KNPE 355
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
125 Terms
Before beginning a clinical skills task
Introduce yourself
Hand hygiene
Confirm the client’s first and last name, and ask how they would like you to address them (preferred name)
Provide an overview of the session/rationale and obtain client’s permission
SOAP Notes
Subjective
Objective
Analysis/Assessment
Plan
Analysis statement - components
client profile/summary
D.O.B., age, gender, pronouns, significant presentation
present condition/diagnosis
Current medical diagnosis or working differential diagnoses or physical
diagnosis or potential differential diagnoses and/or present condition
any risks
acuity/chronicity/stability, any risks – including clinician primary concerns,
precautions, contraindications or patient primary concerns/goals.
prognosis and rationale
what is/are the possible etiology(ies) of the diagnosis(es) and/or impairments (the ‘why?’), and what possible ramifications there may be for interventions &/or for the future
Prognosis do they have support, do they express high or low levels of self-
efficacy and/or motivation?)
potential for kinesiology or referral to other services
the likelihood that a RKIN has something to offer and that the client is likely to, or not to, benefit from KIN.
If a referral to other services is warranted (e.g., med, PT, OT, dietician etc.)
Problem list
A list of problems that are amenable to kinesiology (within the scope of practice)
Forms the basis of your treatment plan (next step)
Problems can be function, impairments, activity or participation limitations
Problems can be actual or potential (at risk for)
Relate to the underlying cause or treatable issue
Goal setting
Made in collaboration with the client
Based on:
Client’s stated goals and the problem list
Prognosis, which is based on:
Nature, acuity/chronicity of illness/injury
Prior and current level of function
Social supports, living environment, apparent motivation
• Must be client-driven/person-centered
Should be SMART
Specific
Measurable
Action-oriented
Realistic
Time-bound
Short-term goals
Steps or milestones along the way to achieving long-term goals (outcomes)
Short-term goals typically address:
Function
Impairments
Education
Can have one or more for each long-term goal
Long-term goals
Outcomes
Often linked to resolving the problem list and returning to performing a meaningful activity/role and/or optimizing health and well-being
Should be prioritized by importance
Plan
A concise statement of the overall intervention plan and follow-up proposal for next session
Body Composition
Body composition refers to the components that make up the body
Body weight and relative amounts of muscle, fat, bone and other vital tissues
Often limited to fat and lean body mass (fat-free mass) and expressed as relative (percentage) and absolute (kilograms)
Body composition is frequently used as an outcome measure to determine the effectiveness of community-based obesity prevention strategies
Body Composition Standards
Currently, universally accepted norms for body composition do not exist.
A consensus opinion for an exact percent body fat value associated with optimal health risk has yet to be defined.
However, based on skinfold percentile reference values, the “good” category for body fat values across a wide age spectrum are:
12%– 23% for males
17%–26% for females
Why do we measure body composition?
Risk of metabolic diseases
Obesity is related to health risks
Maximize performance/health
Research outcome
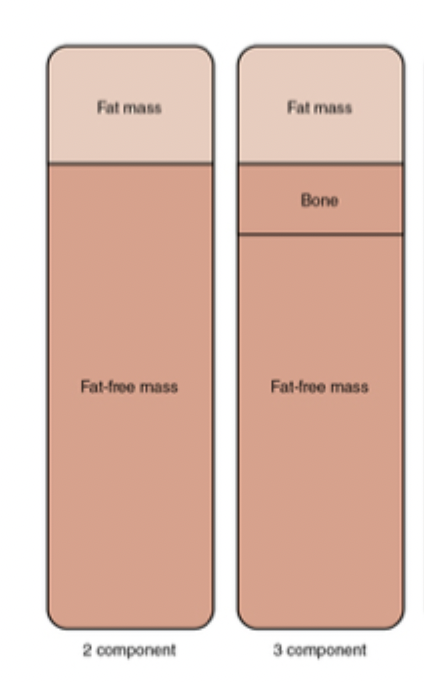
Body composition models
Two-component models
Anthropometry (circumference measures)
Skinfold thickness
Bioelectrical impedance analysis
Underwater weighing
Plethysmography (Bod Pod)
Ultrasound
Three-component models
Dual-energy x-ray absorptiometry (DEXA, DXA)
Magnetic resonance imaging (MRI)
Computed tomography (CT)
Body composition - Valid/Reliable
A body composition technique is considered valid if it measures what it says it measures (relative body fat).
A body composition technique is considered reliable if the results are reproducible.
Dual-energy x-ray absorptiometry (DEXA, DXA)
Considered the gold-standard
A 3-component model which provides an estimate of bone, fat, and lean tissue densities
Expensive equipment that is usually found in research and clinical settings
Full-body x-ray is used to evaluate various tissue densities
Underwater weighing (UWW)
Also called hydrostatic weighing or hydrodensitometry
Considered one of the most valid methods of estimating relative body fat
Densitometry - fat and lean tissues have different densities
Water density ~ 1 g • ml-1
Fat density < 1 g • ml-1 or approx. 0.9 g • ml-1
Lean tissue density = 1.1 g • ml-1
2-component model
Air-Displacement Plethysmography
Commercial name: BOD POD
Densitometry technique
Displacement of air in a sealed compartment
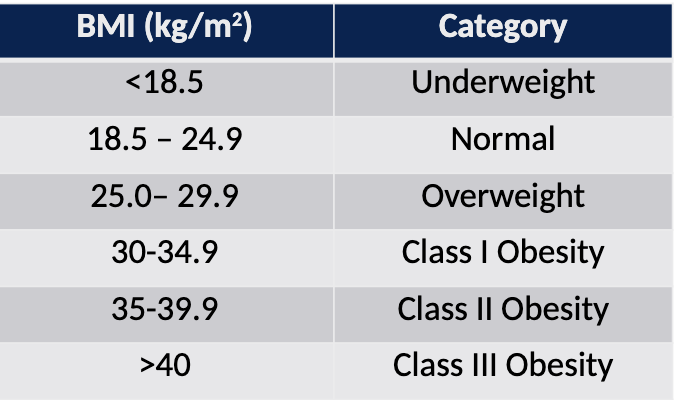
Body Mass Index (BMI)
Proxy measure for body fat.
