MIDI Module 3 Ultrasound Exam
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
The 60 minutes following injury when definitive care is crucial to a trauma patient's survival
What is the "golden hour of trauma"?
CT scan but patient needs to be cooperative, stable, and still during imaging
What is the most accurate imaging modality in trauma? What are disadvantages of this, however?
The Focused Assessment with Sonography in Trauma (FAST) while not as accurate as a CT scan, is widely considered the best initial screening modality in trauma, over DPL and physical examination;
Should initiate a FAST exam if a patient has a blunt or penetrating trauma to the abdomen or chest, a pregnant patient is in the trauma bay, and any time a patient suddenly becomes hypotensive
What is the best initial screening modality in trauma? What are indications to initiate this testing?
DPL can be used to detect intraperitoneal hemorrhage but it is limited to the abdomen (cannot evaluate chest/heart), has a lot of false positives, and can cause complications
What is Diagnostic Peritoneal Lavage (DPT) used for and what is an issue with it?
Positive FAST and stable--get CT scan;
Positive FAST and unstable--go to OR immediately;
Negative FAST and stable--get CT scan;
Negative FAST and unstable--think about what else could be causing them to be unstable that a FAST exam would not pick up (hemorrhaging in extremities or head, spinal cord injury
If patient has a positive FAST exam and is stable, what is the next step? What if they have a positive FAST exam and are unstable? What about if the FAST exam is negative and they are stable or negative FAST and unstable?
Hepatorenal window, the cardiac window (which is really two views of the heart: a subxiphoid and a parasternal long), a splenorenal window, and a suprapubic window;
Has also recently expanded to include right and left hemithoraces for a pneumothorax
What are the four main windows that comprise a FAST exam? What has it expanded to include over the recent years?
C. Pericardial, peritoneal, and pleural space
In which of the following anatomic spaces can free fluid be reliably detected with an eFAST exam?
A. Pericardial, retroperitoneal, peritoneal, and pleural
B. Pericardial, retroperitoneal, and pleural space
C. Pericardial, peritoneal, and pleural space
D. Retroperitoneal, peritoneal, and pleural
E. None of the above
Space between the liver and kidney called Morison's pouch;
The transducer is placed at the 8th to 10th intercostal space along right mid-axillary line while the transducer indicator is pointing towards the head;
Spleen between the spleen and kidney and the indicator is pointed towards the head as well
What is the space we are observing in the right upper quadrant and what is it called? What position is the indicator pointing towards in this view and where is the transducer places itself? What is the space we are observing in the left upper quadrant and what is the position of the indicator on that view?
Because it is the largest parenchymal organ in the body, has a high fluid content, and homogenous nature
Why is the liver a very useful sonographic acoustic window for imaging upper abdominal and retroperitoneal anatomy?
Subxiphoid view with the indicator towards the patient's right flank
Parasternal view in the third or fourth intercostal space with the indicator towards the patient's left elbow
What are the two views of the heart we can do on FAST exam? Where is the indicator pointed in each?
It sits deep to the ninth through eleventh ribs along the left lower chest
At what part on the chest wall does the spleen sit?
Transverse with the indicator towards the right flank/hip
Sagittal with the indicator towards the head
What are the two views of the pelvis FAST exam? Where are the indicators pointed?
It is started on the second or third intercostal space;
Probe indicator is pointed towards the head
What is the lung ultrasound started on FAST exam? Where is the probe indicator pointed?
Generally, low frequency transducers are more appropriate for FAST exam because they penetrate deeper into the body tissues, which is what we need to see unlike high frequency transducers which are better for superficial structures and will have a better resolution
In general, what transducers are most appropriate for a FAST exam and why?
Endocavity--8 to 4 MHz
Curvilinear-- 5 to 2 MHz
Linear sequential-array--10 to 5 MHz
Phased array--5 to 1 MHz
What are the frequency ranges of each transducer?
A. coronal
The eFAST right upper quadrant window should be imaged along which of the following body planes?
A. coronal
B. Parasagittal
C. Sagittal
D. Oblique
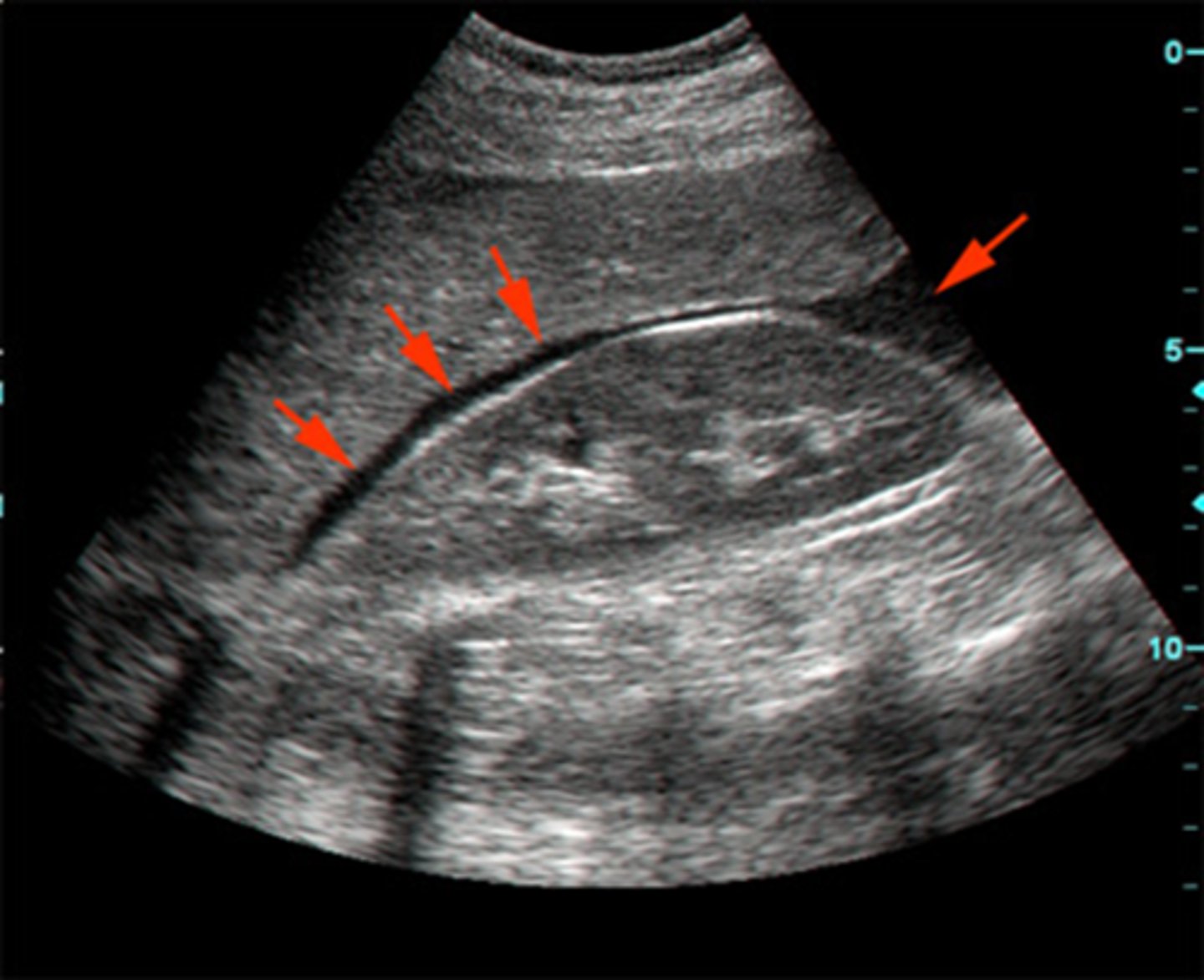
Morison's pouch because it is the most dependent portion of the peritoneal cavity;
This means that it is important to fan through the entirety of the RUQ to make sure you are not missing any fluid
Where is the mostly likely site you will find blood in a supine patient? Why? What does this mean?
