week 6: Major Histocompatibility complex (MHC) and antigen processing/presentation
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
what is the MHC?
describe the genes
expression
protein product roles
Tightly linked cluster of genes
Expressed in all mammals studied
Protein products
play role in recognition:
cell-cell
self/nonself
present antigens to T cells
essential for normal immune response
implications for disease susceptibility
what do class I and class II MHC do?
classical MHCs
closely related membrane-bound glycoproteins
form stable complexes with peptides
antigen presentation
what is class III
group of unrelated proteins, some may have immune functions
compare the structures of the MHC class I and class II molecules
MHC class I
has one alpha chain with 3 domains (alpha is variable)
has one beta chain
MHC class II
has one alpha chain with 2 domains
has one beta chain with 2 domains
alpha domain 1 and beta domain one are variable
*the peptide-binding grooves are where Ag’s will be bound, these grooves differ between MHC1 and MHC2 because their corresponding peptides differ
*alpha gene is encoded in MHC locus and varies from person to person
*the Beta2 microglobulin gene is outside of MHC locus, less variable, more for structure

compare the peptides that bind in the peptide binding groove in MHC class I and MHC class 2
class I: peptides 8 - 10 amino acids
peptides have particular anchor residues (usually hydrophobic) at termini (beginning and end of amino acid chain)
ex. glycine, proline, leucine, isoleucine, tyrosine, valine
class II: peptides 13 - 18 amino acids
because the groove is more open ended so larger peptides can bind
compare which cells express class I vs class 2 MHC and why this is necessary
Class I molecules
glycoproteins on surface of almost all nucleated cells (cells that need to be deleted by Tc)
presentation to cytotoxic T cells (TC)
Class II molecules
glycoproteins expressed mainly on antigen presenting cells (macs, B, dendritic) → cells that help helper T cells
present to helper T cells (TH)
*note: APCs also express class 1
what else is MHC called in humans?
what chromosome is it found on?
human leukocyte antigen (HLA)
found on chromosome 6
what else is MHC called in mice?
what chromosome is it found on?
MHC called H2 complex
on chromosome 17
haplotypes
haploid genotype
specific combination of linked alleles in a cluster of related genes
one haplotype inherited from each parent
allelic variation (denoted as a superscript)
what are the MHC class 1 genes?
class 2?
class 1: alpha chains: K, D, L; constant beta chain
class 2: alpha chains: E, A; constant beta chain (a heterozygote can express any alpha chain with any beta chain - can mix and match mom and dad)
explain how MHC genes are inherited
how are they expressed?
mouse strains
inherited as haloptypes because they are so tightly linked
MHC is highly polymorphic (vary in population) and very tightly linked (0.5% crossover frequency) → inherit one maternal haplotype and one paternal haplotype (basically never get recombination)
MHC alleles are codominantly expressed (express the genes from both mom and dad)
Mouse strains
some have been inbred with particular MHC haplotypes
Syngeneic
identical at all genetic loci
Congenic:
genetically identical except at a single genetic locus or region
any phenotypic differences can thus be attributed to the region that is different
strains made by series of specific crosses
MHC congenic:
identical at all loci except MHC
e.g. strain A.B (genetic background of strain A with MHC of strain B)
recombinant strains: differences at only a few genes within MHC
describe the genes of MHC
introns/exons?
alleles?
Separate exons encode the different regions on the class I and class II molecules
Polymorphism
hundreds of different allelic variants
how many different class 1 and class 2 molecules can each human have?
Each human individual
up to 6 different class I molecules
up to 12 different class II molecules
explain MHC diversity
MHC considered polygenic
genes with similar but nonidentical function
High polymorphism
Sequence differences mainly in regions encoding antigen-binding domains → which allows for diff Ag binding/presentation
Implications for disease susceptibility and immune responsiveness
the more diverse, the less of a problem
describe the cellular distribution of MHC class 1
what cells express them? which express them the most? the least?
in healhty cells what do they display?
in infected cells what do they display?
on almost all nucleated cells, to varying degrees
highest on lymphocytes
low on fibroblasts, muscle, hepatocytes, neural cells
displays self-peptide in normal, healthy cells (shows the T cells what is healthy, helpful in T cell differentiation)
displays viral peptide in infected cells
expressed on thymic stromal cells for T cell education
used in T cell screening by showing the T cell the MHC is self, so don’t respond)
describe the cellular distribution of MHC class 2
what cells express them?
