Blood Banking Exam 4 (draft)
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
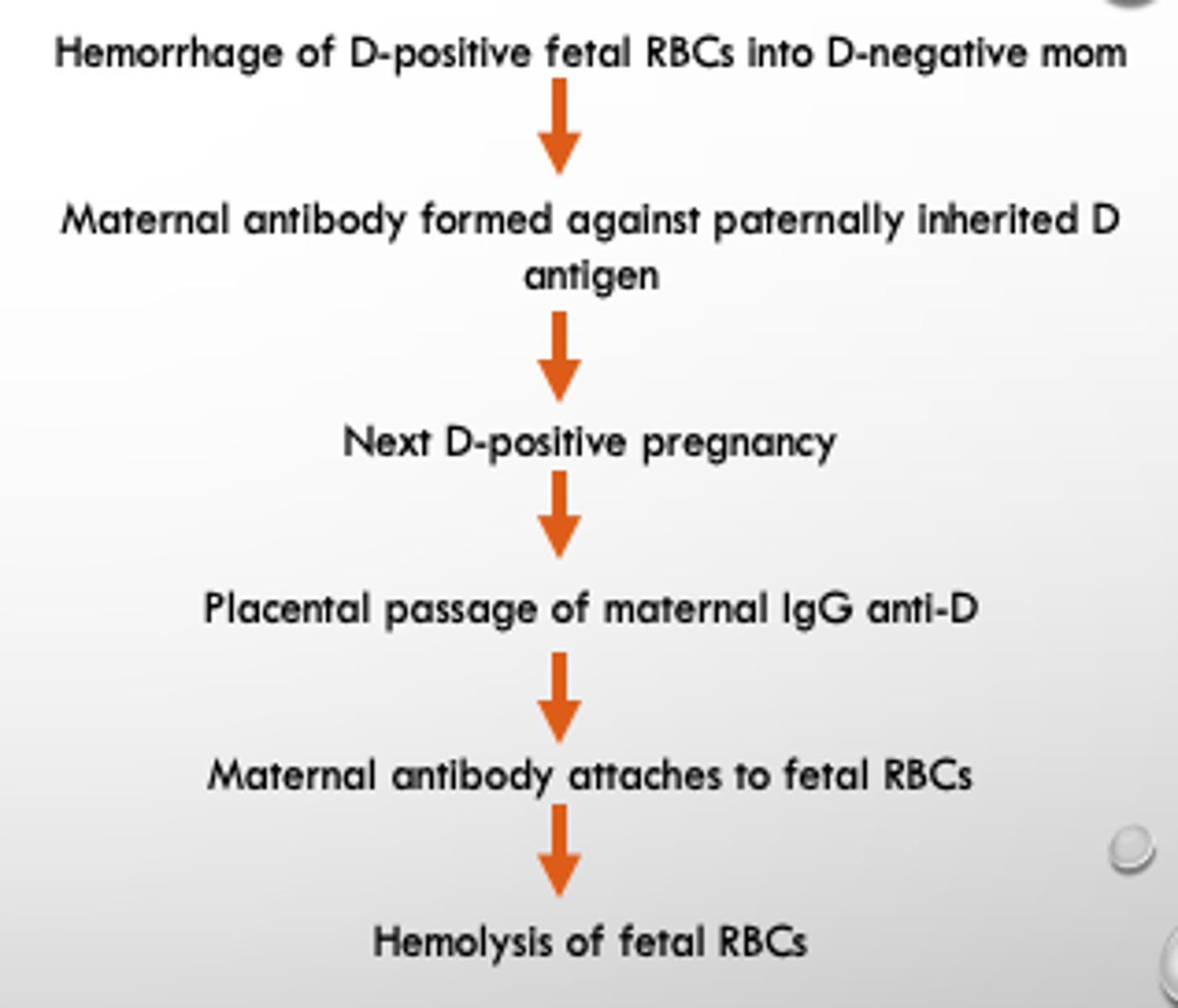
What is HDFN?
is the destruction of the red blood cells of a fetus and neonates by antibodies produced by the mother
What is RhIg?
a concentrated Human Derived anti-D IgG
What size doses does RhIg come in the US?
50 ug dose and 300 ug dose
HDF Etiology
What is the significance of anti-K in HDFN?
K and other Kell BGS antigens are present on immature erythroid cells in the BM, so if anti-K is present, severe anemia can occur
When a mother is ABO incompatible with the fetus, the incidence of detectable fetomaternal hemorrhage is decreased. WHY?