When the lower pole of the kidney comes halfway down your ultrasound window;
If there was fluid in Morison's pouch, there would be an anechoic area between the homogenous liver and kidney
How do you know you have scanned the entirety of Morison's pouch? What would it look like if there was fluid here?
Patient will lie in a supine position with the knees slightly bent;
The transducer should be placed just below the xiphoid process, at a 15- to 30-degree angle to the skin with the beam pointed towards the patient's anatomic-left shoulder;
Transducer indicator is pointed to the patient's right flank;
Should remember to ask your patient to take a deep breath causing the diaphragm and heart to drop lower in the chest, improving the image quality
How does the patient sit when performing the subxiphoid view on FAST exam? How is the transducer positioned and where is the indicator pointed towards? What is important to keep in mind during this view?
Closest to the ultrasound--liver-->pericardium-->right atrium and right ventricle-->inter ventricular septum-->left atrium and left ventricle-->pericardium (all the way around it)
On the subxiphoid view, list the contents on the desired ultrasound image window from the closest to the ultrasound beam to the farthest away?
E. A and B only (Position the transducer with the indicator towards the patient's anatomic right. Aim the transducer toward the patient's chin, and hold the probe nearly parallel to the patient's abdominal wall. If the ultrasound transducer were a flashlight, aim the beam of the flashlight toward the patient's chin, with the transducer's footprint against the soft tissue, just under the xiphoid process.)
To optimize the subxiphoid cardiac view, _________.
A. use the liver as an acoustic window
B. be sure the patient's bed is flat
C. position the ultrasound transducer at a 90-degree angle, perpendicular to the patient's abdomen
D. All of the above
E. A and B only
B. False (Neither cardiac view is attainable in all patients. Sonographers should attempt to obtain both views and use whichever view provides the most optimal visualization.)
The parasternal long (PLAX) cardiac view is always easier to obtain than the subxiphoid cardiac view.
A. True
B. False
The stomach can get in the way if probe is too anterior and creates misreadings;
When there is air in the stomach, it looks very hyperechoic and gets in the way but when there is fluid in the stomach, it looks very anechoic and be mistaken for fluid in the LUQ space