describe the level of their expression
expressed on
antigen presenting cells (APCs)
macrophages, dendritic cells, B cells
constitutive expression (constantly expressed)
level depends on developmental stage
thymic epithelial cells and some others if induced
helpful in T cell education/screening to show T cell self MHC
explain the hypotheses for explaining how haplotype influences immune response
Class II gene expression very important (because they present to helper T cells)
Experiments in mice showed haplotype influences response
hypotheses (possible that both are true)
determinant-selection model
different class II molecules have different abilities in binding antigen
holes-in-the-repertoire model
T cells that could bind foreign antigens that are similar to self antigens are eliminated
explain MHC and disease susceptibility
Some diseases occur more (or less) among individuals with particular haplotypes
e.g.
some autoimmune diseases
some viral infections
some allergies
some neurological disorders
regulation of MHC expression
what factors are involved
5’ promoter sequences regulate expression
associated transcription factors
Cytokines, e.g.
interferons (alpha, beta, gamma)
tumour necrosis factor
interleukin 4 (IL-4)
effect depends on cell type and developmental stage
Viral infection
some viruses can decrease MHC expression (so cell cannot present viral peptides so the virus can go undetected)
decreased expression helps virus evade system
explain the concept of self-MHC restriction of T cells
T cells recognize antigen only when presented by self-MHC
same MHC haplotype as the T cell
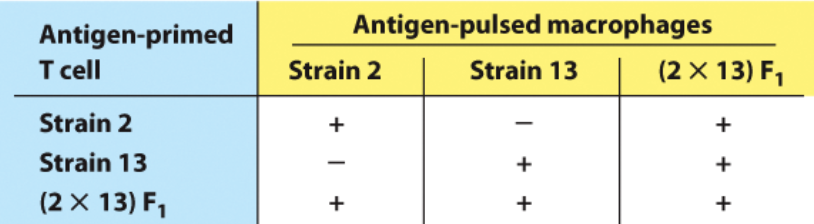
Experiment by Rosenthal and Shevach
describe the set up of the experiment (where the cells came from)
what they did
what did the results confirm?
Proliferation of TH cells
source of TH cells: lymph node cells from immunized guinea pigs
strain 2, strain 13, (2 x 13)F1
APCs: macrophages
isolated from nonimmunized guinea pigs
from strain 2, strain 13, (2 x 13)F1
“pulsed” with same antigen as used to immunized guinea pigs above
coincubation of primed T cells (trained to react to Ag) and pulsed APCs (present the Ag)
Results confirmed by repeating experiments with congenic and recombinant congenic strains
need to look at different haplotypes because talking about MHC restriction
Experiment by Rosenthal and Shevach
results
+ = helper Ts were activated and proliferated
- = helper Ts were not activated and did not proliferate
got response (+) when the helper Ts were able to recognize their specific MHC
Experiment by Zinkernagel and Doherty
describe the set up of the experiment (where the cells came from)
what they did
what did the results confirm?
looked at Cell lysis mediated by TC cells
detected by chromium-release assay (target cells were injected with radioactive chromium, if T cells lyse the cells you see chromium in the media)
TC cells: splenocytes (spleen cells) from mice immunized specific with LCM virus
target cells: LCMV-infected cells of the same or different haplotype as the T cells
results confirmed with congenic and recombinant congenic mice
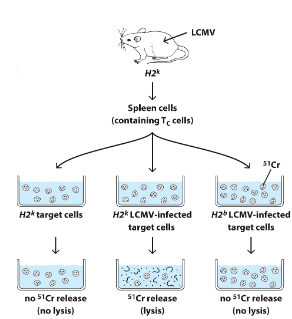
Experiment by Zinkernagel and Doherty
explain the results
no lysis because the T cells only kill infected cells
lysis because the infected cells had the correct MHC haplotype to match the T cell
no lysis because the infected cells had a different MHC haplotype
Predict whether TH-cell proliferation or CTL-mediated cytolysis of target cells will occur with the following mixtures of cells. The CD4+ TH cells are from lysozyme-primed mice and the CD8+ CTLs are from influenza-infected mice.
