Chap 23 Acute Respiratory Distress Syndrome
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
Acute Respiratory Distress Syndrome
Form of hypoxemic respiratory failure
Associated pulmonary edema leads to:
Severe hypoxemia
Intrapulmonary shunting
Reduced lung compliance
In some cases, irreversible damage to lung tissue
Management of Acute Respiratory Distress Syndrome
Replace fluids.
Provide drug therapy to support mechanical ventilation.
Administer pharmacologic agents to stabilize pulmonary, capillary, and alveolar walls.
Provide diuretics.
Consider cause of the underlying problem.
Provide high-flow nasal oxygen and ventilator support.
Pulmonary Embolism
Blockage of a pulmonary artery by a clot or other foreign material
Usually originates in lower extremities or pelvis
Relatively common
Sudden death is the first sign in about one-fourth of patients.
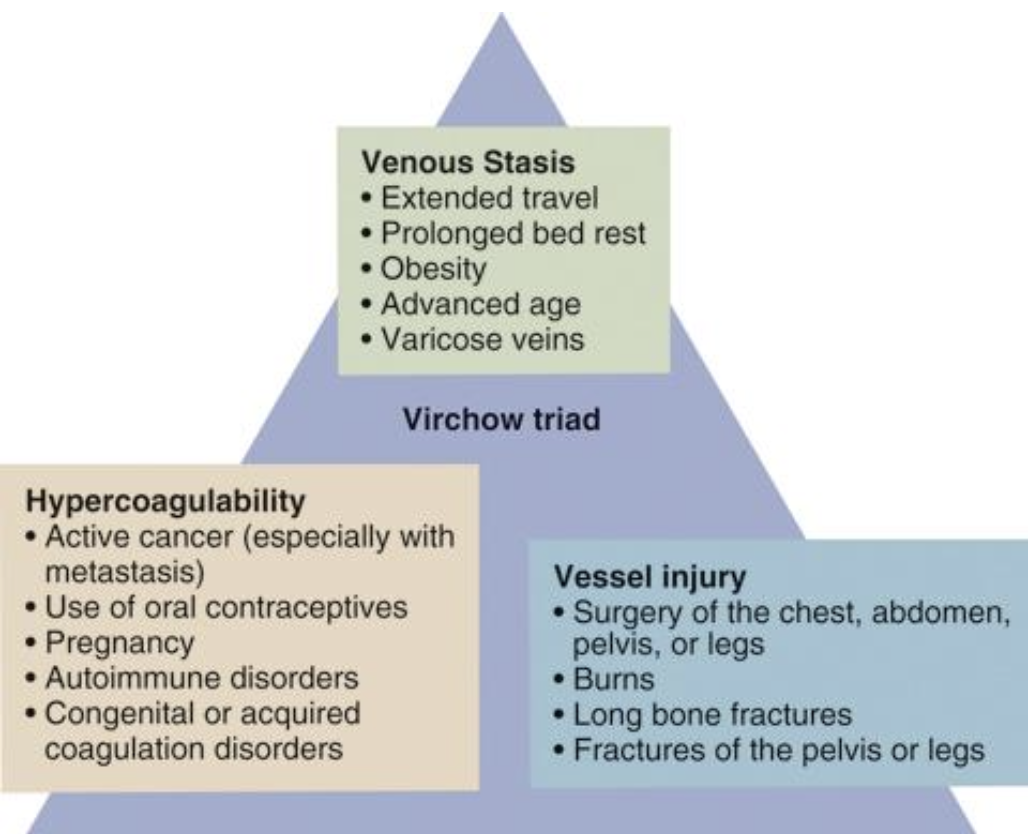
Virchow triad
factors contribute to clot formation
Hypercoagulability
Stasis
Vessel injury
Signs and symptoms of Pulmonary Embolism
Dyspnea, cough
Hemoptysis (rare)
Pain
Anxiety
Syncope
Hypotension
Diaphoresis
Tachypnea
Sinus tachycardia
Fever
Distended neck veins
Chest splinting, pleuritic pain, pleural friction rub, crackles, and localized wheezing
Management of Pulmonary Embolism
Prehospital care is mainly supportive.
Administer supplemental high-concentration oxygen.
Apply cardiac monitor and pulse oximeter.