Simple and reliable measure commonly used in clinical situations and epidemiological research.
Used to classify underweight, normal, overweight and obesity classes in adults and children.
Method:
BMI = Wt (kg) / Ht2 (m2)
BMI Strengths & Weaknesses
Strengths
Simple, inexpensive, reliable measure.
National and international standards are available.
High specificity for detecting excessive adiposity with higher BMI values in adults.
Weakness
Does not provide a direct body fat measure.
Poor estimates of body fat in some body build/frame sizes.
The American Medical Association recognizes that BMI is an "imperfect way to measure body fat in multiple groups given that it does not account for differences across race/ethnic groups, sexes, genders, and age-span
Waist Circumference (WC)
Proxy method for measuringintra-abdominal fat
Method
The WHO STEPwise Approach to Surveillance (STEPS) protocol for measuring waist circumference:
Measurement at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest
Tape should be snug around the body and parallel to the floor
Participants should stand with arms at the sides; feet positioned close together, weight evenly distributed
Measure at the end of normal respiration
Relaxed position
Waist Circumference Strengths & Weaknesses
Strengths
WC is closely linked to increased risk for chronic disease in both adults and children.
It may provide a better indicator of chronic disease risk than BMI, especially in individuals with normal BMI values.
Weakness
Does not directly measure intra-abdominal fat
The practitioner must be trained
2 measures need to be taken and averaged
Skinfold thickness
Estimation of body fat
Most widely used field technique
Rationale = age-dependent proportion of body fat is deposited subcutaneously
The amount of adipose tissue that can be pinched provides some indication of the amount of overall body fat
Estimation of percent body fat from skinfold measures has an error of approx. 3.5%
Skinfold thickness - Method
Using skinfold calipers, all measurements are taken on the right side of the body
Carefully landmark and measure skinfold sites
Generalized body density formulas using 3-7 measurement sites
Body composition is estimated from the Siri equation:
%body fat = (4.95 / density) – 4.50
Skinfold Thickness Strengths & Weaknesses
Strengths
Relatively easy measurement with minimal equipment
The relationship between subcutaneous fat and total body fat varies with race, age and sex. Therefore, population-specific equations have been developed.
Weakness
Calipers vary in quality, and some can be grossly inaccurate
Intra and inter-rater reliability
Not recommended for people with BMI > 30kg/m2
Factors that may contribute to skinfold thickness measurement errors
poor anatomical landmark identification
poor measurement technique
inexperienced evaluator
extremely obese or extremely lean participant
improperly calibrated caliper
Bioelectrical impedance analysis
Estimates fat-free mass and total body water.
Based on the body’s ability to conduct a mild electrical current to indirectly estimate fat-free mass or % body fat.
Impedance: opposition to the flow of current , where electrolytes in body water conduct electrical current
Measured with BIA analyzer
Greater total body water current passes more easily through the body
Fat tissue has lower water content than fat-free mass Impedance is greater in individuals with more body fat.
• SEE = 2.7 to 6.3%
Bioelectrical impedance analysis - Strengths & Weaknesses
Strengths
Validated equation available for adults and children
Standard error estimates available for BIA published equation
Weakness
Equations less valid for identifying adiposity in individuals with high or low BMI values
Accuracy depends on following standardized procedures (normal hydration, fasting, and avoiding exercise
What are vital signs?
Measures of the body’s core ability to stay alive
pumping blood through the heart
breathing
maintaining a core temperature
Vital signs are the most frequently measured objective data for monitoring vital body functions and are often the first and most important indicator that the patient’s condition is changing
Four vital signs are internationally recognized and accepted in medicine:
Respiration (ventilation)
Pulse or heart rate (HR)
Blood pressure (BP)
Temperature
Three other signs may be considered:
Pulse oximetry
Pain rating scales
Level of perceived exertion
Vital signs are used to establish:
Baseline physiological information to guide exercise program development
Physiological response to activity to guide continuation, modification, or discontinuation of an exercise program
Patient’s/client’s immediate health risk (physiological risks, contraindication, and/or improvements)
Emergency cardiac or respiratory interventions
What’s the point of measuring Heart Rate (HR)?
Goal = to determine the client’s physiological response to activity
To obtain an accurate picture of a client’s cardiac response to an activity, we typically assess:
Resting HR (5 minutes before activity)
Activity HR (during or immediately following activity)
Recovery HR (1 to 5 minutes post-activity)
What is Heart Rate (HR) and what’s documented?
Heart rate (pulse) is an indirect measure of the rate and rhythm of the contraction of the left ventricle.
