Motor systems II
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Cerebellum
closely involved with brainstem mechanisms- unconscious movement
control of muscle tone
sensorimotor coordination
motor learning
basal ganglia
integration of sensory and motor information
cortex —> basal ganglia —> cortex loop (via thalamus)
Cerebellum + basal ganglia
Loop pathways in brain, take info from cortex and send it back to a different part of the cortex
coming from premotor areas, partly goes back to primary motor cortex
like each other less than cerebellum + brainstem
Spino-cerebellum
medial region of cerebellum
sensory input from spinal cord- sensory info mixing with motor info, unconscious muscle contractions keep you upright
output to the reticular formation + red nucleus
then to motor cortex, and via this:
output to spinal cord
control over axial musculature and posture
damage causes:
hypotonia
ataxia
dysmetria and intention tremor
vestibulo-cerebellum
caudal region of cerebellum
input from and output to vestibular nucleus
control over posture/balance, also eye movement
damage causes:
slow saccades (fast tracking ocular movement impaired)- abnormal eye movement
mystagmus (due to failed vestibulo-oculomotor integration
ataxia
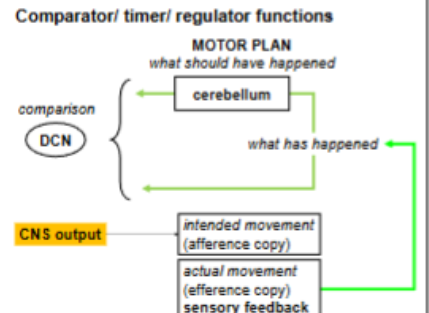
cerebro-(ponto)-cerebellum
lateral hemispheres of cerebellum
an intracerebral motor loop
instructs the primary motor cortex (M1)
regarding movement direction, timing and force
compares intended movements w/actual- compensatory instructions to rectify movements that aren’t going as planned
damage causes:
incoordination/ataxia
dysmetria
asynergy- uncoordinated agonist and antagonist muscles
dysarthria- inarticulate speech, poor oropharyngeal muscular control
cerebro-(ponto)-cerebellum loop
cortex —> pons —> cerebellum —> dentate nucleus (deep cerebellar nuclei) —> ventrolateral thalamus —> cortex (M1)
outline the inputs of the cerebellar cortex
climbing fibres input from inferior olive
excitatory and act on purkinje cells
mossy fibres from brainstem nuclei
indirectly excite purkinje cells via parallel fibres of granule cells

outline the outputs of the circuitry of the cerebellar cortex
only purkinje cells- project to deep cerebellar nuclei
deep cerebellar nuclei receiving sensory information directly + indirectly (going into network and back out through purkinje fibres)
purkinje fibre receives lots of input coming from parallel fibres coming from granule cells, also input from climbing fibres
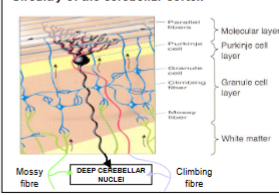
