Diseases of the Large Intestine
1/163
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
164 Terms
large intestine =
colon
what is the major function of the proximal (right, ascending) portion of the colon?
reclaims most of the salts & water that do not get absorbed in the small intestine
what is the major function of the distal (left, descending) portion of the colon?
stores solid wastes for evacuation
the colon is approx. _____ meters in length
1.5 meters
what are the 6 parts of the colon?
- cecum
- ascending
- transverse
- descending
- sigmoid
- rectum
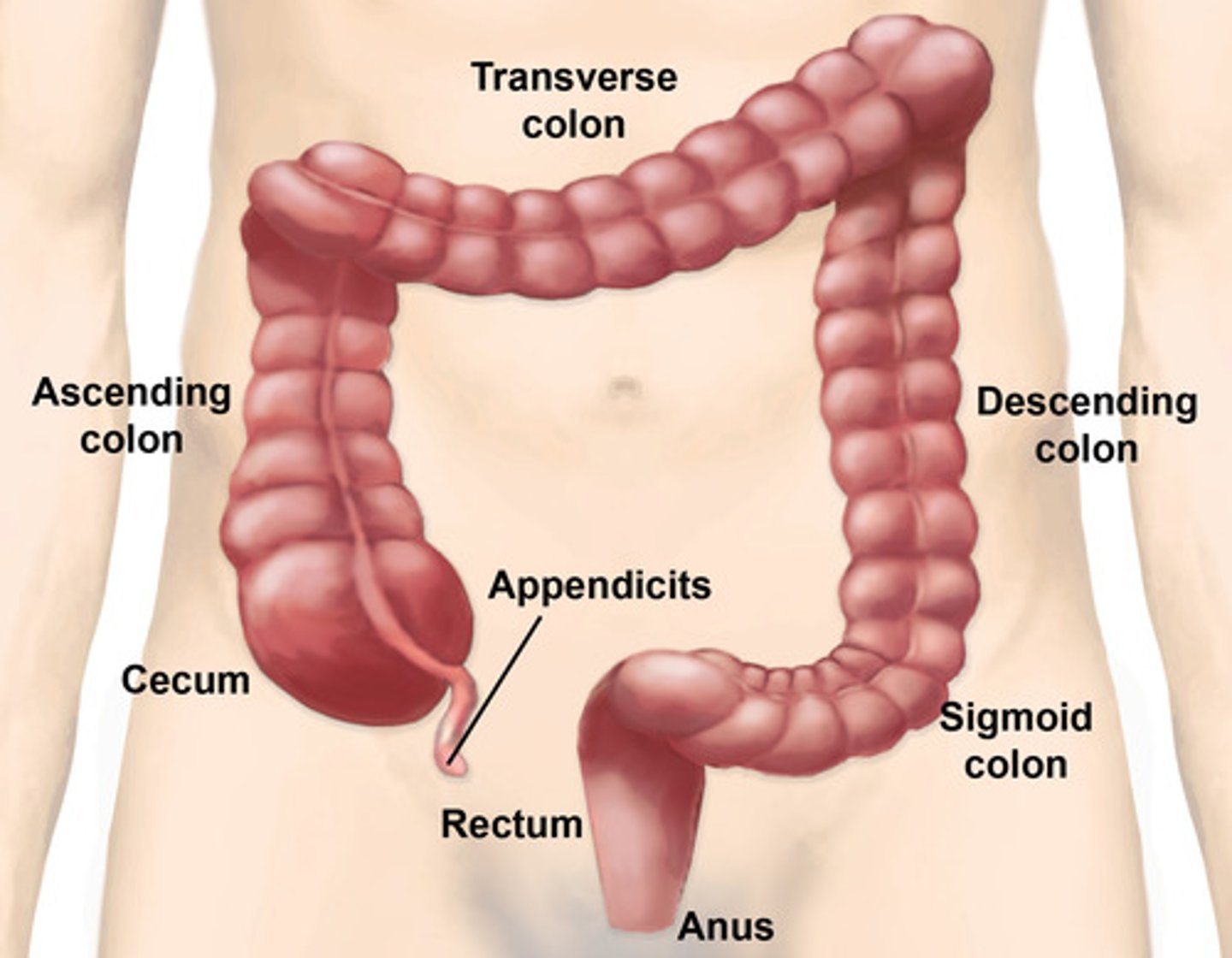
what is the cecum?
a blind pouch below the ileocecal valve
why is the cecum more prone to perforation than other areas?
bc it has the largest diameter & thinnest wall of any part of the intestines
which parts of the large intestine are retroperitoneal?