Establish IV line.
Transport in position of comfort.
Upper Respiratory Tract Infection
Common and rarely life-threatening
Can affect nose, throat, sinuses, and larynx
Includes common cold, pharyngitis, tonsillitis, sinusitis, and laryngitis
May exacerbate underlying pulmonary conditions
Signs and symptoms of Upper Respiratory Tract Infection
Sore throat
Fever
Chills
Headache
Facial pain (sinusitis)
Purulent nasal drainage
Halitosis (bad breath)
Cervical adenopathy
Erythematous pharynx
Spontaneous Pneumothorax
Usually results when bleb ruptures, allowing air to enter pleural space
May occur in seemingly healthy people aged 20–40 years
Secondary spontaneous pneumothorax may develop from underlying disease.
Common signs and symptoms of Spontaneous Pneumothorax
Shortness of breath
Sudden onset of chest pain
Pallor
Diaphoresis
Tachypnea
severe cases:
Altered mental status
Cyanosis
Tachycardia
Decreased breath sounds on affected side
Local hyperresonance to percussion
Subcutaneous edema
Management of Spontaneous Pneumothorax
Prehospital care is based on patient’s symptoms and degree of respiratory distress:
High-concentration oxygen
Airway, ventilator, and circulatory support
Transport in position of comfort.
If tension pneumothorax develops, perform needle chest decompression.
Hyperventilation Syndrome
Abnormally deep or rapid breathing that results in excessive loss of carbon dioxide
Produces hypocapnia
Leads to:
Cerebrovascular constriction
Reduced cerebral perfusion
Paresthesia
Dizziness
Feelings of euphoria
Conditions that can cause hyperventilation syndrome
Anxiety
Hypoxia
Pulmonary disease
Cardiovascular disorders
Metabolic disorders
Neurologic disorders
Fever
Infection
Pain
Pregnancy
Drug use
Signs and symptoms of Hyperventilation Syndrome
Dyspnea with rapid breathing and high minute volume
Chest pain
Facial tingling
Carpopedal spasm
Management of Hyperventilation Syndrome
Provide supportive care if life threats have been ruled out.
Administer oxygen administration.
Provide airway/ventilator support.
Calm patient and coach ventilations.
Do not attempt to slow ventilations if patient is compensating for hypoxia or metabolic acidosis.
If severe or complicated, transport for evaluation by physician.
Lung Cancer
Most cases develop in people age 65 years or older.
Of new cases reported, most patients die within 1 year.
Most common cause is cigarette smoking.
Other risk factors include:
Passive smoking
Exposure to asbestos, radon gas, dust, or coal products
Radiation therapy
Pulmonary fibrosis
Human immunodeficiency virus infection
Genetic factors
Alcohol consumption and exposure to other toxins
Pathophysiology of Lung cancer
Lung cancer—uncontrolled growth of abnormal cells
At least a dozen different cell types of tumors are associated with primary lung cancer.
Two major cell types: small cell and non-small cell
Most abnormal cell growth begins in bronchi or bronchioles.
Signs and symptoms of Lung cancer
Cough
Hemoptysis
Dyspnea
Hoarseness or voice change
Dysphagia
Weight loss/anorexia
Weakness
Chest pain
Management of Lung cancer
Provide airway, ventilator, and circulatory support.
Administer oxygen if indicated.
Transport for evaluation by physician.
Administer IV fluids if needed.
Provide drug therapy and analgesics if needed.
End-stage patients may have advance directives or DNR orders.
