RM - Lecture 10: Airway smooth muscle control and asthma
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
- depolarisation of voltage gated calcium channel (VOC)
- Binding of contractile agonist at G-protein coupled receptor (GPCR)
Name 2 possible pathways that trigger smooth muscle contraction
1. VOC is depolarised and opens, causing a calcium influx
2. calcium binds to calmodulin and activates it
3. active calmodulin activates myosin light-chain kinase (MLCK)
4. active MLCK phosphorylates myosin light chain and activates its myosin ATPase
5. phosphorylated myosin ATPase can now facilitate cross-bridge cycling
Describe the steps that occur to produce smooth muscle contraction from depolarisation
1. Contractile agonist binds to GPCR
2. g-aplha subunit activates phospholipase C (PLC)
3. PLC cleaves phosphotidyl inositol 4,5-bisphosphate (Pt-IP2) into inositol triphosphate (IP3) and Diacylglycerol (DAG)
4. IP3 triggers release of Ca2+ from sarcoplasmic reticulum (SR)
5. DAG activates protein kinase C (PKC) which contributes to force maintenance.
6. Ca2+ from SR triggers contraction by activating calmodulin and the rest of the pathway is the same as via depolarisation
Describe the steps that occur to produce smooth muscle contraction from GPCR activation
1. Acetylcholine (ACh)
2. M3 receptor
3. M2 receptor
Fill the blanks
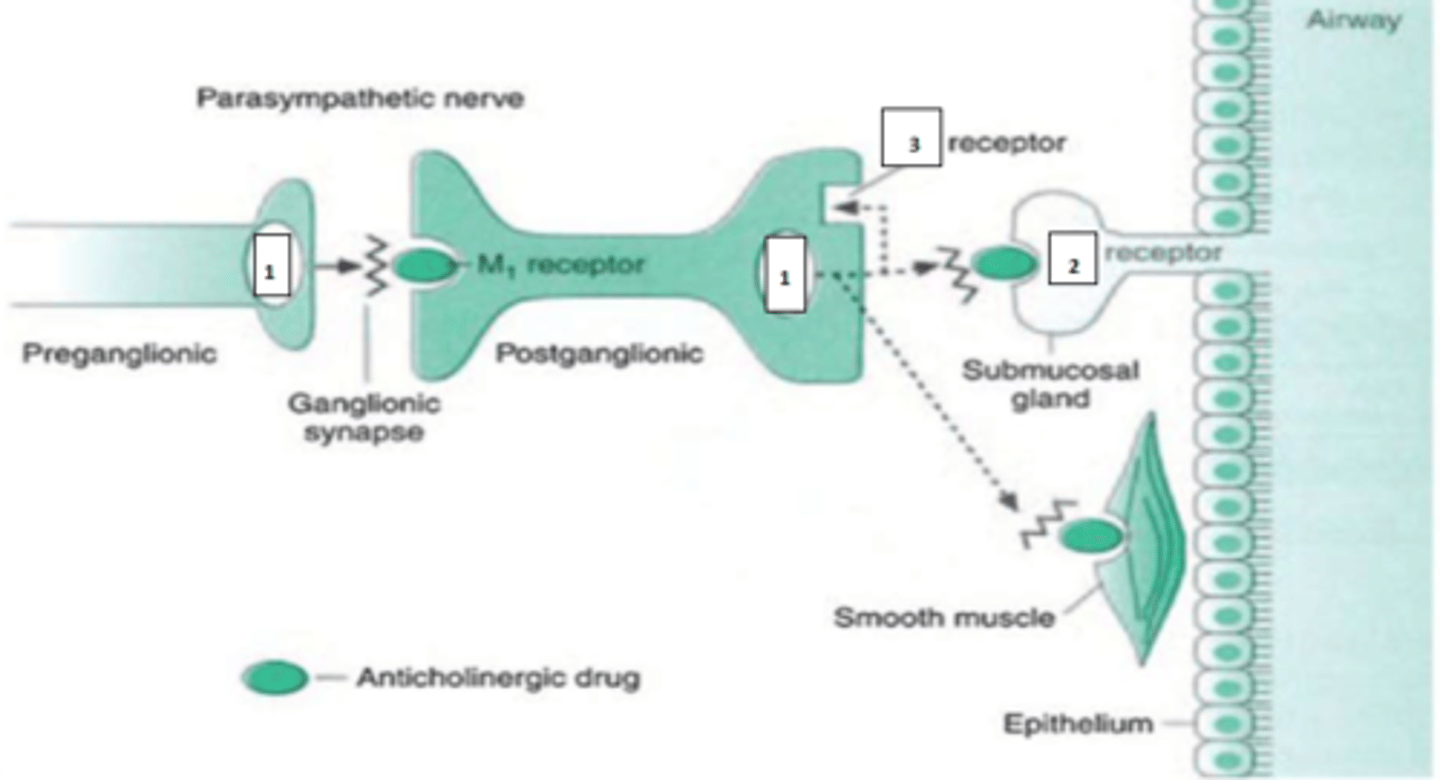
M3 muscarinic cholinergic receptors
What kind of receptor detects parasympathetic input in the airways?
