FF: Class Questions
1/329
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
330 Terms
A PT performs the special test shown below. The pt is instructed to stand on one leg with the knee slightly flexed and rotate the body while maintaining balance on the supporting leg. The test is considered positive if the patient reports joint line discomfort or catching. What special test is being performed, and what is the MOST LIKELY diagnosis?
Thessaly test, medial meniscus tear
McMurray’s test, medial meniscus tear
Apley’s test, medial meniscus tear
Valgus stress test, MCL tear
Thessaly test, medial meniscus tear
❌McMurrays: knee flex+rot, not in WBing
❌Apleys: compression+rot, prone not in WBing
❌Valgus stress test: assesses MCL
The pt has been recommended by the physician to ambulate with PWB. Which would be the MOST APPROPRIATE AD for the weightbearing status advised to the pt?
Bilat canes
Unilat axillary crutch
Unilat Lofstrand crutch
Bilat axillary crutches
Bilat axillary crutches →approp for PWB and NWB
After several sessions of PT, the pt’s POC now includes mobilizations to increase knee extension in an open chain position. Which mobilization technique is MOST APPROPRIATE for achieving this range of motion?
Anterior glide to the tibia
Anterior glide to the femur
Posterior glide to the tibia
Posterior glide to the femur
Anterior glide to the tibia
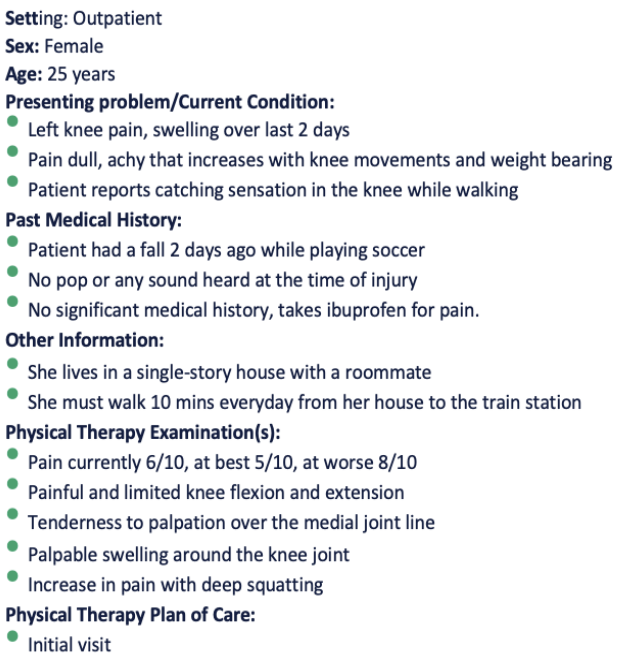
A patient was diagnosed with a stroke that affected the area marked in the image. Which of the following impairments are MOST LIKELY to be seen in this patient?
Resting tremors
Dystonia
Visual field disturbances
Dysmetria
Dysmetria →cerebellar involvement
❌Basal Ganglia: restring tremors, dystonia
❌Occipital lobe: visual field disturbances

During a baseline examination, the physical therapist examines the patient’s heart sounds. Which valve is being auscultated in the picture shown below?
mitral valve
pulmonary valve
tricuspid valve
aortic valve
tricuspid valve
think APTM 2245
Aortic: R 2nd ICS, sternal border
Pulmonic: L 2nd ICS, sternal border
Tricuspid: L 4th ICS, sternal border
Mitral: L 5th ICS, midclavicular line
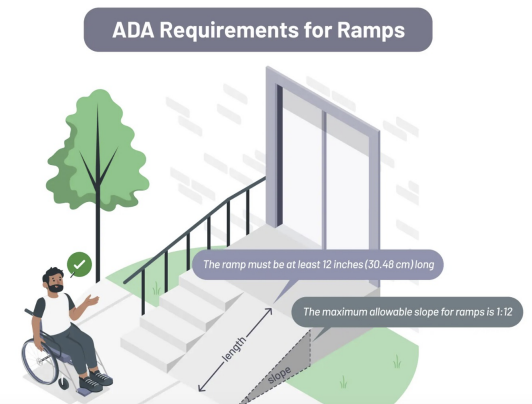
A patient using a wheelchair needs a ramp to access a building with two steps totaling a rise of 14in. According to the ADA guidelines, what is the minimum ramp length in feet required?
10ft
12ft
14ft
16ft
14ft →every 1in rise req 1ft ramp length
Each step is typ 7in high, so two steps = 14in total rise
A recreational soccer player reports hip and knee discomfort. On gait examination, there is toe-in throughout stance and swing phases, with patellae facing medially. No structural leg length discrepancy is observed. Which of the following interventions is MOST APPROPRIATE to improve this patient’s functional movement pattern?
strengthen hip internal rotators and abductors
stretch hip internal rotators and strengthen hip external rotators
stretch hip abductors and strengthen internal rotators
provide patient education on limiting activity until symptoms resolve
stretch hip internal rotators and strengthen hip external rotators
Rationale: The patient’s toe-in gait and medially facing patellae suggest excessive hip internal rotation, often due to femoral anteversion. This causes the foot to point inward and alters knee tracking. Stretching hip internal rotators and strengthening hip external rotators and abductors helps correct this imbalance, improving gait mechanics and reducing symptoms. Strengthening internal rotators or adductors would worsen the pattern, while rest alone does not address the underlying movement dysfunction.
A PT examines a patient with chief concerns of tingling into the 4th and 5th digits along with muscle wasting over the hypothenar eminence. Which of the following testing procedures would be the BEST to assess the integrity of the nerve?
Have the pt flex both wrists while holding them for one min
Have the pt make a fist around the thumb and perform ulnar deviation
Have the pt grasp a piece of paper between their first and second digit while the examiner pulls the paper and monitors the first digit
Have the patient perform extension of the third digit of the hand against the examiner resistance
Have the pt grasp a piece of paper between their first and second digit while the examiner pulls the paper and monitors the first digit →froment’s sign for ulnar N injury (adductor pollicis weakness)
❌1→Phalen’s for Carpal Tunnel
❌2→Finkelstein for DeQuervains
❌4→Maudsley’s for Lateral Epicondylitis
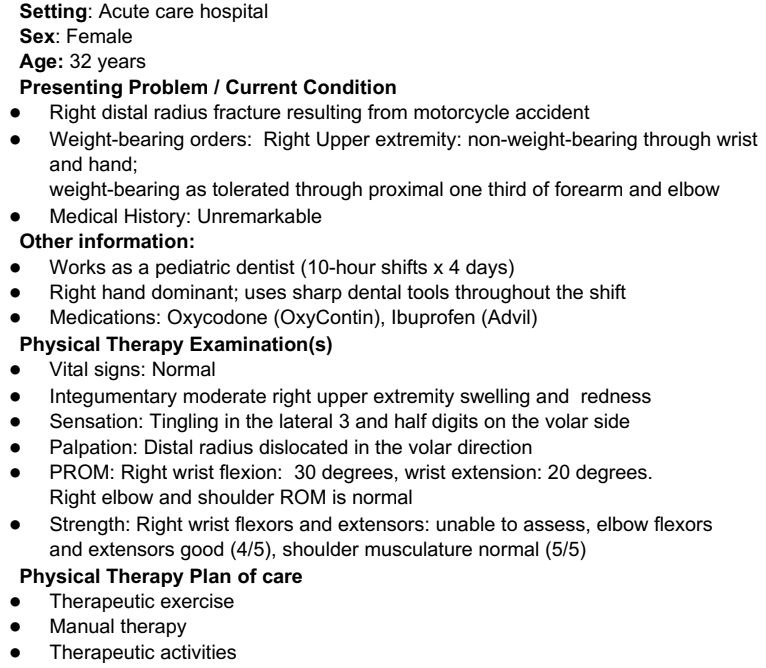
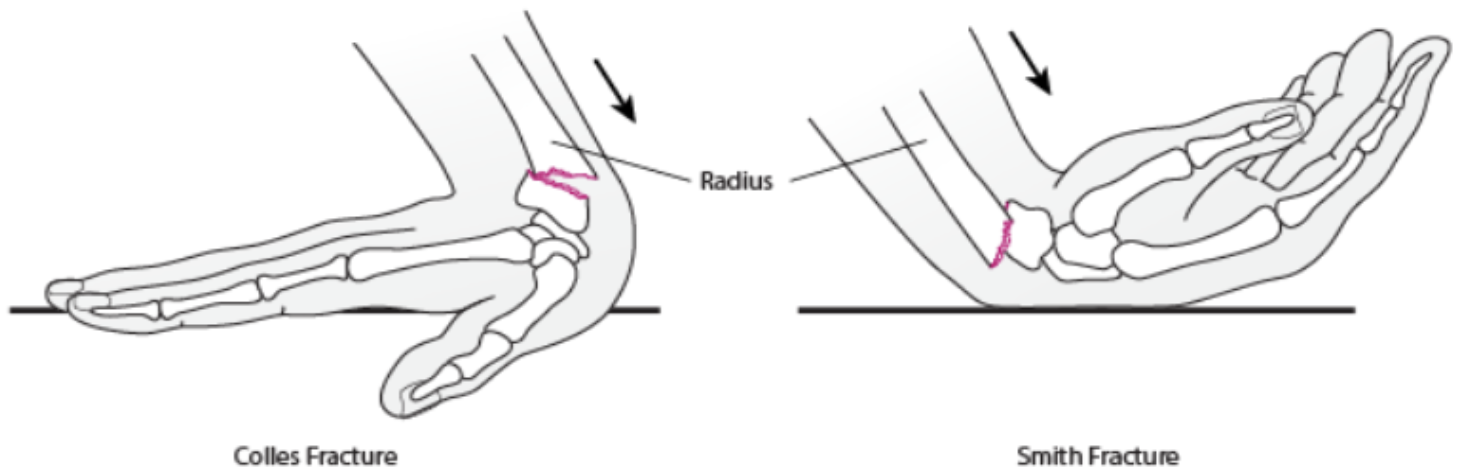
Which of the following would be the MOST LIKELY diagnosis?
