Module 4/5: Fluid and Electrolytes
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
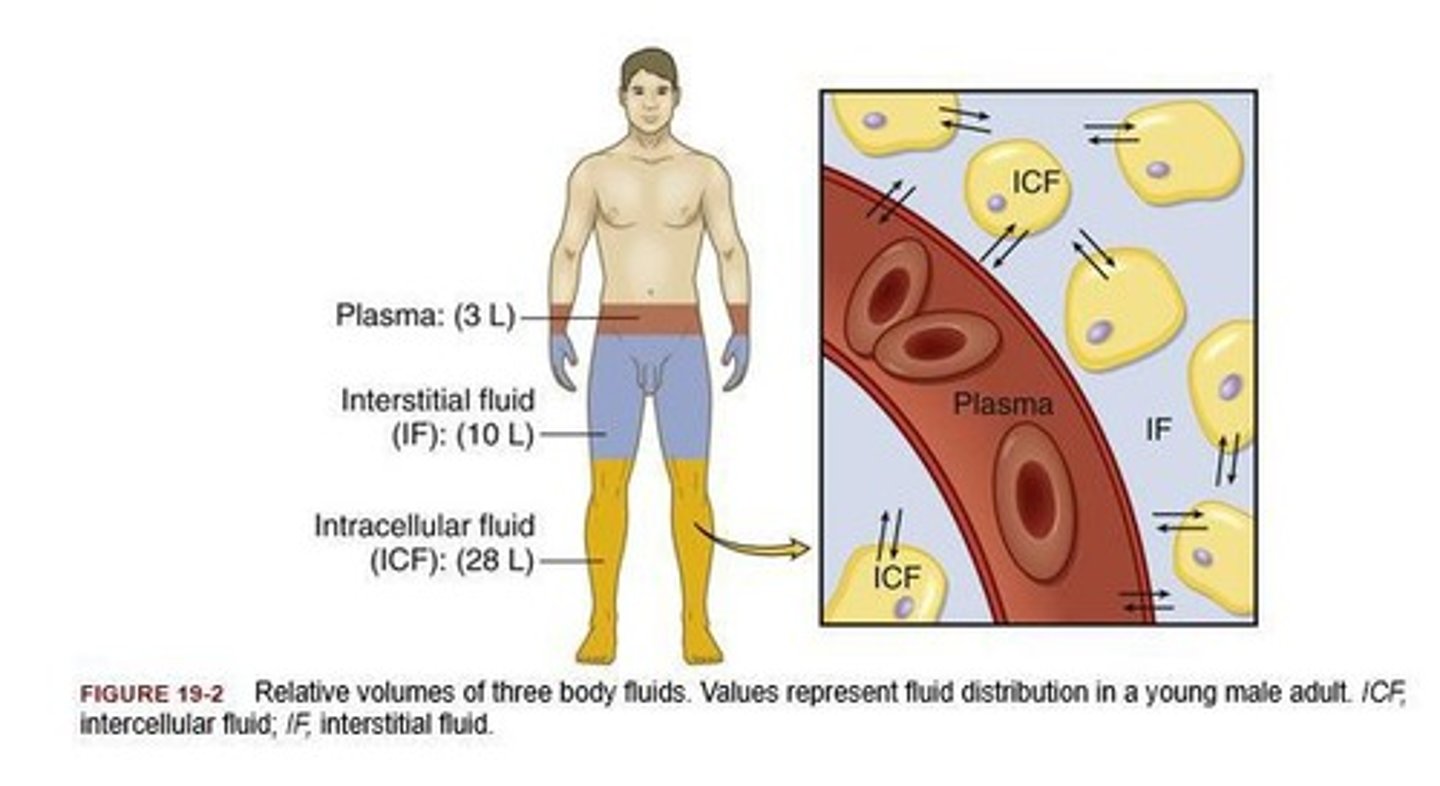
What percentage of body weight is composed of body fluids?
50-60%
What are the main components of body fluids?
Water, electrolytes, glucose, urea, creatinine
What are the three compartments of extracellular fluid (ECF)?