This is because any fetal cells that leak into the maternal circulation are rapidly destroyed by potent maternal anti-A and/or anti-B, reducing the likelihood of maternal exposure to the D antigen.
ABO incompatibility can also protect against Rh immunization. WHY?
If the fetal red cells are ABO incompatible with maternal anti-A anti-B, they are immediately agglutinated and hemolyzed in the uterine sinuses so that the Rh antigen is not available to provide the antigenic stimulus.
Severe anemia and hypoproteinemia lead to high output cardiac failure with generalized edema, anemia, effusions, and ascites. A condition known as _______________
Hydrops fetalis
What happens to the pathogenicity of HDFN post delivery?
•Rate of RBC destruction decreases since no additional maternal antibody is entering fetal circulation
•Antibody is distributed both extravascularly and intravascularly
At what phase are we most concerned with when performing an ABSC on a future mother?
AHG (IgG detection)
- should also use enhancement media such as LISS or PeG
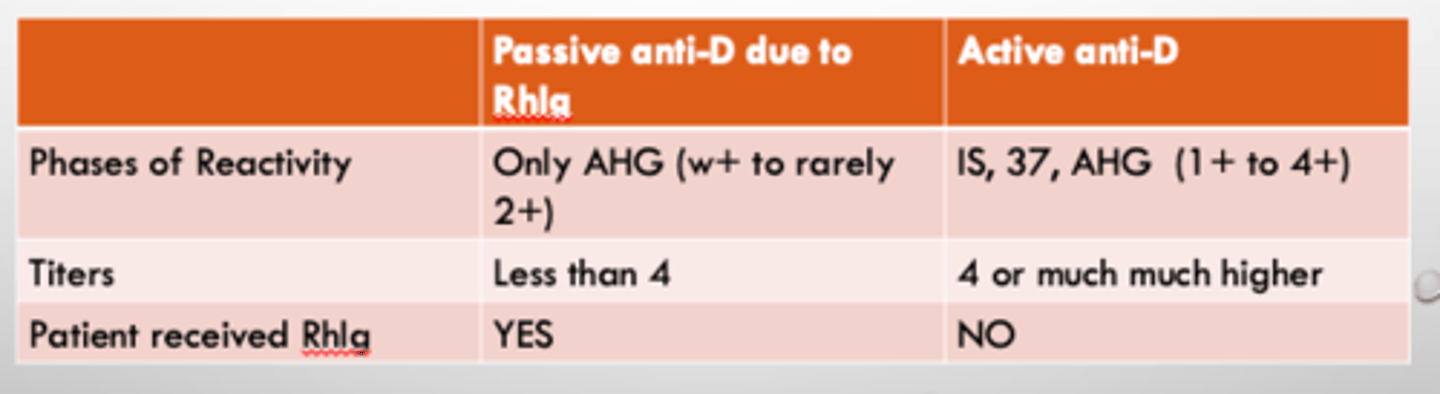
If a mother is Rh negative and she has a positive ABSC in her third trimester and the antibody is anti-D, do you need to distinguish passive anti-D (due to RhIg administration) from active anti-D?
yes
What are serological differences we see between Passive anti-D and Active anti-D?
Can a titer by itself predict the severity of HDFN?
A TITER BY ITSELF CANNOT PREDICT SEVERITY OF HDFN, a continuous and repeated titer below critical values through out pregnancy can predict a mild or unaffected fetus.
What initial titer value is considered critical?
an initial titer of 16 is considered critical and a follow up titer should be performed at 18-20 weeks gestation
If fetal Hgb is less than 10 g/dL =
intrauterine transfusion
What are the requirements for an intrauterine transfusion?
- Type O (typically O neg)
- Antigen negative for corresponding antibody
- Less than 7 days post donation (fresh)
- XM compatible with mom's plasma
- CMV seronegative
- HgbS negative
- Irradiated
- Volume reduced or washed to obtain high hematocrit (80-85%)
When is phototherapy used?
Phototherapy at 460-490 nm is used to change the unconjugated bilirubin into isomers that are less lipophilic and less toxic to the brain
When is Intravenous Immune Globulin (IVIG) used?
IVIG is used to compete with maternal antibodies for Fc receptors on the macrophage, thus reducing hemolysis
Why is a weak D test done when a mom has a positive fetal bleed screen?