Smith’s fracture
Colles fracture
Scaphoid fracture
Dinner fork deformity
Smith’s fracture (garden spade deformity) →radius dislocated volarly
❌Colles fracture (dinner fork deformity) →radius dislocated dorsally
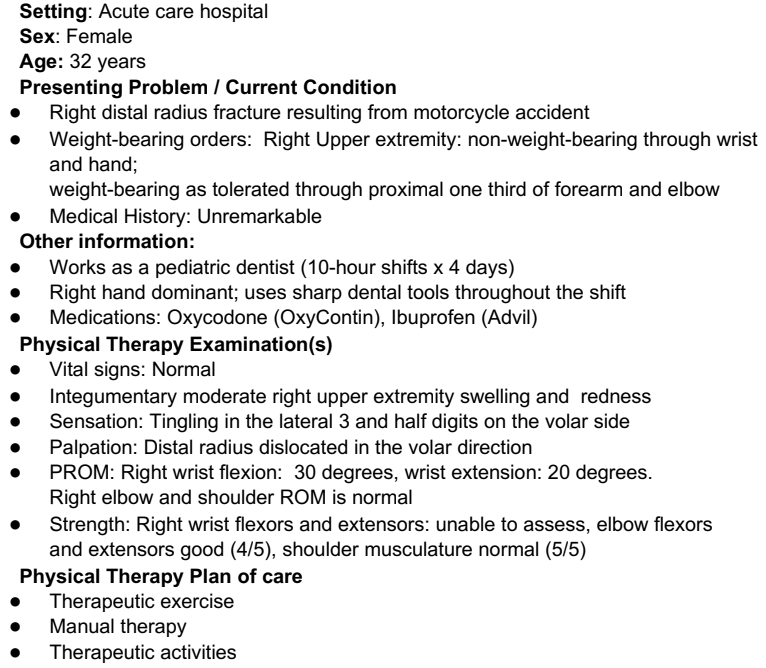
Which of the following would be the MOST LIKELY presentation in this patient?
Wasting of thenar eminence
Wasting of hypothenar eminence
Unable to perform little finger adduction
Unable to perform index finger extension
Wasting of thenar eminence →median N (N/T along lateral 3.5 digits on volar side)
❌Ulnar N: interossei weakness
❌Radial N: finger extensor weakness
The patient has been coming to PT for 4 weeks and has significant improvement in wrist ROM but continues to experience limited end range wrist EXT. Which is the MOST APPROPRIATE intervention?
dorsal glide of carpal bones
volar glide of carpal bones
medial glide of carpal bones
lateral glide of carpal boones
volar glide of carpal bones
A clinician is evaluating patient with a vague diagnosis of LBP. The patient displays a positive Thomas test. Which sub phase of the gait cycle will MOST LIKELY show limitation in the hip ROM?
loading response
initial contact
midstance
terminal stance
terminal stance
Rationale: Terminal stance requires maximum hip extension. Patient will either present with anterior trunk lean or excessive lumbar lordosis to compensate for limited hip extension due to hip flexor contracture or tightness.
A PT observes R pelvic hike during swing phase of the R gait cycle. Which of the following conditions is MOST LIKELY to cause the problem?
excessive R hip flexion
inadequate R knee flexion
excessive ankle DF
R ankle PF weakness
inadequate R knee flexion
Rationale: Possible causes for pelvic hike in wing phase are reduced hip flexion, reduced knee flexion, and/or lack of ankle dorsiflexion. Tightness (not weakness) of the plantarflexors will cause pelvic hike.
Which of the following is MOST LIKELY seen in a patient with facial nerve (CN7) palsy?
absent pupillary reflex
absence of sensation in the anterior 2/3 of the tongue
hyperacusis
increased lacrimation
hyperacusis
Rationale: Hyperacusis (Option C) is defined as the collapsed tolerance to normal environmental sounds. Facial nerve controls the excessive movements of the stapedius bone and dampens the sound, and its injury can cause hyperacusis. Sensation in anterior 2/3 of tongue is by trigeminal nerve and not by facial nerve. Facial nerve is for taste on anterior 2/3 of the tongue. The efferent arc for Corneal reflex is the facial nerve. Decreased lacrimation is seen with facial nerve palsy.
A pt is evaluated 3mo s/p R ankle fracture. AROM PF 0-10deg, DF 0-20deg. Which joint mobilization technique is MOST APPROPRIATE to improve plantarflexion?
anterior glide of the talus on the tibia
lateral glide of the calcaneus on the talus
medial glide of the calcaneus on the tibia
posterior glide of the talus on the tibia
anterior glide of the talus on the tibia
Rationale: Dorsiflexion and plantarflexion occur at the talocrural joint, where the convex talus articulates with the concave tibia and fibula. Based on the convex–concave rule, the roll and glide occur in opposite directions. To improve plantarflexion, an anterior glide of the talus is performed. Option B improves inversion. Option C improves eversion. Option D improves dorsiflexion
A clinician is testing shoulder AROM and asks the patient to move the shoulder into full IR; during this motion, which direction will the humerus slide in?
anterior
superior
inferior
posterior
posterior
Rationale: During medial (internal) rotation of the shoulder at the glenohumeral (GH) joint, the head of the humerus moves on the glenoid fossa. Due to the convex-concave rule, the humeral head (convex) will slide in the opposite direction. According to convex concave rule at shoulder ---> Convex on concave = roll and glide occurs in opposite direction. A posterior glide improves IR.
During examination of the shoulder, a patient demonstrated limited and painful shoulder flexion ROM. Which of the following joint mobilization techniques is MOST APPROPRIATE?
Large amplitude oscillations performed at the beginning of the ROM in an anterior direction
Small amplitude oscillation into tissue resistance up to the limit of available motion in an anterior direction
Large amplitude oscillations within the available ROM in a posterior direction
Small amplitude oscillations into tissue resistance at the limit of available joint motion in a posterior direction
Large amplitude oscillations within the available ROM in a posterior direction
❌1/2—wrong direction glide
❌4—grade 4 mob (for ROM, not pain)
PT examination reveals that the L PSIS low+ASIS high. Which of the following is the BEST intervention?
Stretching the R hip flexors to correct R anterior rotated innominate
Strengthening of L hip flexors to correct L posterior rotated innominate
Stretching the L hip extensors to correct L posterior rotated innominate
Strengthening the R hip extensors to correct R posterior rotated innominate
Stretching the L hip extensors to correct L posterior rotated innominate
Always stretch before strengthening!!
While examining the patient, the PT notices a drop of the L hip during R midstance. INjury to which nerve is MOST LIEKLY the cause of the impairment?
R inferior gluteal nerve
R superior gluteal nerve
R femoral nerve
R obturator nerve
R superior gluteal nerve →L4-S1
R GMed weakness
What would be the MOST APPROPRIATE treatment for this impairment?
Stand on R leg and abduct L leg
Stand on L leg and extend R leg
Stand on R leg and flex R leg
Stand on L leg and flex R leg
Stand on R leg and abduct L leg
Rationale: Stick to the plane! Work in frontal plane and best choice is CKC for the RLE. Stabilize on weak side, move left leg into abduction will increase strength more than abduction on the right.
Which of the following mobilization techniques is MOST APPROPRIATE to improve the limited hip external rotation ROM?
anterior glide to femur
posterior glide to femur
superior glide to femur
inferior glide to femur
anterior glide to femur →convex femur moves on concave acetabulum (opp roll/glide)
❌2. post glide—improves flex
❌3. superior glide—improves ADD
❌4. inferior glide—improves ABD
A PT is evaluating muscle function during gait. During which phase do the hamstring muscles contract eccentrically?
initial swing
terminal swing
midstance
terminal stance
terminal swing
Rationale: HS most elongated when hip flex+knee ext (think stretching position)
❌1. InSw - needs knee flexion (conc)
❌3. MidSt (HS not getting elongated enough)
❌4. TmSt (HS not getting elongated enough)
A patient comes to an outpatient clinic reporting neck problems. Which of the following exercise combinations is MOST APPROPRIATE for a patient who has a forward head posture?
strengthen the deep cervical flexors and stretch the SCMs and upper cervical extensors
strengthen the deep cervical flexors and SCMs and stretch the upper cervical extensors
strengthen the cervical extensors and stretch the SCMs and deep cervical flexors
strengthen the cervical extensors and SCMs and stretch the deep cervical flexors
strengthen the deep cervical flexors and stretch the SCMs and upper cervical extensors
Upper Crossed Syndrome- Forward head posture
Tight: UT, levator, pecs, SCM
Weak: DNF, LT, serratus

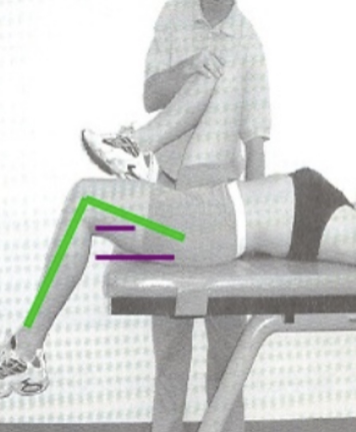
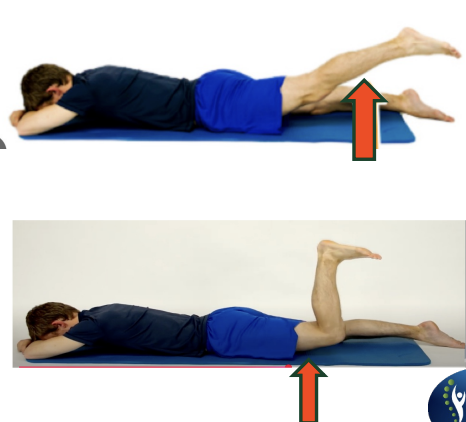
To unlock the knee, when going from position A to B as shown in the image, which of the following motions is MOST LIKELY to occur?
Lateral rotation of the femur on the tibia
Medial rotation of the femur on the tibia
Lateral rotation of the tibia on the femur
Medial rotation of the tibia on the femur
Lateral rotation of the femur on the tibia
Rationale: During knee flexion (From A to B) in a closed-chain movement, the femur undergoes lateral rotation on the tibia. This rotation allows the knee to unlock and flex into the squat position.
Excessive upward rotation of the L scapula is noted as the pt attempts shoulder abduction. Which of the following muscles is NOT LIKELY to contribute to excessive scapular rotation?
Weakness of serratus anterior
Weakness of lower trap
Weakness of rhomboid major and minor
Weakness of pectoralis major
Weakness of rhomboid major and minor →downward rotator
Rationale: Rhomboids is a downward rotator. If weak, it is not able to control the upward rotation, hence an excessive movement of upward rotation occurs. Strengthening the rhomboids would be the most appropriate intervention to improve downward rotation. Serratus anterior and lower trapezius are upwards rotators and they should have been tight to cause excessive upward rotation. Pec major does not cause rotation at the Scapula.