Respiratory Failure
Respiratory emergencies can result from many disease states, including:
Ventilatory failure
Oxygenation failure
Shock
Occurs when pulmonary gas exchange is sufficiently impaired to cause hypoxemia with or without hypercapnia
Hypoxemia
(oxygenation failure)
Conventional criteria:
PaO2 <60mm Hg
Causes:
Perfusion defect
Pneumonia
Pulmonary edema
Pulmonary embolism
Pulmonary contusion
Sepsis
V/Q mismatch
Hypercapnia
(Ventilatory failure)
Conventional criteria:
PaC02 >55mm Hg
Causes:
Asthma
Bronchiectasis
CNS injury
COPD
Drug overdose
Fatigue
Pump failure
Physiology Review
Exchange of gases between cells and environment
Ventilation—brings oxygen to lungs and removes carbon dioxide, which enables external or internal respiration
Other essential elements
Structure and function of chest wall
Control of breathing by central nervous system
Acid–base balance mediated by buffer systems
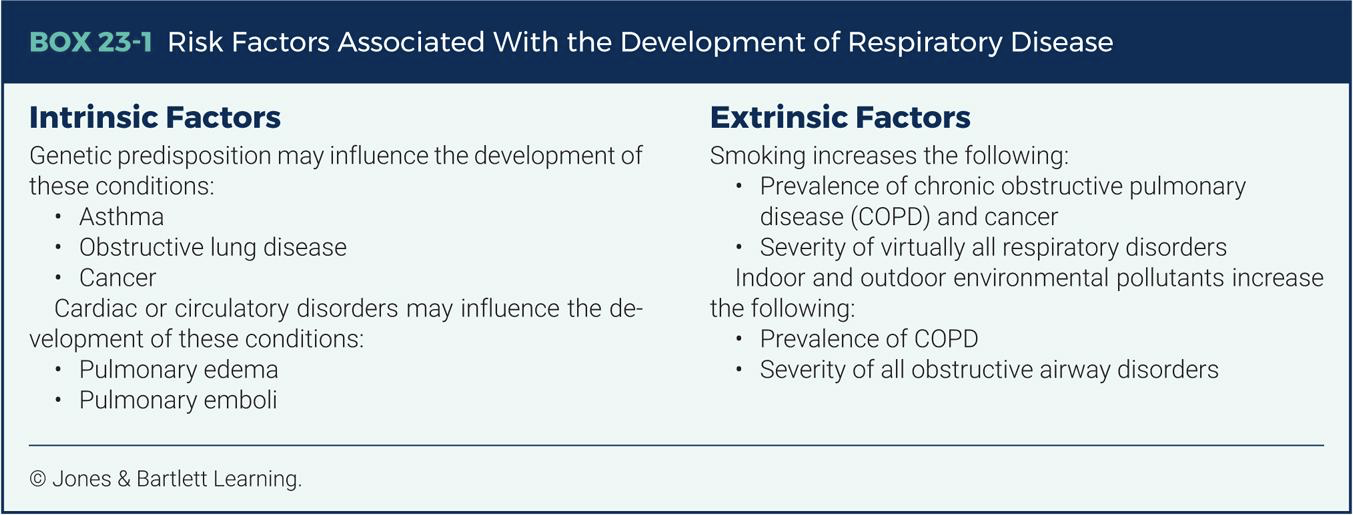
Risk Factors Associated With the Development of Respiratory Disease - Intrinsic Factors
Genetic predisposition may influence the development of these conditions:
Asthma
Obstructive lung disease
Cancer
Cardiac or circulatory disorders may influence the de-velopment of these conditions:
Pulmonary edema
Pulmonary emboli
Risk Factors Associated With the Development of Respiratory Disease - Extrinsic Factors
Smoking increases the following:
Prevalence of chronic obstructive pulmonary disease (COPD) and cancer
Severity of virtually all respiratory disorders
Indoor and outdoor environmental pollutants increase the following:
Prevalence of COPD
Severity of all obstructive airway disorders
Ventilation
Air movement into and out of lungs
To occur, following must be intact:
Neurologic control
Nerves between brainstem and respiration muscles
Functional diaphragm and intercostal muscles
Patent upper airway
Functional lower airway
Alveoli functional and not collapsed
Emergency treatments: ensuring upper and lower airways are open and clear and providing assisted ventilation
Diffusion
Movement of a substance from area with a higher concentration of particles to area with a lower concentration
Results in an even distribution of particles within the medium
Occurs between air-filled alveoli and pulmonary capillary bed
The following must be intact:
Alveolar and capillary walls that are not thickened or damaged
Interstitial space between alveoli and capillary wall that is not enlarged or filled with fluid
Emergency treatment
Providing high-concentration oxygen
Reducing inflammation in interstitial space
Identify underlying cause
Perfusion
Circulation of blood through lung tissues
The following must be intact:
Adequate blood volume
Adequate hemoglobin in the blood
Pulmonary capillaries that are not occluded
Efficient pumping by the heart, providing a smooth flow of blood through the pulmonary capillary bed
To treat perfusion problems:
Ensure circulating blood volume and hemoglobin levels are adequate
Respiratory Failure
Syndrome in which respiratory system fails in one or both of its gas-exchange functions
Key signs of impending respiratory failure
Decreasing SaO2 level despite oxygen therapy
Increasing ETCO2 level
Evidence of fatigue
Decreasing consciousness
Nasal flaring
Seesaw ventilation
Arrhythmias
Cyanosis
Primary assessment
Focus is to detect and manage life-threatening conditions
Signs of life-threatening respiratory distress
Alterations in mental status
Severe cyanosis
Stridor
Inability to speak one or two words without dyspnea
Tachycardia
Pallor and diaphoresis
Retractions/use of accessory muscles to assist breathing
Note any abnormal breath sounds and patient position.