Because if mom is weak D positive, it could cause a false positive FBS
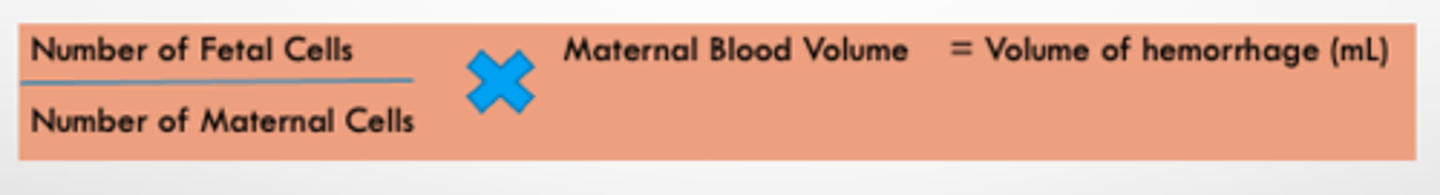
The results from which test are used to determine the recommended the number of doses of RhIg?
Kleihauer Betke
What is the equation used to determine RhIg dosage?
What dose of RhIg is given at less than 12 weeks?
micro dose (50ug)
What dose of RhIg is given at between 12 and 20 weeks?
one full dose (300ug)
What dose of RhIg is given at greater that 20 weeks?
AT LEAST one full dose (maybe more)
What dose of RhIg is given at 28 weeks?
a prophylactic dose
What dose of RhIg is given post delivery?
AT LEAST one full dose (maybe more)
ABO HDFN is nearly always limited to _____ or _____ infants of group O mothers and can occur in the first pregnancy
A or B
What is an ABO discrepancy?
an unexpected reaction in either the forward, reverse, or both in an ABO typing
What are causes of ABO discrepancy?
- Misidentification of the patient (pre-analytical)
- Technical (tech, reagents, equipment; analytical)
- Incorrect entry (post-analytical)
The most common ABO discrepancies occur in the patients _______, this will be seen when doing a _________
plasma / back type
What patient history is useful in looking into ABO discrepancies?
- Age
- Diagnosis
- Transfusion hx
- Is the patient a bone marrow transplant recipient?
- Medications
What does the short cold panel tell you?
- Suspected subgroup
- Suspected interfering antibody
What are the most common cold allo antibodies?
Anti-M
Anti-N
Anti-P1
What is acquired B antigen?
If the patient has bacteremia associated with a leaky gut or bowel, they are a young kid, and they were originally a type A, and now have an extra reaction with the B antisera in the front type ...... The gut/bowel bacteria have an enzyme capable of de-acytelating the N-acetylgalactosamine in group A individuals, leaving behind galactosamine which closely resembles L-galactose in type B and cross reacts with your B sera (if poly-clonal).
What can titrations be used for?
- monitor maternal antibody levels in HDN
- to characterize HTLA
What antigens are enhanced by enzymes?
Rh, ABO, I, Le, P, Kidd.
What antigens are resistant to enzymes?
Kell, Lutheran, s, U
What antigens are sensitive/destroyed to enzymes?
Duffy, MN, sometimes S
How do enzymes work in blood bank?
Proteolytic enzymes like papain and ficin cleave polypeptides containing negatively charged sialic acid molecules from poly saccharides
--> reduces cell charge and zeta potential
What are some examples of enzyme applications?
•Enzymes can be used to reduce activity of antibodies to see what's underneath
•Destroy antigens to create purposefully non-reactive cells
•Enhance weakly reacting antibodies
•Enhance unwanted cold reactions (anti-I, or -H) ----> Typically read at AHG
What are the sulfhydryl reagents used?
DTT, 2-ME, AET, ZZAP, Chloroquin
DTT, 2-ME, AET all destroy
Kell BGS, Lutheran BGS, and LW
ZZAP destroys
all of the DTT destroyed antigens plus all of the enzyme destroyed antigens.
ZZAP is typically used for what?
to pretreat cells for an auto or allo adsorption.
What happens to a patients cells when they are treated with Chloroquin? When is it used?
Chloroquin can remove bound IgG by breaking the disulfide bonds of the IgG or IgM molecules and therefore making the DAT negative.
If the DAT is negative with treated cells, the phenotyping seras that are ran in an IAT can then be ran.
When are elutions done?
Eluates are performed when there is a positive DAT IgG to see if the antibodies coating the patient's cells have a blood bank specificity.
Do you use enhancement media with elutions?
no
How do elutions work?
dissociate antigen-antibody complexes, releasing the intact antibody into the fluid or "eluate". This "eluate" can be tested like patient plasma.