A PT is initiating passive and assisted movements for a patient who underwent surgical repair of a full-thickness RCT 6d ago. Which of the following positions is MOST APPROPRIATE for the patient?
Patient in sitting with arm abducted 70deg with slight flexion
Patient in supine with arm abducted 45deg with slight flexion
Patient in sitting with arm abducted 15deg with slight flexion
Patient in supine with arm abducted 90deg with slight flexion
Patient in supine with arm abducted 45deg with slight flexion
❌1/3—early post-op supine»sitting for better stabilization
❌4—too soon based on 1wk post-op status (may damage repair)
On examination, which special test is MOST LIEKLY to be positive in this patient?
Anterior drawer test
Kleiger’s test
Thompson test
Talar tilt test
Thompson test →achilles tendon rupture (+ demos no PF)
❌Anterior drawer—ATFL/ACL injury
❌Kleiger’s—Tibiofibular injury
❌Talar tilt—For CFL and deltoid sprain
The pt underwent R achilles tendon repair and returned to the PT clinic at 2wks wearing a CAM boot. Which intervention would most likely be CONTRAINDICATED in the initial phase of rehab?
hip and knee strengthening
ankle muscle setting exercises
heel raises in standing
ambulation training with CAM boot
heel raises in standing
Pt now 6wks post-op and able to fully WB. Which of the following shoe modifications would be MOST APPROPRIATE for the patient?
normal shoes
shoes with 1-1.5cm heel lift
shoes with lower than the regular heel
shoes with 5cm heel lift
shoes with 1-1.5cm heel lift →allows slight PF to reduce strain on healing achilles tendon
❌1/4—excessive DF. strains repaired tendon
❌3—excessive PF, not recommended/beneficial at 6wks post-op
Pt presents with reduced hip mobility, particularly hip EXT. The PT notes that the patient experiences greater hip extension when the knee is extended compared to when the knee is flexed. What is the MOST LIKELY cause of the reduced hip extension with knee flexion?
Passive insufficiency of the hamstrings
Passive insufficiency of the gluteus maximus
Active insufficiency of the hamstrings
Active insufficiency of the rectus femoris
Active insufficiency of the hamstrings
Rationale: Active Insufficiency occurs when a 2-jt muscle can’t shorten enough to produce full ROM at both joints simultaneously. The hamstrings cross both the hip and knee joints. When the knee is flexed and the hip is extended, the hamstrings are shortening at both the knee and the hip. This dual action can lead to active insufficiency of the hamstrings because they are unable to generate sufficient force in this overly shortened state. In contrast, when the knee is extended, the hamstrings are lengthened over the knee, which allows them to contract more effectively at the hip, thus improving hip extension. Passive insufficiency of the hamstrings: This occurs when a muscle cannot lengthen enough to allow full range of motion at both joints it crosses.
A worker reports of difficulty gripping their tools tightly, and they repeatedly fall from their hand. On exam, the PT notices they can grip the tools tightly with their wrist in extension, but struggles to do so with the wrist in flexion. What is the MOST LIKELY cause of this issue?
Passive insufficiency of both flexor digitorum profundus and extensor digitorum
Passive insufficiency of flexor digitorum and active insufficiency of extensor digitorum
Active insufficiency of flexor digitorum profundus and passive insufficiency of extensor digitorum
Active insufficiency of both flexor digitorum profundus and extensor digitorum
Active insufficiency of flexor digitorum profundus and passive insufficiency of extensor digitorum
Rationale: When the wrist is flexed, the flexor digitorum profundus becomes shortened, limiting its ability to generate force for gripping. This is active insufficiency, The extensor digitorum is in a stretched position when the wrist is flexed, reducing its ability to extend the fingers efficiently. This is passive insufficiency. The flexor digitorum profundus (finger flexors) becomes actively insufficient, and the extensor digitorum (finger extensors) becomes passively insufficient, both contributing to the worker's difficulty gripping with the wrist in flexion.
A pt reports foot pain during running with excessive foot pronation. Which of the following orthotic interventions would MOST LIKELY benefit this patient?
medial post under first metatatsal head
cushion heel
lateral post under 5th metatarsal head
posterior leaf spring
medial post under first metatarsal head
Rationale: Correction of the overpronation can be done by a medial post placed just proximal to the first metatarsal head. This approach involves bringing the ground up to meet the foot. A post under the fifth metatarsal head would accentuate the problem. Cushion heel can be used for plantar fasciitis and a posterior leaf spring is used for a foot drop. Posterior leaf spring is used in weak dorsiflexors conditions.
Which of the following is MOST APPROPRIATE to measure the increased metabolic demand placed on the heart?
Systolic blood pressure
Rate product pressure
Diastolic blood pressure
Heart rate
Rate product pressure = myocardial O2 demand (HR*SBP)
Measures how hard heart working; useful in evaluating cardiac fxn during exs or stress testing
Higher RPP = incr cardiac workload and oxygen consumption
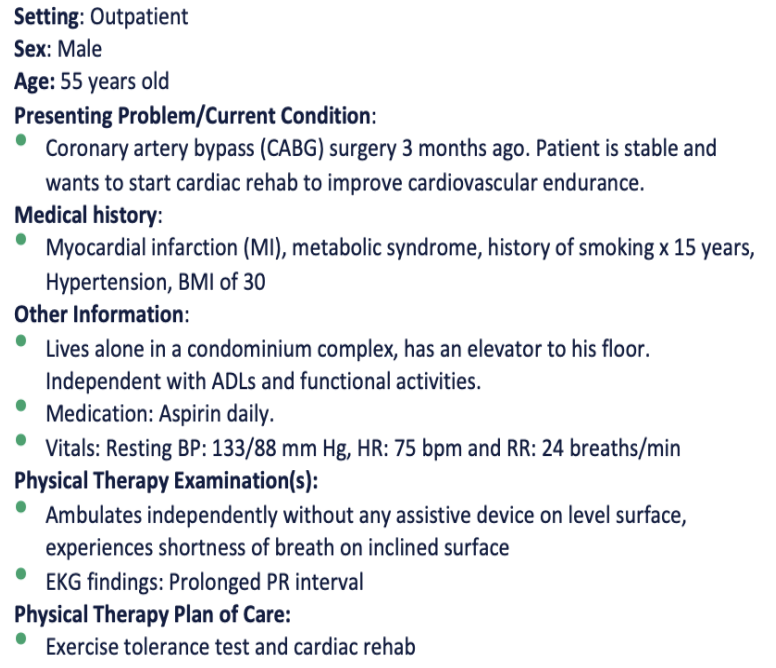
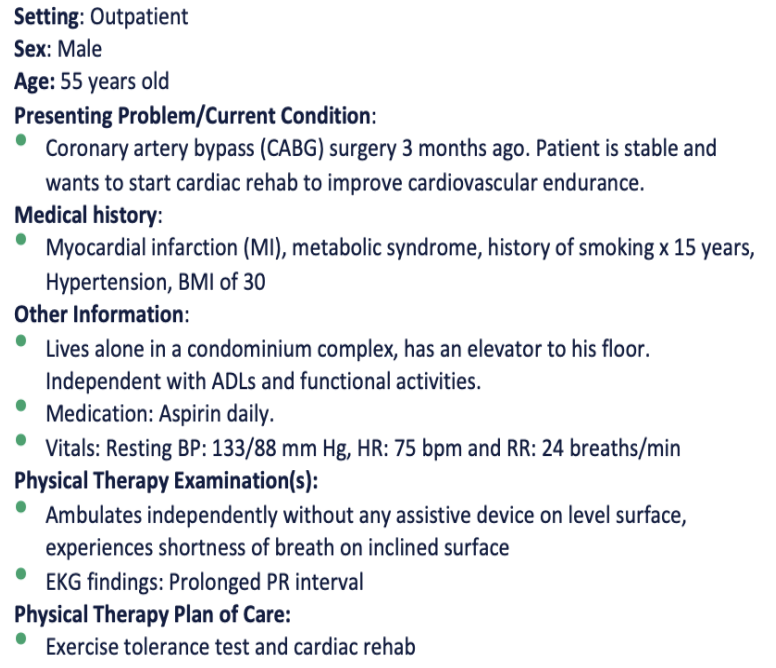
A PT is administering the 6MWT to assess the aerobic capacity of this patient. Which of the following statements regarding the test is MOST ACCURATE?
The PT must walk with the pt to observe SpO2 on the pulse oximeter
“Warm-up” or practice test should not be performed immediately before the test
The patient is allowed to take rest/breaks with the timer paused
The results of this test help to determine the cause of dyspnea
“Warm-up” or practice test should not be performed immediately before the test
Rationale: If a practice test is done, wait for at least 1 hour before the second test. The SpO2 should not be used for constant monitoring during the exercise. The technician must not walk with the patient to observe the SpO2. The patient is allowed to slow down, stop and rest as necessary but the timer continues to run. The 6MWT does not determine peak oxygen uptake, diagnose the cause of dyspnea on exertion, or evaluate the causes or mechanisms of exercise limitation.
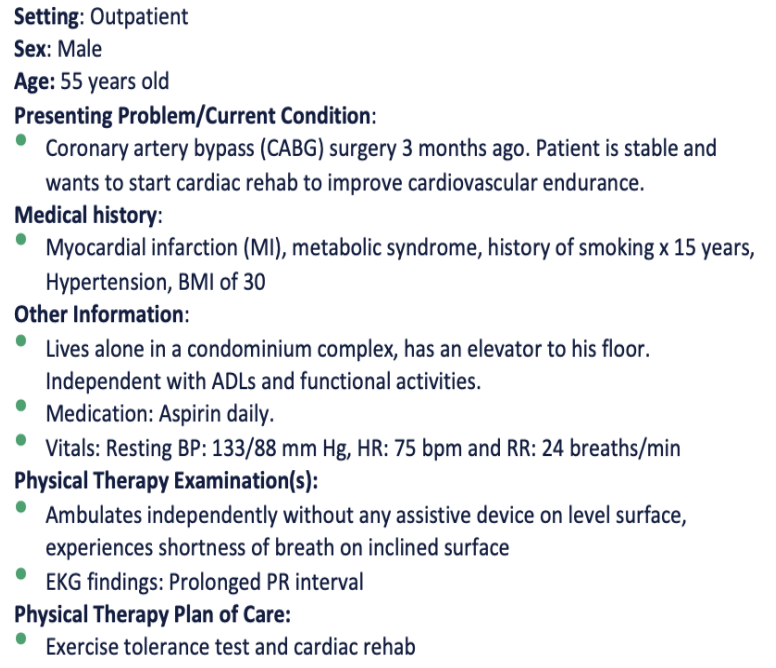
Which of the following categories is the MOST APPROPRIATE description for this type of hypertension?