H-2k TH cells + lysozyme-pulsed H-2k macrophages
H-2k TH cells + lysozyme-pulsed H-2b/k macrophages
H-2k TH cells + lysozyme-pulsed H-2d macrophages
H-2k CTLs + influenza-infected H-2k macrophages
H-2k CTLs + influenza-infected H-2d macrophages
H-2d CTLs + influenza-infected H-2d/k macrophages
H-2d/k CTLs + influenza-infected H-2k macrophages
yes because helper Ts recognize MHC on macrophage
yes
no
yes
no
yes
yes
roles of APCs
Internalize antigen proteins (endocytosis)
Process the proteins into peptides
Present the peptides on MHC class II molecules
Provide costimulatory signals (confirmation for T cell to get excited and activated after seeing the Ag)
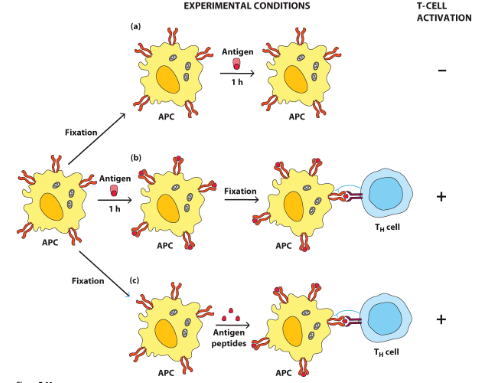
explain the evidence for antigen processing requirement in APCs to activate T cells
a) APC get fixated (kills APC, so proteins get fixed on surface, blocks Ag pick up), then Ag is given, but the Ag cannot bind because of fixation so no T cell activation
b) APC is given Ag, Ag binds and is processed then but on PM, APC is fixated, T cell gets activated
c) APC is fixated, then given Ag peptides (already cut up/processed Ags), MHC can present the peptides even after fixation because they were already processed, T cells get activated
this is evidence that Ag needs processing before MHC presentation
processing was either done by the APC or given processed but either allowed presentation to T cell
describe MHC class 1, MHC class 2
location
type of cells they present to
types of Ags they present
MHC Class I molecules
on most nucleated cells (infected cells)
present:
to TC (CD8+)
“endogenous” (Ags inside the cell, ex. viral, tumor Ags) antigens processed in cytosolic pathway
includes antigens of viruses that have infected cells
MHC Class II molecules
on APCs (engulf and process Ags, not infected)
present:
to TH (CD4+)
exogenous (extracellular, anything forgien in serum, need to be taken in but are not infected) antigens processed in endocytic pathway
if an APC was infected, what MHC class would it present its Ag on?
class 1 (always for infection to present to killer Ts)
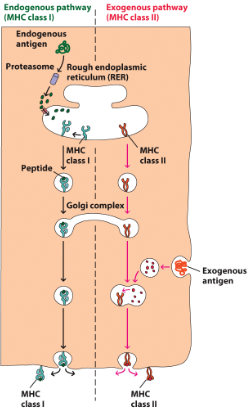
describe the endogenous and exogenous processing pathways
endogenous/cytosolic (MHC class 1)
Ag gets degraded by a proteasome in the cytosol into Ag peptides. Chaperons guide the peptide to assemble it onto MHC in the RER then progresses through the endomembrane system (vesicle, golgi, vesicle, PM), to present on PM
exogenous pathway
MHC class 2 leaves the RER in a vesicle and travels to golgi
leaves golgi in a vesicle
exogenous antigen gets engulfed in an acidic vesicle which degrades the Ag into Ag peptides
the MHC and Ag peptide vesicles merge so the MHC and peptide assemble and move to PM
describe the evidence for the two different presentation pathways
experimental design
Experimental design: test whether class I-restricted or class II-restricted TC cells lyse targets after different treatments of targets:
infectious virus (positive control to make sure assay works to infect cells with virus and T cells can lyse)
noninfectious virus (UV-inactivated)
can not get into the cell, can only do endocytic pathway
infectious virus + emetine (inhibits viral protein synthesis)
prevents viral protein from produced in the cytosol, but virus can get in cell
no viral proteins in the cytosol
eliminates cytosolic Ag (eliminates cytosolic pathway)
infectious virus + chloroquine (blocks endocytic pathway in target cells)
exogenous pathway only
virus can still infect and get into cytosol
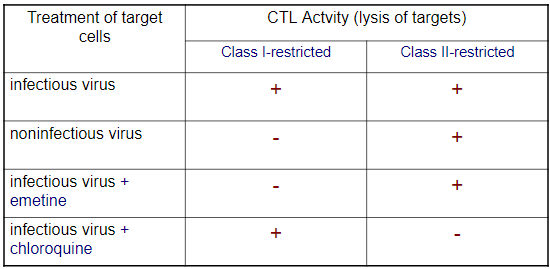
explain the results of the experiment
a) positive control → virus gets into cell by infection, but cell can endocytose virus too, both pathways worked, positive control works
b and c) no viral protein in cytosol, but endocytosis occurs, no class 1 restricted activity but still class 2 restricted activity, therefore T cells in class 2 endocytic pathway still worked, but not cytosolic
d) infectious virus gets into cell and makes viral protein, get cytosolic Ag, endocytic pathway blocked, class 1 restricted activity is there but not class 2, shows cytosolic pathway functions, but not endocytic
thus there must be 2 separate pathways because diff results for each condition
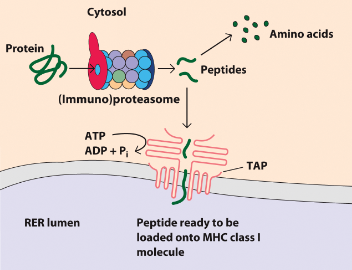
cytosolic pathway
Processes endogenous antigens (intracellular proteins, including viral proteins if virus has infected cell)
Features:
degradation of proteins in proteasomes (organelles)
unique to class 1
peptide transport to and through rough endoplasmic reticulum (RER)
class I MHC-peptide complex assembly assisted by chaperone proteins
shuttled to PM
explain proteolytic degradation
both normal/constitutive proteosomes (all cells have) and immuno-proteosomes (special to immune cells) cut Ag into specific peptides that are ideal for MHC class 1 binding
ideal aa sequence
ideal size
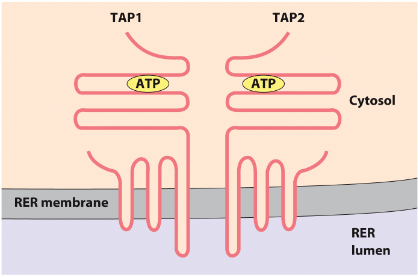
overview of peptide transports into RER for MHC class 1
assisted by?