Intravascular (plasma), interstitial (between cells), transcellular (e.g., cerebral spinal fluid)
What is the process of filtration in fluid movement?
Movement through a semi-permeable membrane due to differences in water volume/pressure.
What is hydrostatic pressure?
The force exerted by water in the blood that pushes fluid out of capillaries.
What role do plasma proteins play in fluid balance?
They create osmotic pressure to pull fluids into the vascular space.
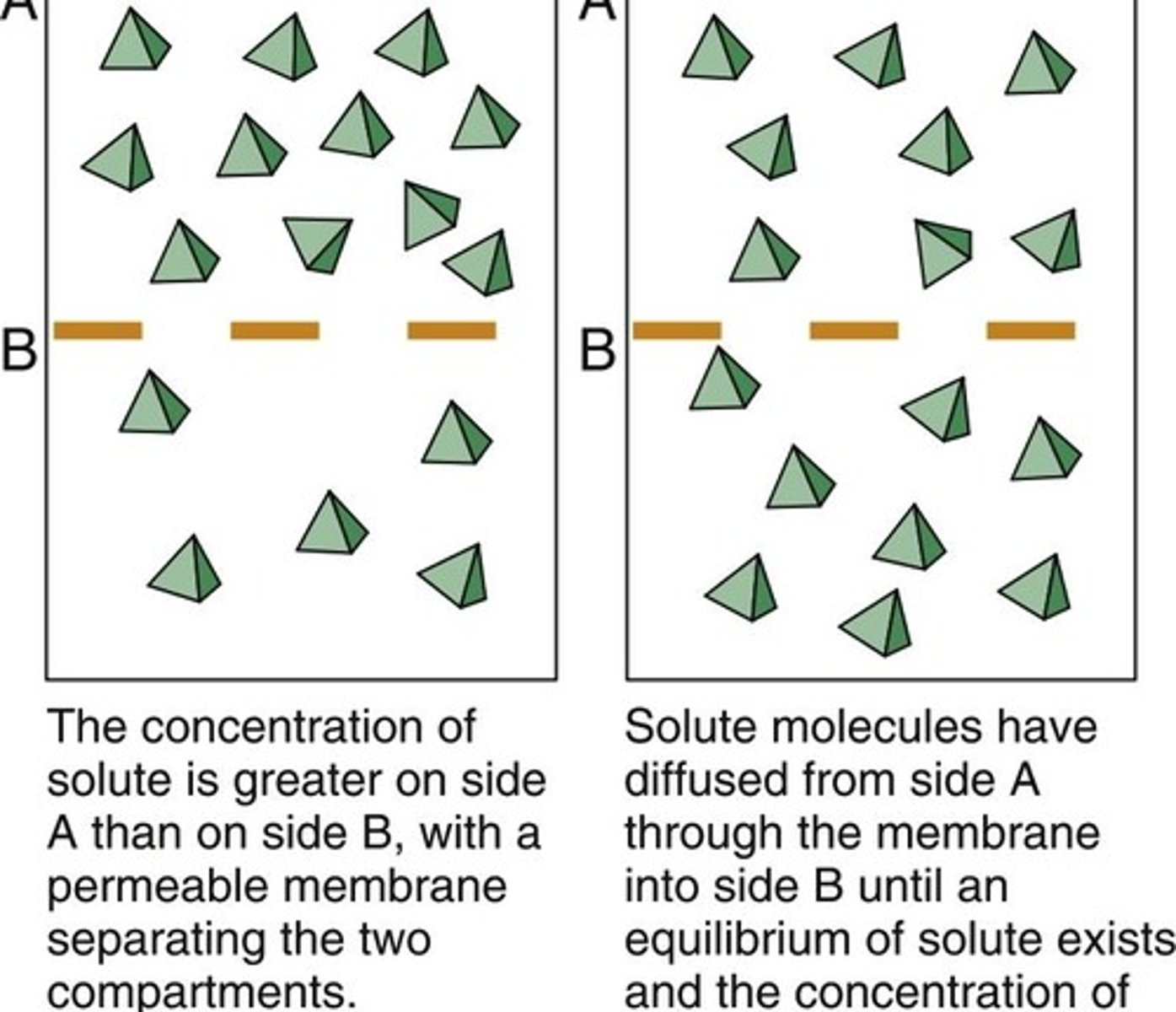
What is diffusion?