Normal
Elevated
Prehypertension
Stage 1
Stage 1
Pre-hypertension is not used as a category any more based on the revised guidelines.
Normal: <120/80
Elevated: 120-129 / <80
Stage 1: 130-139 / 80-89
Stage 2: >140 / >90 mm Hg
Hypertensive crisis: >180 / >120 (req prompt med changes if no other indications of problems OR immediate hospitalization if S/S organ damage)
A healthy patient is working out on a stationary bike in an outpatient PT clinic. After the first four minutes of constant-load and submax exs, the VO2 reaches steady state. What does this indicate?
Levels of lactic acid in the blood has reached steady state
The ATP demand is being met aerobically
The exercise should be discontinued immediately
The respiratory rate is insufficient to meet the ATP demand
The ATP demand is being met aerobically
Rationale: Initially ATP produced by anaerobic pathways and after steady state is reached, ATP is produced aerobically. The volume of oxygen (not necessarily RR) needs to be sufficient to meet ATP demands.
Aerobic exercise: Uses oxygen for energy. Performed at moderate intensity over a long duration. (ex: jogging, cycling, swimming). Builds endurance and improves cardiovascular health.
Anaerobic exercise: Does not rely on oxygen; uses stored energy (glycogen/ATP). Done at high intensity for a short duration (ex: sprinting, heavy lifting, HIIT). Builds strength, power, and muscle mass.
A person goes for a hiking expedition. The base camp is at an altitude of 10,000ft above sea level. What are the INITIAL responses during their first few days at this altitude?
Increased respiratory rate, increased heart rate, increased cardiac output and no significant change in stroke volume
Decreased respiratory rate, decreased heart rate, decreased cardiac output and increased stroke volume
Increased respiratory rate, decreased heart rate with decreased cardiac output and increased stroke volume
Increased respiratory rate, increased heart rate with decreased cardiac output and decreased stroke volume
Increased respiratory rate, increased heart rate, increased cardiac output and no significant change in stroke volume
Rationale: At high altitudes, the body experiences hypoxia due to lower oxygen levels. The initial response includes an increase in respiratory rate (hyperventilation) to improve oxygen intake. The heart rate also increases (tachycardia) to enhance oxygen delivery to tissues. Initially, cardiac output increases because of the increased heart rate, while stroke volume typically remains unchanged.
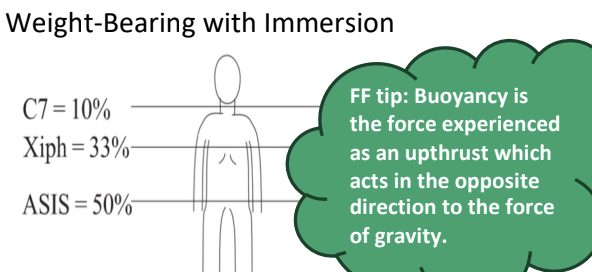
During aquatic therapy, a patient is immersed to the level of sternoclavicular notch. Which of the following is the MOST EXPECTED physiological response of aquatic tehrapy?
decreased cardiac output
increased venous return
increased heart rate
increased VO2 response
increased venous return →2/2 incr hydrostatic pressure of water, incr CO and SV
Everything else decreases (HR, SBP, VO2 response to exercise)
A pt’s chart states that they have been taking beta-blockers for the past 5yrs. Which of the following statements is correct regarding an exercise training program?
Greater benefits from cardiovascular exercise to be achieved at lower SBP rather than at higher SBP levels
Need to use measures other than HR to determine intensity of exercise
Greater benefits from cardiovascular exercise to be achieved at lower HR than at higher HR lvls
Need for longer warm-up periods and cool down periods during exercise sessions
Need to use measures other than HR to determine intensity of exercise
Beta blockers BLUNT HR →use RPE scale
Longer warm up and cool down ideal but for cardiac transplant
A patient recently completed a 10wk aerobic condition program. Compared to their initial evaluation, which of the following responses would MOST LIKELY be observed after the program?
slower HR recovery following exercise
higher resting RR
higher BP
lower resting HR
lower resting HR →2/2 incr SV and enhanced parasympathetic tone
also faster HR recovery, decr resting RR and BP at submax workloads (reliable indicator of improved fitness)

A patient reports SOB and fatigue. Which valve is being auscultated in the picture?
tricuspid valve
pulmonary valve
mitral valve
aortic valve
pulmonary valve
APTM 2245
Aortic— Rt 2nd IC space at sternal border
Pulmonary— Lt 2nd IC space at sternal border
Tricuspid— Lt 4th IC space at sternal border
Mitral—Lt 5th IC space at mid clavicular line
A clinician is performing cardiac auscultation and hears a “dub” sound. Which of the following is associated with this heart sound?
closing of bicuspid and tricuspid valves
opening of bicuspid and tricuspid valves
closing of aortic and pulmonary valves
abnormal heart rate
closing of aortic and pulmonary valves
❌1/2—closure mitral and tricuspid valves = “lub” S1 heart sound
S4 is most commonly heard in patients with HTN, left ventricular hypertrophy, increased left ventricular end diastolic pressure, pulmonary hypertension, and pulmonary stenosis. S3 is the common in CHF which is an indication of a insufficient left ventricular which occurs as blood continuously fill a relaxed left ventricle during early diastole.
A pt presents with speech difficulties such that their speech is slow and laborious. They frequently omit small grammatical words, such as “is” and “the”, while speaking. However, they seem to understand the spoken language quite well. Based on this information, which of the following conditions does the patient MOST LIKELY have?
Wernicke’s aphasia
Broca’s aphasia
Global aphasia
Lesion to CN V
Broca’s aphasia
Rationale:
Broca's aphasia: non-fluent, expressive aphasia (difficulty with speech production)
Wernicke's aphasia: fluent but nonsensical speech, receptive aphasia (difficulty understanding)
Global aphasia: severe impairments in both speech production and comprehension, which is inconsistent with the patient’s preserved comprehension abilities.
CN V lesion will not cause Aphasia.
During assessment of pupillary light reflex, when the light is shone into the L eye, the L pupil constricts, and the R pupil remains dilated. What is the MOST LIKELY explanation for these findings?
R optic nerve damage
L optic nerve damage
R oculomotor nerve damage
L oculomotor nerve damage
R oculomotor nerve damage
Rationale:
In the pupillary light reflex, when light is shone into one eye, both the IL and CL eye responses should occur.
When light is shone into the right eye, both pupils constrict, indicating that the sensory input from the right eye (via the right optic nerve) and the motor output to both pupils (via the oculomotor nerves) are functioning correctly.
When light is shone into the left eye, only the left pupil constricts, and the right pupil remains dilated. This suggests that the sensory input from the left eye is intact (as the left pupil constricts directly), but the consensual response is impaired.
This pattern indicates damage to the right oculomotor nerve. The right oculomotor nerve is responsible for constriction of the right pupil in response to light shone in either eye. If the right oculomotor nerve is damaged, the right pupil will not constrict in response to light shone in the left eye, leading to the observed finding of the left pupil constricting but the right pupil remaining dilated.
A pt presents with lesion to CN V (trigeminal) and CN VII (facial). Considering the location of lesion, which other nerve is MOST LIKELY to be affected?
CN III (oculumotor)
CN IX (glossopharyngeal)
CN VIII (vestibulocochlear)
CN XII (hypoglossal)
CN VIII (vestibulocochlear)
Rationale:
CN V (Trigeminal) and CN VII (facial) are both located in the pons and so is CN VIII (Vestibulocochlear)
CN III (Oculomotor) is in the Midbrain and CN IX (Glossopharyngeal) and XII (Hypoglossal) are in the medulla
Ophthalmic nerve (V1), Maxillary nerve (V2), and Mandibular nerve (V3).
A patient presents to a TMJ specialist for jaw pain. On exam, there’s weakness of the masseter and temporalis muscles on the same side, and their jaw deviates to the R when they open their mouth. Sensory exam revealed reduced sensation over R lower jaw+chin. Which of the following functions is MOST LIKELY impaired along with this presentation due to the nerve damage described?
Smiling
Chewing
Swallowing
Moving tongue
Chewing →triCHEWminal nerve
❌1. Smiling—facial (CN7)
❌3. Swallowing—glossopharyngeal and vagus (CN9/10)
❌4. Moving tongue—hypoglossal (CN12)
A pt reports experiencing sudden onset mild hearing loss on L side. Rinne’s test was consistent with bone conduction greater than air conduction on both sides. Weber’s test findings show sound was louder in the L ear. Which of the following is MOST APPROPRIATE?
R side sensorineural hearing loss
L side conduction hearing loss
R side conduction hearing loss
L side sensorineural hearing loss
L side conduction hearing loss
Rationale: BC > AC === Conductive hearing loss;
Using mnemonic CANS – with conductive hearing loss, sound is LOUD in affected ear i.e. left ear;
In the Weber test, a tuning fork is placed on the forehead. If the sound is localized by the patient to the contralateral side of the involved ear, then the hearing loss is sensorineural. In unilateral conductive loss, the sound is localized to the involved side. In Rinne test, vibrating tuning fork is placed on mastoid bone, then close to ear canal. Normal finding include sound heard longer through air than bone. With Conductive loss, sound heard through bone is equal to or longer than air; with Sensorineural loss: sound heard longer through air. The results of these two tests are used together to differentiate a sensorineural loss from a conductive loss.
A pt presents with concerns of difficulty speaking and swallowing. Upon exam, the pt’s tongue deviates to the R when protruded, and there is noticeable atrophy of the R side of the tongue. What is the MOST LIKELY diagnosis related to the findings observed and which CN is affected?
R vagus nerve (CN X) lesion
L hypoglossal nerve (CN XII) lesion
R hypoglossal nerve (CN XII) lesion
L facial nerve (CN VII) lesion
R hypoglossal nerve (CN XII) lesion →weakness and atrophy on SAME side
Considering the pt’s presentation, which lobe is MOST LIKELY affected?