What is a challenge when obtaining the left upper quadrant image? What are potential misreadings?
D. All of the above (The transducer should be held in a coronal plane, relative to the body. Since the spleen is small relative to the liver, the left kidney and, therefore, the splenorenal interface will sit more superiorly and posteriorly, when compared to the right upper quadrant hepatorenal interface. This slight shift will often require the ultrasonographer to hold the transducer with their knuckles buried deep into the cushion of the gurney to be able to use the spleen as an acoustic window, commonly described as "knuckles to the bed." Additionally, the spleen and the left kidney are often tightly tethered together, causing the splenorenal interface to be less likely to gather free fluid. Free fluid will alternatively pool along the inferior pole of the left kidney and along the dome of the spleen, just under the diaphragm.)
To obtain an optimal left upper quadrant view of the splenorenal interface, __________.
A. hold the ultrasound transducer in a coronal plane
B. hold the ultrasound transducer slightly superior and posterior with respect to the position that was held for the right upper quadrant view
C. avoid imaging the stomach
D. All of the above
E. None of the above
A. fan the transducer slightly posteriorly (Imaging of the left upper quadrant view begins in a coronal plane at about the midaxillary line. When the spleen and diaphragm have been located, fan the transducer slightly posteriorly to bring the left kidney into view, without sliding the probe along the patient's skin. This brings the retroperitoneal space into the plane of view. Another way to imagine the movement is to pretend the probe is a flashlight and shine the flashlight slightly towards the spine.)
When visualizing the left upper quadrant, if the spleen and diaphragm have been visualized, but the kidney is not in its expected place, __________.
A. fan the transducer slightly posteriorly
B. fan the transducer slightly anteriorly
C. rotate the transducer 90 degrees clockwise
D. rotate the transducer 90 degrees counterclockwise
E. None of the above
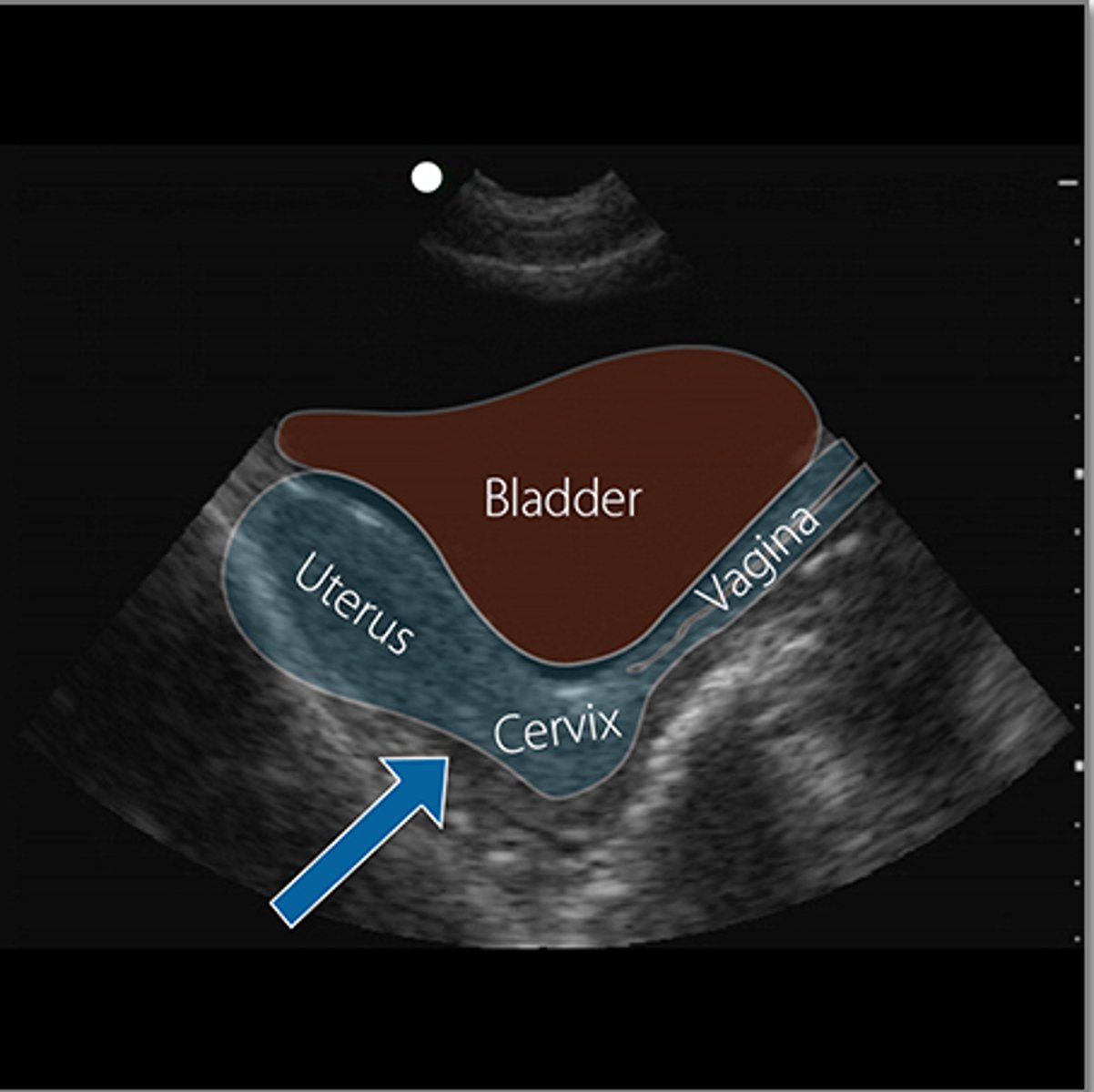
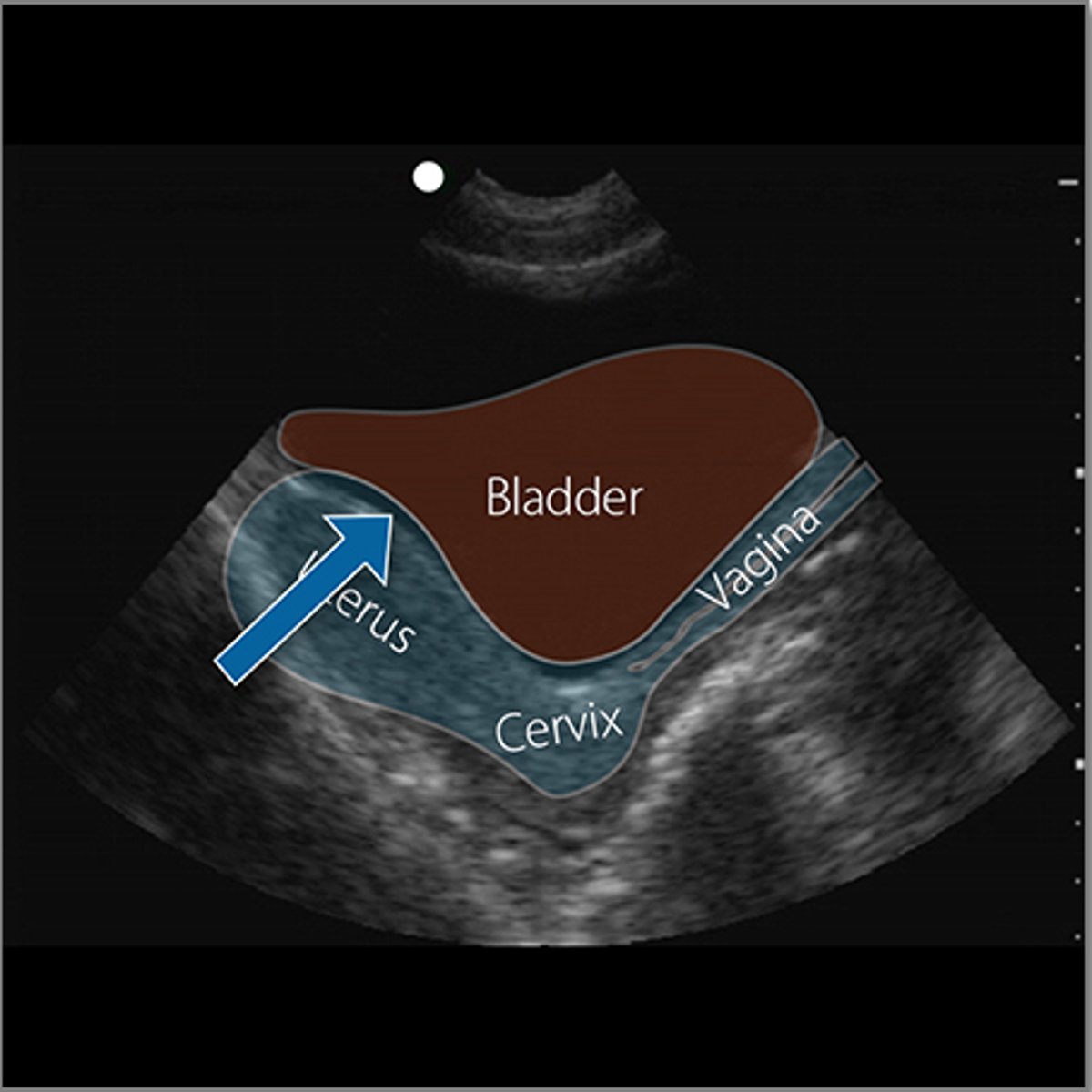
Endovaginal stripe indicating the wall of the vagina;
It ends at the cervix
In the transfer pelvic view, what is the white, echogenic, hyperechoic structure just inferior to the bladder and what does this indicate? Where does it end?
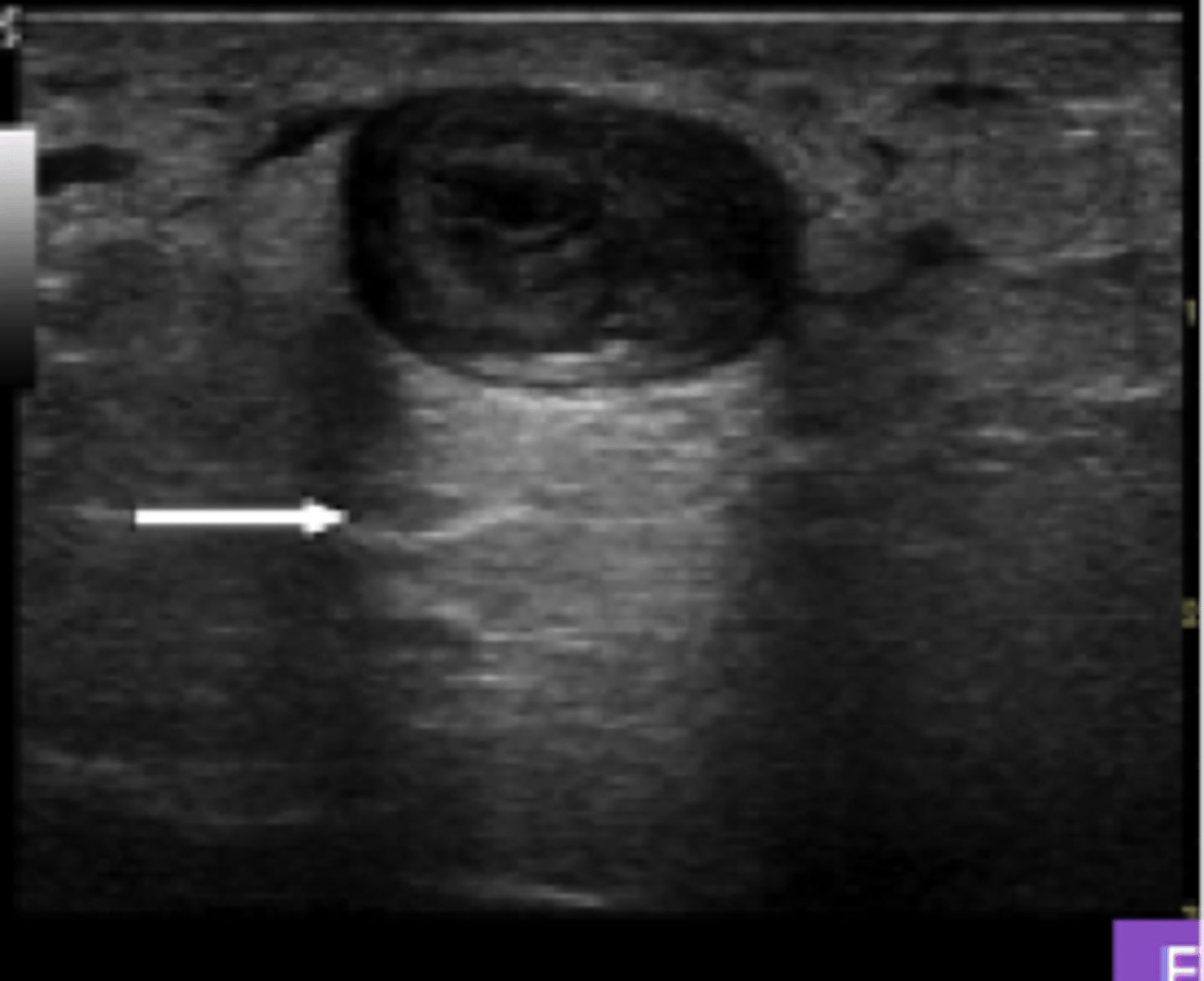
Posterior cul-de-sac
What is the arrow pointing to in this ultrasound image?