The movement of gases and particles from an area of high concentration to low concentration.
Define osmosis.
The movement of water across a semi-permeable membrane towards an area with more solutes.
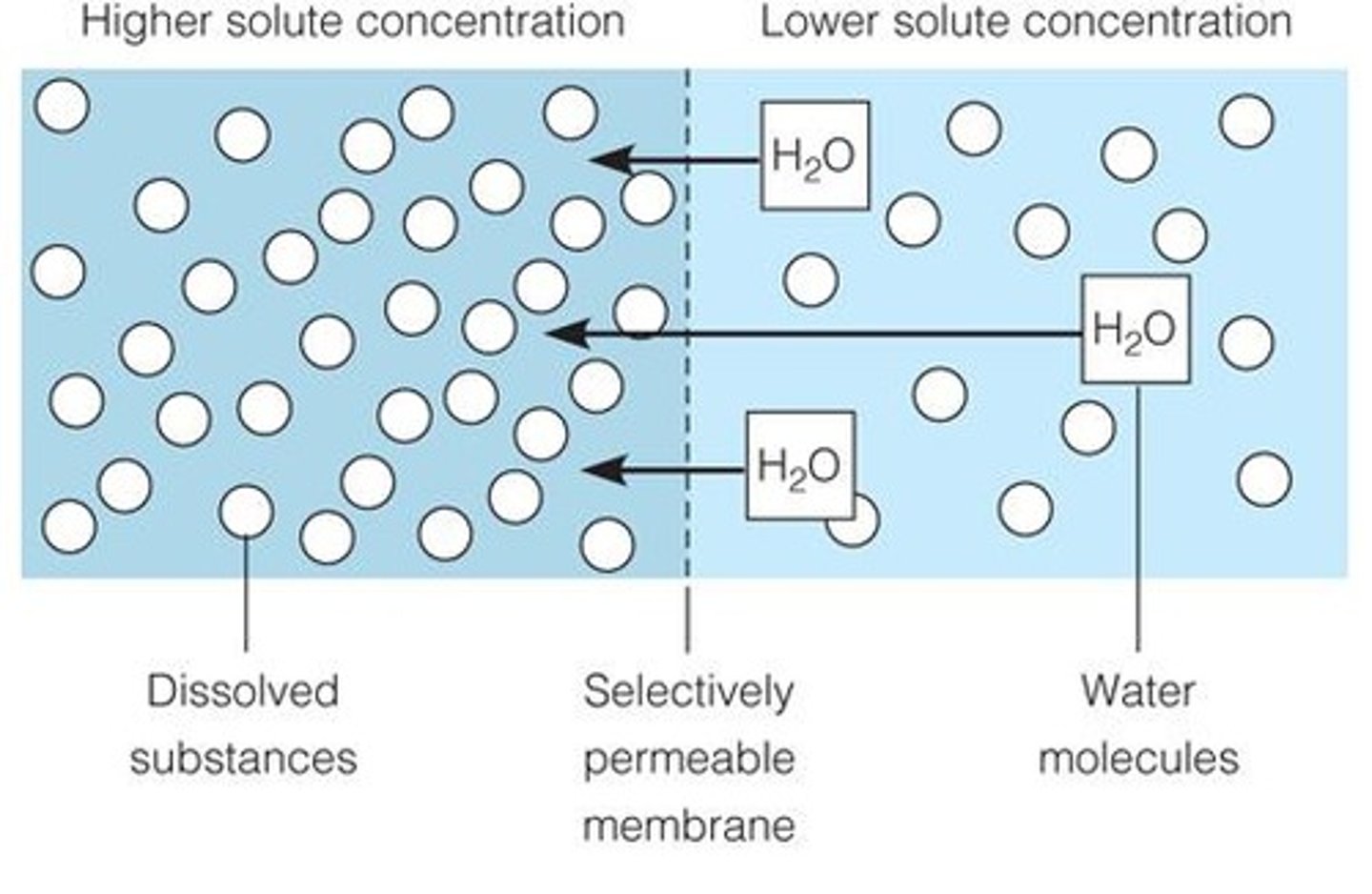
What is tonicity?