R parietal lobe
L temporal lobe
L frontal lobe
R occipital lobe
R parietal lobe
❌2/3—L hemineglect and sensation loss so lesion has to be on R
❌4—occipital lobe assists vision, no deficits in case description
Considering that the pt has a lesion to spinal accessory N, which of the following will MOST LIKELY be seen?
inability to extend the spine
inability to shrug shoulders
inability to push up from chair
inability to extend the arm beyond neutral
inability to shrug shoulders →innervate UT/SCM (SB+opp rot also affected)
Based on the pt’s assessment, which of the following functions are expected to be intact in this case?
ability to taste from anterior tongue
ability to smile
pupillary light reflex
ability to open eyelids
ability to open eyelids →intact bc CN3 not involved
❌1/2—smile and taste ant tongue = facial (CN7)
❌3—pupillary reflex = optic (CN2)
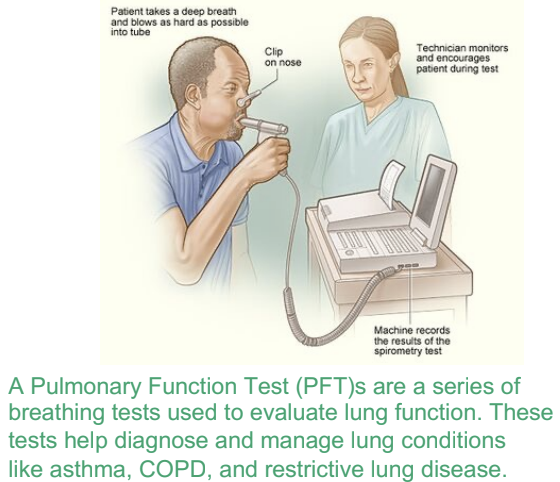
A clinician is performing spirometry to assess the lung function of patient. After a normal exhalation, the clinician asks the patient to exhale the maximal amount of air they can. Which of the following parameters is being assessed with this action?
inspiratory capacity
expiratory reserve volume
total lung capacity
tidal volume
expiratory reserve volume
❌TV=normal inhale+exhale each quiet breath
❌IC=max air that can be inhaled after normal tidal exhalation (TV+IRV)
❌TLC=TV +IRV +ERV +RV
A patient diagnosed with idiopathic pulmonary fibrosis has been participating in PT in the hospital. Which of the following is MOST LIKELY to be seen on a pulmonary function test?
increased tidal volume
decreased inspiratory reserve volume
increased residual volume
increased functional residual capacity
decreased inspiratory reserve volume
Rationale: All lung volumes are decreased in restrictive conditions. With COPD, RV, FRC and TLC increases
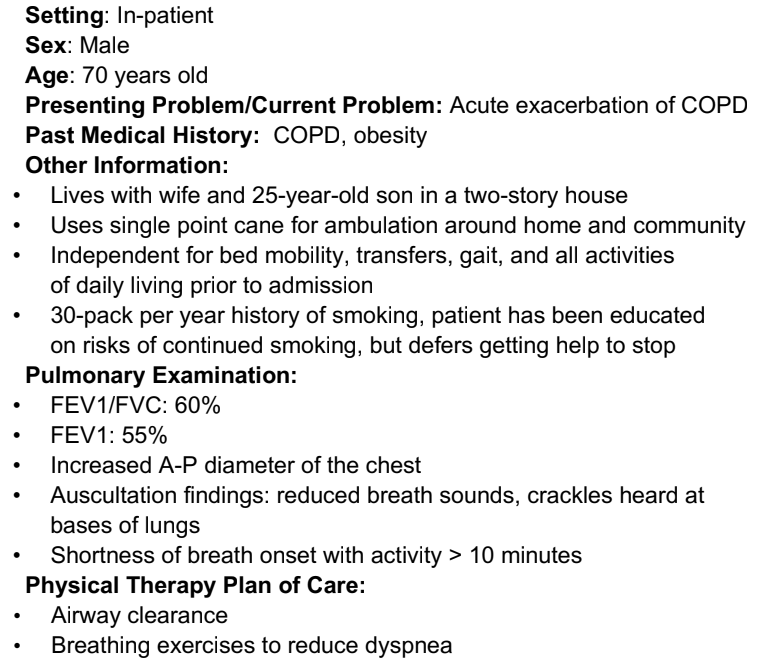
Which of the following changes are MOST LIKELY seen on pulmonary function tests during exacerbation of symptoms?
increased FEV1 and reduced RV
reduced FEV1 and reduced RV
increased FEV1 and increased RV
reduced FEV1 and increased RV
reduced FEV1 and increased RV
COPD = obstructive so air can’t get OUT
Dec FEV1 2/2 airway narrowing (<80% predicted value)
Inc FRC and RV 2/2 air trapped
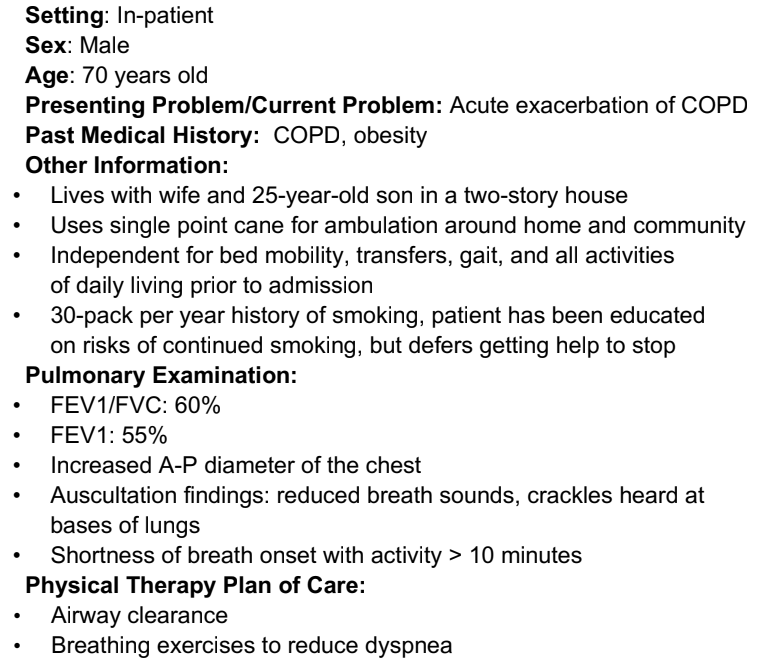
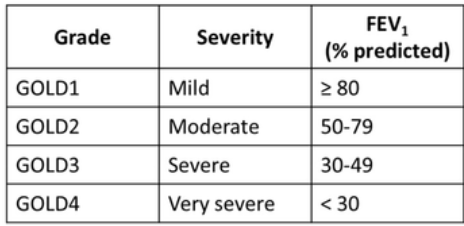
According ot the GOLD classification, how would a PT classify the patient’s severity of COPD?
very severe
severe
moderate
mild
moderate
During examination, the PT finds that a patient has a weak wet cough. Which is MOST APPROPRIATE to help this patient clear secretions?
assisted coughing in the supine position
postural drainage in the sidelying position
huffing
mechanical percussion
huffing
Rationale: Patient has the ability to cough so we want to train/facilitate it further.
3— Huffing is a gentler form of coughing used to remove secretions. with an open glottis (opening between the vocal cords) while exhaling without pursing lips. This is similar to fogging the mirror. Huffing makes it easier to move mucus out of the lungs and stabilizes airways, prevents collapse.
1— is used for weak abdominals in SCI and not applicable in this condition.
2— Postural drainage facilitates drainage of secretions to the level of the segmental bronchus only. In addition, a cough is needed to clear secretions.
4— Percussion helps mobilize secretions from the periphery of the lungs; however, it does not improve to clear the secretions.
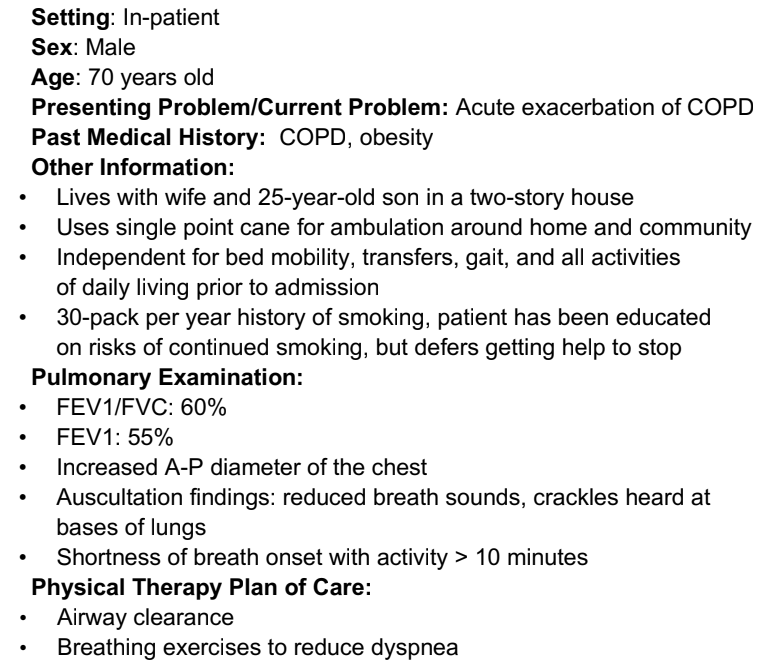
During a pulmonary exam, the clinician hears low-pitched sounds over the lateral border of the scapula. Which of the following sounds is the clinician auscultating?
vesicular sounds
bronchial sounds
broncho-vesicular sounds
tracheal sounds
vesicular sounds →soft/low pitch normal breath sounds throughout lungs (best heard at lung bases)
❌2. bronchial—heard over manubrium
❌3. broncho-vesicular—medium pitched w/ equal ins+exp heard over 1st/2nd interspace anteriorly b/w scapulae
❌4. tracheal—heard over trachea
Which of the following high-pitched breath sounds is MOST LIKELY associated with the diagnosis of CHF?
rhonchi
wheeze
crackles
pleural rub
crackles
❌rhonchi—low pitch
❌wheeze—asthma/COPD
❌pleural rub—pneumonia
During a pulmonary exam, the PT places the stethoscope on the patient’s thorax and asks the patient to say “E”, but hears an “A” sound instead. What is the MOST LIKELY diagnosis?
bronchial asthma
lobectomy
pneumonia
pneumothorax
pneumonia
aka “egophony” 2/2 lung consolidation
pneumonia inflames air sacs →consolidate w/fluid or pus →enhances sound transmission
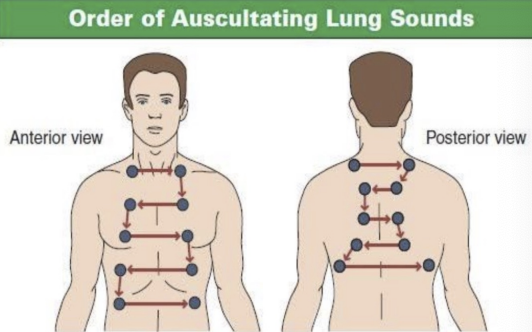
The PT is reviewing the chart of an ICU patient. Based on the following lab report, the pt MOST LIKELY has been diagnosed with an uncompensated form of which condition?
metabolic acidosis
respiratory alkalosis
respiratory acidosis
metabolic alkalosis
respiratory alkalosis
Norm pH 7.35-7.45 →high pH means alkalosis
Norm PaCO2 35-45 →low means respiratory issue
Norm HCO3 22-26 →norm in case
A patient, who is a chronic smoker, is diagnosed with COPD and undergoes ABG analysis. The PT is MOST LIKELY to see which of the following changes in the ABG report?
decreased PaCO2, increased PaO2, and decreased pH
decreased PaCO2, decreased PaO2, and increased pH
increased PaCO2, increased PaO2, and increased pH
increased PaCO2, decreased PaO2, and decreased pH
increased PaCO2, decreased PaO2, and decreased pH
air trapped in COPD (can’t get OUT)
CO2 builds up, Lower O2 →strongly drives pH to be acidic or lower
Presence of which of the following signs is MOST INDICATIVE of a lesion distal to the anterior horn cell?