Three characteristics are documented:
Rate (bpm)
Rhythm
Intensity
How to measure Heart Rate (HR)
Count begins with the first beat that occurs after the time interval has begun (“one count method”)
HR is a measurement of beats per minute therefore, you should count for one full minute
Once you have established a baseline pulse rate (and it is regular and strong) you can use the 30 seconds x 2 method
Measuring HR – carotid pulse
Caution, if you decide to assess the carotid
pulse:
Stand on the same side of the carotid artery you are assessing (never reach across)
Do not press too hard
Carotid sinus reflex = massage-like actions can decrease HR and produce bradycardia
Never palpate bilateral carotid arteries, this can potentially cut off blood supply to the brain
Measuring HR – radial and brachial pulse
Support the left arm on a stable surface or with your arm at the level of their heart with their elbow extended and forearm supinated
Using your 2nd and 3rd digits, palpate gently for the:
brachial pulse: medially on the elbow crease
radial pulse: 1-2 cm above the wrist crease, lateral to the flexor tendons
Measure the number of beats in 1 minute
Record your findings in beats per minute (bpm)
Safety – Heart rate and exercise
HR increases with progressive workloads at a rate of approx. 10 bpm per 1 metabolic equivalent of a task (MET)
HR should decrease by at least 12 beats during the first minute of recovery.
HR should decrease by 22 beats by the end of the second minute of recovery.
Respiratory Rate (RR)
It’s actually ventilation that we measure, the movement of airflow. Ventilation is characterized in 4 main ways:
Rate: # breaths per minute (bpm)
Pattern
eupnea: a ventilatory rate within normal limits (~12 breaths per min)
tachypnea: an elevated ventilatory rate
bradypnea: a low ventilatory rate
apnea: absence of ventilations
Mechanics
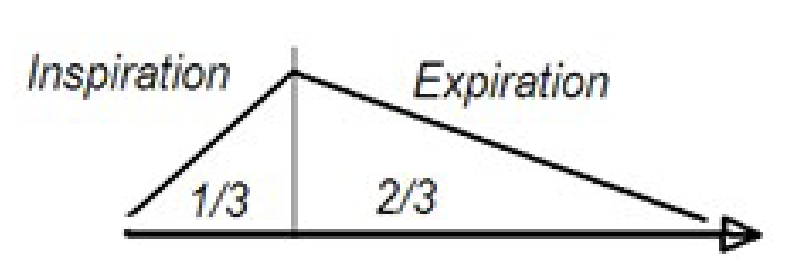
RR – Mechanics
Inspiratory to Expiratory Ratio (I : E ratio)
Ratio of time for inspiration versus expiration
Normal is 1:2 or 1:3
In obstructive disease, the expiratory time is increased because the patient has increased expiratory resistance, and it takes longer to empty the lungs before the next breath.
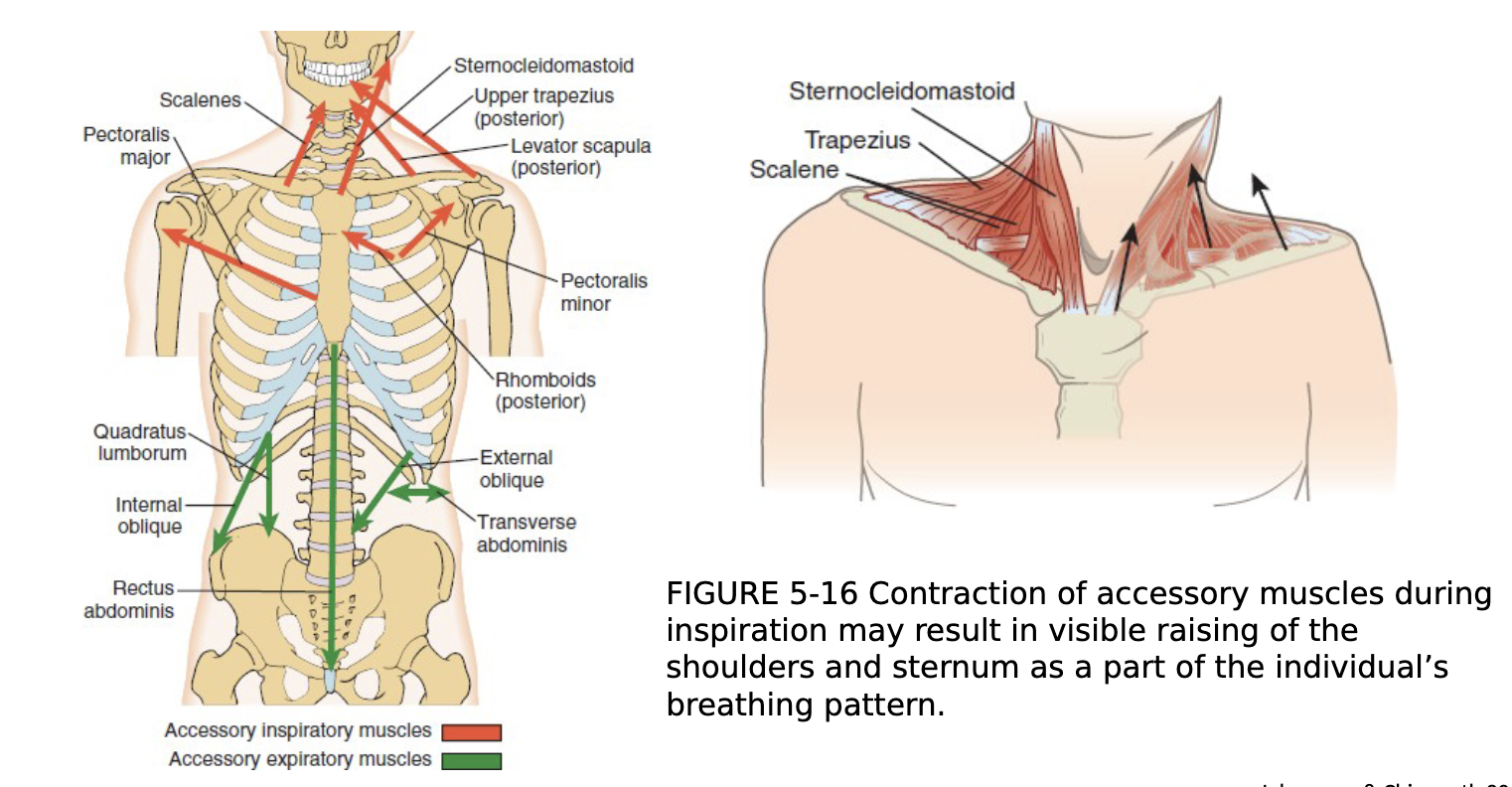
RR mechanics – accessory muscles
Blood Pressure (BP)
Blood pressure is a physiological variable which reflects the effects of cardiac output, peripheral vascular resistance and haemodynamic factors.
