Calcium, phosphorous and magnesium imbalances. Vitamin D disturbances in relation to osteopathies, tetany, and metabolic disorders of dairy cows. Hypo/hyperparathyroidism
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
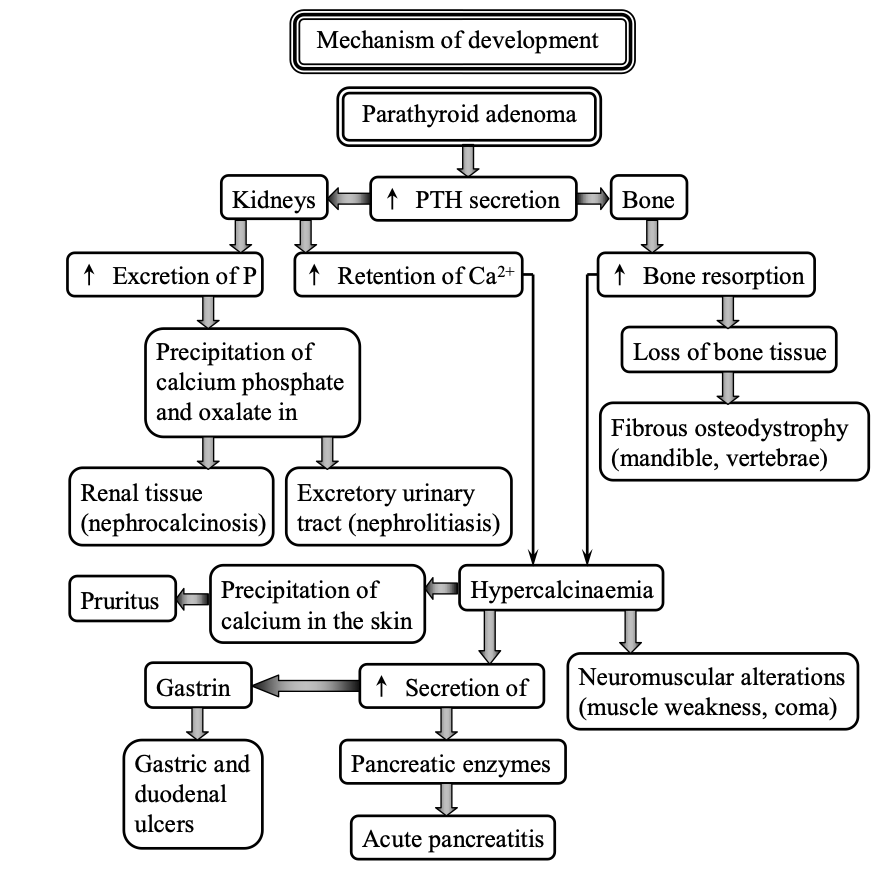
Primary hyperparathyroidism
· Characterized by excessive secretion of PTH which causes hypercalcemia, muscle weakness, demineralization and fracture of bone and excessive resorption of bone matrix produces increase in excretion of hydroxyproline by urine
· Mechanism of development:
o Parathyroid adenoma leads to increased secretion of PTH, which stimulate kidneys to increase excretion of P and increase retention of Ca2+. PTH stimulate bone to increase bone resorption, leading to loss of bone tissue and fibrous osteodystrophy (mandible, vertebra)
o Excretion of P leads to precipitation of calcium phosphate and oxalate in renal tissue (nephrocalcinosis), and excretory urinary tract (nephrolithiasis)
o Increased retension of Ca2+ together with increased bone resorption leads to hyoercalcinemia
o Hypercalcinemia causes neuromuscular alterations (muscle weakness, coma), precipitation of Ca in the skin (pruritus), and increased secretion of gastrin (gastric and duodenal ulcers) and pancreatic enzymes (acute pancreatitis)
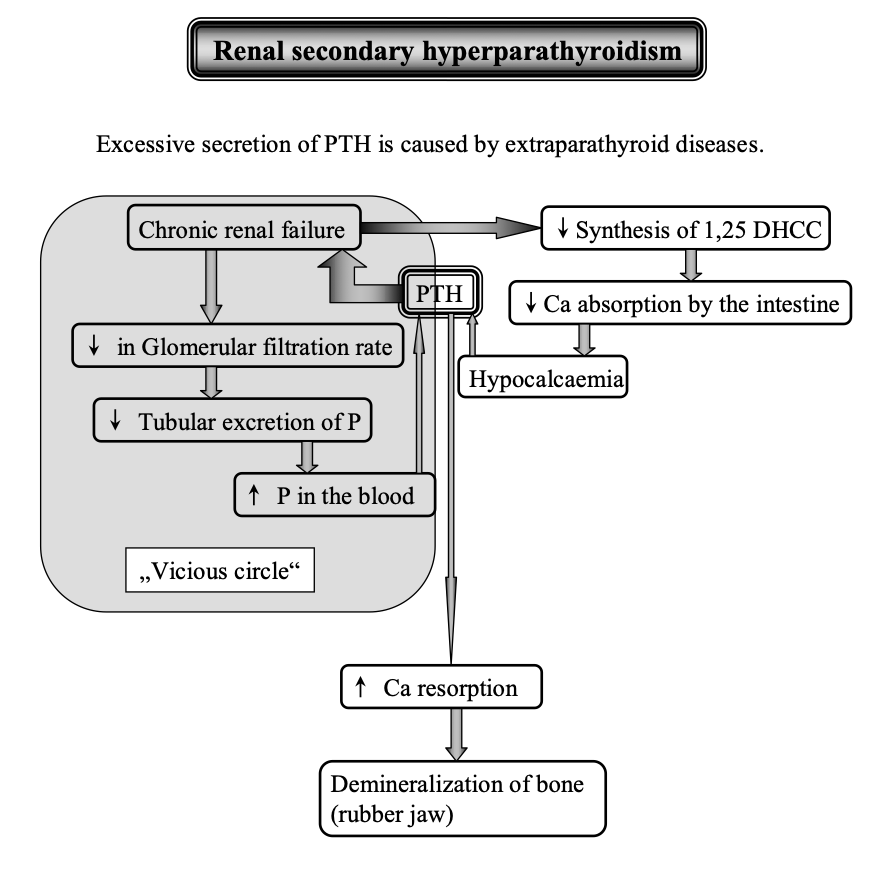
Secondary hyperparathyroid disease, mechanism
· Mechanism of development:
Renal secondary hyperparathyroidism
o Chronic renal failure: decrease in glomerular filtration rate leads to decreased tubular excretion of P, resulting in increased P in the blood
o This stimulate the release of PTH which affects the chronic renal failure, forming “Vicious circle”