- ascending colon
- descending colon
- rectum
- anal canal
which parts of the large intestine are intra-abdominal (NOT retroperitoneal)?
- cecum
- appendix
- transverse colon
- sigmoid colon
the retroperitoneal portions of the large intestine are ______________________.
relatively fixed
the intra-abdominal portions of the large intestine are ______________________.
freely mobile on their attached mesentery
which artery supplies the proximal colon, jejunum & ileum?
superior mesenteric
which artery supplies the mid-transverse colon to rectum?
inferior mesenteric
do the lymphatic vessels of the colon extend to the lamina propria like in the small intestine?
NO
1 multiple choice option
why are infection or cancer less prone to spread through the lymph system when in the colon?
bc lymphatic vessels of the colon do NOT extend to the lamina propria like in the small intestine
when can cancer from the colon spread?
only when the invasive process penetrates to the submucosa
does the colon have villi like the small intestine?
no
1 multiple choice option
what are crypts?
long straight pits of colonic epithelium
- have secretory cells which produce mucus & absorptive cells
in the small intestine, the longitudinal muscle is a continuous circumferential sheet.
how is the longitudinal muscle of the large intestine divided?
into 3 discrete ribbon-like bands, called taeniae coli
- which run the length of the colon
what forms the haustra?
contraction of the taeniae coli which shortens the colon
what do the intestines (both small & large) do?
- secrete (from crypts)
- digest plant & some simple carbs poorly
- absorbs fatty acids & residual water along ascending & transverse colon
do humans digest complex plant carbs (dietary fiber) & some simple carbs (stachyose, sorbitol, lactulose) well?
no, poor digestion of these things
1 multiple choice option
where are fatty acids & residual water absorbed?
along the course of the ascending colon & transverse colon
retrograde waves of contraction originate in the __________________ colon & serve to retain liquid stool in cecum
midtransverse
what stimulates antegrade contractions to move stool along?
distention of the colonic wall
what provokes the gastrocolic reflex?
food in the stomach & small intestine
- to encourage the colon to propel contents of the cecum
what produces the "call to stool?"
when stool reaches the rectum, stretch receptors initiate the anorectal inhibitory reflex which relaxes the anal sphincter
what allows us to pass stool?
coordination of relaxation of the external anal sphincter & puborectal muscles
- which allow the rectum to straighten
- then via the valsalva maneuver (bearing down) the sigmoid colon & rectal muscles contract, creating increased intra-abdominal pressure
what is irritable bowel syndrome (IBS)?
idiopathic, characterized by chronic abdominal pain or discomfort occurring w/ altered bowel habits
- can be continuous or intermittent
what are the diagnostic features of IBS?
2 of 3 required:
- relieved w/ defecation
- onset assoc. w/ change in frequency of stool
- onset w/ a change in form of stool
what may cause IBS?
- abnormal motility
- visceral hypersensitivity
- enteric infection
- psychosocial abnormalities
how does visceral hypersensitivity cause IBS?
lower visceral pain threshold
- w/ complaints of bloating & distention as well as rectal urgency, despite small rectal volumes of stool
w/ IBS, enteric infection seems to cause a ___________________ syndrome in a small amount of patients (possibly due to alterations in distribution of bacterial species or overgrowth of bacteria in intestines)
"post-infectious"
s/s of IBS:
- intermittent, crampy lower abdominal pain (does NOT occur at night or interfere w/ sleep)
- bowel habit (w/ diarrhea or w/ constipation)
what does IBS w/ diarrhea refer to?
loose or watery stools > 3x/day
- urgency & possible fecal incontinence
what does IBS w/ constipation refer to?