An eluate that is panreactive is most likely
a warm auto antibody (WAA)
An eluate that is negative often indicates
drug induced positive DAT
What are the elution chemicals that are used?
- Chloroquine Diphosphate
- EGA
- Gamma Elu-Kit elution (most common)
Elution techniques in combination with adsorption studies are useful for:
-Separating multiple antibodies
-Clarification of "compound" specificities like anti-G
-Detecting the presence of weak antigens on the red cell = adsorption and elution technique
If there is reactivity in the eluate, an antibody can be identified using..
the standard ABID method
If the eluate is negative, the source of the positive DAT may have been...
drug related
If the eluate is panreactive, we could be looking at....
multiple antibodies, WAA, or an antibody towards a high frequency antigen
What are some sources of error in a eluate?
•Not testing the last wash. Possibly leaving unbound antibody = improper washing
•Left over red cell stroma or debris can make reading and grading tricky
•If your eluate is red, the red cells are fragile to begin with, you might get hemolysis
What do you need to perform if your auto-control is positive in your ABID panel?
DAT
Can you still perform rule outs if you have negative cells on the panel and the auto control is positive?
YES.
The antibody coating the cells in the auto-control may show specificity to a particular antigen. Remember, the auto control might not just contain patient cells but donor cells as well. An antibody might be coating the donor cells.
What is adsorption?
•Antibody(ies) can be removed from serum by adsorbing them onto red cells that express the corresponding antigen
•After the antibody attaches to the red cell antigens, the sample will be spun down and serum will be separated from the cells.
What can adsorbed serum be used for?
to further identify or isolate antibodies
What are some adsorption techniques?