The number of dissolved particles in a fluid and its ability to create an oncotic force into/out of cells.
What is a hypertonic solution?
A solution with a total osmolality greater than serum, which pulls fluid out of cells.
What is an isotonic solution?
A solution that remains in the extracellular fluid and has the same osmolality as blood.
What is a hypotonic solution?
A solution with a total osmolality less than blood, which shifts fluids into cells.
What is the normal osmolality of serum?
280-300 mOsm/L
What are colloids?
Molecules that are not soluble and stay in the vascular system, helping to maintain high osmotic pressure.
What are crystalloids?
Solutions that can move across cellular membranes and replenish intracellular volume.
What is oliguria?
A condition where the body needs to excrete 400-600 ml/day to eliminate necessary toxins.
What regulates body water homeostasis?
The hypothalamus, through thirst recognition and renal excretion.
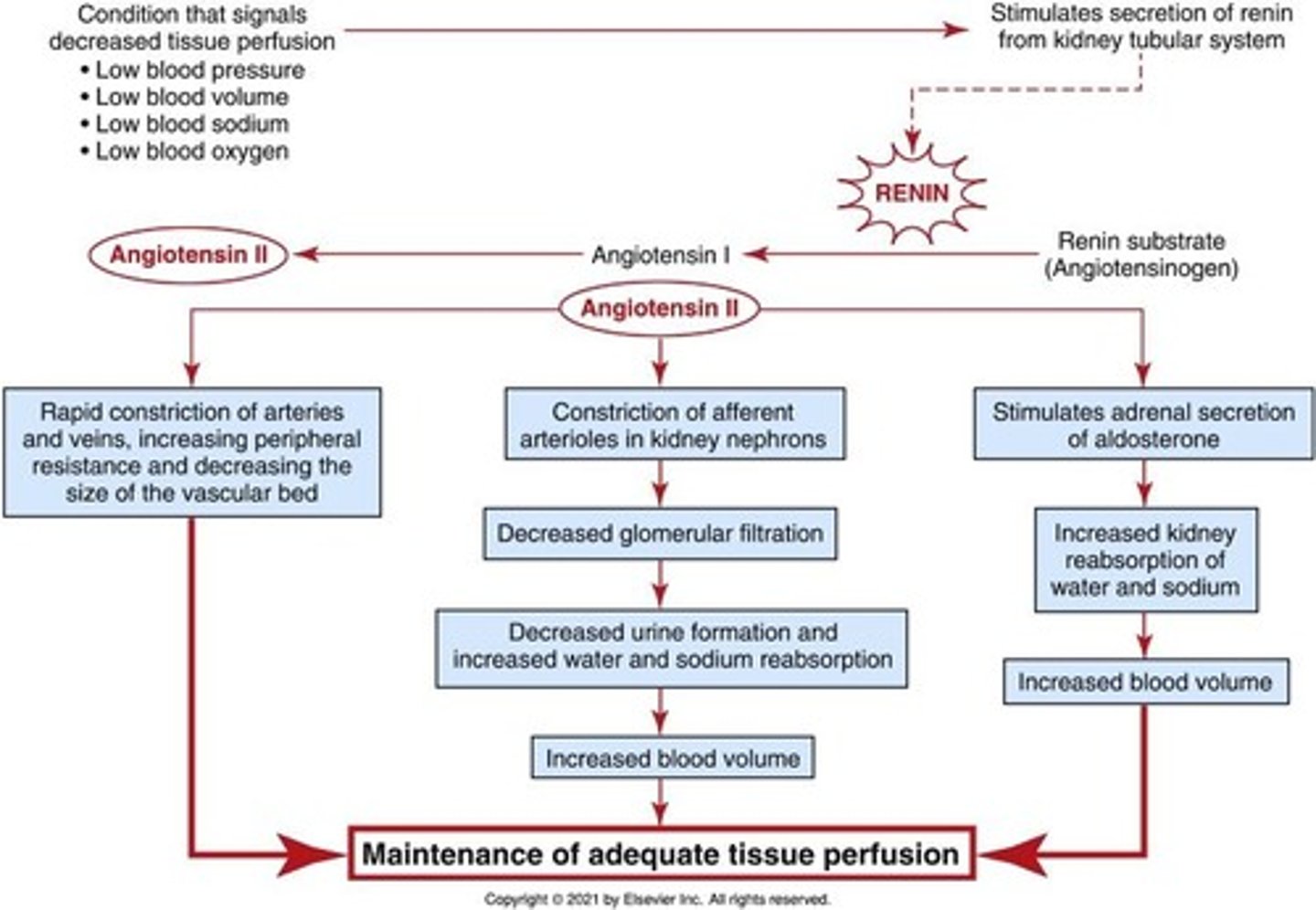
What is the role of aldosterone in fluid balance?
