1.03 Medical Sciences
1/382
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
383 Terms
what is one unit of alcohol?
8 grams/10ml
how do you calculate alcohol units?
alcohol percentage (ABV) x volume (ml) / 1000
what are the NHS recommended limits of alcohol consumption?
no more than 14 units per week (but spread out over at least 3 days)
how can alcohol enter the body?
- Ingestion
(slowly absorbed from the stomach & quickly absorbed from small intestine)
- nasal passage
- lungs
- skin
- other epithelia
how many calories per gram in ethanol?
7 calories per gram
is ethanol water soluble?
no, so it does not enter fat
what can affect the uptake of ethanol?
- size and body build (women have a higher relative fat percentage and lower water content = higher concentration in blood)
- the alcohol type and concentration
- faster uptake with carbonated alcohol
- greater effect with an empty stomach
- uptake increased by drugs that enhance gastric emptying and drugs that inhibit gastric alcohol dehydrogenase
- delayed by food (especially carbohydrates)
- caffeine counters alcohols soporific (sleeping) effects
how is alcohol distributed in the body?
- throughout the water in the body
- most tissues are exposed to same conc of alcohol in the blood
- exposure for the liver is greater because blood is received directly from the small intestine via the hepatic portal vein
how quickly does alcohol diffuse?
fairly slowly into the tissues, except from organs with a rich blood supply e.g. brain and lungs
what are the short-term physiological effects of alcohol?
mouth - slurred/confused speech
stomach + oesophagus - nausea, vomiting, heartburn gastritis
intestines - diarrhoea
pancreas + sugar digestion - pancreatitis + hyperglycaemia
kidney + fluid balance - dehydration + depleted salts + minerals
heart + blood pressure - tachycardia, arrythmias and increases in blood pressure
brain + nervous system - impaired concentration, memory loss, coma
- sweating, flushing and bruising
- body is at increased risk of rapid heat loss and hypothermia
what are the long-term effects of alcohol? (7)
mouth - cancer of mouth, larynx, throat
oesophagus - cancer
stomach - chronic gastritis
intestines - bowel cancer
liver - cancer, alcoholic liver disease
pancreas + sugar digestion - acute and chronic pancreatitis
heart + blood pressure - coronary heart disease, hypertension, heart failure due to cardiomyopathy
blood + immune system - anaemia, hepatitis C, TB, infections
lungs - pneumonia
brain + nervous system - brain damage (Wernicke's, Korsakoff, nerve damage, epilepsy, sleep disturbances, stroke
mental health - addiction/dependence, mood disorders, withdrawal symptoms
what is Wernicke's encephalopathy?
- from chronic excessive alcohol consumption
- leads to thiamine (vitamin B1) deficiency
- causes brain tissue ischaemia + death
what are the signs of Wernicke's encephalopathy? (3)
- acute confusion
- opthalmoplegia
- ataxia
what is opthalmoplegia?
paralysis of the extraocular muscles
how do you treat Wernicke's encephalopathy?
Pabrinex IV (thiamine replacement)
what does Wernicke's encephalopathy lead to if untreated?
Korsakoff's psychosis
what is Korsakoff's psychosis?
irreversible amnesic disorder
what are the signs for Korsakoff's?
- amnesia (anterograde + retrograde)
- psychosis
- confabulation
what is anterograde amnesia?
cannot form new memories
what is retrograde amnesia?
cannot remember old memories prior to brain damage
what is confabulation?
fabricating events to fill in memory gaps
what causes increased blood pressure and heart rate?
stimulation of hypothalamus
what causes dehydration?
kidneys secrete more urine due to osmotic effect of alcohol and inhibition of anti-diuretic hormone
what are the 2 mechanisms for alcohol metabolism?
- oxidative metabolism
- microsomal ethanol-oxidising system (MEOS)
what is the first step in oxidative alcohol metabolism?
- takes place in the hepatocytes
- ethanol is oxidised to acetaldehyde, which is catalysed by ADH (alcohol dehydrogenase found in cytosol) containing coenzyme NAD+
- ethanol ----ADH----> acetaldehyde
- CH₃+OH ---> CH₃CHO
- NAD+ ---> NADH - NAD+ is reduced
what is the second step in oxidative alcohol metabolism?