Vagus CNX
Which nerve provides parasympathetic input?
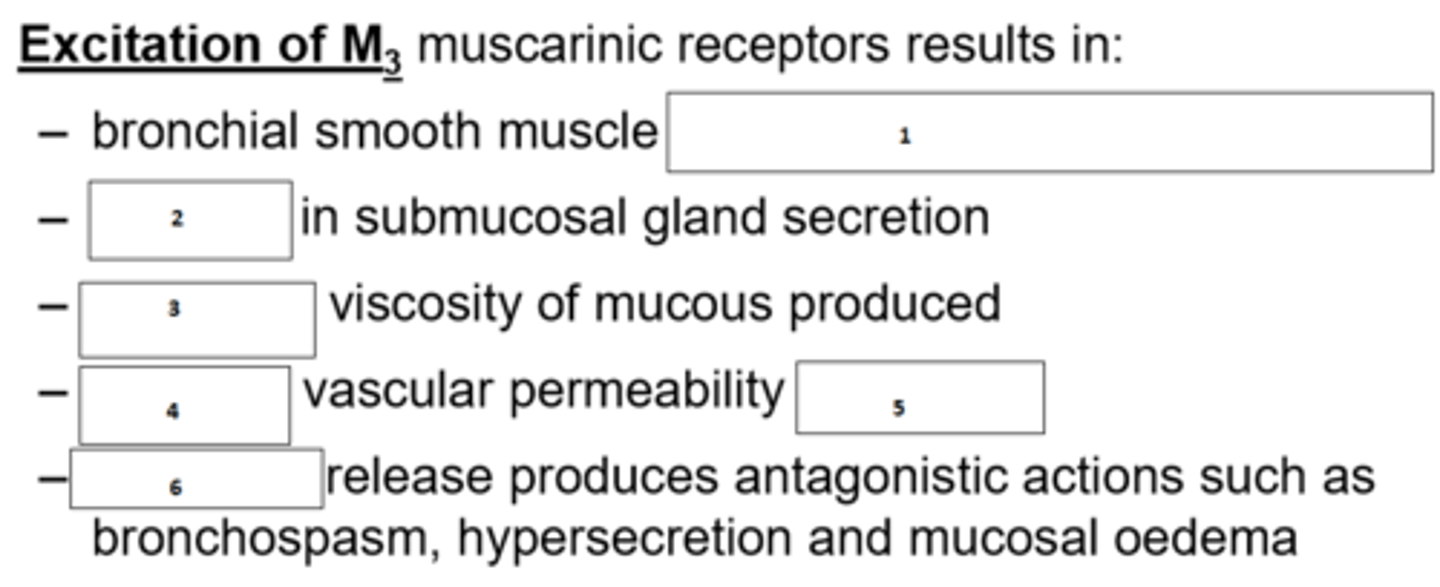
1. constriction (bronchoconstriction)
2. increase
3. increase
4. increase
5. oedema
6. histamine
Fill the blanks
- Acetylcholine (ACh)
- Leukotriene C4 (LTC4)
- LTD4
- LTE4
Which are the currently regarded most important chemical mediators of asthmatic bronchoconstriction? (4 in total)
- Parasympathetic nervous system nerves (ACh)
- Leukocytes: Mast cells, eosinophils, macrophages, neutrophils, platelets
- inflammatory cells
- epithelial cells
What are the main sources of the main mediators of asthmatic bronchoconstriction?
Beta-2 agonists are more effective. This is because even without ACh, there are mediators which can trigger airway smooth muscle (ASM) contraction and thereby bronchoconstriction. In contrast, beta agonists will definitely stimulate dilation.