Positive Babinski, presence of spasticity and foot drop
Negative Babinski, decrease in muscle tone and sensation
Increase in muscle tone and no change in sensation, presence of resting tremor
Presence of intentional tremors and nystagmus
Negative Babinski, decreased in muscle tone and sensation
UMN: +Babinski, exaggerated cutaneous reflexes/incr reflexes, disuse atrophy, synergy, incr tone
LMN: fasciculations, neurogenic atrophy, hyporeflexia, dec/absent cutaneous reflexes
Cerebellar: intentional tremor
BG: resting tremor
Which of the following is MOST LIKELY to be seen in a patient with diagnosis of Parkinson’s disease?
increased trunk rotation
increased step width
anosmia
macrographia
anosmia
❌1—trunk rotation reduced 2/2 rigidity and bradykinesia
❌2—NBOS shuffling gait
❌4—micrographia (small handwriting, not enlarged writing)
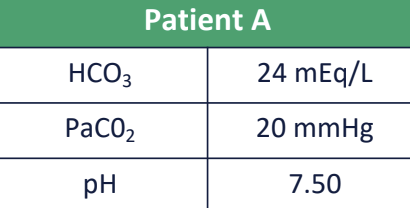
According to the Hoehn and Yahr classification of disability, which of the following classification of disability is the MOST APPROPRIATE about Stage III?
inability to walk without rollator
confined to wheelchair
may be able to live independently and continue employment
balance not impaired
may be able to live independently and continue employment
❌1—rollator use is stage 4
❌2—WC use is stage 5
❌4—balance not impaired with stages 1/2
During the PT session, the clinician notices that the patient with Parkinson’s disease suddenly begins twitching their lips and performs involumtary snake-like motions with their arms. What could be the cause of present symptoms?
Patient has skipped his levodopa dose
Patient is at peak levodopa dose
Patient is in honeymoon period
Patient is in the off state of levodopa
Patient is at peak levodopa dose
The twitching lips and invol snake-like arm motions are likely a manifestation of dyskinesia (common side effect of PD treatment), particularly at peak doses of levodopa
Which of the following clinical findings is MOST CHARACTERISTIC of Multiple Sclerosis?
Symmetrical distal muscle weakness with sensory loss in a glove-and-stocking pattern
Sudden onset of flaccid paralysis with absent reflexes
Visual disturbances, fatigue, and limb weakness that vary in intensity over time
Resting tremor and bradykinesia with unilateral onset
Visual disturbances, fatigue, and limb weakness that vary in intensity over time →chr demyelinating disorder
❌1—Peripheral neuropathy
❌2—GBS
❌4—Parkinson’s
A patient with ALS has weakness of all extremities and gets fatigued very easily while doing activities of daily living. Which of the following will be CONTRAINDICATED for this patient to maintain mobility and function as much as possible?
recommending soft foam collar for neck
taking frequent breaks during activities
recommended HKAFO and walking for ambulation
slow, prolonged stretches and ROM exercises for upper and lower extremities
recommended HKAFO and walking for ambulation
Rationale: Weight of the device is an important factor to consider in decision making, while also considering which device will ensure optimal function and safety. Wheeled walkers, which do not require the patient to lift the device, are usually recommended. It is also important to consider the weight of the orthosis as individuals with ALS will have energy expenditure issues, and it may be more fatiguing for the patient to ambulate with a heavy orthosis than to ambulate without the impairment being corrected. For this reason, a KAFO is not recommended. Head drooping forward can lead to impairment in ambulation and feeding. Patients may compensate by increasing lordosis as they attempt to maintain their posture during ambulation. For mild to moderate cervical weakness, a soft foam collar may be worn during specific activities. Physical therapists can perform and instruct caregivers in slow prolonged stretches and passive ROM exercises to address spasticity. Educating on activity pacing and importance of taking frequent breaks is essential.
A patient with GBS is in rehab and is beginning to regain some muscle strength. Which of the following is the MOST APPROPRIATE initial intervention to address muscle weakness and functional recovery?
High-intensity interval training to rapidly increase muscle strength and endurance
Progressive resistance exercises with a focus on low-mod intensity and high repetitions
Functional task-specific training with a focus on activities like running and jumping
Continuous passive motion exercises to maintain joint range of motion without muscle engagement
Progressive resistance exercises with a focus on low-mod intensity and high repetitions
Rationale: In the recovery phase of Guillain-Barré Syndrome, the goal is to gradually rebuild muscle strength and functional ability while avoiding overexertion. Progressive resistance exercises at a low to moderate intensity and high repetitions help in strengthening muscles safely as the patient regains strength. High-intensity interval training and complex activities like running and jumping may be too strenuous and premature, while continuous passive motion exercises do not sufficiently engage the muscles needed for functional recovery
Which of the following diagnosis is the patient MOST LIKELY expected to have?
ALS
GBS
MS
Cerebellar tumor
MS
❌UMN signs so either ALS/MS, rule out GBS
❌ALS does not have sensory deficits
❌Cerebellar tumor does not cause inc’d tone
The PT decides to assess the patients pupillary reflexes. On shining light into the pt’s L eye, both pupils constrict; however, on shining light into the pt’s R eye, both pupils paradoxically dilate. Which of the following is MOST LIKELY diagnosis and cause of this presentation?
Marcus Gunn pupil; Lesion to R CN II
Cataract; Lesion to R CN III
Cataract; Lesion to L CN II
Marcus Gunn pipil; Lesion to L CN III
Marcus Gunn pupil; Lesion to R CN II
❌2/3—Cataracts is clouded lens, would not cause abn dilation
❌4—MGP assoc’d w/CN2 not 3
Which of the following is the MOST APPROPRIATE recommendation for this patient?
Exercise sessions should be scheduled at the same time every day in the evening for consistency
Rest breaks and activity pacing should be incorporated based on the patient’s symptoms
During pool therapy, the temperature of the water should be 87°F
Balance and proprioceptive training must be avoided to prevent falls during rehabilitation
Rest breaks and activity pacing should be incorporated based on the patient’s symptoms
MS pts = heat intol +fatigue!!
❌1—exs sessions should alt days and during optimal times e.g., AM (core temp lowest, before fatigue!!)
❌3—pool should be <85°F
❌4—helps control ataxic mvts (tremor, dysmetria)
A patient with a diagnosis of L MCA is MOST LIKELY to have which of the following signs and symptoms?
excessive weakness of the RLE
neglect of the L side of the body
L homonymous hemianopsia
Inability to understand words spoken by the therapist
Inability to understand words spoken by the therapist
❌1—LE weakness = ACA stroke
❌2—Hemi neglect = R stroke
❌3—Homonymous hemianopsia = PCA stroke
A patient presents with sudden onset of weakness on one side of the body. When asked, they were unable to name their friend who accompanied them to the hospital. During assessment, they were able to write a sentence perfectly but was unable to read their sentence. A lesion in which of the following is the MOST LIKELY cause of this symptom?
Superior division of MCA
Central territory of PCA
Inferior division of MCA
Peripheral territory of PCA
Peripheral territory of PCA →dyslexia w/o agraphia
❌1—superior MCA = Broca’s aphasia
❌3—inferior MCA = Wernicke’s aphasia
❌2—central PCA = thalamic pain
With respect to the upper extremity, which of the following MOST ACCURATELY describes the position at rest?
forearm pronation with wrist and finger flexion and thumb abduction
forearm supination with wrist extension finger flexion, thumb adduction
shoulder in adduction and internal rotation and thumb adduction
shoulder abducted, externally rotated, elbow flexed, forearm supinated
shoulder in adduction and internal rotation and thumb adduction
Rationale: Position at rest is the position due to spasticity. For upper extremity spasticity the shoulder is abducted and internally rotated, elbow is flexed, forearm is pronated, wrist and fingers are flexed, thumb is adducted.
The pt has extreme spasticity, and she demonstrates flexion synergy patterns of the UE while attempting to move her UE. Which is MOST LIKELY to be seen when she lifts her arm and what is the appropriate classification per the Brunnstrom staging?
shoulder ER, abducted, elbow and wrist flexed and forearm supinated; Stage III
shoulder IR, adducted, elbow and wrist flexed and forearm supinated; Stage III
shoulder ER, abducted, elbow and wrist extended, and forearm pronated; Stage IV
shoulder IR, abducted, elbow and wrist flexed and forearm pronated; Stage V
shoulder ER, abducted, elbow and wrist flexed and forearm supinated; Stage III
Rationale: Stage III– increase spasticity and synergy. Flexion Synergy pattern for upper extremity is shoulder external rotation, abduction, elbow flexed, forearm supinate, wrist and fingers flexed.
Which is the MOST APPROPRIATE position while lying on the right side?