Use of a blood pressure cuff is an indirect measure of the pressure inside an artery caused by blood flow through the artery.
BP is recorded as millimeters of mercury (mmHg).
Systolic Pressure: the pressure at the time of contraction of the left ventricle.
Diastolic Pressure: the pressure at the time of ventricular filling (‘resting’ pressure).
Blood Pressure - equipment
Clean equipment before using and ensure it is fitted to your client
Check stethoscope is situated correctly

Blood Pressure Measurement
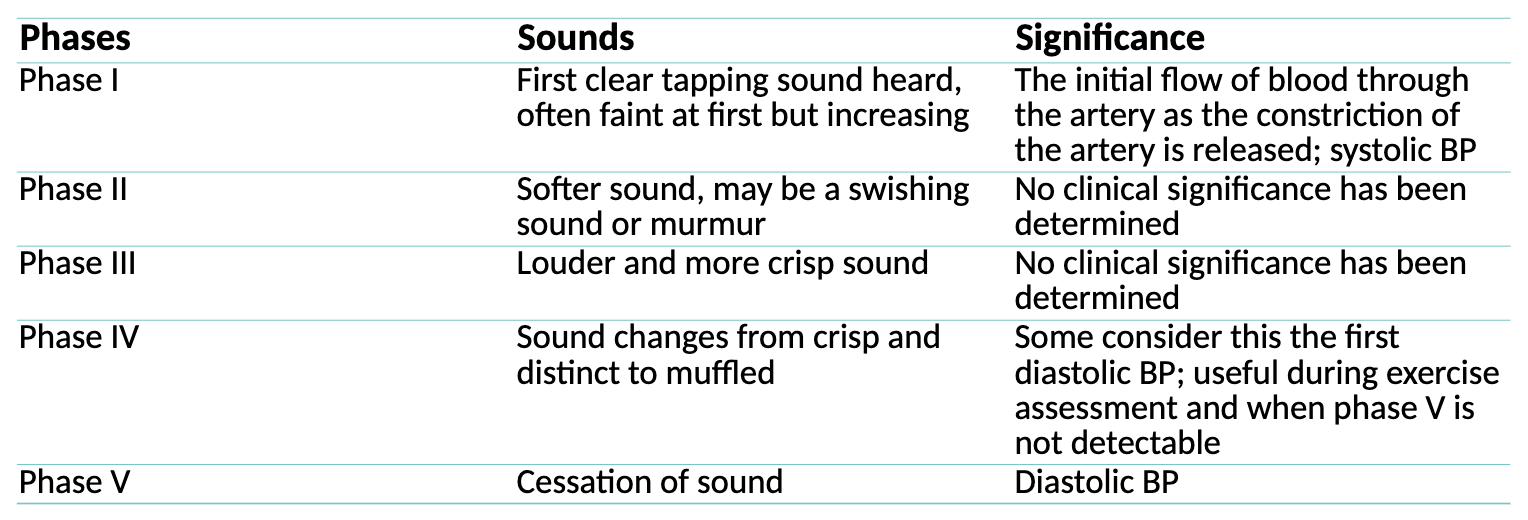
Korotkoff’s Sounds: assessment of blood pressure by auscultation, using a sphygmomanometer and a stethoscope:
the systolic pressure is indicated by the first faint clear tapping sounds heard upon gradually releasing the air in the cuff
the diastolic pressure is indicated by the disappearance of all sounds (last sound heard).
Safety – Blood pressure
SBP increases with increasing workloads at a rate of approx. 10 mm Hg per 1 MET
Normally no change in DBP or a slight decrease during exercise.
Post-exercise SBP returns to pre-exercise levels or lower by 6 minutes of recovery
Blood Pressure Emergencies
BP changes during exercise or other high-level activity serve as serious warnings.
These warning signs include the following:
Systolic reading greater than 250 mm Hg
Diastolic reading greater than 115 mm Hg
A drop in the systolic pressure of more than 10 mm Hg from baseline
Failure of the systolic pressure to increase with the increasing workload
STOP! Any one of these BP findings should result in immediate cessation of activity.
Blood Pressure sounds heard can be broken down into five phases
Oxygen Saturation
Percent saturation of arterial oxygen (SpO2) = estimate of how much oxygen is travelling through your body in your red blood cells
95% - 100%
Pulse oximeter
Exercise-induced hypoxemia = decrease in SpO2 greater than or equal to 5% during exercise
Cardiorespiratory fitness
Total body health: reflects the ability of our heart, blood vessels, lungs, and muscles to use and transport oxygen to do physical work (exercise, move, daily activities of living)
Benefits of improving CRF
Reduced risk of:
Developing dementia and Alzheimer disease
Adverse health outcomes such as developing prediabetes, metabolic syndrome, and type II diabetes
Developing cardiovascular disease
Developing breast cancer, lung cancer, and cancers of the gastrointestinal system
Disability later in life
Maximal Oxygen Uptake - What is VO2max?