Anterior cul-de-sac
What is the arrow pointing to in this ultrasound image?
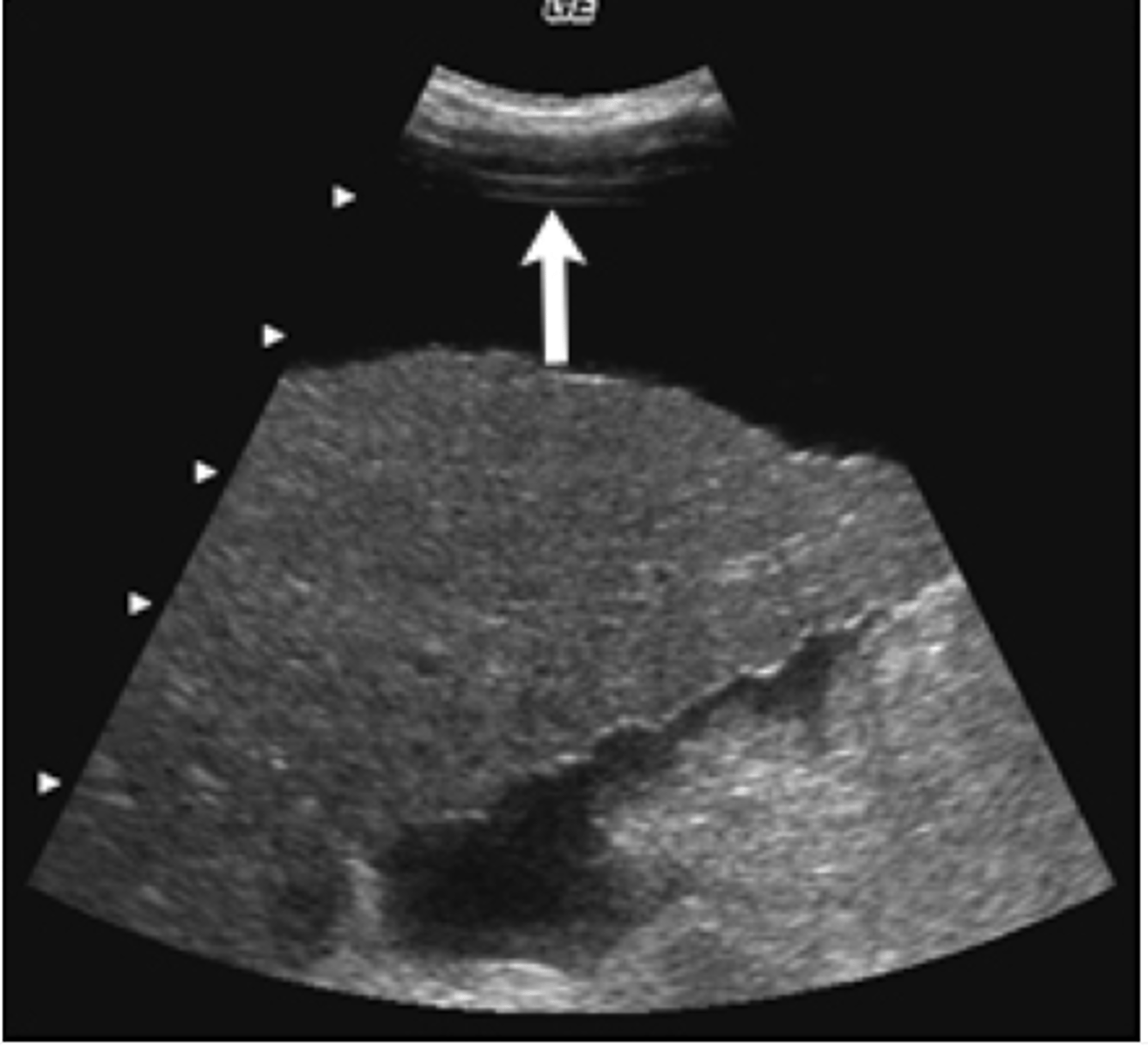
Showing fluid in Morison's pouch in the RUQ view
What is indicated in this photo and in what location is it found?