It stimulates kidneys to reabsorb sodium in response to decreased sodium levels.
What does ADH (antidiuretic hormone) do?
It promotes water retention in response to increased osmolality.
What is the Renin-Angiotensin-Aldosterone System (RAAS)?
A hormone system that regulates blood pressure and fluid balance.
What is hypervolemia?
An abnormally high circulating fluid volume.
What is hypovolemia?
An abnormally low circulating fluid volume.
What can cause fluid volume deficit (FVD)?
Gastrointestinal losses, urinary losses, integumentary losses, and insensible losses.
What are signs of fluid volume deficit?
Dry mucous membranes, decreased urine output, weak pulse, increased heart rate, and low blood pressure.
What laboratory tests are used to assess fluid balance?
Urinalysis, urine specific gravity, creatinine clearance, BUN, and serum creatinine.
What is the effect of stress on fluid and electrolyte balance?
High acuity patients have an increased risk of fluid and electrolyte imbalances.
What is Fluid Volume Deficit (FVD)?
Hypovolemia; abnormally low circulating fluid volume specific to the intravascular compartment.
What is the primary goal in managing Fluid Volume Deficit?
Identify and control the source of fluid loss and correct the deficit by replacing fluids.
What are the preferred methods for fluid replacement in FVD?
Intravenous (IV), oral, or enteral methods.
What is Fluid Volume Excess (FVE)?
Hypervolemia; fluid overload with abnormally high circulating fluid volume in the intravascular compartment.
What are common causes of Fluid Volume Excess?
Heart failure, kidney failure, cirrhosis, cancer, high sodium intake, and certain drug therapies.
What are some signs of Fluid Volume Excess?
Weight gain, distended neck veins, bounding pulses, edema, crackles in lungs, and shortness of breath.
What laboratory findings may indicate Fluid Volume Excess?
Increased blood pressure, central venous pressure, pulmonary artery pressures, and decreased hematocrit.
What is the normal range for Sodium (Na+) levels?
135-145 mmol/L.
What is Hyponatremia?
Sodium levels less than 135 mmol/L, often caused by loss of sodium-containing fluids or excess water.
What are the symptoms of Hyponatremia?
Hypotension, confusion, headache, lethargy, seizures, and coma.
What is Hypernatremia?
Sodium levels greater than 145 mmol/L, indicating low extracellular water relative to sodium.
What are the symptoms of Hypernatremia?
Confusion, thirst, hypertension, tachycardia, restlessness, seizures, and coma.
What is the normal range for Chloride (Cl-) levels?
95-105 mEq/L.
What is the relationship between Sodium and Chloride?
Chloride works with sodium to regulate body fluids through osmotic pressures.
What is Hypochloremia?
Low chloride levels due to inadequate intake, decreased excretion, or fluid shifts.
What are the symptoms of Hyperchloremia?
Increased blood pressure, increased heart rate, edema, agitation, headache, and changes in LOC.
What is the normal range for Calcium (Ca++) levels?