VO2max is the measurement of the maximum (max) rate of volume (V) of oxygen (O2) your body can use during exercise.
An individual’s VHO2max is determined by measuring gas exchange during intense physical exercise.
The VHO2max test involves incrementally increasing exercise intensity (work rate) to ensure maximal aerobic energy transfer.
How do we measure VO2max?
The four different ways of measuring CRF are:
Cardiopulmonary exercise tests (CPET)
Maximal Exercise Test (GXT)
Submaximal Exercise Test
Estimated CRF (eCRF)
Submaximal exercise testing
Measures VO2 max indirectly through predictive equations based on the HR –workload relationship
Not as accurate as VO2max prediction from max tests
Uses submaximal work rates (i.e., less than 85% HR max)
Limited diagnostic capabilities
More accessible in the community or clinical setting:
easier to administer
less expensive
safer(?)
Factors can increase your heart rate during submaximal exercise testing
Caffeine: Drinking caffeine within 3 hours of completing your test can increase your heart rate at rest and during activity
After eating a meal: After eating a meal, your heart rate will increase. Your heart needs to pump additional blood to the stomach to aid digestion. After eating and digesting food, your heart rate should return to normal
Feeling anxious: Any form of emotional stress can increase your heart rate.
Smoking: Smoking damages the cardiovascular system and can affect the heart by increasing blood pressure, narrowing the arteries, and increasing heart rate.
Humid weather/environment: High temperatures and high humidity result in more blood flow to the skin as the body attempts to cool itself off. This can cause the heart to beat faster while circulating twice as much blood per minute than on a normal day.
Disadvantages to be aware of when using submaximal exercise testing
For some people, this type of test could be a maximal test.
The Individual’s motivation and pacing strategy during the test can have a profound effect on the final outcome,
Does not allow comprehensive monitoring of both HR and BP during the test.
Relatively large standard error of the estimate (SEE) ± 10% - 15%
Field tests (submaximal exercise tests) are generally not recommended for sedentary individuals who have been identified in pretesting screening to be at moderate or high risk of cardiorespiratory or musculoskeletal complications
We must consider the ___ and ___ effects of testing – especially when using submaximal exercise testing
Ceiling effect: the test is too easy to produce sufficient CV response to get an accurate functional capacity (e.g., not enough stages or peak intensity).
Floor effect: the test is too difficult (from a vascular or physical perspective) so that the test is not limited by the cardiovascular system but by other barriers (e.g., anxiety, peripheral claudication, Aimexercise specificity (e.g., LE muscle fatigue during cycle ergometry testing or in UE muscles during arm ergometery testing, osteoarthritis)
Submaximal exercise testing: Aim & Objective measures collected
Aim: to determine the HR response to one or more submaximal work rates and use the results to predict VO2max
Objective measures collected:
HR
BP
Workload
RPE
SpO2
Symptoms
Results of exercise testing: Exercise Prescription
Information to develop an individualized aerobic exercise prescription based on:
Peak HR during exercise (and how that relates to the predicted HR max for age and sex)
BP responses to exercise
VO2max
Functional capacity as a calculated estimate of maximal oxygen uptake in Metabolic Equivalents of Task (METs)
Results of exercise testing: Other
Educating clients about their present fitness status relative to age and sex- matched norms
Collecting baseline and follow-up data to evaluate progress
Motivating patients by establishing reasonable and attainable exercise goals
Providing information to inform return-to-work (RTW) decisions
Disability/mobility assessment
How do we obtain the most accurate estimate of VO2max?
A steady state HR is obtained for each exercise work rate
A linear relationship exists between HR and work rate
The difference between actual and predicted maximal HR is minimal
Mechanical efficiency (i.e., VO2 at a given work rate) is the same for everyone
The client is not on any HR altering medications
The client is not consuming high quantities of caffeine, is ill or in a high-temperature environment
Pretest procedure - Submaximal exercise testing
Review the client’s medical history, exercise clearance, reasons for the chosen test, recent symptoms (if any) and current medications
Explain the test/procedure to the client
Inform the client that the test may make them feel uncomfortable and that they should let you know if they feel any symptoms, including:
Chest discomfort
Dyspnea
Claudication
Rockport Fitness walking test (one-mile track walk test)
Developed for a wide age range (30-79 years) of males and females
Prediction equations developed using sex, age, weight, time and HR
Rockport Fitness walking test - Pros & Cons
Advantages
Applicable to a wide range of individuals
Limited equipment needed
Familiar activity
Disadvantages
Inability to monitor physiological variables during test
20-meter shuttle test (Beep test)
Multi-stage shuttle run test used to estimate VO2max and maximal aerobic speed
20-meter shuttle test - Pros & Cons
Advantages
Multiple stages allows for a wide range of fitness levels to be tested
Limited amount of equipment needed
More than one participant can be tested at once
Paces individuals with pre-recorded sound signals
Disadvantages
Frequent stopping and starting
Pacing
Inability to monitor physiological variables during test
How do we ensure this is a submaximal test?
6-minute walk test
The 6MWT has been primarily used to assess individuals with chronic obstructive pulmonary disease and heart failure and healthy older and elderly populations.
Widely considered a measure of functional status that represents the capacity to carry out ambulatory activities of daily living.