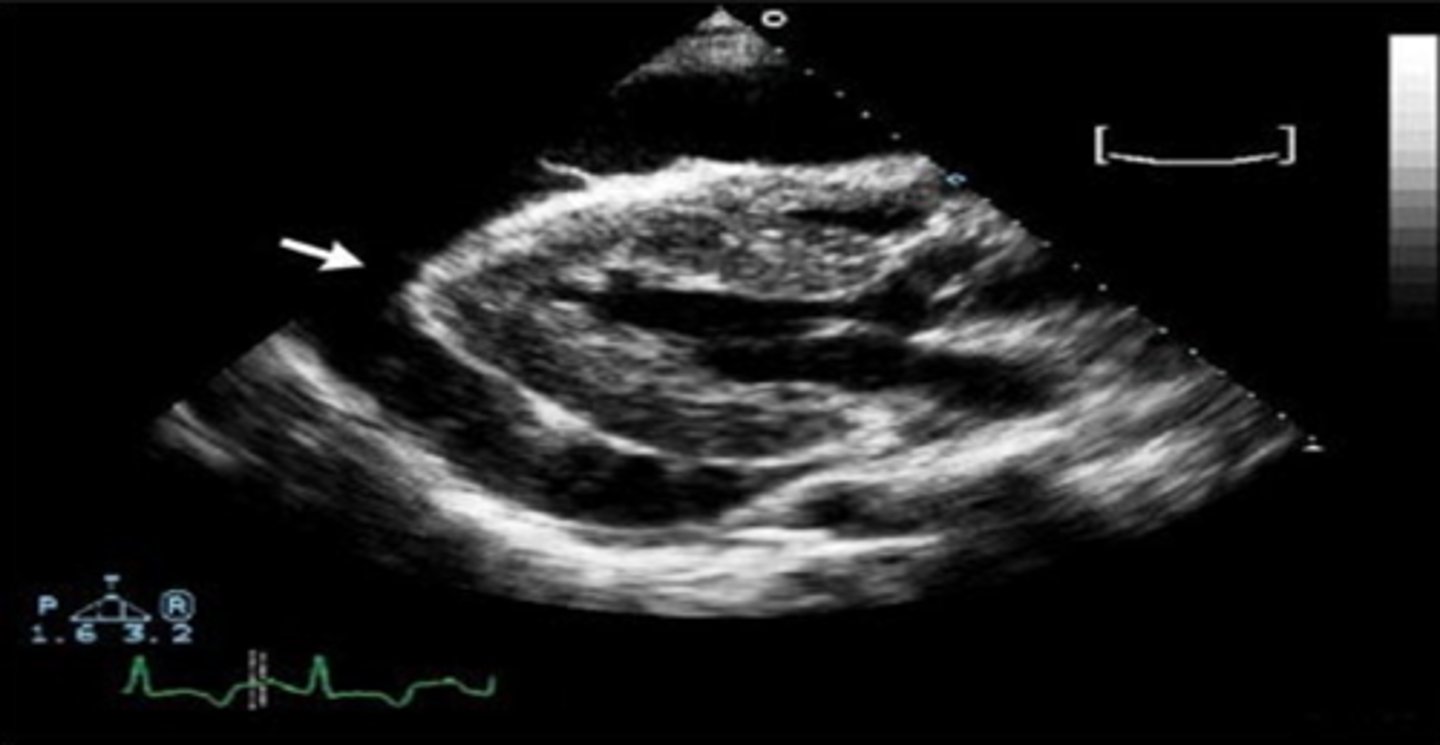
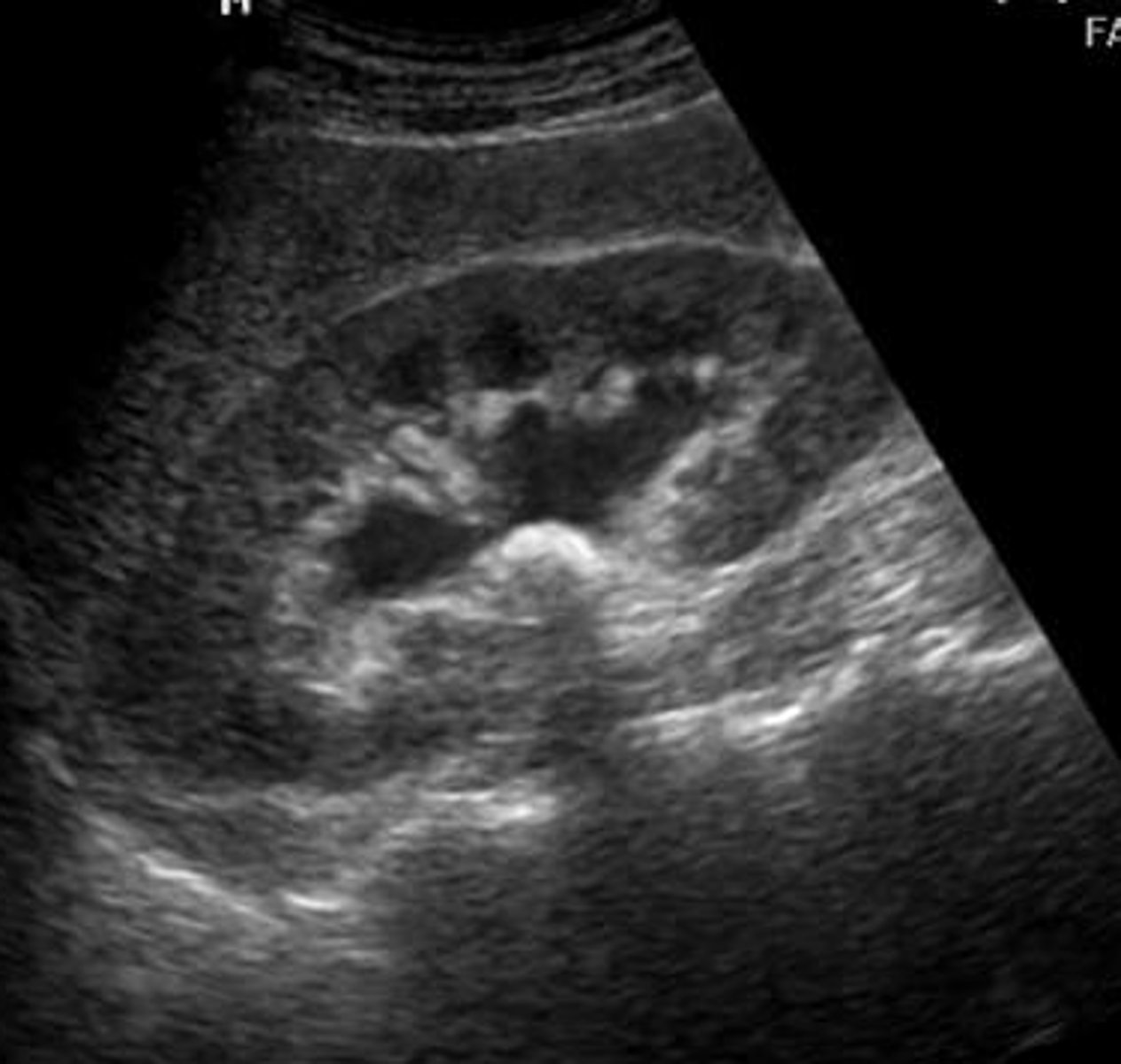
Pericardial effusion surrounding the heart
What is shown in this picture?
D. All of the above (The sagittal pelvic view translates to the peritoneal cavity/pelvic cavity interface appearing on the left side of the ultrasound screen. Therefore, free fluid in the pelvis and the peritoneal cavity appears on the left side of the screen. The free fluid will fill potential spaces of the pelvis, including the vesicouterine space (anterior cul-de-sac) and the rectouterine space (posterior cul-de-sac or pouch of Douglas).
On the sagittal pelvic view, free fluid can be found collecting in the __________.
A. vesicouterine space (anterior cul-de-sac)
B. rectouterine space (posterior cul-de-sac or pouch of Douglas)
C. on the left side of the ultrasound screen
D. All of the above
E. None of the above
Upper lung field;
FAST exam of the lung field is started here because free air in the thoracic cavity will rise to the least gravity-dependent region so most likely to see a pneumothorax here
What is the least gravitationally dependent area of the inner hemithorax and why is this where the exam is started?
Pleural line showing the sliding-lung sign as the visceral and parietal pleurals slide past each other;
If there is no sliding-lung sign, there is a possibility of pneumothorax, emphysema, or hyperinflated lung states, and following lung pleurodesis
What is the hyperechoic line seen on this moving image and what is it displaying? When this is absent, what could that indicate?
A sliding-lung sign, comet-tail artifacts (B-line artifacts), and a lung pulse
What is the absence of a pneumothorax supported by?