how does the circuitry of the cerebellar cortex talk to each other?
deep cerebellar nuclei (DCN) cells compare input from mossy and climbing afferent input
before (via collaterals from axons to P cell- excitatory) and after cerebellar processing (via inhibitory P cell output)
results in an error signal if inputs don’t match
draw the circuitry of the cerebellar cortex
ataxia
unsteady, staggering gait
functional components:
spino cerebellum
cerebro-ponto-cerebellum
vestibulo-cerebellum
dysmetria
inaccurate termination of movement
functional component:
spino-cerebellum
cerebro-ponto-cerebellum
hypotonia
reduced muscle tone
spino-cerebellum
slow saccades + nystagmus
impaired eye movement, vestibulo-cerebellum
dysathria
inarticulate speech due to poor oropharyngeal muscular control
cerebro-ponto-cerebellum
summarise the functions of the cerebellum
regulates posture indirectly by adjusting output of major descending motor pathways
acts as a comparator, identifying and correcting discrepancies between intended and actual movement
acts as a timer, sequencing motor activation resulting in smooth performance
role in motor memory, and in instigating learned motor sequences when appropriate
not required for perception or muscle activation
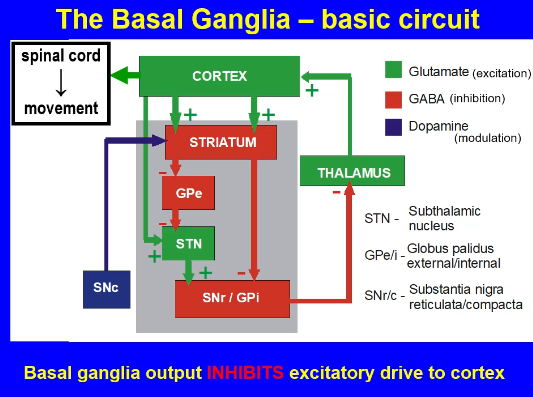
cortico-basal ganglia-cortical loop
integrates motor and sensory information from the cortex
relays back to the cortex via thalamus
motor circuit output to premotor/SMA cortex
selection and initiation of voluntary movement
basal ganglia —>ventrolateral thalamus—>motor cortex—>brainstem + SC
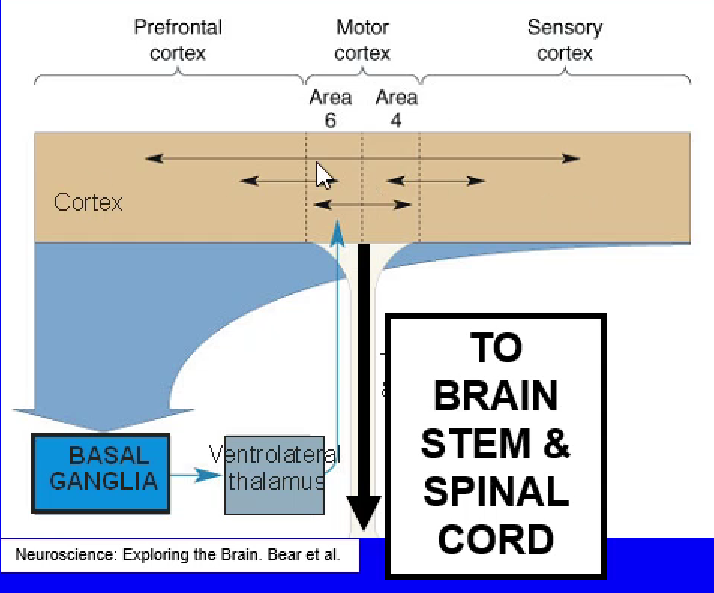
Draw the Motor loop of cortico-basal ganglia-cortical loop
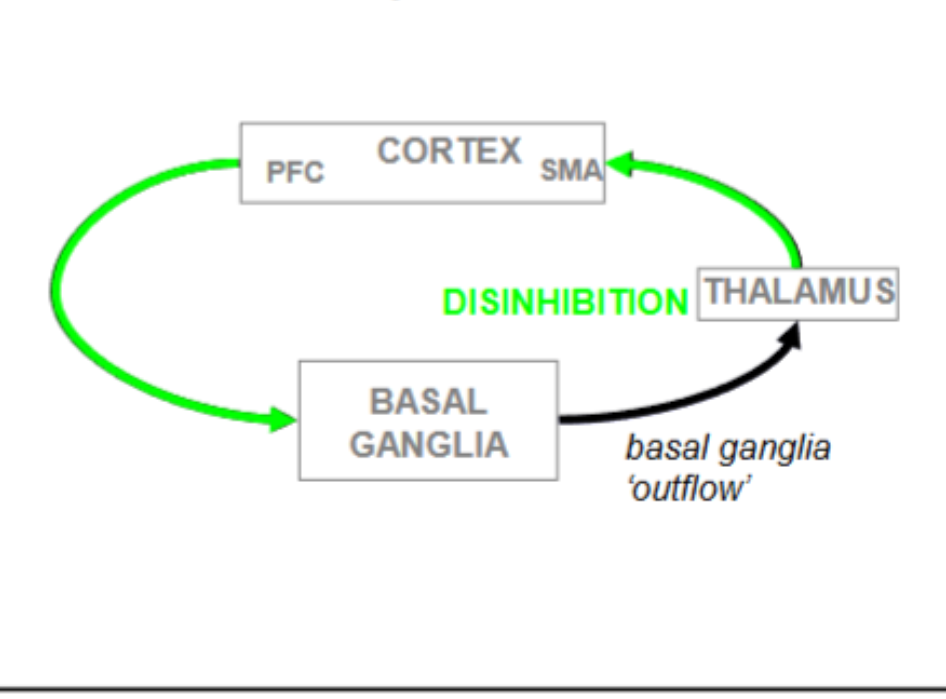
Signal from BG to thalamus = inhibitory
Need to switch off inhibitory output to move
Switching off inhibitory output means thalamus can get excited, sends excitatory signal to cortex
PFC gives excitatory signal to BG, switches off output, thalamus is now disinhibited
BG needs to suppress other potentially conflicting motor pathways, moderates information
Striatum
Part of basal ganglia
caudate nucleus
putamen
nucleus accumbens
Basal ganglia (all the major structures)
caudate nucleus
putamen
nucleus accumbens
globus pallidus (GP)- internal and external
substantia nigra
subthalamic nucleus (STN)
Sub-types of globus pallidus
Internal = GPi
External = GPe
Sub-types of substantia nigra
Reticulata (SNr)
Pars compacta (SNc)
Name the direct pathways of the basal ganglia
striato-nigral pathway
striato-pallidal pathway GPi
Where do the indirect pathways project?