hard, lumpy stools
- frequency < 3x/wk or straining to defecate
bristol stool chart
**know this
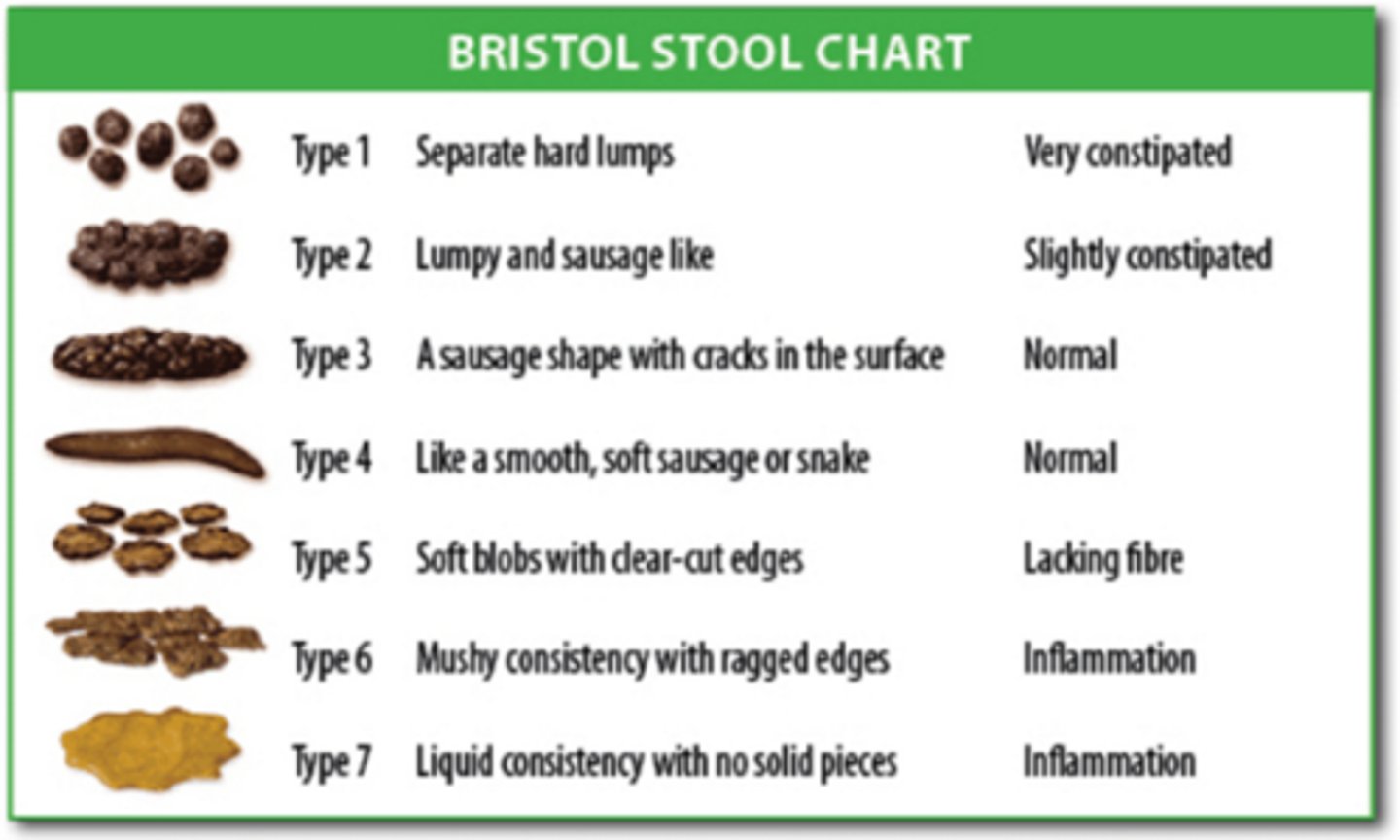
bristol stool chart:
type 1
separate hard lumps
- very constipated

bristol stool chart:
type 2
lumpy & sausage like
- slightly constipated

bristol stool chart:
type 3
a sausage shape w/ cracks in the surface
- normal

bristol stool chart:
type 4
like a smooth, soft, sausage or snake
- normal

bristol stool chart:
type 5
soft blobs, w/ clear cut edges
- lacking fiber

bristol stool chart:
type 6
mushy consistency w/ ragged edges
- inflammation

bristol stool chart:
type 7
liquid consistency w/ no solid pieces
- inflammation

what are the alarm sx w/ IBS?