Are beta-2 agonists or anticholinergics more effective for bronchodilation? Why?
Blocking contraction:
- decrease PNS activation
- block contractile mediators
- block receptors
Decreasing intracellular calcium:
- increasing cAMP
- increasing cGMP
- decreasing breakdown of cAMP and cGMP
- modulation of cell membrane ion channels
How can ASM relaxation be achieved?
Via circulation (rather than sympathetic innervation)
How do catecholamines and beta2 agonsits mainly reach ASM?
- small airways
- submucosal glands
- mast cells
Where are beta2 receptors most numerous in the lungs?
- Beta-2 agonist stimulates GPCR
- Adenylyl cyclase is activated
- AC converts ATP to cAMP
- cAMP deactivates MLCK
By which mechanism does sympathetic receptor stimulation in ASM primarily trigger bronchodilation?
1. Ca2+ activated K+ channel activation
2. phosphoinositide hydrolysis (PI: regulator of inflammatory mediators)
3. Na+/Ca2+ exchange
4. Na+/K+ exchange
5. MLCK
Fill the blanks
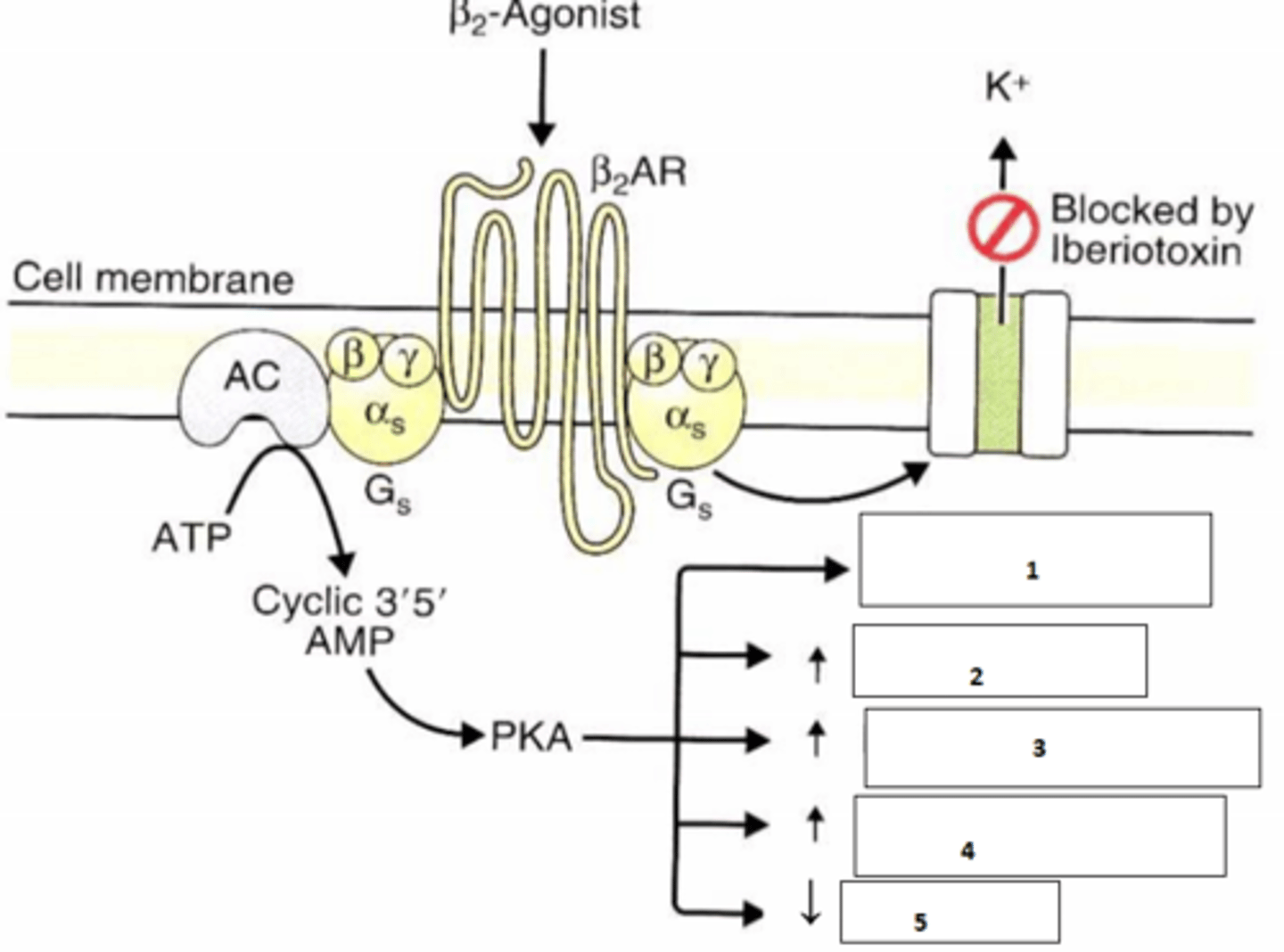
- bronchodilation
- decreased submucosal gland secretion
- decreased mast cell mediator release
What are the 3 main responses to beta-2 receptor activation?