Standardized protocol
May be max for low fitness/severe disease, yet it can produce a ceiling effect for others
< 300 m = poor short-term survival
6-minute walk test - Pros & Cons
Advantages
Simple, inexpensive test
Corresponds to a functional activity of daily living
It can be used with a wide population with a variety of diagnoses
Standard time rather than a predetermined distance may provide a better test of endurance
Allows participants to set their own pace and stop if necessary
Disadvantages
Requires 2 practice tests
Inability to monitor BP during test
Single Stage Submaximal Treadmill Walking Test (SSTWT) - Pros & Cons
Advantages
Suitable for people with various diagnoses
Familiar activity
Single stage
Disadvantages
Based on HR therefore, factors that affect HR must be controlled
Astrand-Rhyming Cycle Ergometry Test - Pros & Cons
Advantages
Set pedal rate (50rpm) and predetermined workload
Short test
Disadvantages
Underestimates VO2 for men
Overestimates VO2 for women
May be limited by LE discomfort rather than CV status
Selecting the appropriate test
Inappropriate test selection can lead to under-stressing or overstressing the client.
The goal of the test should be to produce a sufficient level of exercise stress without physiologic or biomechanical strain.
Things to consider when selecting the appropriate test
Has the test been validated in this population?
Effect of a person’s condition on daily function and abilities
Cognitive status
Age
Weight
Mobility, use of orthotics or prosthetics, balance, gait
Current level of pain
Client’s goals
Muscular Strength
The largest force that a muscle or group of muscles can generate during a single contraction.
Muscular strength is recognized as a marker of cardiometabolic risk and is associated with morbidity in young and older adults
E.g. Lifting groceries
Muscular Endurance
The muscle’s ability to continue performing successive exertions or repetitions against a submaximal load.
Climbing stairs
Carrying groceries from the car to our fridge
Muscular Power
The muscle’s ability to exert force per unit of time (i.e., rate). Muscle power output is a product of the force and the velocity of muscle shortening.
Functional independence
Low hand grip strength is associated with:
Sarcopenia
Functional limitations and disabilities
Higher levels of handgrip strength associated with:
30% lower risk of all-cause mortality in men, 40% lower risk in women
Decreased lower extremity strength is associated with:
Ability to perform ADLs
Risk of hospitalization
Higher levels of lower body strength (knee extension) associated with:
14% lower risk of all-cause mortality
Why do we assess muscular fitness?
Provide information about our baseline physical fitness to show change over time
Identify weaknesses in certain muscle groups
Serve as a basis for designing individualized exercise training programs.
To monitor progress and improvements over time
How to evaluate total -body muscular strength or endurance
No single assessment evaluates total-body muscular strength or endurance
Musculoskeletal fitness testing is specific to:
The muscle groups tested
the velocity of the movement
the type of contraction
the ROM used
the type of equipment used to perform the assessment
Before beginning your assessments
Familiarize the client with the test procedure.
Familiarize the client with the equipment.
Warm-up
5–10 min of light-intensity aerobic exercise (i.e., treadmill or bike)
dynamic stretching
several light-intensity repetitions of the specific testing exercise.
Standardized conditions for muscular fitness
assessments
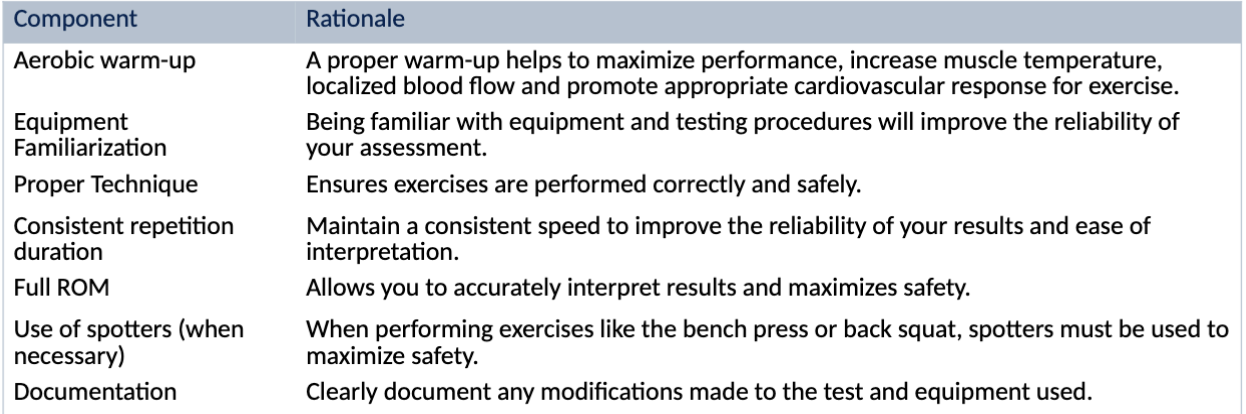
Principles of muscular fitness testing
Informed consent
Ensure general demographics have been collected (see lab worksheet)
An aerobic warm-up (5-10 minutes)
Equipment familiarization
Education/cueing on optimal posture/positioning for each test
Consistent repetition duration (movement speed) when appropriate
Full range of motion (ROM) should be used/achieved
Use of spotters (when necessary)
1-repetition maximum (1RM)
The 1RM test is considered the standard when evaluating dynamic muscular strength.
requires the client to exert maximal force dynamically through a ROM in a controlled manner with the proper technique.
Respect the rest time
Muscular fitness testing - Sources of Error
Client Factors
Control for the effects of learning on performance
Encourage clients to achieve their maximal effort
Allow for adequate rest between trials
Equipment
Equipment needs to be calibrated regularly
Technician Skill
Correct any performance errors you see
Environmental Factors
Room temperature and humidity
Distractions
Pre and post-test should be at the same time of day
Flexibility
the ability of joints to move through their full range of motion.
Static flexibility
The ability to hold an extended position at one end or point in a joint’s range of motion
Dynamic flexibility
The ability to move a joint through its range of motion with little resistance.