- acute onset (esp. in older pts)
- nocturnal diarrhea
- severe diarrhea or constipation
- hematochezia
- weight loss
- fever
when should IBS pts undergo additional evaluation?
fam hx of:
- cancer
- IBD
- celiac disease
when should stool for O & P be obtained in an IBS patient?
only if there is a high likelihood of infection
- ex: daycare workers, campers, foreign travelers
when should endoscopy be conducted in an IBS patient?
if do not improve w/ conservative therapy or if > 50 y/o who have not had previous eval
how is IBS treated initially?
- reassurance
- education
- support
- identify & respond to patient's concerns
- investigate possible psychosocial stressors, changes in diet, meds or other life events
- dietary therapy (food diaries)
if the IBS pt does not respond to conservative therapy, what pharmacological agents can be added adjunctively?
- antispasmodic/anticholinergics (hyoscyamine, dicyclomine or methscopalamine)
- antidiarrheals (loperamide)
- bile salt binding agents (cholestyramine)
- anti constipation agents (Miralax)
- psychotropic agents (TCAs)
- serotonin receptor antagonists
- abx (Rifaximin)
- probiotic (bifidobacterium infantis)
- CBT
what is Rifaximin?
abx shown to reduce sx of IBS (likely through alteration in the gut flora)
- limited to 14 days usage
- can be used twice if necessary
what is constipation?
infrequent or hard stools, excessive straining or sense of incomplete evacuation
what is the normal colon transit time?
35 hrs
> 72 hrs is significantly abnormal
can primary constipation be attributed to structural abnormalities or systemic disease?
no
1 multiple choice option
what does normal defecation require?
coordination between the anal sphincter & pelvic floor relaxation, along with ↑ intra-abdominal pressure through valsalva maneuver
what may secondary constipation be caused by?
- systemic disorders (neurologic gut dysfunction, myopathies, endocrine disorders or electrolyte abnormalities)
- medication side effects (anticholinergics or opioids)
- colonic lesions (neoplasms or strictures)
how is constipation diagnosed?
thorough history (including psychosocial investigation)
- PE including DRE (to assess for anatomic abnormalities, anal stricture, rectocele, rectal prolapse); assessment of pelvic floor motion is done by having patient try to expel the examiners finger
how is constipation treated?
- dietary & lifestyle changes
- laxatives prn or scheduled
which type of laxatives can be used daily?
osmotic laxatives
- increase secretion of water into the intestinal lumen, softening stools
- increased water intake needed to avoid dehydration
which type of laxatives can be used as a rescue agent intermittently?
stimulant laxatives
- cause decreased normal bowel function if overused & lead to laxative dependence
which type of laxatives are effective, but expensive & therefore are reserved for refractory cases of constipation?
chloride secretory agents
opioid receptor antagonists have become more necessary in constipation tx, due to increased opioid use.
what do they do?
block peripheral opioid receptors, including those in the gut
- while not affecting CNS analgesia
if fecal impaction is palpable on DRE, what is required for tx?
enema & digital removal of the impaction
how can diarrhea be classified?
as acute (non-inflammatory or inflammatory) or chronic
acute diarrhea
acute in onset, lasting for < 2 wks
- MOST commonly caused by infectious agents, bacterial toxins or meds
what do community outbreaks of acute diarrhea suggest?
viral infection or common food source
- ex: family exposure or improper food storage
daycare attendance or exposure to unpurified water (such as, camping or swimming in a stream or creek) may result in infection w/:
- giardia
- cryptosporidium
recent antibiotic use indicates possible ________________________ infection
clostridium difficile
HIV or risk factors for STDs suggest possible _______ infection
CMV
non-inflammatory acute diarrhea
watery, non-bloody diarrhea
- assoc. w/ periumbilical cramps, bloating, nausea or vomiting
- likely a small bowel source (such as, viruses or giardia)
- can be voluminous & result in dehydration, hypokalemia, &/or metabolic acidosis
- fecal leukocytes are NOT present
what does prominent vomiting suggest?
viral enteritis or "food poisoning"
inflammatory acute diarrhea
presence of fever & bloody diarrhea (dysentery) indicates colonic tissue damage
- caused by invasion of either organisms or toxins
- mostly involves colon, so the volume of diarrhea will be smaller & assoc. w/ LLQ cramps, urgency & tenesmus
- fecal leukocytes or lactoferrin are usually present
what is the major complication of shiga-toxin producing organisms?