•Used to remove cold or warm autoantibodies that interfere with the identification of clinically significant antibodies
•Separate multiple antibodies by adsorbing with red cells of a known specific phenotype
•Verify antigen status if the antigen is weakly expressed and direct testing isn't working
•Remove isoagglutinins or other contaminating antibodies from specific anti-sera such as those used for phenotyping
When is the prewarming technique used?
to eliminate interfering cold reactive antibodies from the test system so that we can identify underlying warm reactive antibodies.
What it the neutralizing technique?
Blood group antigens that exist in soluble forms in body fluids can be used to neutralize serum antibodies so that other underlying alloantibodies can be revealed
Can neutralization be used to characterize a suspected antibody?
yes
What neutralizes Anti-Lea, -Leb?
Lewis substance from human saliva
What neutralizes Anti-P, -P1?
P1 substance from pigeon ehh whites or hydatid cyst fluid or liver flukes
What neutralizes Anti-Sda?
Sda substance found in human urine
What neutralizes Anti-Ch/Rg?
Chido Rogers substance found in human plasma
What are titers most useful for?
-Monitoring the quantity of antibody in a woman's serum during pregnancy
-To characterize HTLA antibodies (in which case these are usually read to the microscopic end point)
What is the weak D phenotype?
a quantitative reduction in the amount of D antigen on a RBS
---- no antibody made/normal D epitope -----
What is the partial D phenotype?
a qualitative change in the expression of the D epitope or missing parts of the D epitope
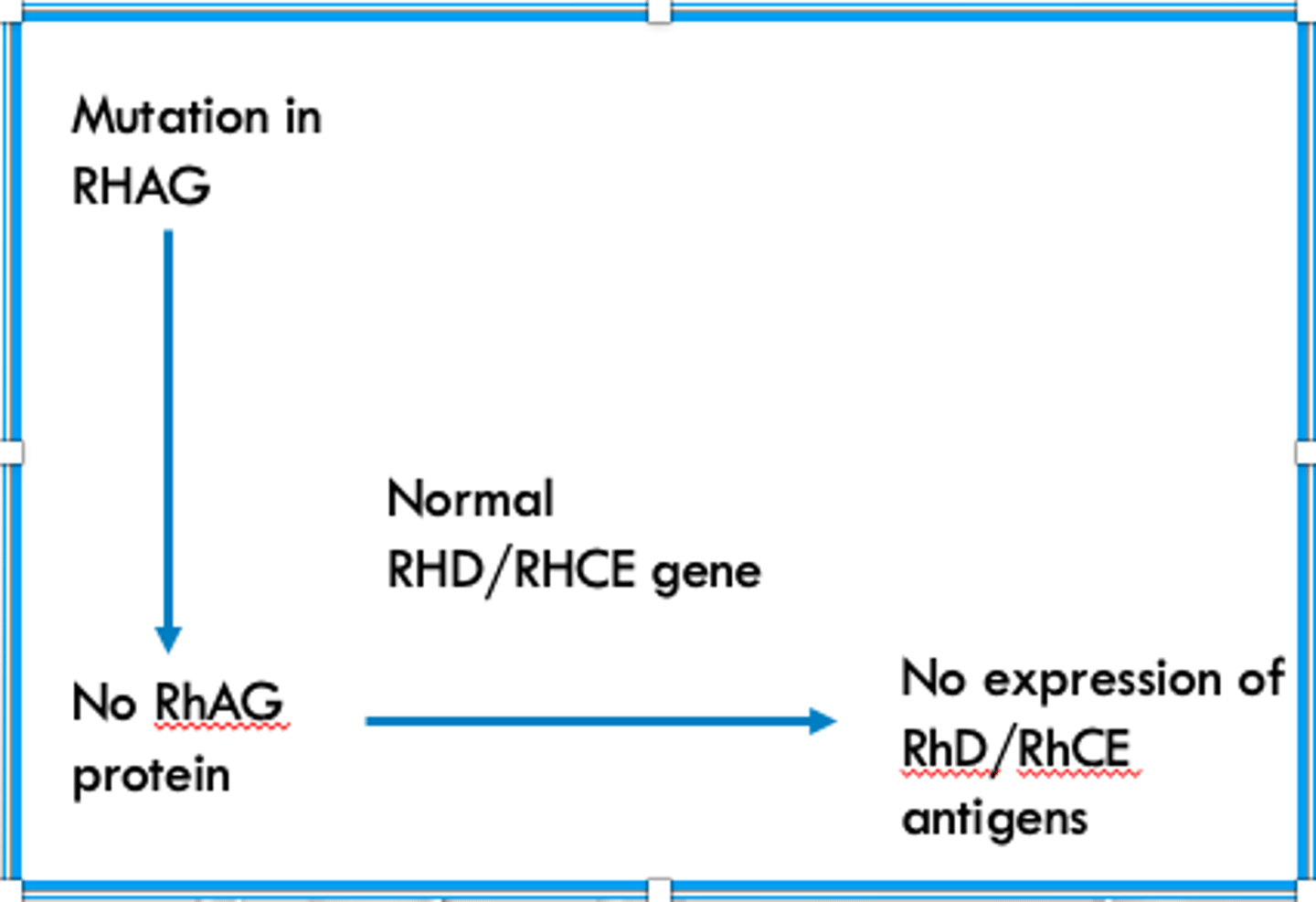
What happens in the "regulator pathway" that forms a Rh Null phenotype?
There is a mutation in the RHAG gene and/or RhAG protein, so even though the RHD and RHCE genes are normal their proteins do no get expressed
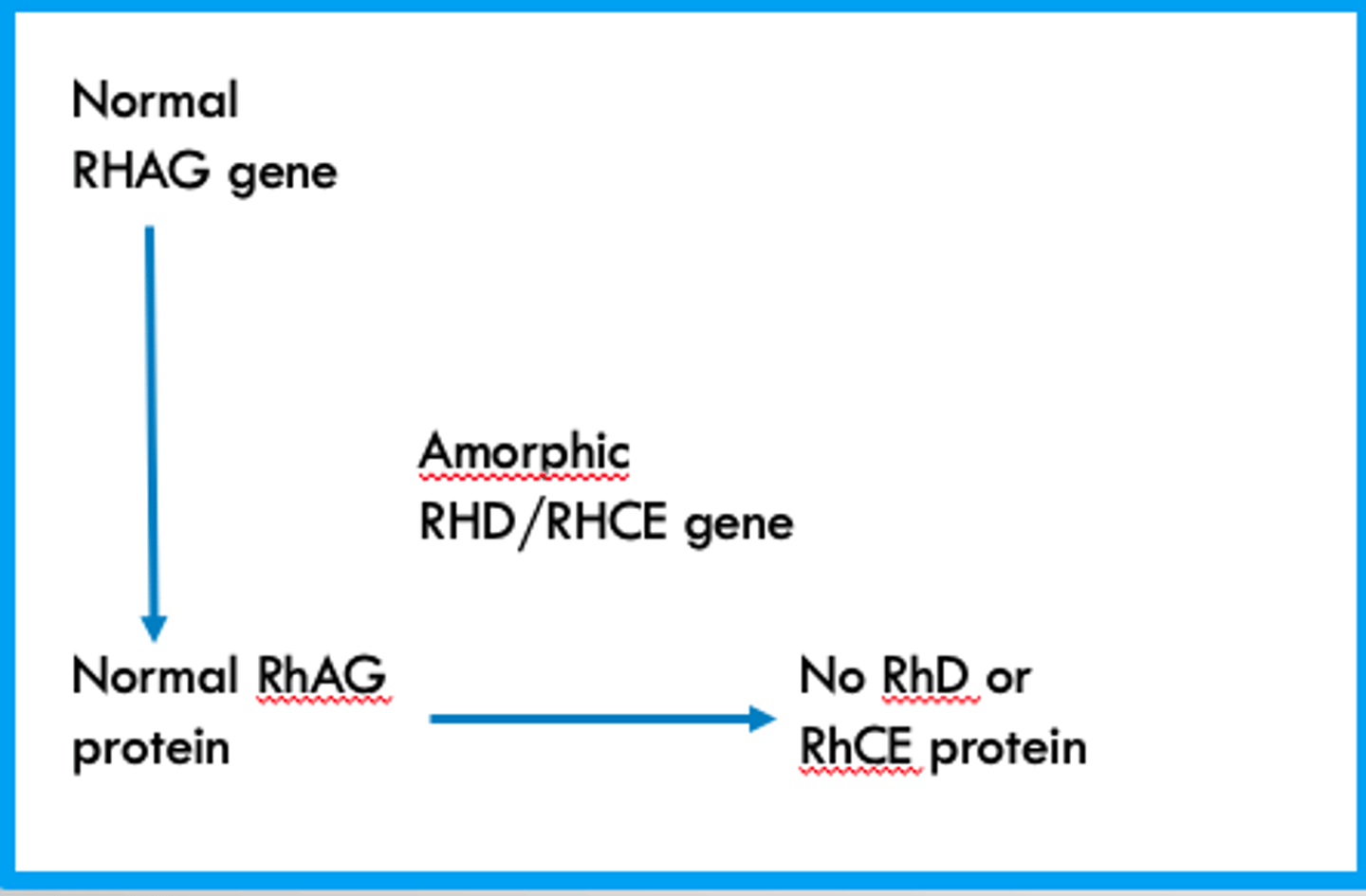
What happens in the "amorph pathway" that forms a Rh Null phenotype?