Balance
the ability to control the centre of mass in relationship to the base of support
Static balance
the ability to maintain the centre of gravity within the supporting base while standing or sitting
E.g., quiet standing
Dynamic balance
the ability to maintain an upright position while the centre of gravity and base of support are moving, and the centre of gravity is moving outside of the supporting base
E.g., walking, playing sports
Reactive balance
the ability to compensate and recover from perturbations while standing or walking
Functional balance
the ability to perform daily movement tasks requiring balance.
Senior’s Falls in Canada
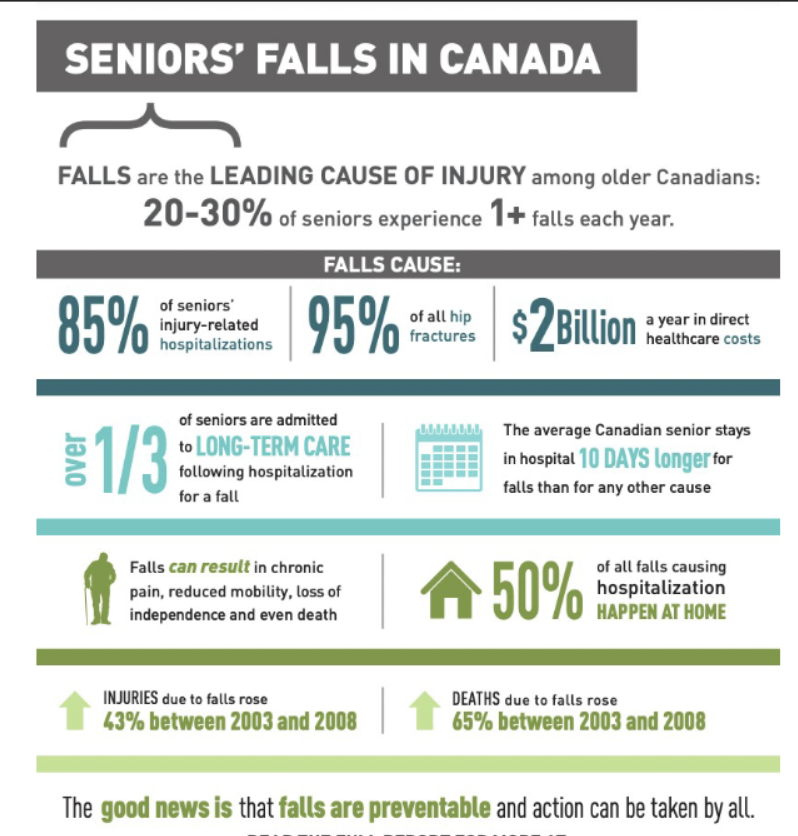
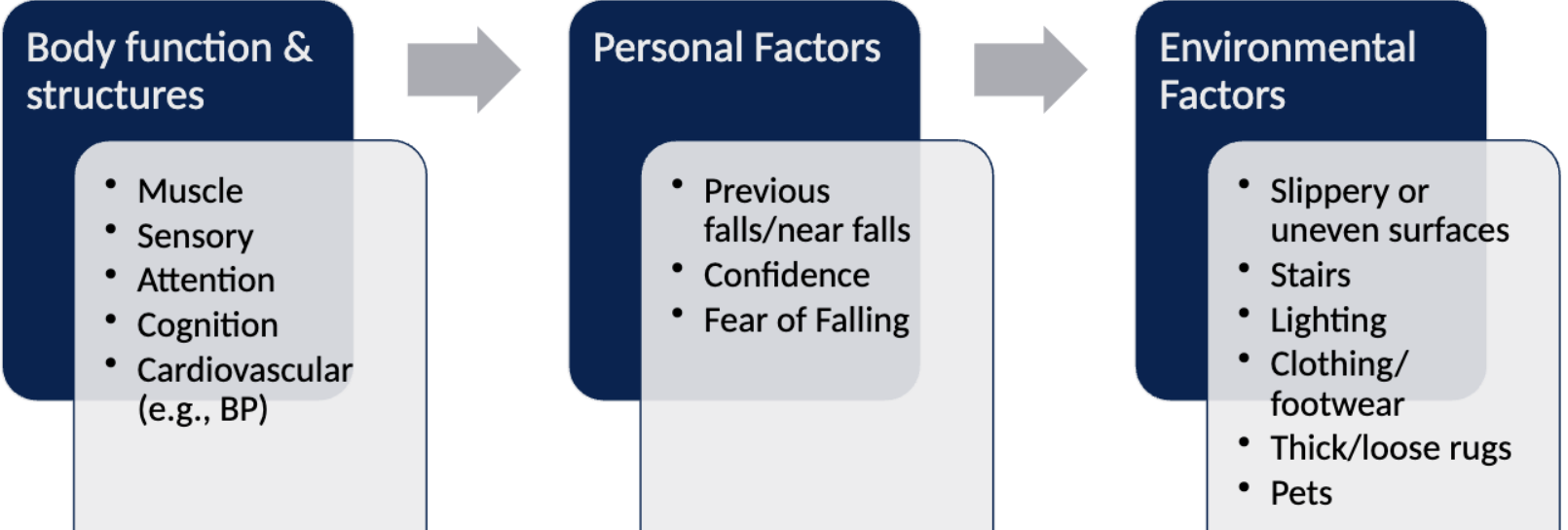
What factors contribute to the risk of falls?