Head/neck: right scapula protracted; right arm slight abd and ER; elbow extended and forearm supinated, wrist neutral, fingers extended, and thumb abducted
Head/neck: neutral, right scapula retracted; right arm slight abd and IR; elbow extended and forearm pronated, wrist neutral, fingers extended, and thumb adducted
Head/neck: neutral, right scapula retracted; left arm slight abd and IR; elbow extended and forearm pronated, wrist neutral, fingers extended and thumb adducted
Head/neck: neutral, left scapula protracted; left arm slight add and ER; elbow flexed, forearm supinated, wrist extended, fingers flexed, and thumb abducted
Head/neck: right scapula protracted; right arm slight abd and ER; elbow extended and forearm supinated, wrist neutral, fingers extended, and thumb abducted
Rationale: L CVA = R hemiparesis. Effective strategies while sidelying on affected side:
• Head/neck: Neutral and symmetrical
• Trunk: Aligned in midline
• More affected UE: Scapular protracted; shoulder forward; arm placed in slight abduction and external rotation; elbow extended, forearm supinated, wrist neutral, fingers extended, and thumb abducted
• More affected LE: Hip extended and knee flexed and supported by pillows. An alternative position is slight hip and knee flexion with pelvic protraction
Upon further exam, the pt seems to be in a heightened state of activity and is making up stories. They are not coordinating with the therapist at all. How would the PT MOST LIKELY classify this patient’s level of cognition?
Level VI
Level IV
Level V
Level III
Level IV →confused agitated →erratic/non purposeful behavior, incoherent confabulation and verbalizations
❌1. Level VI (confused appropriate) →goal directed behavior but relies on external input, simple commands consistent, demos carryover for all task
❌3. Level V (confused inappropriate) →consistent simple commands, not purposeful responses, random/fragmented and verbalization inappropriate at times with confabulating
❌4. Level III (localized response) →pt reacts specifically but inconsistently to stimuli, inconsistent simple commands (EC, squeeze hand)
Which of the following strategies will be MOST BENEFICIAL while working with the patient?
Having a different clinician work with the patient every day so he gets used to meeting new people
Involving patient in group therapy so he can make friends
Informing the patient two days in advance about what to expect in the next few physical therapy sessions
Giving the patient two options and having the patient select one
Giving the patient two options and having the patient select one
Rationale: Since the patient is confused and agitated, orienting the patient is important and giving them options is beneficial so they think they are in control. Involving multiple people or doing group therapy will agitate the patient even more and will not be beneficial. Informing the patient 2 days in advance is of no use since patient has memory deficits.
If the patient becomes agitated during a session, what is the best initial response?
Leave the patient alone to calm down on their own
Use calming techniques to distract the patient
Correct the patient to discourage aggressive behavior
Restraint the patient to calm them and avoid harm
Use calming techniques to distract the patient
Rationale: Gently redirecting after the patient regains control helps refocus their attention without escalating the situation. Confrontation or demanding explanations may increase agitation. Restraint is a last resort and should only be used if the patient is a danger to themselves or others.
A patient presents with lymphedema post mastectomy. All of the following are causes of secondary lymphedema EXCEPT which cause?
Infection
Milroy’s disease
Fibrosis
Chronic venous insufficiency
Milroy’s disease
Rationale: Milroy's disease is a familial disease characterized by lymphedema, commonly in the legs, caused by congenital abnormalities in the lymphatic system. Disruption of the normal drainage of lymph leads to fluid accumulation and hypertrophy of soft tissues. Milroy’s disease is congenital and is a primary cause of lymphedema. Infection, Fibrosis and Chronic venous insufficiency are secondary causes of lymphedema. Secondary lymphedema is a result of an injury to the lymphatic system. Forms of secondary lymphedema are surgery, inflammation or infection, obstruction, or fibrosis, combined venous-lymphatic dysfunction (chronic venous insufficiency).
A patient with lymphedema presents with notable swelling that is hard and fibrotic, has a positive Stemmer’s sign, and hyperkeratosis of skin. Which of the following stages of lymphedema would the patient MOST LIKELY be in?
Stage 0
Stage 1
Stage 2
Stage 3
Stage 3
❌0—no edema
❌1—edema w/activity, reduced on elevation
❌2—hard swelling→non pitting brawny, +Stemmer’s sign
A clinician is evaluating a patient with lymphedema and documents it is an “early-stage 2 lymphedema with pitting edema grade 3+”. Which of the following MOST APPROPRIATELY describes the clinical presentation?
the indentation produced is greater than 1 inch
the indentation on finger pressure lasts for less than 15sec
the indentation on finger pressure lasts for 20sec
the indentation produced is less than ½ inch
the indentation of finger pressure lasts for 20sec →3+ =severe, lasts 15-30sec, ½-1in pitting
2+ Indentation is <½in for <15sec (Option B and D)
Which of the following signs would indicate INITIAL development of lymphedema in a patient seen post radical mastectomy with axillary node removal?
non-pitting edema of the forearm
shallow wound beds on the forearm
atrophy of the biceps muscle
decreased range of motion of the fingers
decreased range of motion of the fingers
❌1—non pitting fibrotic edema is Stage 3
❌2—shallow wound beds in later stages or 2/2 venous insufficiency
❌3—biceps atrophy in later stages 2/2 disuse or musculocutaneous N injury
A clinician is evaluating a patient with lipedema. Which of the following is MOST LIKELY seen as patient’s presentation?
Pt is susceptible to bruising of the affected area
Pt would have a positive Stemmer’s sign
Pt has a high likelihood of developing cellulitis
Pt would have asymmetrical involvement of the LE
Pt is susceptible to bruising of the affected area
Lipedema: pain on pressure, susceptible to bruising of affected extremity
Lymphedema: +Stemmer’s sign, susceptible to cellulitis
When examining the lymph nodes, which presentations are MOST LIKELY to require referral to physician?
small (<1cm in diameter), mobile, and non-tender lymph nodes in the axillary region
soft and freely moveable lymph nodes in the axillary region
firm, non-tender and fixed lymph nodes in the axillary region
enlarged (>1cm in diameter), tender, mobile lymph nodes following a recent diagnosis of upper respiratory infection
firm, non-tender and fixed lymph nodes in the axillary region
Rationale: Lymph nodes up to 1 cm in diameter of soft-to-firm consistency that move freely and easily without tenderness are considered within normal limits. Lymph nodes more than 1 cm in diameter that are firm and rubbery in consistency or tender are considered suspicious. Enlarged lymph nodes associated with infection are more likely to be tender, soft, and movable than slow-growing nodes associated with cancer.
What would be the BEST way to measure edema around the upper arm?
circumferential measurement
water displacement method
doppler US
lymphoscintigraphy
circumferential measurement →for proximal area lymphedema
❌2—water displacement for distal edema measurement
❌3—doppler for venous insufficiency measurement
❌4—lymphoscintigraphy for lymphatic insufficiency measurement
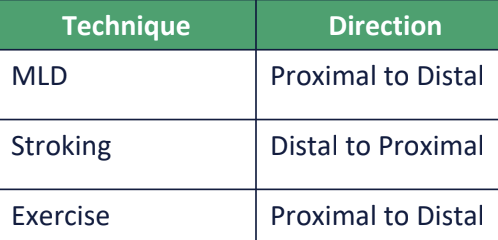
Which of the following statements is the CORRECT intervention for this patient?
the trunk and axilla should be decongested first followed by arm and hand
manual lymphatic drainage should involve proximal to distal stroking
the hand should be decongested first followed by trunk and axilla
affected limbs are bandaged with high-stretch compression bandages
the trunk and axilla should be decongested first followed by arm and hand
❌2—dist→prox stroking
❌3—prox→dist drainage!!
❌4—short compression bandages!
PT is developing an exercise program. Which exercise should the pt perform FIRST?
elbow flexion
cervical rotation
shoulder abduction
shoulder circumduction
cervical rotation
Rationale: Exercises are performed from proximal to distal areas. Cervical rotation (trunk) will be performed before shoulder movement and elbow flexion will be performed last.
A patient presents to the clinic with RLE edema that reduces on elevation of the LE. Which of the following should be AVOIDED for this patient?
Treadmill walking
Swimming
Walking barefoot outdoors
Air travel
Walking barefoot outdoors →skin breakdown!!
❌4—air travel w/compression garments, periodic walking breaks to reduce swelling 2/2 decr air pressure
❌1/2—recommended
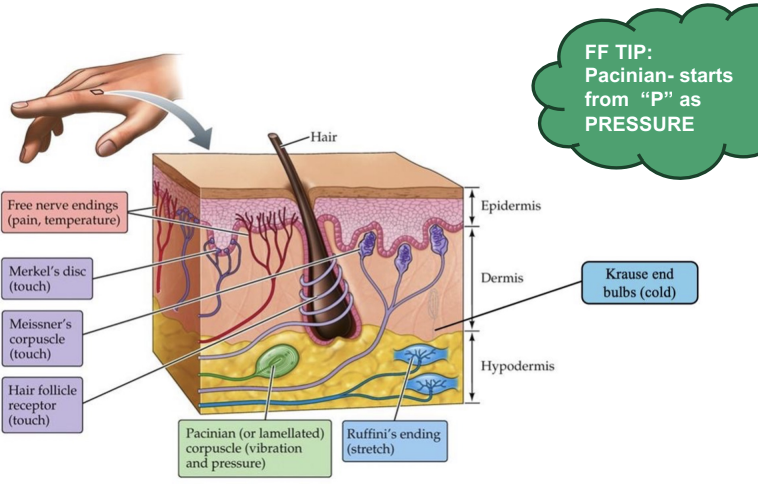
During assessment of skin sensation, which of the following structures are responsible for transmission of pressure and vibration sensation?
Meissner corpuscles
Krause end bulbs
Pacinian corpuscles
Ruffini endings
Pacinian corpuscles →Pressure and vibration sensory modalities
❌1—Meissner corpuscles = fine/discriminative touch, vibration
❌2—Krause end bulbs = cold sensation
❌4—Ruffini endings = heat sensation
A patient presents with a RLE wound and has h/o painful cramping in the legs, esp after walking for a few minutes. Medical history significant for DM2 and HTN. Which would BEST describe the characteristic of this wound?
wound located on the dorsum of toes, base of the wound is pale and necrotic with lack of granulation tissue
wound located on the dorsum of the foot, hemosiderin staining present along with fibrosis of dermis
wound located on the medial malleolus with swelling of BLEs that is relieved with rest
pitting edema in the LEs, numbness and tingling along the hyperkeratosis of the skin
wound located on the dorsum of toes, base of the wound is pale and necrotic with lack of granulation tissue →PMH/int claud indicates arterial insufficiency

A PT is treating a patient, who was originally diagnosed with a pressure injury stage 3. The patient presents to the lcinic with ulcer shown below. Which of the following is true?