hemolytic-uremic syndrome
diarrhea which persists for > 14 days should be evaluated as chronic diarrhea, except in the case of _____________.
c. difficile
what does infectious dysentery (diarrhea) present similar to?
acute ulcerative colitis (IBD)
- should be distinguished
acute diarrhea red flag symptoms requiring medical evaluation include:
- signs of inflammation (fever, WBC >15000, bloody diarrhea or severe abdominal pain)
- passage of >/= 6 unformed stools in 24 hrs
- profuse watery diarrhea & dehydration
- frail or immunocompromised patients
- recent use of abx
- hospital acquired (HA) diarrhea
- systemic illness
possible signs of acute diarrhea on PE:
- dehydration
- mental status change
- abdominal tenderness
- signs of peritonitis (w/ invasive infectious diarrhea)
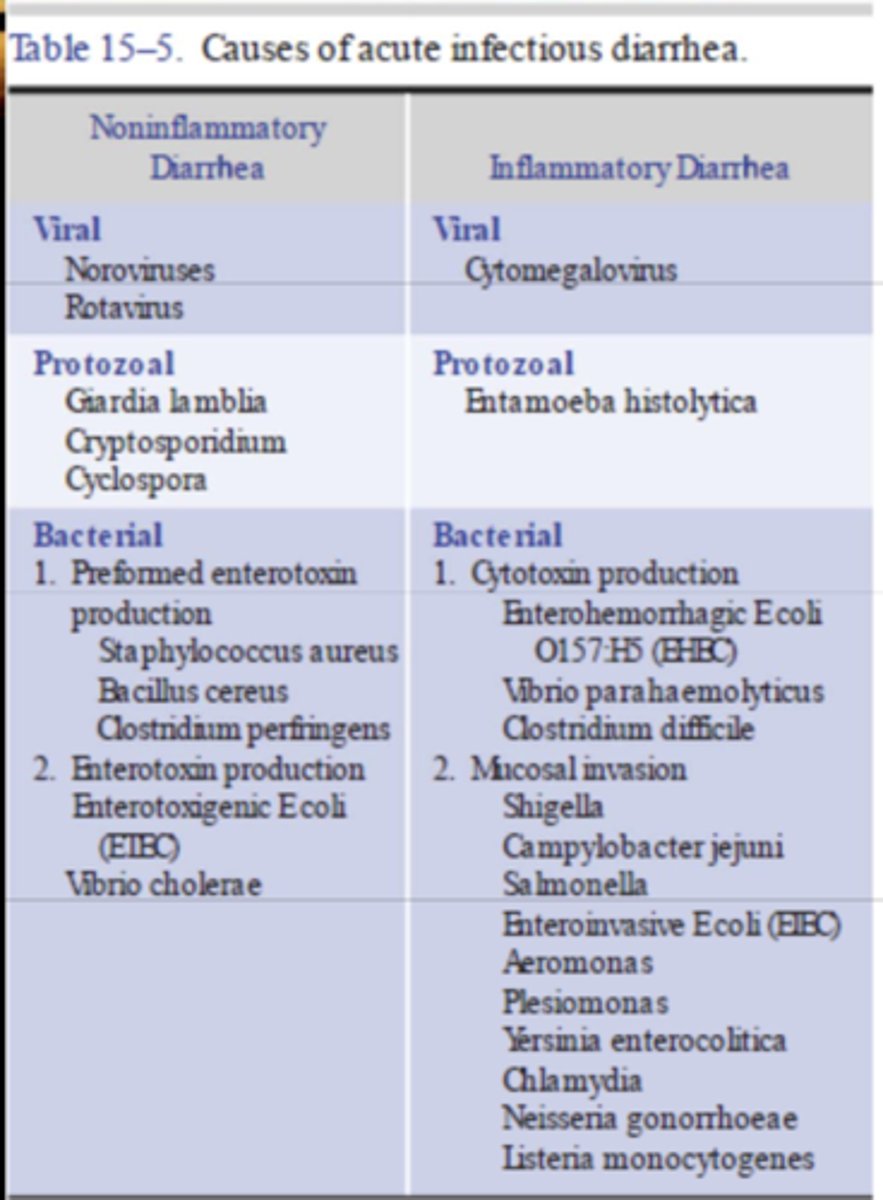
causes of acute infectious diarrhea
**keep in mind preformed vs not preformed enterotoxins
when may protozoal infections be seen?