- in the mitochondria
- acetaldehyde is converted to acetate by ALDH (acetaldehyde dehydrogenase found in mitochondria)
- also results in NAD+ ---> NADH
what is NADH?
an electron transporter that enables oxidative phosphorylation to take place in mitochondria
what is the third step in oxidative alcohol metabolism?
- acetate is further oxidized in mitochondrial extrahepatic oxidation to CO₂ and water through the citric acid cycle
- acetate entering citric acid cycle generates more NADH
what happens in the microsomal ethanol-oxidising system (MEOS)?
ethanol converted to acetaldehyde by cytochrome P450 enzyme
when does the MEOS occur instead of oxidative metabolism?
chronic alcohol consumption
what is the metabolism of alcohol like in heavy drinkers?
- faster metabolsim
- high blood acetate levels
- lots of microsomal ethanol oxidising system
- dependent on a live chromosome
- uses NADPH to produce NADP+ by using ATP
- enzyme induction produced by drugs metabolised by the liver
what is the effect of alcohol on body temperature?
- it warms people up for a short amount of time
- rapid NADH production from alcohol metabolism increases energy availability and body temperature
- however risk of hypothermia
what metabolic processes are disrupted by alcohol and why?
- the oxidation of alcohol uses up a lot of energy so can inhibit metabolism of other nutrients
1) converts pyruvic acid to lactic acid
- hepatic gluconeogenesis inhibited so risk of hypoglycaemia
- overproduction of lactic acid blocks uric acid excretion of kidneys so risk of acidosis
2) inhibits lipolysis and increases lipogenesis
- too many fatty acids converted to ketones & lipids so leads to weight gain and ketosis
3) makes excess ATP
- inhibits fat oxidation leads to excess fat in liver and blood (and myocardial infarction)
how does alcohol damage the GI tract?
- inflammation of tongue, stomach, pancreas, liver and intestines
- alcohol metabolism leads to fat deposition, fibrosis and scarring of liver
- acetaldehyde interferes with absorption & activation of vitamins
- affects metabolism of drugs
- motility problems e.g. diarrhoea
what is ASH?
alcoholic steato hepatitis (ash)
- inflammation causes accumulation of extracellular matrix (collagen) from hepatic stellate cells
- leads to liver fibrosis
- scar tissue, and in severe cases can be fatal but can be reversed
what is cirrhosis of liver?
growth of connective tissue destroys liver cells with irreversible damage
what are the effects of alcohol intoxication?
- elation, euphoria, stimulation of pleasure & reward centres brain
- altered behaviour
- sedation (as it is a mild anaesthetic)
- after effects include insomnia, tiredness, nausea and headaches
what are the effects of alcohol on the brain?
- increases dopamine release -> euphoria
- inhibits glutamate receptor function -> amnesia
- potentiates GABA-A receptor function -> this is an inhibitory neurotransmitter in the brain
- increases serotonin release -> sleepiness
what are the 2 different components of pancreatic secretions?
- enzymatic
- aqueous
which enzymes does the pancreas produce?
- protease
- amylase
- lipase
which enzymes are secreted in active form?
lipases and amylase
which enzymes are secreted in an inactive form?
proteases
which cells secrete enzymes?
acinar cells
how do acinar cells secrete enzymes? (4)
- synthesised on RER and modified by golgi body
- placed in zymogen granules
- secreted upon stimulation by CCK
- granules leave by exocytosis
which cells release aqueous secretions?
ductal cells
what happens to pancreatic juice composition when flow rate increases?
- Na+ and K+ stays same
- Cl- decreases
- HCO3- increases
what happens to pancreatic juice composition when flow rate decreases?
- Na+ and K+ stays same
- Cl- increases
- HCO3 - decreases
which cell is involved in pancreatic enzyme secretion stimulation?
I cells
what stimulates I cells? (2)
small peptides and fatty acids
what do I cells do?
secrete CCK
what does CCK do?
- stimulate gallbladder contraction
- stimulate pancreatic enzyme secretion
what cell is involved in pancreatic aqueous secretion stimulation?
S cells
what stimulates S cells?
H+
what do S cells do?
secrete secretin
what does secretin do?
stimulates aqueous secretions of pancreas (ductal cells)
what 3 things does the liver store?