The pressure injury is now an unstageable ulcer
The pressure ulcer is now a stage 1 ulcer
The pressure ulcer is now a stage 2 ulcer
A pressure ulcer can not be back-staged
A pressure ulcer can not be back-staged
Rationale: A stage III pressure ulcer is classified as full-thickness tissue loss in which subcutaneous fat is visible but muscle, tendon, and bone are not visible. Once a pressure injury is designated Stage 1, 2, 3, or 4, it remains classified in that stage. Pressure injuries are not back-staged even though they improve.
A pt develops a stage 2 pressure injury over the sacrum and is referred to PT for wound care. Which of the following is the MOST APPROPRIATE initial application to clean the wound?
povidone-iodine solution
sterile normal saline
zinc oxide cream
nitrofurazone solution
sterile normal saline →initial agent to clean wound
❌1—povidone iodine to prepare skin for surgery
❌3—zinc oxide for dental fillings, local surface treatment of skin disorders
❌4—nitrofurazone for infected burns, skin infections 2/2 skin grafts
A patient has a deep partial-thickness wound with 70% necrosis and 30% granulation tissue. Which of the following is MOST APPROPRIATE wound care option?
wet to dry dressings
autolytic debridement
enzymatic debridement
biological debridement
wet to dry dressings
>50% necrotic so need nonselective debridement
all other options are selective debridement

A patient has a grade 3 pressure ulcer. The wound has excessive amounts of exudate present. Which of the following is the MOST APPROPRIATE dressing to use?
hydrofiber dressing
hydrocolloid dressing
hydrogel dressing
transparent film
hydrofiber dressing
❌4—transparent film: min drainage
❌2/3—hydrogel/hydrocolloid for min exudate
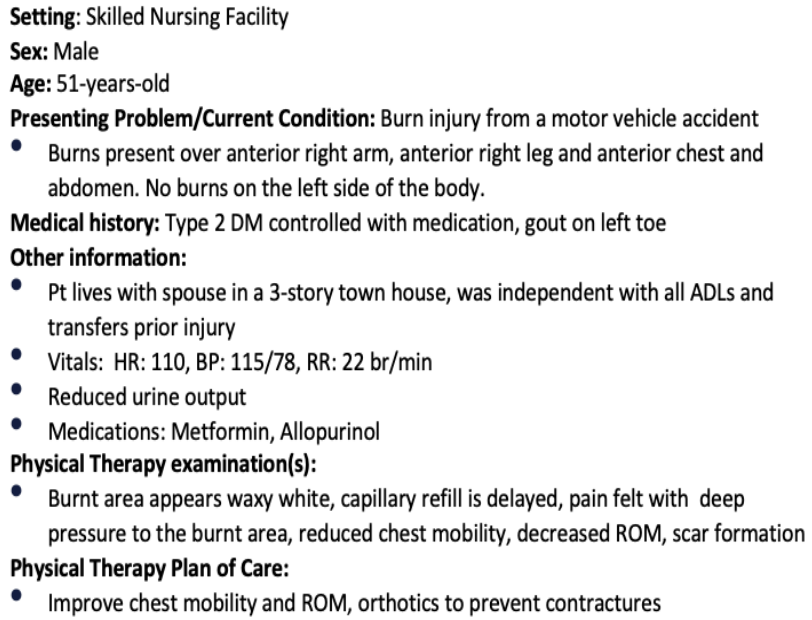
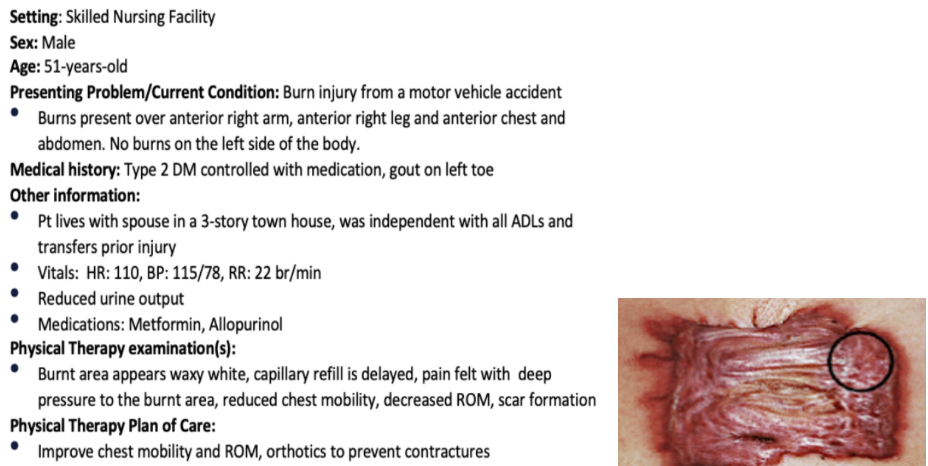
Which type of burn does this patient have?
superficial burn
superficial partial-thickness burn
deep partial thickness burn
subdermal burn
deep partial thickness burn
Rationale: Epidermal produces no scar and have intact skin. Superficial partial-thickness are painful to touch, temperature, have a brisk capillary refill produces minimal scarring. Deep partial-thickness are waxy white, have pain on deep pressure, delayed capillary refill and results in excessive scarring and the development of hypertrophic and keloid scars is a frequent consequence. Subdermal burns are Charred, dry and exposed deep tissue and often require amputation.
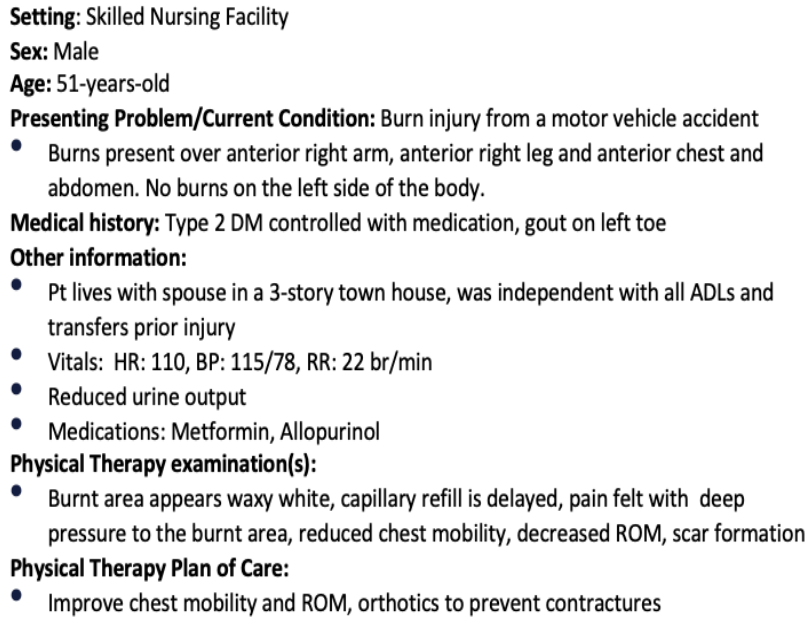
Which of the following BEST represents the percentage of body surface area involved?
31.5%
18%
36.5%
45%
31.5%
Rationale: Anterior trunk = 18%
Anterior R LE = 9%
Anterior R UE = 4.5%
During follow-up a few months later, the patient is concerned about a scar on his right arm, as shown below. What is the type of scar seen in this patient?
normal scar
hypertrophic scar
atrophic scar
keloid scar
keloid scar →excessive scar tissue grows outside original wound margins
❌1—normal scar: flat, similar to skin color
❌2—hypertrophic scar: thick fibrous tissue that remains w/in original wound border
❌3—atrophic scar: sunken, hyperpigmented 2/2 collagen loss (rare)
A PT is examining the gait of a patient and suspects a leg length discrepancy. Which of the following gait deviations is MOST LIKELY seen by the therapist?
increased dorsiflexion of the short limb during swing and increased plantarflexion of the long limb during stance
decreased knee flexion and increased dorsiflexion of the long limb during stance and increased dorsiflexion of the short limb during swing
increased dorsiflexion with early heel rise of the long limb at heel off and increased plantarflexion of the short limb during stance
increased plantarflexion of the long limb at heel strike and decreased knee flexion of the short limb during heel off
increased dorsiflexion with early heel rise of the long limb at heel off and increased plantarflexion of the short limb during stance
Compensations: longer leg=more DF to shorten, shorter leg=more PF to lengthen

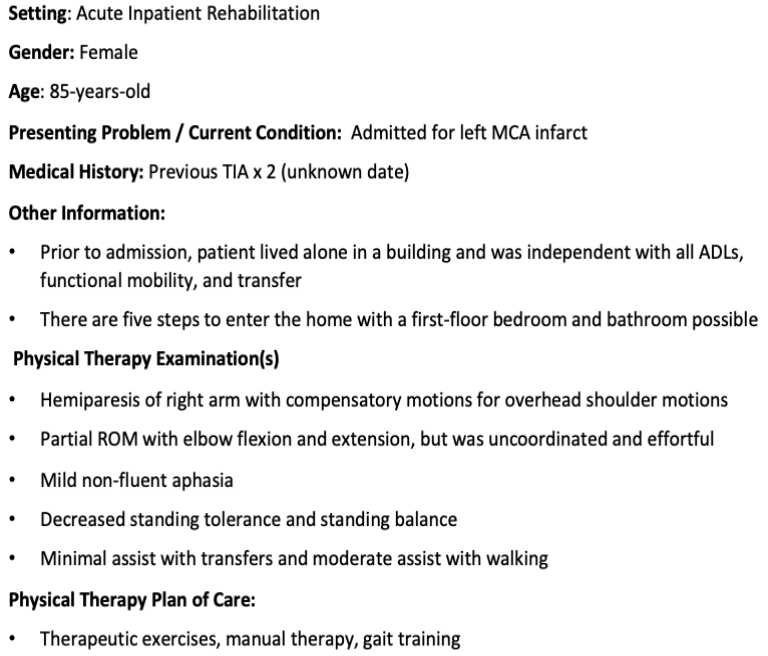
Following surgery of the R hip, a patient ambulates as shown in the picture. To improve gait pattern, functional electrical stimulation should be initiated for which of the following?
R abductors during swing on the R
R abductors during stance on the R
L abductors during stance on the L
L abductors during swing on the L
R abductors during stance on the R
Rationale: Patient is demonstrating a left side pelvic drop while walking. A left pelvic drop is caused by weak glut med muscles on the right. The function of the glut med muscle in stance is to maintain the pelvis alignment. To prevent pelvic drop and to improve the gait pattern, functional electrical stimulation (FES) should be given over the weak right hip abductors in stance