Nonadrenergic, noncholinergic (NANC) system
Aside from SNS and PNS, what is the 3rd autonomic ASM modulation system?
Direct innervation.
Neurotransmitters:
- Nitric oxide (NO)
- Vasoactive intestinal peptide (VIP)
- ATP
- others
NO promotes ASM relaxation
NO activates a second messenger system which decreases intracellular calcium in ASM, which causes bronchodilation
How does the NANC system function? (focus on NO)
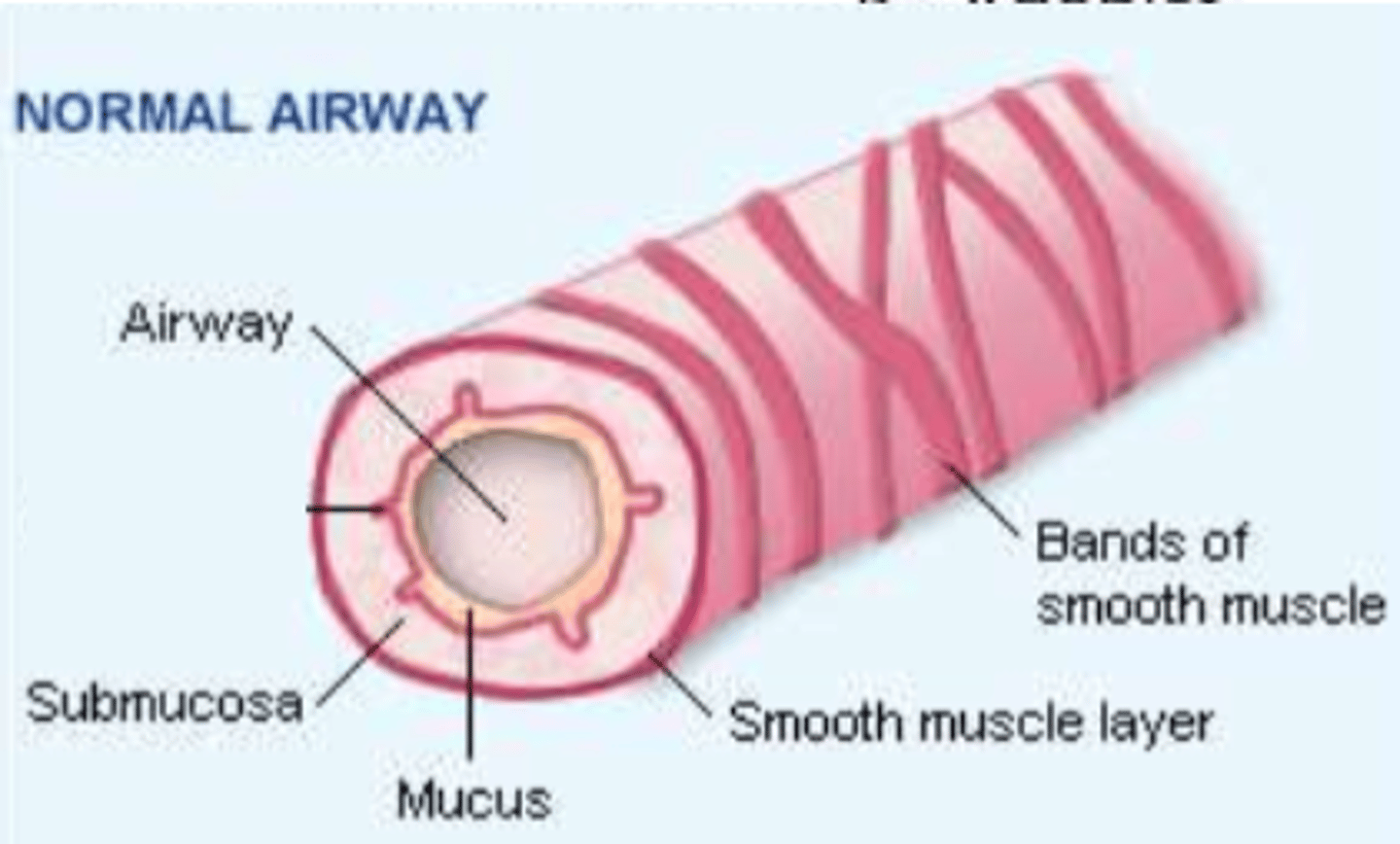
airway: narrows
submucosa: swollen
Mucus: excess production
Smooth muscle layer: thickens
Bands of smooth muscle: tighten
Describe the changes at each point in asthma
- chronic inflammatory disease of the airway
- recurrent attacks of breathlessness and wheezing
- inflammation causes airways to spasm and swell periodically and reversibly, causing obstruction