How do we assess balance - Direct and indirect methods
Direct measures
Force plates
Indirect measures
Field and clinical tests (outcome measures)
General screen
One-legged stance test
BBS
Y-balance
How do we assess balance - Static and dynamic
Static balance
Standing eyes open and closed
Decrease BOS
Feet together, tandem stance, unipedal stance
Dynamic balance
Rotating, bending, turning 360 degrees, alternate stepping etc.
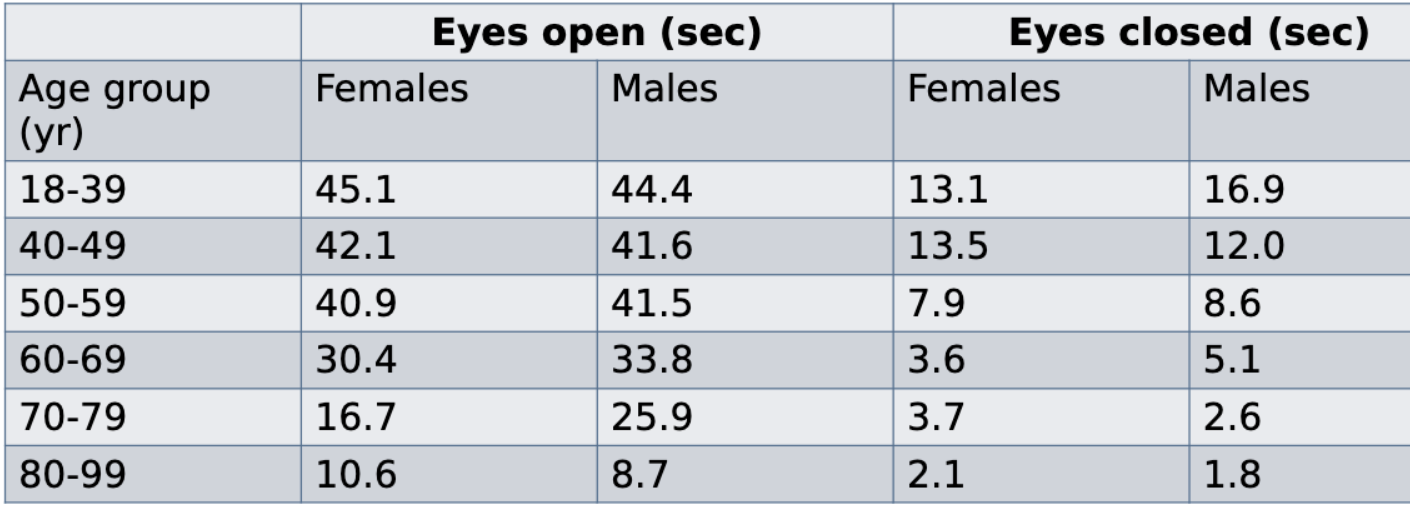
Unipedal (One-leg) Stance Test
Simple assessment of static balance
Not a standardized test, many variations exist
Age-sex norms for the one-leg stance test
Berg Balance Scale
14-item objective measure that assesses static balance and fall risk in older adults
Used in many clinical populations including:
Older adults, Stroke, Spinal injuries, Pulmonary diseases, Parkinson’s disease, Osteoarthritis, Alzheimer's
Standardized test, gait aids can not be used during test
5-point ordinal scale (0-4)
Maximum score = 56
Berg Balance Scale - Fall risk
≤40 is associated with almost a 100% risk of falling.
< 45 on BBS indicates an individual may be at increased risk of falls and may benefit from a walker or other walking aid.
≤50 indicates the individual is more likely to fall and should be assessed further for fall risk.
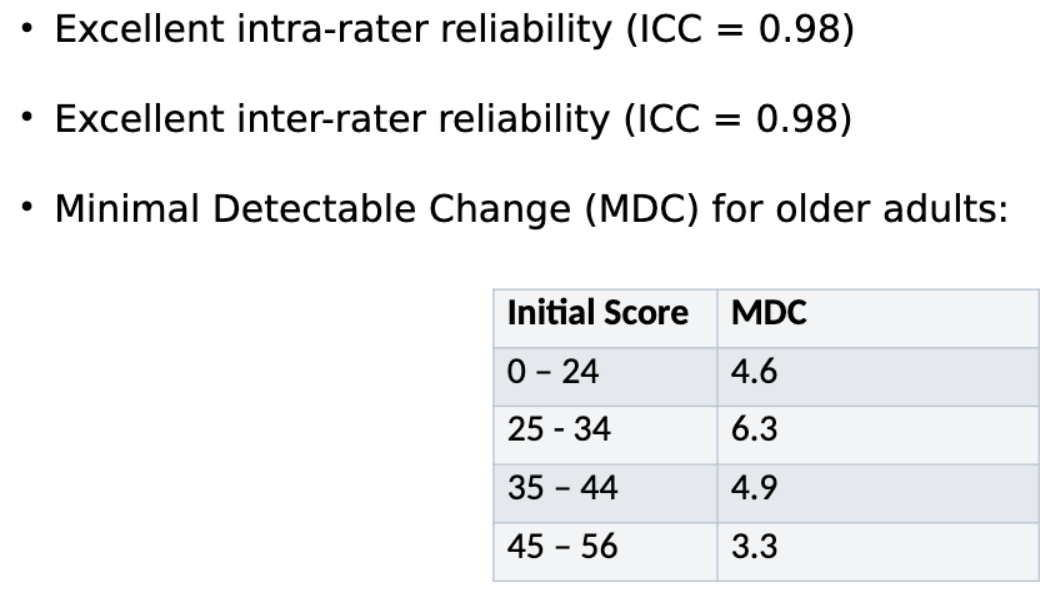
Berg Balance Scale - ?