2.12-2.52 mmol/L.
What is Hypocalcemia?
Calcium levels less than 2.12 mmol/L, often causing muscle cramps, tingling, and seizures.
What is Hypercalcemia?
Calcium levels greater than 2.52 mmol/L, often leading to lethargy, confusion, and cardiac dysrhythmias.
What is the role of electrolytes in the body?
Electrolytes are required for enzyme activities, muscle contraction, and metabolism.
What are the two types of electrolytes?
Cations (positively charged) and anions (negatively charged).
What is the normal range for Potassium (K+) levels?
3.5-5.1 mmol/L.
What is the normal range for Magnesium (Mg++) levels?
0.74-1.07 mmol/L.
What is the normal range for Phosphate (PO4) levels?
0.81-1.45 mmol/L.
What should be monitored in patients with electrolyte imbalances?
Vital signs, especially blood pressure and other reflectors of fluid status.
What is the first action to take for patients with Sodium imbalances?
Identify high-risk patients and find the underlying cause.
What can happen if sodium levels are increased too quickly?
It can cause CNS irritation and pulmonary edema.
What are Chvostek's and Trousseau's signs used to assess?
They are used to assess for signs of tetany, often related to calcium imbalances.
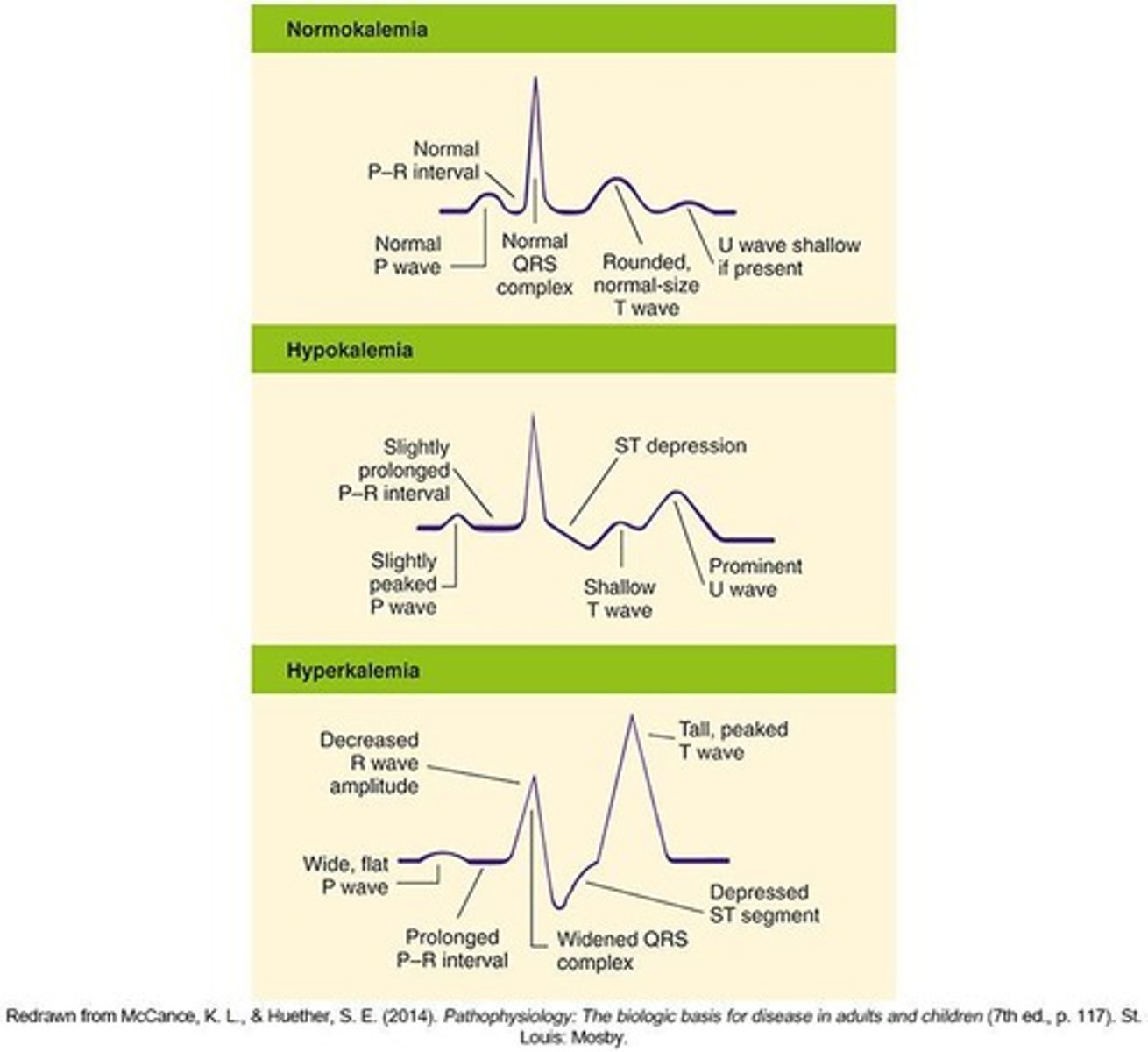
What is hypokalemia?
