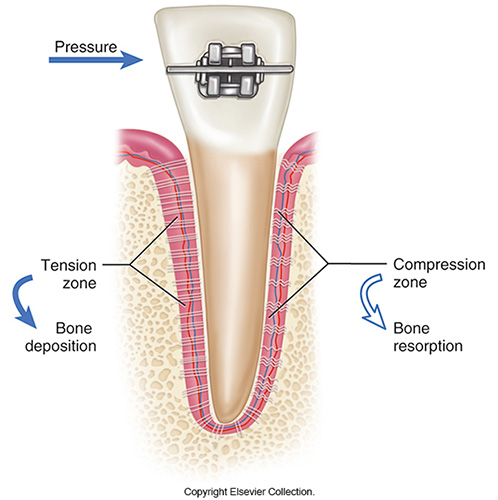
Osteoblasts vs osteoclasts
Osteoblasts are the cells that are responsible for new bone formation. Osteoclasts are responsible for resorption, or when the body removes bone. Working together, they both remodel bone.
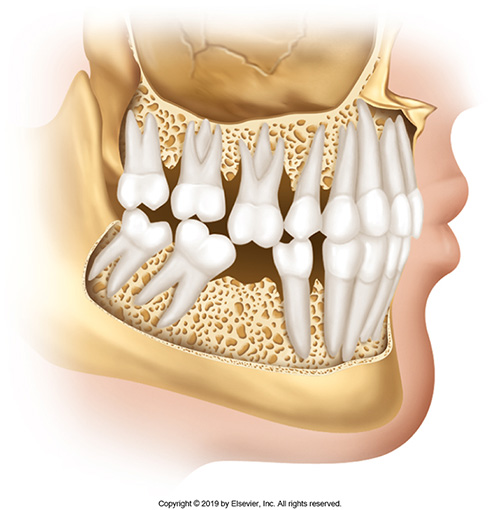
Alveolar process
Surrounds and supports the teeth in the maxilla and the mandible. It forms when teeth are present and resorbs if teeth are extracted; it consists of alveolar bone proper and supporting alveolar bone.
Alveolar bone composition
The composition varies, depending on whether the bone is old or young. Adult bone is about 65% inorganic crystal, and the remaining 35% organic composition is about 89% collagen and 11% noncollagenous material.
Cortical plate
The layer of compact bone on the buccal or lingual surface. Radiographically, the cortical plate cannot be seen because it is only on the buccal and lingual sides of the socket.
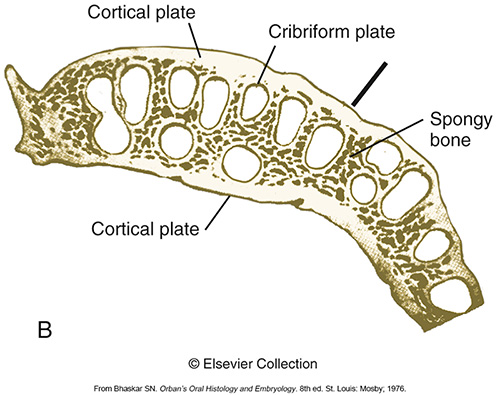
Cribriform plate (lamina dura)
The bone that forms the socket for the tooth. It is also a compact bone and contains numerous holes that allow for the passage of blood vessels, connecting the deeper part of the bone with the vessels of the periodontal space. It can also be called the alveolar bone proper. A radiograph will show the cribriform plate and the crest of bone that joins two sockets – the interproximal alveolar crest of bone.
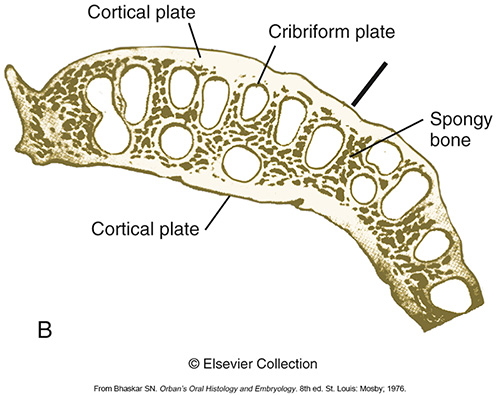
Spongy bone/cancellous bone
The bone is found in between the cortical plate and the cribriform plate and is a layer of spongy or cancellous bone – also known as bone marrow, or trabecular bone. The size and amount of trabecular bone is determined by function. If a tooth is removed from function by loss of opposing teeth, the trabeculae bone will become less numerous, but will not absorb. If the tooth is placed back into occlusion, the trabecular bone will increase in size.
Interdental septum
Bone between two teeth
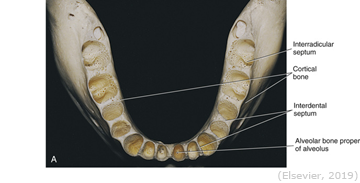
Interradicular septum
Bone between two roots
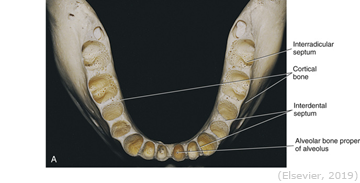
Alveolar bone radiographically
Radiographically, the cortical plate cannot be seen because it is only on the buccal and lingual sides of the socket. A radiograph will show the cribriform plate, the spongy bone and the crest of bone that joins the two sockets (the interproximal alveolar crest of bone). The contours of this area are a good indicator of periodontal health.
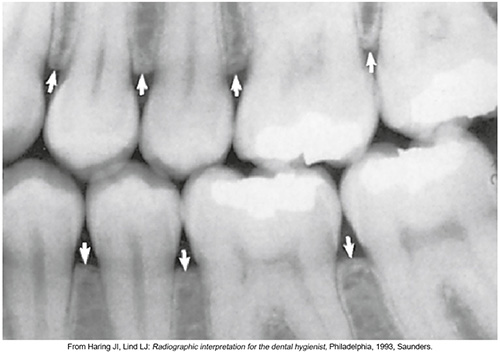
Resorption of bone
Will occur due to the following:
Trauma due to faulty occlusion
Periodontitis
Orthodontics
Mesial drift
Attrition
May cause addition to alveolar bone (tori) due to grinding. Removal of irritants may cause some bone regrowth, but not as much as the original.