Focused history
Ascertain chief complaint
Obtain focused history using OPQRST
Obtain medication history
Secondary assessment
Guided by paramedic’s general impression of patient and patient’s chief complaint
Note patient’s:
Position
Mental status
Ability to speak
Respiratory effort
Skin color
Obtain vital signs:
Pulse rate
Blood pressure
Respiratory rate
Assess patient’s face and neck for:
Pursed-lip breathing
Grunting
Nasal flaring
Use of accessory muscles
Inspect chest for injury or indicators of chronic disease.
Examine extremities for:
Peripheral cyanosis
Pitting edema
Clubbing of the fingers
Asterixis
Carpopedal spasm
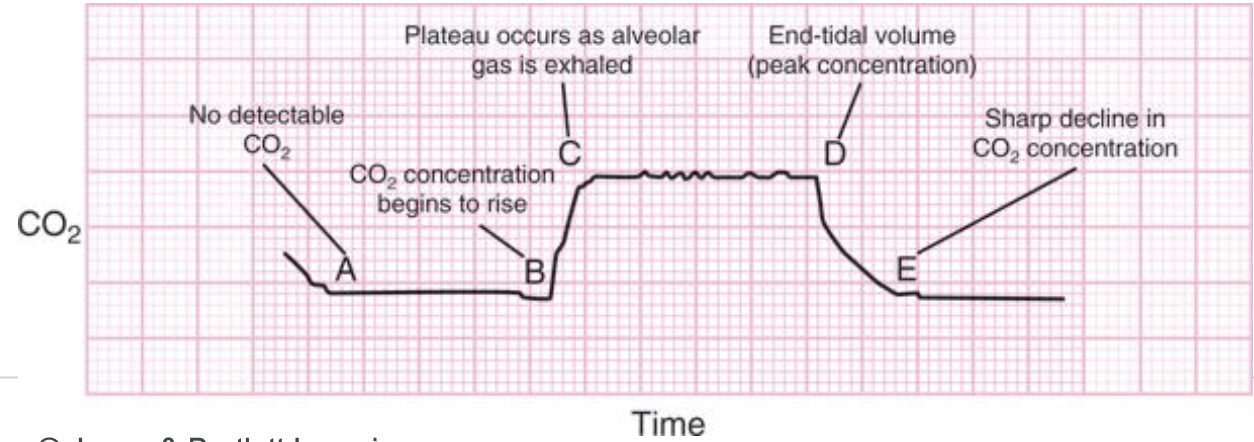
Diagnostic Testing: Capnography
Noninvasive monitoring technique used in the prehospital setting
Provides information regarding:
Ventilatory status
Effect of interventions
Correct tracheal tube placement
Numeric and graphical representation of carbon dioxide concentration exhaled through breath
Capnography
Diagnostic Testing: Peak Flowmeters
Measure a patient’s peak expiratory flow rate (PEFR)
Used most often to help determine severity of an asthma attack
Require cooperative patient
Obstructive Airway Disease
Triad of diseases that often coexist: bronchitis and emphysema (COPD), and chronic obstructive asthma
Major health problem affecting nearly 41 million people in US
Predisposing factors: smoking, environmental pollution, industrial exposures, and various pulmonary infectious processes
Chronic Bronchitis
Characterized by an increase in number and size of mucus-producing glands
Low PO2 level
Frequent respiratory tract infections
Irreversible changes in the lung may result in:
Emphysema
Bronchiectasis
Emphysema
Results from pathologic changes in lungs
Characterized by:
Permanent abnormal enlargement of air spaces beyond terminal bronchioles
Destruction and collapse of alveoli
Over time, chest becomes barrel-shaped from air trapping.