via GPe and STN
Outline the types of pathway in the basal ganglia
From striatum, cortical input relayed to two major output areas w/in the basal ganglia, SNr and GPi
opposing effects on thalamocortical output
balance between the direct and indirect pathways
dopamine plays a key modulatory role
Draw the basic circuit of the basal ganglia
Ignore cortex to STN pathway
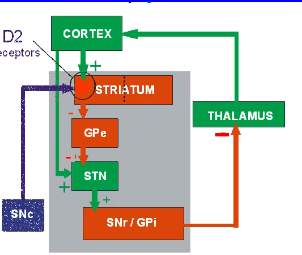
Draw the direct pathway of the basal ganglia

Direct pathway BG
promotes movement
striatum gets excited, releasing GABA which inhibits SNr/GPi, inhibiting SNr/GPi inhibits thalamus
dopamine acts on excitatory D1 receptors on striato-GPi/SNr neurons
this further reduces BG output and facilitates movement
Draw the indirect pathway of the basal ganglia
Indirect pathway BG
suppresses movement
dopamine acts on inhibitory D2 receptors on striato-GPe neurons
this reduces STN activity, BG output and facilitates movement
GABAergic cells different cells in striatum to the ones that go down the indirect pathway
How can the basal ganglia cause motor dysfunction?
imbalance between the indirect and direct pathways —> motor dysfunction
hypokinetic disorders such as HD, ballism, tardive dyskinesia
hyperkinetic disorders such as PD
Parkinson’s disease symptomology
tremor- resting not intention
bradykinesia - slowness of movement
rigidity- resistance to passive movement
dementia, depression, bladder disturbance
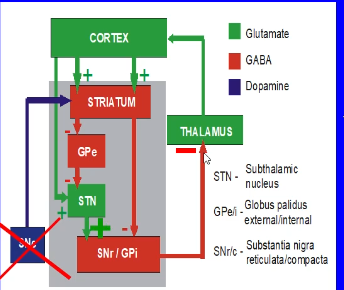
PD pathology
Progressive degenerative loss of the nigro-striatal dopaminergic pathway
Over 80% lost by the time symptoms start + diagnosis is made
Excessive inhibition of thalamo-cortical pathway
Accompanied/driven by increase in subthalamic nucleus
Draw how PD affects the circuitry of the BG
Treatments for PD
drugs to boost dopamine in brain:
L-DOPA = dopamine precursor
dopamine agonists
drugs to reduce dopamine breakdown (MAO-B inhibitors)
Deep brain stimulation
Inhibit STN
No treatments address the underlying degeneration
Dopamine replacement therapy for PD
reduces rigidity and hypokinesia
L-DOPA metabolised to produce dopamine by DOPA-decarboxylase in DA-ergic neuron
But L-DOPA also elevates NAdr synthesis in sympathetic NS
Non-brain penetrating carbidopa or benserazide co-administered to inhibit peripheral DOPA decarboxylase
Huntington’s disease symptomology
excessive ‘choreiform’ movement
uncontrollable, relatively rapid motor patterns disrupts normal motor activity
later stages —> psychiatric disturbance, dementia
Primary pathology HD
In early stages:
loss of striatal output neurons in indirect pathway
suppression of STN
predominance of direct pathway
reduced BG output
overactive thalamocortical pathway
involuntary movement
HD treatments
Only symptomatic relief
Drugs that inhibit VMAT, reduce DA storage and release
drugs that are DA antagonists (antipsychotic)
Drugs that are GABA-B agonists, reduce spinal reflexes
Hemiballismus
caused by damage to subthalamic nucleus (usually by unilateral stroke)
effect: violent flailing movements of limbs contralateral to damaged side
tardive dyskenesia
caused by long-term exposure to antipsychotic dopamine receptor antagonist drugs
uncontrolled movement, especially of facial and trunk muscles