B-line artifacts are vertical, laser-like lines projecting from the pleural surface into the far field;
The absence of these signs suggests the possibility of a pneumothorax under the transducer
What are B-line artifacts? What does the absence of these indicate?
It is more useful when documenting lung sliding of normal lungs on a still image with the "seashore sign";
When viewing the lungs, non-moving tissue appears as a straight line while moving tissue, pleural sliding, yields a granular pattern
What is M-mode helpful for? What does this show on exam of helpful view?
Lung point, intersection between the lung moving against the inner chest wall and the pneumothorax
What is the the most reliable sonographic finding for a pneumothorax?
Since the liver (RUQ) and spleen (LUQ) are just inferior to the diaphragm and the chest cavity is just superior to it, a normal finding would be to see mirror imaging of both the liver and spleen across the diaphragm;
An abnormal result would be if there is no mirror imaging and will look anechoic, meaning that the chest cavity is filled with fluid
What is typical to see on the RUQ and LUQ imaging above the diaphragm? What is abnormal finding?
Epicardial fat will be heteroechoic and is tacked down to the heart, so it moves with the heart as the heart is beating and pericardial effusion will appear as an anechoic stripe around the beating heart;
While both the clot and fat are not anechoic or hyperechoic, an epicardial fat is rarely more than 1cm and clots are usually bigger than that
How do you distinguish between epicardial fat and a pericardial effusion? What about between a pericardial clot and epicardial fat?
Can use an NG tube to remove the fluid if it is in the stomach and then recheck ultrasound to make sure there is no lingering fluid
If you are concerned about if fluid seen on ultrasound is in the stomach or between the spleen and the kidney, how can you differentiate without surgery?
D. All of the above (A pericardial fat pad is a common finding. It is often mistaken for a pericardial effusion. It is a thin layer of fat found primarily along the anterior surface of the heart. Of note, from a terminology perspective, an epicardial fat pad refers to visceral fat that is directly in contact with the myocardium and is located beneath the visceral pericardial layer (Talman et al.). Pericardial fat refers to fat located between the visceral and parietal pericardial layers, while paracardial fat (or mediastinal fat) is located external to the parietal pericardial layer)
A pericardial fat pad __________.
A. can be mistaken for a pericardial effusion
B. is usually less than one centimeter in thickness
C. does not typically surround the entire heart
D. All of the above
E. None of the above
D. All of the above (During an eFAST exam, placing the regions of interest in a dependent position will increase imaging sensitivity. For example, complete the right upper quadrant view before the patient is moved. Supine patient positioning facilitates imaging of this quadrant. Complete the left upper quadrant view just after the patient is rolled onto his or her left side for the back exam. Placing a nasogastric tube will help decompress the stomach and minimize the chance of misinterpreting gastric contents for free intraperitoneal fluid. Obtaining a pelvic view prior to placement of a Foley catheter will ensure the distended bladder serves as an acoustic window for ultrasound imaging.)
To increase the accuracy of the eFAST exam, __________.
A. place the abdominal quadrant of interest in a dependent position
B. insert a nasogastric tube
C. perform the exam prior to Foley catheter insertion
D. All of the above
E. None of the above
D. Perinephric fat displays mixed echogenicity (Perinephric fat can often be mistaken for free fluid because it displays mixed echogenicity, when compared to anechoic free fluid. It can be distinguished from free fluid because it has a heterogeneous and hyperechoic appearance when compared to anechoic free fluid. It also does not fill potential spaces, as free fluid does. When free fluid fills potential spaces between solid organs, its edges become pointed)
Which of the following best characterizes perinephric fat?
A. Perinephric fat has a uniform anechoic appearance
B. Perinephric fat is an extremely rare sonographic finding
C. Perinephric fat has a uniform hyperechoic appearance
D. Perinephric fat displays mixed echogenicty
E. A, B, and C
Which of the following choices may optimize the subxiphoid cardiac view?
A. Ensure the patient's bed is flat.
B. Use the liver as an acoustic window.
C. Hold the ultrasound transducer flat against, and often nearly parallel, to the patient's abdomen.
D. A and B
E. A, B, and C
D. All of the above
Which of the following statements is correct regarding lung sonography performed during an eFAST exam?
A. The exam is started on the anterior chest in the second or third intercostal space.
B. Lung sliding excludes pneumothorax at that location.
C. The probe should be positioned perpendicular to the chest wall between two adjacent ribs.
D. All of the above
E. A and B only
B. False
The FAST examination is more accurate than CT imaging for detecting retroperitoneal pathology.
A. True
B. False
E. All of the above
Which of the following choices increases sensitivity of the FAST exam?
A. Completing pelvic imaging prior to Foley catheter insertion
B. Placing the abdominal quadrant of interest in a dependent position
C. Slowly fanning the transducer during window imaging to detect subtle pockets of free fluid
D. Performing serial FAST exams at varying stages of a patient's resuscitation
E. All of the above
B. False
The recto-uterine space is also referred to as the anterior cul-de-sac.
A. True
B. False
B. False
The parasternal long cardiac view is always obtainable and is the preferred cardiac view.
A. True
B. False
A. Left upper quadrant, right upper quadrant, cardiac, pelvic
What are the basic views for the FAST exam?
A. Left upper quadrant, right upper quadrant, cardiac, pelvic
B. Left upper quadrant, right upper quadrant, pleural, retroperitoneal, cardiac
C. Left upper quadrant, right upper quadrant, pleural, pelvic
D. Right upper quadrant, cardiac, pleural, retroperitoneal, pelvic
E. None of the above
B. False
There is no benefit in repeating a FAST exam following initiation of resuscitation (e.g., within 10 minutes of the initial FAST exam), because it is rare to have new findings appear.
A. True
B. False
B. False
A high-frequency linear transducer should always be used to perform an eFAST examination.
A. True
B. False
E. All of the above
Which of the following choices may help obtain an optimal right upper quadrant view of the hepatorenal interface?
A. Hold the ultrasound transducer slightly inferior and anterior with respect to the position that was held for the left upper quadrant view.
B. Hold the ultrasound transducer in a coronal plane.
C. Avoid placing the transducer directly over ribs.
D. When using an abdominal curved-array transducer, rotate the transducer slightly counterclockwise (5 to 10 degrees) from the coronal plane to position the transducer between ribs.
E. All of the above
A. True
The acronym "FAST" stands for "focused assessment with sonography in trauma".
A. True
B. False
B. False
FAST is more accurate than diagnostic peritoneal lavage for detecting intraperitoneal hemorrhage.
A. True
B. False
E. All of the above
When obtaining a transverse pelvic view in the setting of trauma, if the bladder cannot be visualized, __________.
A. the bladder may be empty due to recent voiding
B. the bladder may be ruptured
C. overlying subcutaneous emphysema may be limiting visualization
D. the transducer may be overlying the pubic symphysis
E. All of the above
D. All of the above
Which of the following statements regarding left upper quadrant FAST imaging is correct?
A. Fluid in the stomach can be mistaken for free intraperitoneal fluid.
B. Stomach fluid is often anechoic.
C. Stomach fluid is encapsulated and does not fill the splenorenal interspace.
D. All of the above
E. None of the above
E. All of the above
When inspecting the thoracic cavity for a hemothorax, __________.