- Symptoms: coughing, dyspnoea, wheezing, chest tightness, severity varies
- chronic inflammation makes airways hypersensitive
Briefly describe the main characteristics that define asthma (pattern of onset and timing, symptomts)
1 in 10 adults and 1 in 4 or 5 children
How common is asthma?
around half (46%)
How many asthma deaths are currently thought to have been preventable?
- hypertrophied smooth muscle contracts during an attack
- mucus glands hypertrophy
- bronchial wall oedema
- infiltration of eosinophils and lymphocytes
- increase mucus production and viscosity
- mucus plugs may form (which can be coughed up)
Briefly describe the pathology of asthma
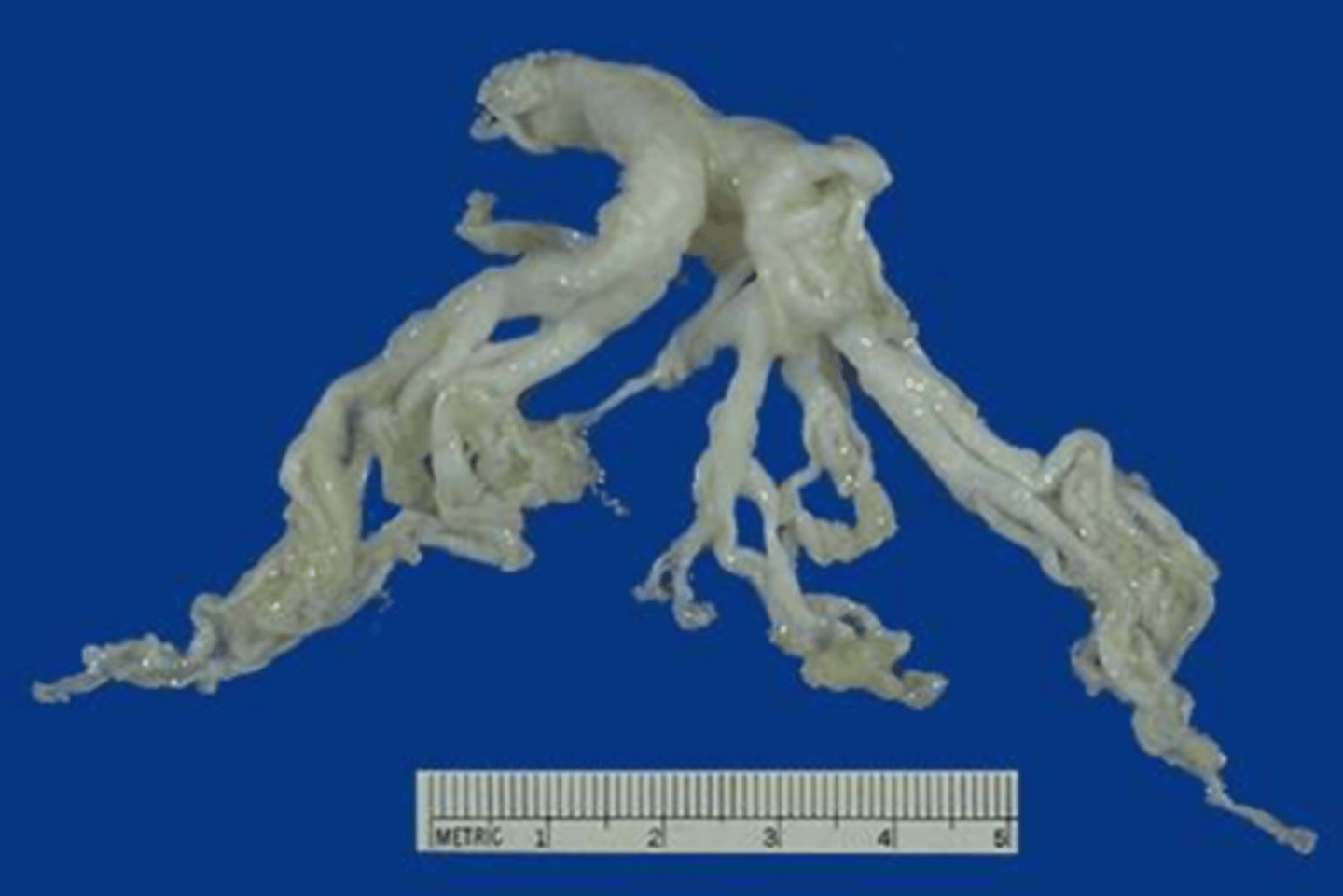
A mucus plug
What is depicted here?