o Chronic renal failure leads to decreased synthesis of 1,25 DHCC, which causes decreased Ca absorption by the intestine, resulting in hypocalcemia
o Hypocalcemia stimulate the release of more PTH
o PTH stimulate increased Ca resorption leading to demineralization of bone (rubber jaw)
Nutritional secondary hyperparathyroidism
occurs in young growing animals or adult horses, cat, domestic birds or zoo animals kept on unbalanced diet and is characterized by a cessation of growth, bone resorption and fibrous osteodystrophy
o Dog, cat: diet with low Ca2+ leads to hypocalcemia, leading to increased PTH secretion, causing increased bone resorption and demineralization of bones
o Horse, domestic birds: diet with high P and normal Ca content leads to hyperphosphatemia, leading to increased secretion of PTH
Differences between osteomalacia and osteoporosis
· In osteomalacia, there is demineralisation of bone, abnormal composition of the bone making the bone soft and weak. Metabolic disorder. Osteomalacia is caused by a decrease of the mineral component of the bone.
· In osteoporosis, there is low bone density, and the bone mass disappear over time, but there is normal composition of the bone. This makes the bone weak and brittle, more susceptible to fracture. Disorder of bone matrix formation, often caused by hormonal disorders like hyperthyroidism and drug therapy. Osteoporosis is caused by excessive loss of the bone mass (mineral and organic).
· Difference: osteomalacia involves decrease of anorganic fraction of bones, while osteoporosis involves excessive loss of both organic and anorganic fraction of bone.