A. a hemothorax will appear hyperechoic if the blood is clotted
B. a hemothorax will appear anechoic if the hemorrhage is fresh
C. sensitivity can be increased if the patient is put in reverse Trendelenburg position
D. a small hemothorax may be difficult to distinguish from a sliver of intraperitoneal blood layering out under the diaphragm
E. All of the above
A. True
In a supine patient, the hepatorenal interface, or Morison's pouch, is one of the most dependent points within the peritoneal cavity.
A. True
B. False
E. All of the above
When obtaining a parasternal long cardiac view, if the heart cannot be visualized, __________.
A. slide the transducer directly over a rib interspace
B. the patient may have subcutaneous emphysema, obscuring the view
C. ensure the transducer is not positioned over the sternum
D. attempt a subxiphoid view as an alternative
E. All of the above
C. Coronal
The left upper quadrant FAST view requires the ultrasound transducer to be held in a __________ plane.
A. Sagittal
B. Transverse
C. Coronal
D. Oblique
E. Horizontal
Contains small piezoelectric crystals that vibrate when an electric signal is applied to them producing sound waves that penetrate the body
What does an ultrasound probe contain that produce an image?
Sound waves travel fastest through solids, slower through liquids, and slowest through gases;
Solids--highest amplitude, Liquids--lower amplitude, Gases--lowest amplitude
What is the rate of sound waves through each of the following structures: solids, liquids, gases? How are the amplitudes of the electrical waves after hitting each of these objects returning back to the probe?
Moving--either sliding, moving the probe parallel to the indicator, or sweeping, which means moving the probe perpendicular to the indicator in a translational plane;
Tilting--moving the probe perpendicular to the indicator; this is perpendicular to rocking;
Rocking--"heel-toeing"; rocking the probe towards and away from the probe indicator;
Rotating--turning the probe clockwise or counterclockwise without moving the probe from the surface
What do the following movements with an ultrasound probe indicate: moving, tilting, rocking, and rotating?
D. All of the above (Cardiologists have long ago established the historical standard imaging conventions for echocardiography. The default probe indicator setting in echocardiography machines is set along the right side of the echocardiography machine screen, from a viewer's perspective. Some non-cardiologists using standard point-of-care ultrasound machines may view the heart with an abdominal-imaging preset. The default probe indicator setting is aligned along the left side of the ultrasound unit screen, from a viewer's perspective)
Which statement regarding cardiac ultrasound imaging conventions and techniques is correct?
A. Historical echocardiography convention places the probe indicator on the right side of the ultrasound screen from a viewer's perspective.
B. An abdominal-imaging preset mode will place the probe indicator on the left side of the ultrasound screen from a viewer's perspective.
C. Point-of-care practitioners performing a time-sensitive FAST exam often image the heart with an abdominal-imaging preset mode.
D. All of the above
E. None of the above
D. All of the above (The parasternal long-axis view is used for overall assessment of left ventricular chamber sizes, systolic function, and regional wall motion. It also gives one a good view of the mitral and aortic valves and helps one to evaluate valvular stenosis and regurgitation. Finally, one gets a good look at the pericardium and can evaluate for the presence of a pericardial effusion. Of note, this view is not ideally suited for evaluation of the right heart, as right ventricle size will vary greatly based on image window location.)
Which of the following statements regarding the parasternal long-axis view is correct?
A. It typically provides excellent views of the mitral and aortic valves.
B. It can be used to screen for pericardial effusion.
C. The left ventricle appears at the bottom, or far field, of the screen with the cardiac apex on the left side of the ultrasound screen, from a viewer's perspective.
D. All of the above
E. None of the above
A. The patient should be lying flat on the bed to enable optimal cardiac imaging. (In most patients, to obtain the parasternal imaging window one needs to place the patient in the left lateral decubitus position. When the patient is in 30- to 45-degree left lateral decubitus positioning, the heart is brought closer to the chest wall. Supine positioning would have the effect of moving the heart posteriorly and pulmonary gas more anteriorly. The parasternal long-axis imaging plane travels from the patient's anatomic right shoulder to the patient's anatomic left hip. It is oriented along the long axis of the heart, which travels from base to apex. The indicator on the transducer should be aimed towards the patient's anatomic right shoulder when observing echocardiography convention. The scanning window is immediately to the anatomic left of the sternum in the 3rd to 5th intercostal spaces. The location of a particular imaging window may vary in an individual patient based on body habitus, heart size, and heart orientation.)
Which of the following statements regarding the parasternal window is incorrect?
A. The patient should be lying flat on the bed to enable optimal cardiac imaging.
B. The transducer is placed in the 3rd to 5th intercostal space, to the anatomic left of the sternum.
C. The probe indicator should appear on the right of the ultrasound screen, from a viewer's perspective, in a cardiac-imaging preset mode.
D. The probe indicator should point to the patient's anatomic right shoulder during parasternal long-axis window acquisition.
E. The parasternal long-axis window is oriented along the long axis of the heart.
Used for overall assessment of left ventricular chamber size and systolic function, right ventricular size and systolic function, and presence of a pericardial effusion
What is the parasternal short-axis view on ultrasound used for?
D. All of the above (The parasternal short-axis view is obtained by initially observing the imaging conventions for obtaining the parasternal long-axis view. From the parasternal long-axis view, one should rotate the transducer 90 degrees clockwise to obtain the mid-ventricular parasternal short-axis view. The parasternal short-axis view at the mid-ventricular level is used for overall assessment of left ventricular chamber size and systolic function. It is also a great view for regional wall motion assessment, as one is able to see wall motion at the mid-ventricular level for all the walls of the heart, and in all three coronary artery distributions. One can also get a good overall view of the interventricular septum and right ventricular size and systolic function.)
Which of the statements most accurately describes the parasternal short-axis view at the mid-ventricle?
A. The transducer indicator is rotated clockwise 90 degrees relative to its location when obtaining a parasternal long-axis view.
B. A circumferential view of the left ventricle is provided.
C. The right ventricle size and systolic function can be appreciated.
D. All of the above
E. None of the above
Parasternal short-axis view at the base of the heart-- can assess for thickening, calcification, or restriction in motion
What is the best view for the assessment of the morphology of the aortic valve?
Subcostal view
What view is the best to evaluate for a pericardial effusion?
C. It provides excellent visualization of the pericardial space (The subcostal four-chamber view is obtained with the patient in the supine position, with the knees slightly bent. The transducer should be placed just below the xiphoid process, nearly parallel to the skin, with the ultrasound beam pointed towards the patient's anatomic left shoulder. Asking the patient to breathe deeply will cause the diaphragm to lower and will improve the subcostal image window. The subcostal view is excellent for assessment of a pericardial effusion. One gets an excellent view of not only the size and location of the effusion, but also its corresponding effect on the right ventricle.)
Which of the following statements regarding the subcostal four-chamber view is correct?
A. A left lateral decubitus body position should be used to optimize image acquisition.
B. The transducer should be routinely placed several centimeters to the anatomic left of the xiphoid process to optimize image acquisition.
C. It provides excellent visualization of the pericardial space.
D. All of the above
E. None of the above
A low-frequency transducer should be selected like curved-abdominal probe or phased-array;
By determining the degree of collapse of the IVC upon inspiration (less than 2.1cm and inspiratory collapses by more than 50%, it is normal)
When evaluating the inferior vena cava, what probe should be used? How can you estimate the right atrial pressure in this view?