This describes a severe condition where asthma attacks occur continually without breaks. This can be life-threatening
What is status asthmaticus?
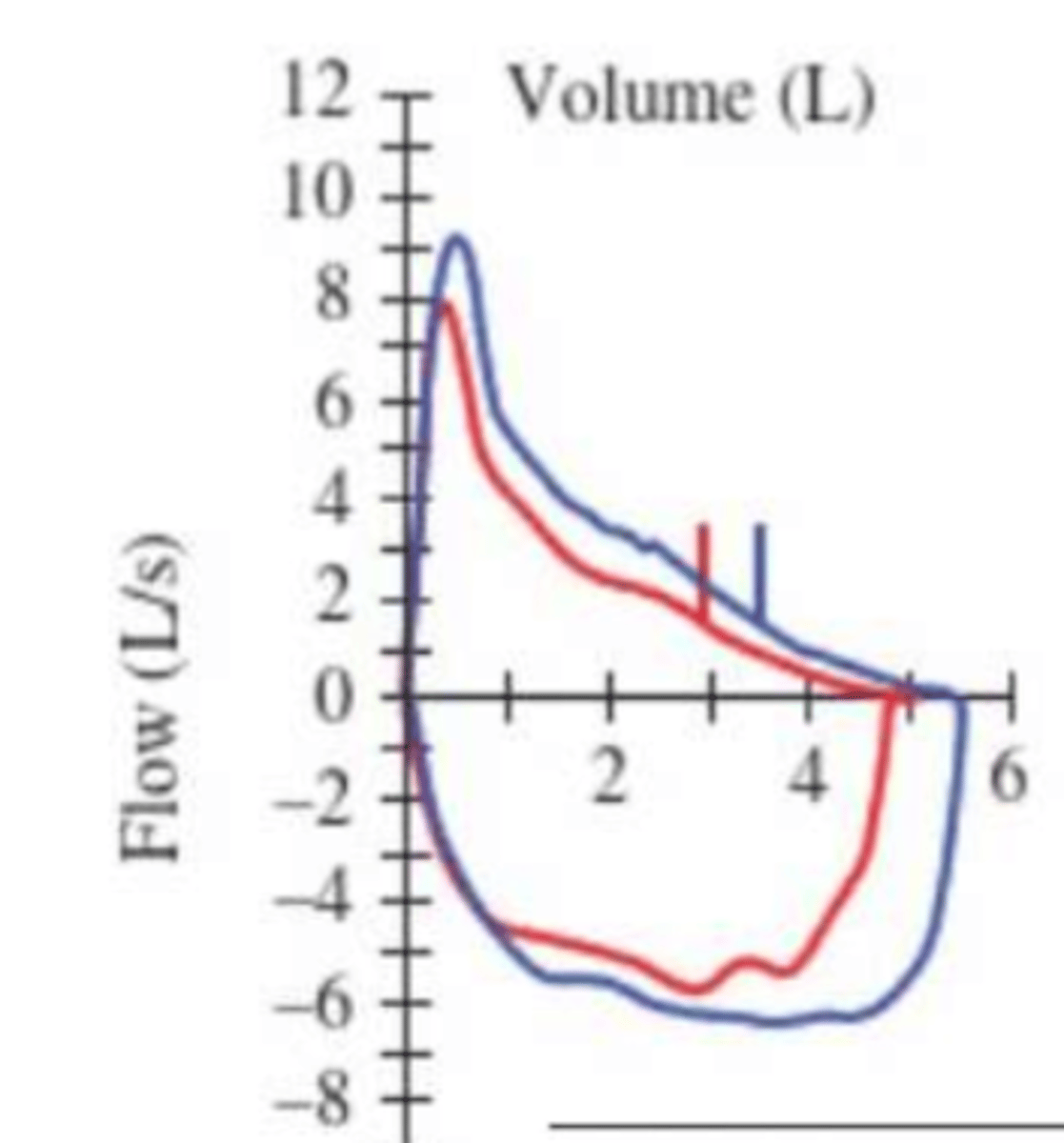
All indicators worsen. All drop except residual volume which rises
What happens to:
FEV1; FEV1/FVC, RV, PEFR
respectively during an asthma attack?
