2.7 Equine repro abnormalities and disease
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Indications for Caslick’s vulvoplasty (5)
Poor perineal conformation and subfertility
Pneumovagina (incompetent vestubular fold → air sucking)
Cervicitis and endometritis (possibly from faecal contamination)
Endometritis is main reason
Perineal tears
Repetitive foaling
When does a Caslick’s vulvoplasty need to be removed?
Before foaling → foal needs to come out
Path of least resistance - if Caslick’s then could force itself out elsewhere with fatal damage
Steps of Caslick’s vulvoplasty (3)
Anaesthetise and restrain the horse
Remove 0.5-1cm of mucosa close to the internal margin of the vulva
Appose and suture the vulva lips
leave space for peeing at bottom of vulva
What impact on the cervix does ageing have and how does this lead to inflammation? (3)
Cervical fibrosis
Cervix cannot fully relax after oestrus
Semen debris builds up → inflammation
Most common uterine neoplasia
Leiomyoma (smooth muscle)
but rare
How do foreign bodies in the uterus affect the horse?
Mimic pregnancy → pauses cycle, mare cannot come into oestrus
marbles can be used for same effect
What causes CEM and where is it carried asymptomatically?
Taylorella equigenitalis → notifiable
Pseudomonas and Klebsiella can cause similar disease
Clitoral fossa and sinus
3 clinical signs of CEM
Acute metritis
Copious creamy vulval discharge
Early return to oestrus (occurs with basically any infection)
Metritis V endometritis
Endometritis is more superficial tissue → less severe
2 main pathogens responsible for endometritis (if infectious)
Ascending urogenital or GIT pathogens
E. coli
beta haemolytic Strep
Cutoff point for inflammation indicating endometritis after breeding
If inflammatory response persists 12+ hours (free fluid in lumen of uterus) → endometritis
3 conformational abnormalities potentially responsible for endometritis
Sloped perineum
Pendulous uterus
Urine pooling
3 clinical signs for endometritis
Excessive intraluminal fluid
Prolonged, early return or erratic oestrus (without ovulation)
Failure to conceive or early embryonic death
3 methods to extract a pathogen for culture in endometritis
Endometrial swab
Low volume lavage
Endometrial biopsy
2 treatments to remove the fluid in utero for endometritis
Oxytocin (ecbolic agent)
Uterine lavage with saline or Hartmans (clean but not sterile)
3 methods to treat endometritis infection
Intrauterine antibiotics
Antibiofilm agents (H2O2, EDTA)
Lavage
2 indications for uterine lavage
Prevention of endometritis (lavage with penicillin during oestrus)
Used for culture and cytology
Endometrial V lymphatic cysts
Endometrial cysts <10mm
Lymphatic cysts >10mm
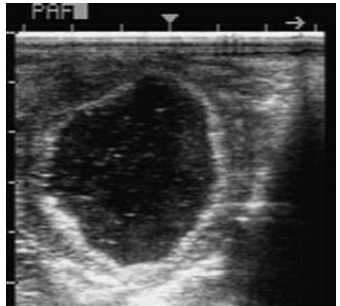
What is this in the ovary and what is it caused by? (2)
AHF (anovulatory haemorrhagic follicle)
Anechoic, irregular wall, ‘snowball’ fibrin speck effect
Idiopathic lack of LH surge → failure to progress ovulation
(some suggest PGF2a treatment but most eventually regress with time to return to normal cycling)
What does the contralateral ovary look like in AHF and granulosa theca cell tumour?
AHF → contralateral ovary normal
Tumour → produces hormones → -ve feedback → contralateral ovary smaller
4 signs of granulosa theca cell tumour
Hormone producing benign tumour:
Locally enlarged - discomfort
Inferfility
Extreme aggression
Nymphomania
Most sensitive assay for granulosa theca cell tumour
Elevated AMH
2 most common causes of foetal loss after 6+ month gestation
Excessive twisting of umbilical cord (long in horse)
does not predispose subsequent pregnancies
Placentitis
3 signs of chronic placentitis during pregnancy
(acute - mare aborts with no signs)
Chronic
vulval discharge
premature lactation (running milk)
Preliminary foaling signs (e.g. softening of pelvic ligaments
What is CTUP and how thick should it be? What does increased and reduced CTUP mean?
CTUP = combined thickness of uterus + placenta
1+ gestational age in months (e.g. 7 month gestation = 8mm)
Increased = placentitis
Reduced = placental insufficiency
2 types of antibiotic treatment for placentitis
Need to cross placenta:
Penicillin + gentamicin
Sulfonamides + trimethoprim
First pathogen assumed when abortion is seen
Equine herpesvirus
3 pathological signs of EHV
(only definitive diagnosis is PCR)
Jaundiced mucous membranes
Increased peritoneal and pleural fluid
White or yellow pinpoint liver lesions
What do red, yellow and green groups mean in terms of EHV?
Red = affected
Yellow = in contact
Green = safe geographical distance away (since EHV is respiratory and spread via aerosols)
When should EHV vaccinations be given to in-foal mares?
5, 7, 9 months of gestation
Why do equine cryptorchidism cases always need to be castrated?
Behaviour and neoplasia risk
What does a horse being cut proud mean?
Incomplete castration (often juvie or undeveloped testicle when castrated) → make testosterone
3 causes of paraphimosis + priapism
Paraphimosis → inability to retract penis into prepuce
Secondary to trauma and oedema
Pudendal nerve damage
Acepromazine
3 signs of paraphimosis + priapism
Oedema + increased weight → fatigued retractor muscle
Swelling → venous and lymphatic drainage impaired
Exposure of penis → tauma, infection, cellulitis → fibrosis and loss of erectile function
3 treatments for paraphimosis and priapism
Reduce oedema
Replace penis (if possible) - pursestring suture on sheath
Long term → retractor muscle too fatigued to keep it in: amputation, salvage procedure, perineal urethrostomy