D. All of the above (Start from a subcostal view, with the probe indicator aiming towards the anatomic left side of the patient and the transducer head, or scanning surface of the probe, aimed at the anatomic left shoulder of the patient. The transducer head should be rotated counterclockwise towards the patient's anatomic right shoulder. Simultaneously, the transducer needs to be tilted perpendicular to the long axis of the body. This will create an excellent longitudinal view of the intrahepatic IVC as it enters the right atrium.The size and collapsibility of the IVC are influenced by changes in intravascular volume. This is used to judge whether adequate fluid resuscitation has occurred. One can estimate the right atrial pressure by determining the degree of collapse of the IVC upon inspiration. Recent literature has established the degree of inspiratory collapse of the IVC as more predictive of right atrial pressure than IVC diameter. Respirophasic variation in IVC diameter should be measured two centimeters distal to the entry of the hepatic veins into the IVC)
Ultrasound assessment of the IVC __________.
A. can be performed by transitioning from the subcostal four-chamber view of the heart
B. is useful for assessing intravascular volume
C. can be used to monitor the progress of volume resuscitation by assessing changes in the intrahepatic IVC after fluid boluses
D. All of the above
E. None of the above
In the parasternal long-axis view, the pericardiac effusion will be adjacent to the coronary sinus, which is an intrapericardial structure whereas the pleural effusion will be adjacent to the descending aorta, which suggests that this is an intrapleural collection of fluid
How can we tell the difference on ultrasound of a pericardiac effusion and pleural effusion?
E. B and C only (Assessing left ventricular chamber dimensions, ejection fraction, and regional wall motion can provide a qualitative estimation of left ventricular systolic function. Normal function equates with an ejection fraction of 55 to 70%, while severely reduced function correlates with an ejection fraction of 30% or less. Studies have documented that clinicians can qualitatively classify left ventricular systolic function as normal, mild-to-moderately reduced, and severely reduced with reasonable precision. The apical four-chamber view, along with other cardiac views, can be used to estimate cardiac ejection fraction.)
Estimating ejection fraction __________.
A. requires careful computation and should only be performed via computerized automated algorithms
B. can be accurately performed in a qualitative manner
C. is commonly performed using the apical four-chamber view
D. All of the above
E. B and C only
D. All of the above (Echocardiographic pericardial tamponade is characterized by the triad of: diastolic collapse of the right ventricular free wall, an IVC that is dilated with little respirophasic change, and the appearance of a swinging heart. These features are the result of high intrapericardial pressure compressing the right side of the heart and reducing preload.)
Which of the following represent criteria used to determine whether pericardial tamponade is present?
A. Degree of inferior vena cava collapse with inspiration
B. A "swinging heart" sign
C. Whether there is evidence of diastolic collapse of the right ventricular free wall
D. All of the above
E. B and C only
The progressive weakening of the sound as it travels into and out of the body;
When encountering high-attenuating structures like bone, echoes are weakened posteriorly, and an acoustic shadow results;
When sound waves hit a gallstone (high-attenuating structure), a shadowing occurs posterior to the stone
What does attenuation mean? What happens when sound waves hit a high-attenuating structure? What is an example of this?
When echos travel through a low-attenuating structure (like the bladder) and structures behind it get enhanced;
This is also called posterior acoustic enhancement
What is "through-transmission" artifact? What is this also called?
Dirty shadowing;
Refraction occurs when sound travels across one medium into another and is redirected and changes speed, creating an edge shadow or structure
What kind of artifact does gas usually create? When does refraction artifact occur?
Edge artifacts;
Occurs when sound waves pass distal to smooth, rounded cavities containing fluid like the bladder, aorta, or other fluid-filled cystic structures
What are the blue areas pointing to and where does this usually occur?

Posterior acoustic enhancement
What artifact is this arrow pointing to?
Comet-tail reverberation artifact because of the successive lines of artifact in a linear structure
What artifact is this arrow pointing to and how do you know?

Reverberation
What artifact is this arrow pointing to?
Defined by the absence of lung sliding and the perception of cardiac pulsation at the pleural line;
Pleural line will be characterized by very limited to-and-fro movement, often described as a shimmering appearance that matches the heart rate
What is lung pulse? What does it look like?
They are hyperechoic, horizontal lines that appear at regular intervals deep to the pleural line;
Type of reverberation artifact;
It is normal to have many of these artifacts
What are A-lines? What type of artifact are they? Is it normal or abnormal to have these?
They are hyperechoic, vertical lines that arise at the pleural line, move with respirations, erase the normal A-line pattern, and extend downwards off the screen without fading;
Having more than 3 in an intercostal space is abnormal and indicates fluid in the alveolar-interstitial spaces
What are B-lines? Is it normal or abnormal to have these?
-In the lungs to better document that pleural sliding
-In the bladder to better detect ureteral obstruction
-In the prostate for potential biopsy sites
What have we used color Doppler with this semester?
Obese patients may be best imaged with a low-frequency transducer, for greater depth, while thin adults and pediatric patients may be best imaged with a high-frequency linear transducer, for greater resolution
On what body habitus are you more likely to use a low-frequency transducer? What about a high-frequency? Why?
It is capable of retaining 500 mL or more of urine
How much can the urinary bladder capable of retaining?
The renal cortex is echogenic with the most echogenic area at the renal sinus due to its high fat content and the medullary pyramid is relatively anechoic
How can you tell the different parts of the renal parenchyma apart?
Curved-abdominal probe
What is the ideal transducer for imaging the kidneys?
Because of the large acoustic window provided by the liver on the right
Why is the right kidney easier to view than the left?
If a patient is avoiding voiding, has an overly distended bladder or if the renal sinus shows distention and dilation, or there is splaying or separation of the typically uniform echogenic renal sinus with interposed echo-free areas;
Well-hydrated pregnant women can be mistaken for hydronephrosis because they also have separation of the uniform echogenic renal sinus
What is a sign of bilateral hydronephrosis on renal ultrasound? What case can also be mistaken for bilateral hydronephrosis due to one of these signs?
Grade II--There will be dilation of the major and minor calyces, and the appearance is sometimes described as a "bear claw";
Grade III--There will be dilation of the renal calyces, as well as thinning, or effacement, of the renal parenchyma
How is a Grade II Moderate hydronephrosis viewed on ultrasound? What about Grade III Severe hydronephrosis?
Hydronephrosis most likely due to obstruction to urinary outflow
What is the diagnosis of this patient? What is the most likely cause?
E. A and C only
Renal ultrasound examinations __________.
A. may require a phased-array transducer to image between ribs
B. require transducer frequencies of 2 to 1 MHz
C. necessitate selecting a transducer that matches the patient's body habitus
D. All of the above
E. A and C only
D. All of the above
The normal adult kidney's architecture is characterized by __________.
A. a length of 10 to 12 cm
B. a thickness of up to 3 cm
C. a hyperechoic outer renal capsule
D. All of the above
E. None of the above
B. Proximal ureter
Which structure is readily identifiable along the renal hilum with sonography?
A. Adrenal artery
B. Proximal ureter
C. Renal nerve
D. Adrenal vein
E. None of the above
E. B and C only
Which of the following structures is located within the retroperitoneal space?
A. Ileum
B. Abdominal aorta
C. Inferior vena cava
D. All of the above
E. B and C only