- carbohydrates
- vitamins
- minerals
how does the liver store carbohydrates?
as glycogen
how is glycogen synthesised? (4)
- glucose -> G6P by glucokinase
- G6P -> G1P by phosphoglucomutase
- G1P -> UDP-glucose by UDP-glucose pyrophosphorylase
- UDP-glucose added to glycogen chain by glycogen synthase
which vitamins are stored in the liver?
lipid soluble vitamins:
- A
- D
- E
- K
and vitamin B12
what mineral is stored in the liver?
iron
how is iron stored in the liver?
as ferritin
what substances can the liver synthesise?
- bile salts
- albumin
- clotting factors
- lipoproteins
what does the liver do in terms of detoxification?
- conversion of ammonia to urea
- phagocytosis
- drug metabolism
- alcohol metabolism
what role does the liver play in terms of bilirubin?
excretion of bilirubin
where does bilirubin come from?
product of macrophage destruction of haem molecules
what is the intermediate between haem and bilirubin?
biliverdin
what form is bilirubin initially in?
uncojugated bilirubin
what is the solubility of uncojugated bilirubin?
its lipid-soluble but not water-soluble
how does unconjugated bilirubin travel in the bloodstream?
binds to albumin
where does the unconjugated bilirubin and albumin travel to?
the liver
what does the liver do to unconjugated bilirubin?
hepatocytes conjugate it with glucaronic acid to make it water soluble
where does newly conjugated bilirubin go?
into the biliary system, it is secreted with bile
what happens to conjugated bilirubin in the intestines?
converted to urobilinogen by gut bacteria
what happens to urobilinogen? (2)
either:
90% - converted to stercobilin and excreted as faeces
10% - reabsorbed and excreted via kidneys as urine
what is the major vessel of the portal system?
the portal vein
what forms the portal vein?
the union of the:
- splenic vein
- superior mesenteric vein
where does union forming the portal vein happen?
posterior to the neck of the pancreas level L2
where does the portal vein go after the union?
ascends to the liver passing the superior part of duodenum and bile duct posteriorly
what happens just before the portal vein enters the liver?
it divides into left and right branches
what other smaller tributaries join to form the portal vein? (3)
- right and left gastric veins
- cystic veins
- para-umblical veins
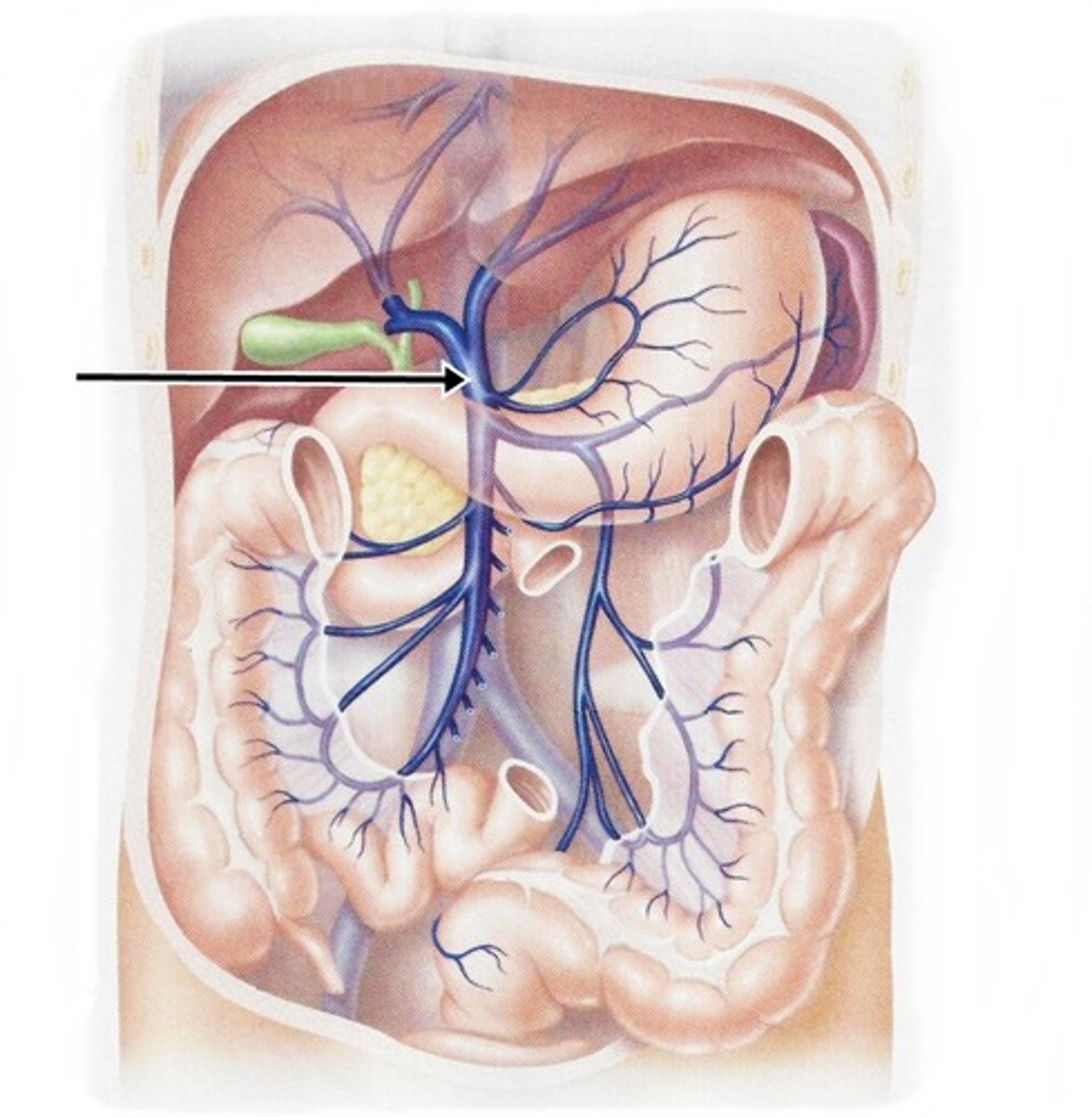