Difference between osteomalacia and rickets
· They have similar etiology: decrease of the inorganic components of the bone
· Rickets is juvenile osteomalacia
· Both have decrease in P, Ca, vit D, occurrence of acidosis and supply – demand imbalance
· Osteomalacia develops in adult (mature) animals, while rickets develop in young (immature) animals
· Consequences in osteomalacia is increased fractures but no bone deformity
· Consequences in rickets is increased bone deformity but no fractures
Characterize rickets and list 3 causes
· Metabolic disease of bone of the young growing animals, characterized by defective calcification of growing bone. There is a failure of calcification with persistence of hypertrophic cartilage and enlargement of epiphysis of long bone and the costochondral junctions
· Causes:
o insufficient solar irradiation
o renal disorders: renal 1-alfa-hydroxylase deficiency, vit D receptor defect and decrease reabsorption of P by the kidneys
· Clinical signs: stiffness of gait, enlargement of the limb joints and costochondral junctions, abnormal curvature of the long bone, rachitic rosary
· Biochemical findings: increased ALP, lack of density of affected bones compared to normal ones..
Development and causes of osteomalacia
· Osteomalacia is a metabolic disease of bone of mature animals characterized by decrease of the mineral component of the bone. It is rickets of adult animals.
· Development:
o Pregnancy, lactation and endogenous metabolism leads to increased resorption of bone minerals
o This results in excessive demineralization, resulting in weakness and fracture
· Causes:
o Lack of vit D due to insufficient solar irradiation of animals, insufficient content of vit D in diet, impaired vit D absorption, or chronic liver disease
o Chronic renal acidosis
o Renal osteomalacia due to increased reabsorption of phosphorous
o Interference with phosphorous absorption (AI)
Consequences of Ca, P, and vitD deficiency
· Calcium deficiency caused by high cereal content in diet and by keeping animals indoor
· Phosphorous deficiency caused by excessive Ca, Al, and Fe content in soil, heavy leaching by rain, the high content of phytates in cereal grains
· Vit D deficiency caused by housing of animals indoor for a long period, xcessive intake of beta-carotene or vitamin A, disorders of the kidney, alteration of the Ca:P ratio (wider than 1:1 to 2:1)
· Consequences:
o Disorders of growth and appetite
o Disorders of reproduction
o Disorders of milk production
o Disorders of bone
Characterize and cause of osteoporosis/name and explain 4 causes of osteoporosis
· Osteoporosis is characterized by excessive loss of the bone mass (mineral and organic) and may produce weakness, stiffness gait, pain in bones and joints and fractures.
· Causes:
o Insufficient stimulation of osteoblasts in:
- prolonged immobilization (immobilization osteoporosis)
- estrogen deficiency
o Disorders of bone matrix formation in:
- Absolute protein deficiency (starvation, malnutrition)
- Relative protein deficiency (increased demand for protein in pregnancy, lactation, endogenous metabolism)
- Glucocorticoids excess (cushing´s syndrome), prolonged glucocorticoid therapy -> increase catabolism of proteins
- Hyperthyroidism: rate of resorption of the bone exceeds the rate of bone formation
- Prolonged heparin therapy: decreased synthesis and increased decomposition of collagen
- Deficiency of calcium due to unbalanced diet or decreased absorption by intestine
Pathological consequences of hypophosphatemia
· Hypophosphatemia is the condition of lowered phosphate concentration in the plasma
· Primary causes of hypophosphatemia: excessive Ca, Al, Fe content in soil (reduces the availability of phosphorous in plants), and the high content of phytates in cereals and soil (phosphorous is organically bound to phytic acid in these feedstuffs, monogastric animals lack enzyme phytase which is present in rumen)
· Secondary causes of hypophosphatemia: heavy leaching by rain, decreased intestinal absorption, primary hyperparathyroidism, milk fever, hyperinsulinism, respiratory alkalosis
· Pathological consequences:
o Reduced capacity of oxygen transport by RBCs transport and release of oxygen are associated with 2,3 DPG and ATP. When phosphate levels are low, 2,3 DPG and ATP levels become low and diminish the release of oxygen to the tissues. OxyHb curve shifts to the left, hypoxia and bradycardia may occur
o Disturbances in energy metabolism: nerve and muscle metabolism impairment, irritability, confusions, coma
o Bone resorption
Hyperphosphatemia
· Elevated serum phosphate levels
· Causes: exogenous or endogenous addition of phosphorous to ECF, secondary renal hyperparathyroidism, cell destruction associated with treatment of metastatic tumors with chemotherapy and release large amounts of phosphate in the serum, and long-term use phosphate containing enemas or laxatives
· Pathological consequences: symptoms are similar to signs of hypocalcemia
Hypercalcemia
· Pathological condition characterized by calcium excess in the plasma
· Mechanisms and causes:
o Suppressed Ca excretion by the kidneys
o Hypervitaminosis D for prevention of parturient paresis in cattle, consumption of vit D containing rodenticides in small animals, enzootic calcinosis in grazing animals
o Primary hyperparathyroidism, pseudohypoparathyroidism
o Secretion of substances with PTH like effects by malignant tumors
· Pathophysiological consequences:
o Since serum Ca levels are increased, a greater amount of Ca is also contained inside cells
o The treshold potential becomes more positive, and the cell membrane becomes refractory to depolarization
o Thus many symptoms are related to loss of cell membrane excitability, such as fatigue, weakness, lethargy, anorexia, nauzea and ileus.