ideal peptides
Assisted by TAP for presentation on MHC class 1
transporter associated with antigen processing
heterodimer encoded within MHC class II
spans RER membrane
ATP-dependent
Ideal peptides for MHC:
8-10 amino acids
hydrophobic or basic carboxy termini
describe TAP structure
ARP dependent
2 chain transporter
selects by size based on what it allows into RER
spans RER membrane
explain TAP activity
proteosome degrades Ag into aa (to be recycled) and into peptides
some of the peptides go through TAP (ATP dependent manner) into RER lumen
in RER lumen the peptide is ready to be loaded onto MHC class 1 molecule (with the help of chaperones to prevent peptide degradation in RER)
name and describe the chaperones involved in Peptide-MHC 1 complex assembly in RER
Assisted by chaperone proteins
calnexin: membrane RER protein
promotes folding of free class I α chain
released when β2 microglobulin binds α chain
calreticulin
remains bound to class I while it has no peptide
tapasin (TAP-associated protein):
membrane-bound
brings TAP close to class I molecule, promotes peptide transfer
releases MHC after peptide bound
ERp57 (protein with enzymatic activity)
disulfide bond with tapasin and association with calreticulin
ERAP1 (exopeptidase in the ER)
trims peptides before they bind to MHC
describe the endocytic/exogenous pathways
what is processed
time?
features
MHC class 2 (APCs presenting to helper Ts)
Processing of exogenous antigens (they must be endocytosed)
Takes 1-3 hours
Features
association of invariant chain with class II molecules (in peptide binding groove to stabilize it and block other things, acts as a place holder) when MHC class leaves RER, until it meets the peptide
invariant chain gradually gets degraded through endomembrane system and becomes CLIP structure
HLA-DM and HLA-DO (positive and negative regulators of the exchange of CLIP and peptide in the peptide binding groove)
generation of peptides in endocytic vesicles
describe Invariant chain (Ii) and CLIP
Trimeric protein
Associates with 3 pairs of class II α and β chains in the RER
Blocks peptide-binding cleft of class II molecules
Guides transport of class II molecules out of ER and to endocytic vesicles (where peptides are)
Gets gradually degraded
small fragment remains bound to cleft:
CLIP (class II-associated invariant chain peptide)
describe HLA-DM
Encoded by class II MHC
Catalyzes exchange of CLIP for peptide
α and β chains, but nonclassical MHC, not polymorphic
Reside in endosomes
Inhibited by HLA-DO
describe HLA-DO
Hinders HLA-DM
In B cells
downregulated in germinal centre B cells
Recently found in DCs
downregulated during DC activation
In thymic medullary epithelial cells
what is cross-presentation of exogenous Ag?
Exogenous antigens internalized and presented via the endogenous presentation pathway (or vice versa)
which would cells do cross-presentation?
why is it important?
dendritic cells
killer T cells need support by APCs to be able to recognize MHC1
need to get exogenous Ag to MHC1 (not MHC2) so that killer T cells can recognize
need to ensure killer Ts does not kill the dendritic cell
allows dendritic cell to not only activate helper Ts but also killer Ts
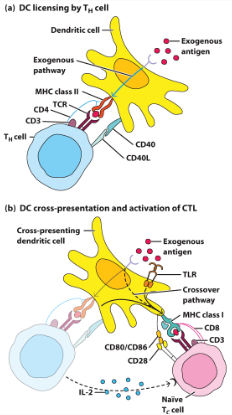
describe dendritic cell licencing and cross presentation
a) dendritic cell presents Ag to helper T to activate it. helper T interacts with DC to license it to allow it to cross present
b) DC can now also present on MHC class 1 to activate killer T cells now (naive). helper T still is around and supports (releases cytokines)