12% or greater increase and 200ml or greater increase in FEV1
What change pre and post bronchodilator administration is indicative of reversible airway obstruction and in support of asthma diagnosis?
- intrinsic
- extrinsic
Name the 2 basic types of asthma
- Atopic/allergic
- Occupational
- Exercise induced bronchoconstriction
Give 3 types of extrinsic asthma
- animal dander (flakes of skin or hair)
- dust
- pollen
- foods
What may trigger atopic asthma?
A rapid (minutes) immunological reaction triggered by combination of antigen and antibody bound to a mast cell or basophil in individuals previously sesitised to the antigen.
What is a type 1 hypersensitivity?
Initial (early) phase: vasodilation, vascular leakage, smooth muscle spasm, glandular secretions
Late phase: increased production of leukocytes which may last for days
What are the phases of type 1 hypersensitivity?
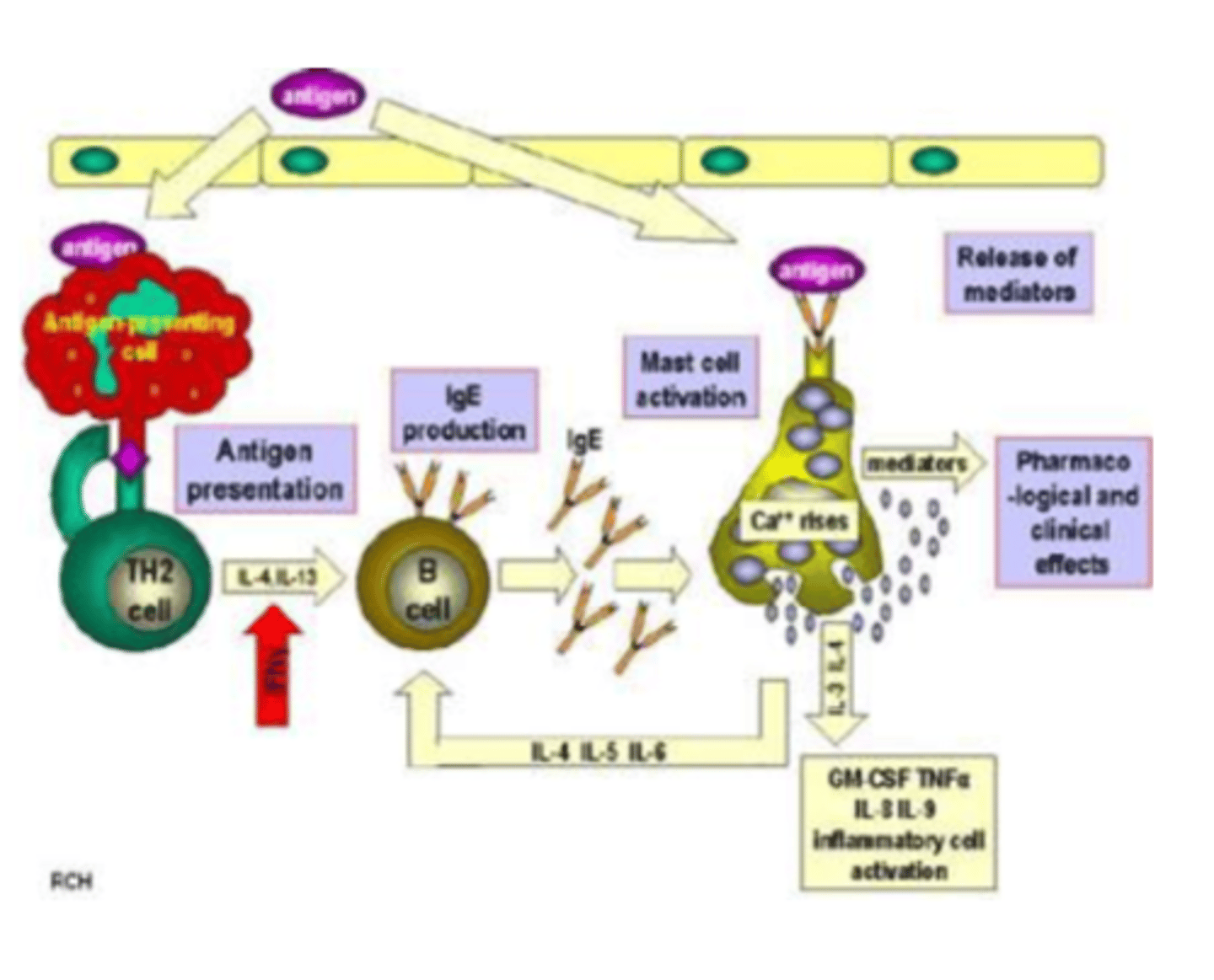
1. antigen presented to Type 2 T-helper cell
2. TH2 cells produces cytokines (particularly Interleukin 4)
3. Cytokines trigger production of IgE antibodies in B cell
4. IgE attaches to mast cell
5. Mast cells releases granules upon exposure to antigen, which releases mediators that trigger the hypersensitivity reaction
With the help of the diagram. Explain the immunological steps of immune system sensitisation and triggering of response
Atopic asthma is characterised by high levels of IgE. If this is not the case, asthma is not atopic/allergic
What is the significance of the type of antibody in asthma?
- Mast cells release chemicals via IgE binding to antigen
- mucus secretion increases
- intercellular junctions of mucosal cells open and antigen penetrates to deeper layers, where submucosal mast cells are activated
- subepithelial nerve terminals are directly stimulated, resulting in bronchoconstriction
What happens in the early phase of the type 1 hypersensitivity reaction?
-Release of mediators from more leukocytes:
mast cells, macrophages, basophils, neutrophils, eosinophils
- leukocyte recruitment
- epithelial cell injury and oedema
- decreased mucociliary function