A condition where potassium levels are less than 3.5 mmol/L, critical if below 2.5 mmol/L.
What are common causes of hyperkalemia?
Massive intake of potassium, impaired renal excretion, and shifts from intracellular to extracellular fluid.
What are the symptoms of hypokalemia?
Weakness, muscle cramps, ECG changes, and potential paralysis.
What is the treatment for hypokalemia?
Restoration of potassium levels and treating the underlying cause.
What is hypermagnesemia?
A condition where magnesium levels are greater than 1.03 mmol/L, critical if above this level.
What are the signs of hypomagnesemia?
Hypotension, life-threatening cardiac arrhythmias, disorientation, and neuromuscular irritability.
What is the role of magnesium in the body?
It ensures sodium and potassium transport across cell membranes and is important for nerve conduction.
What are the causes of hypophosphatemia?
Malnutrition, malabsorption syndrome, and acute respiratory alkalosis.
What are the symptoms of hyperphosphatemia?
Muscle cramping, weakness, tachycardia, and gastrointestinal disturbances.
What is the management for hyperphosphatemia?
Identifying and treating the underlying cause, and possibly using diuretics or oral antacids.
What is the importance of monitoring ECG in electrolyte imbalances?
ECG changes can indicate alterations in potassium, magnesium, or calcium levels, which can lead to serious complications.
What should be monitored in patients with fluid overload?
Vital signs, neck vein distention, and presence of crackles in the lungs.
What is the first step in managing electrolyte imbalances?
Identify high-risk patients and treat the underlying cause.
What is the critical potassium level indicating hyperkalemia?
Greater than 5.1 mmol/L, critical if above 6.0 mmol/L.
What are the common signs of hypomagnesemia?
Neuromuscular blockade, bradycardia, AV block, and hypotension.
What is the treatment for hypermagnesemia?
Identifying the cause and possibly using diuretics to lower serum magnesium levels.
What is the significance of potassium in cardiac function?
Potassium is vital for muscle contraction and influences nerve impulse conduction; abnormal levels can lead to cardiac arrest.
What is the relationship between potassium and acid-base balance?
In metabolic acidosis, potassium shifts from intracellular to extracellular compartments to maintain balance.
What are the symptoms of hypophosphatemia?
Weakness, numbness, tingling, pathologic fractures, and diminished myocardial function.
What should be monitored in patients receiving IV potassium?
Cardiac function and ECG changes due to the high-risk nature of potassium administration.
What is the role of dietary management in electrolyte imbalances?
Monitoring diet is crucial to prevent imbalances and support treatment.
What is the treatment for hypophosphatemia?
Identifying and treating the underlying cause and replacing serum phosphate levels.
What is the potential effect of hypophosphatemia on the musculoskeletal system?
It can lead to muscle weakness and pathologic fractures.
What is the significance of monitoring intake and output (I&O) in electrolyte management?
It helps assess fluid volume status and detect potential imbalances.