The RHAG gene and Protein are normal and functioning correctly but a mutation in the RHD/RHCE genes results in their proteins nor being expressed
weak expression of Kell BGS antigens dues to point mutations in the KEL gene
Kmod
weak expression of Kell BGS dues to the lack of XK protein
McLeod phenotype
What null phenotype can be found in Polynesians and Pacific Islanders?
JK (a-b-)
What null phenotype is found in the African American population? What evolutionary advantage comes with it?
Fy (a-b-)
Resistant to Plasmodium vivax
What is the F antigen?
- present when c and e antigen are present (r and R0)
- anti-f is often seen with anti-e and anti-c
What is the G antigen?
Present when either D or C are present
What is the clinical significance of G antibodies?
•Patients with anti-G should receive units negative for D and C antigens
•Pregnant women with anti-D and -C should be investigated for anti-G. If it is only anti-G, they are still candidates for RhIg.
Which antigens have IgM antibodies?
ABO, H, Lewis, Lu, MN
Which antigens have IgG antibodies?
Fy, Kell, Kidd, MN, Rh
Which Duffy is most common in white people?
Fy (a+b+)
Is the H antigen a high frequency antigen?
yes >99.99%
What are the most common haplotypes of the Kell BGS?
k, Kpb, Jsb
If a person is JK null, they can form _________ which will react with any cell that possesses a JK antigen
α-JK3
How can you differentiate JK null RBC's from normal RBC's?
By using 2M Urea, JK null RBC's will not lyse like normal RBC's
Why do "Kidd's Kill"?
The α-JK3 are known for falling below detectable level and then responding with a very strong anmnestic response
Pregnant women can transiently type as
Le(a-b-)
What is the most common Lewis antigen formed?
Le(a-b+)
Which Lutheran antigen is high frequency?
Lu(a-b+)
Which antigens can absorb reversibly onto RBC's?
Lewis
_______ haplotype is 2x as likely as the ________ haplotype
MS / NS
R1 =
DCe
R2 =
DcE
R0 =
Dce
Rz =
DCE
r =
dce
r' =
dCe
r" =
dcE