- daycare
- unfiltered water source (swimming or drinking)
what is the typical mechanism of acute bacterial infection (which results in acute diarrhea)?
a. a bacterial infection of the intestinal wall
b. bacterial infection due to preformed enterotoxins produced by bacteria
b. bacterial infection due to preformed enterotoxins produced by bacteria
what is the difference between preformed enterotoxin & non-preformed enterotoxin production?
preformed = makes toxin before consumption (make their toxin & put it on food that we eat)
non-preformed = makes toxin after consumption (make their toxin once inside our bodies)
which viruses cause acute noninflammatory diarrhea?
- noroviruses
- rotaviruses
which virus causes acute inflammatory diarrhea?
cytomegalovirus (CMV)
which protozoa cause acute noninflammatory diarrhea?
- giardia lamblia
- cryptosporidium
- cyclospora
which protozoa causes acute inflammatory diarrhea?
entamoeba histolytica
which bacteria cause acute noninflammatory diarrhea?
preformed enterotoxin:
- staphylococcus aureus
- bacillus cereus
- clostridium perfringens
non-preformed enterotoxin:
- enterotoxigenic e. coli
- vibrio cholerae
which bacteria cause acute inflammatory diarrhea?
cytotoxin production:
- enterohemorrhagic e. coli
- vibrio parahaemolyticus
- clostridium difficile
mucosal invasion
- shigella
- campylobacter jejuni
- enteroinvasive e. coli
- aeromonas
- plesimonas
- yersinia enterocolitica
- chlamydia
- neisseria gonorrhoeae
- listeria monocytogenes
which is more common in children?
a. norovirus
b. rotavirus
b. rotavirus
which is more common in adults?
a. norovirus
b. rotavirus
a. norovirus
which is a type of bacteria w/ preformed enterotoxin that may cause non-inflammatory acute diarrhea?
a. clostridium perfringens
b. clostridium difficile
a. clostridium perfringens
c. diff is a cytotoxin producing cause of acute inflammatory diarrhea
which produces a cytotoxin & causes inflammatory diarrhea?
a. clostridium perfringens
b. clostridium difficile
b. clostridium difficile
which type of e. coli bacteria does NOT have preformed enterotoxin (meaning it produces it once inside) & causes non-inflammatory diarrhea?
a. entertoxigenic e. coli
b. enterohemorrhagic e. coli
c. enteroinvasive e. coli
a. entertoxigenic e. coli
enterohemorrhagic = cytotoxin producing cause of inflammatory
enteroinvasive = inflammatory cause by mucosal invasion
which type of e. coli bacteria produces a cytotoxin & causes inflammatory diarrhea?
a. entertoxigenic e. coli
b. enterohemorrhagic e. coli
c. enteroinvasive e. coli
b. enterohemorrhagic e. coli
which type of e. coli bacteria causes inflammatory diarrhea by mucosal invasion?
a. entertoxigenic e. coli
b. enterohemorrhagic e. coli
c. enteroinvasive e. coli
c. enteroinvasive e. coli
which does NOT have preformed enterotoxin (meaning it produces it once inside) & causes non-inflammatory diarrhea?
a. vibrio cholerae
b. vibrio parahaemolyticus
a. vibrio cholerae
vibrio parahaemolyticus = cytotoxin producing cause of inflammatory
which produces a cytotoxin & causes inflammatory diarrhea?
a. vibrio cholerae
b. vibrio parahaemolyticus
b. vibrio parahaemolyticus
if diarrhea worsens or persists for > 7 days, what should the stool be tested for?
- fecal leukocytes or lactoferrin
- O&P
- bacterial culture w/ serotyping for shiga toxin producing e. coli
how is acute diarrhea treated?
- diet (adequate oral fluids, containing carbs & electrolytes + easily ingested foods, such as soups, applesauce)
- oral rehydration (fluids w/ glucose, Na+, K+, Cl-, HCO3)
- antidiarrheal agents
fluids that can be used for oral rehydration therapy?
Pedialyte or Gatorade
- 50 to 200 ml/kg/d
when should anti-diarrheal agents NOT be used?
- bloody diarrhea
- high fever
- systemic toxicity