Full deflation of lungs becomes more difficult; eventually, it becomes impossible.
Assessment & Management of COPD
Patient usually has one or more of:
Acute episode of worsening dyspnea manifested even at rest
Increase or change in sputum production
Increase in malaise that accompanies disease
Other physical findings include wheezes, rhonchi, and crackles.
Management
Administer oxygen, NIPPV, and drug therapy.
Obtain a thorough medical history.
Establish IV line.
Apply cardiac monitor.
Medications
Beta agonists
Nebulized anticholinergic
Steroids
Asthma
Reactive airway disease
Most common chronic disease of childhood
Exacerbating factors tend to be extrinsic in children and intrinsic in adults.
Childhood asthma often improves or resolves with age.
Adult asthma usually is persistent.
Pathophysiology of Asthma
Occurs in acute episodes of variable duration
Creates excessive demand on muscles of respiration
Leads to greater use of accessory muscles and respiratory fatigue
Complications:
Pulmonary edema
Lobar atelectasis
Pneumonia
Tension pneumothorax
Assessment of Asthma
Patient usually in obvious respiratory distress
Note mental status.
Obtain initial history, including any previous intubations.
Prolonged expiratory phase may be noted on auscultation.
Wheezing is usually heard.
Capnography waveform often has shark-fin appearance.
Management of Asthma
Oxygen therapy
Drug therapy
Nebulized albuterol
Corticosteroids
Nebulized magnesium sulfate
NIPPV
IV fluids for rehydration
Transport in position of comfort
Advanced airway management if indicated
Status asthmaticus
Severe, prolonged asthma attack not stopped with repeated doses of bronchodilators; true emergency
Treatment is same as for acute attacks, but more urgent.
Provide IV fluids.
Administer high-concentration oxygen.
Anticipate need for intubation and aggressive ventilator support.
Pneumonia
Group of specific infections that cause acute inflammatory process of respiratory bronchioles and alveoli
Caused by bacterial, viral, or fungal infection
Typical signs and symptoms:
Productive cough
Pleuritic chest pain
Tachypnea
Adventitious breath sounds
Fever that produces “shaking chills”
Management
Provide airway support.
Administer oxygen.
Provide ventilatory assistance as needed.
Administer IV fluids to support blood pressure and to thin and loosen mucus.
Obtain cardiac monitoring.
Transport for evaluation by a physician.
Viral pneumonia
Influenza is the most common cause.
In infants and young children, respiratory syncytial virus is the most frequent cause.
Signs and symptoms include:
Chest pain
Cough
Fever
Dyspnea
Occasionally hemoptysis
General malaise
Auscultation of the chest may reveal:
Wheezing
Fine crackles
Symptoms usually resolve in 7 to 10 days.
Bacterial pneumonia
Pneumococcus bacillus (Streptococcus pneumoniae) is the most common cause.
Instances have declined due to vaccine.
Mycoplasmal pneumonia
Causes mild upper respiratory tract infection in school-age children and young adults
Transmitted by infected respiratory secretions
Signs and symptoms include:
Hypoxemia
Acute shaking chills, fever
Tachypnea, tachycardia
Cough
Sputum production (my be rust colored or yellow, green, or gray)
Anorexia, malaise, flank or back pain, and vomiting
Symptoms usually resolve in 3 to 5 days.
Fungal pneumonia
Caused by environmental fungi
Accounts for small percentage of community-acquired cases
Most common in those with chronic illness or weakened immune systems
Treated with antifungal drugs
Aspiration pneumonia
An inflammation of lung tissue
Results when foreign material enters tracheobronchial tree
Common in the following patients:
Patients with an altered level of consciousness
Patients who are intubated
Patients who have aspirated foreign bodies
May be nonbacterial
Typically called pneumonitis
Poor prognosis
Signs and symptoms vary with scenario and severity of insult:
Dyspnea, cough, bronchospasm
Wheezes, rhonchi, crackles
Cyanosis
Pulmonary and cardiac insufficiency