what do the para-umbillical veins do?
drain the skin of the umbilical region
what tributaries make up the splenic vein? (4)
- short gastric veins
- left gastro-omental vein
- pancreatic veins
- inferior mesenteric vein (has its own tributaries)
what tributaries make up the inferior mesenteric vein? (3)
- superior rectal vein
- sigmoid veins
- left colic veins
what tributaries make up the superior mesenteric vein? (7)
- right gastro-omental vein
- anterior and posterior inferior pancreaticoduodenal veins
- jejunal vein
- ileal vein
- ileocolic vein
- right colic vein
- middle colic vein
draw a rough diagram of the portal venous system

what is metabolism?
sum of all chemical reactions in the body
what is catabolism?
breaking down fuel into simple molecules
what is anabolism?
building up complex molecules
what are the digestive products of carbohydrates?
- monomer sugars (fructose, glucose and galactose)
- disaccharides (maltose and lactose)
what 3 things are blood glucose dependent on?
- glucose absorption from intestine
- glucose production by liver
- glucose uptake and metabolism by all tissues in body
how much hepatic glycogen is stored in the liver?
50-100g
how long does the hepatic glycogen last?
maintains blood glucose for up to a 12-24 hour fast
what is glycogenolysis?
the breakdown of glycogen to glucose via phosphorylation
when does gylcogenolysis in the liver occur?
- when there is a fall in blood glucose concentration
- very important for providing glucose to brain and erythrocytes between meals
what stimulates glycogenolysis?
glucagon and adrenaline
what inhibits glycogenolysis?
insulin
what 4 enzymes are involved in glycogenolysis?
- glycogen phosphorylase - breaks long chains of glucose molecules
- debranching enzyme - removes branches
- phosphoglucomutase - converts G1P to G6P
- glucose-6-phosphotase - coverts G6P to glucose
whats the first step in glycogenolysis?
- removal of terminal glucose by breaking the α1-4 bonds using glycogen phosphorylase or a debranching enzyme
- this releases G1P
what is the second step of glycogenolysis?
- G1P is converted into G6P by enzyme phosphoglucomutase
what is the third step of glycogenolysis?
- G6P is converted to glucose by glucose-6-phosphotase
- glucose is transported out of the cell by GLUT2 straight into the bloodstream