- accumulation of mucus
- increased airway responsiveness
What happens in the late phase of the type 1 hypersensitivity reaction?
Epithelial cells release eotaxin, which triggers recruitment and activation of eosinophils
Eosinophils release major basic protein and eosinophil cationic protein which damage epithelium
Why are epithelial cells damaged in the late phase?
Eosinophilic airway inflammation is neither necessary nor diagnostic of asthma
How diagnostic is eosinophilic airway inflammation of asthma?
Not always
Are TH2 cells necessary for eosinophilic airway inflammation?
- aspirin via bronchoconstricting leukotriene production
- codeine&morphine by directly degranulating mast cells
- Mellitin (bee venom) by directly degranulating mast cells
Name 3 pharmacological agents which provoke asthma and include basic mechanism
Asthma triggered by exposure to allergens or other agents in the workplace
What is occupational asthma?
- fumes (epoxy resins, plastics)
- gases (toluene)
- chemicals (formaldehyde, penicillin products)
- Dusts (wood, cotton, platinum)
Give a few examples of occupational triggers of asthma
May vary with trigger, may be through atopic processes or direct liberation of bronchoconstrictors.
How do occupational triggers cause asthma attacks?
- Triggered by exercise/physical exertion
- symptoms only during exercise
- typical asthma symptoms: coughing, wheezing, chest tightness, and or/shortness of breath
- cold/dry air and high air flow rates
- may co-exist with atopic asthma
Describe exercise induced bronchoconstriction
- frequently triggered by respiratory tract infections
- usually no family history and IgE levels normal
- No other allergies
- viral-induced inflammation of respiratory mucosa lowers the threshold for stimulation of sub-epithelial vagal receptors (leads to bronchoconstriction)
- inhaled pollutants may contribute
Describe idiosyncratic asthma (triggers, diagnostic factors)
- Reverse/prevent bronchoconstriction with bronchodilators
- Halt inflammatory response with anti-inflammatory drugs (preventers/controllers)
What are the main 2 treatment aims in asthma?