o Nephrolithiasis (renal stones) as precipitates of calcium salts
Causes of hypocalcemia
· Lowered calcium concentration in plasma
· Primary causes: rare
· Secondary causes:
o Diet high in cereal or grass hay which contains little calcium, grains which contains high amount of phosphorous (Excessive amounts of phosphorpus also bind with calcium, so neither mineral is absorbed)
o Vitamin D deficiency
o Dietary oxalates combines with calcium to form insoluble salt
o Blood transfusion – citrate solution
o The Ca:P ration wider than 1:1 or 1:2
o Pancreatitis – FFA combines with Ca soap
o Kidney failure
o Neoplasmic bone metastasis
o Removal of parathyroid gland
o Metabolic or respiratory alkalosis
· Pathological consequences: an increase in neuromuscular excitability, confusion, paraesthesia, hyperreflexia, convulsions, tetany
Milk fever
· Metabolic disease occurring in older high-producing dairy cow within 48-72h after parturition
· Clinical symptoms: hypocalcemia, hypophosphatemia, excitation, hypersensitivity, general muscular weakness, circulatory failure, depression, unconsciousness and paresis
· Causes: high-calcium diet and low phosphorous diet in the dry period, calcium deficient diet, excessive Ca and P output in the foetal development, in late gestation, and/or Ca and P output in the colostrum
· 1. When a cow is fed a high Ca diet in last weeks of pregnancy, it causes hypercalcemia. This leads to increase release of calcitonin, and decreased release of parathyroid hormone (PTH), increased 24,25 DHCC in the kidneys
· 24,25 DHCC in the kidneys cause decreased Ca absorption by intestine
· Decreased PTH leads to less active osteoclasts and osteocytes
· At calving and lactation, excessive loss of Ca in the colostrum and for fetal development in older cows, leads to hypocalcemia, decreased Ca mobilization from bones, decreased Ca absorption by intestine and decreased RR motility
· Hypocalcemia develop and there is a delay in the increase of PTH, and increase amount of calcitonin, cortilsol, osteoclasts
· This result in excitement, tetany with hypersensitivity, muscle tremor, sternal recumbency, ruminal stasis, cessation of respiration
· 2. When dairy cow is fed on a low calcium diet in last weeks of pregnancy, this leads to a mild hypocalcemia, causing increase of PTH, and 1,25 DHCC, increase Ca mobilization from bone, Ca reabsorption by kidneys, and Ca absorption by intestine at calving and lactation. This leads to excessive loss of Ca in the colostrum and for fetal development in older cows. Slow mobilization of Ca from bone and Ca absorption by the intestine leads to decreased RR motility, resulting in milk fever
Hypomagnesaemic tetany (grass tetany, wheat posture poisoning)
· Hypomagnasemic tetany is a highly fatal disease of ruminants. It is characterized by hypomagnesemia and sometimes by hypocalcemia
· Clinical signs: tonic-clonic muscular spasms and convulsions, death due to respiratory failure
· Acute lactation tetany: a sudden decline of Mg blood concentration in several hours to days. Ingestion of pastures that have insufficient magnesium to meet dietary requirements. Grass-dominant pasture in the spring (spring tetany).
· Chronic tetany:
o Tetany of calves: calves are fed of whole milk for abnormal length of time with insufficient supplementation of Mg + loss of Mg by diarrhea
o Stable tetany (during winter period): in housed high-producing cattle being fed on conserved feed prepared from pastures with marginal Mg concentration causing insufficient Mg to meet dietary requirements due to high lactation drain