Oral Biology - Exam 2
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
Periodontium
Supporting structures of teeth
Consists of:
Gingiva (gum)
PDL (ligament around cementum)
Cementum (root of tooth)
Alveolar Bone (bone where teeth rest in)
Cementum
Calcified, avascular, and aneural (however, canaliculi do exist and may connect to dentinal tubule)
Mesenchymal tissue (from dental sac) covering root from CEJ to apex
Provides attachment site for PDL (anchors sharpey fibers)
Protects root dentin and compensates for tooth loss with cementum deposition
More resistant to resorption than bone (helpful for orthodontists)
Can rearrange PDL fibers to repair PDL
Two types: Acellular (primary) and cellular (secondary)
Cementum components
Softer than bone and highest fluoride content
45% inorganic (HA) and 55% organic (collagen and non-collagen)
Extrinsic Fibers
Sharpey fibers
Made in ligament by fibroblasts and attach to cementum (type 1 coated by type 3)
Intrinsic Fibers
Made by cementoblasts and in cementum matricx
Calcified interfibrillar matrix
PGs, GP, and phosphoproteins
Produced by cementoblasts
Cementum formation
Dental papilla cells become odontoblasts that line the pulp and place predentin
HERS is laid down to make root shape but will eventually start breaking down
Surrounding dental follicle (sac) cells contact exposed forming dentin
Cell signaling causes follicle cells to differentiate and become cementoblasts to make cementum until reaching apex
Primary/acellular cementum
Found near CEJ
Made before tooth reaches occlusal plane
Sharpey’s fibers exist (no intrinsic fibers because of lack of cementoblasts)
Incremental lines of Salter
Secondary/cellular dentin
Cellular
Has Sharpey and intrinsic fibers
Found from middle to apex of root
Forms throughout life (not so organized; if occlusal forces occur, it can develop to maintain occlusal height)
Intermediate cementum
Poorly defined zone near CDJ
Remnant of HERS
Highly mineralized
Seals dentinal tubules
Abnormal Cementum Levels
Cemental aplasia or hypoplasia - Absence or decrease
Cemental hyperplasia or hypercementosis - Excess cementum deposition (does not need treatment but extractions can be a bit more difficult)
Cementum Resporption
Physiologic resporption - Done by cementoclasts
Pathologic resorption
Local
Occlusal trauma
Orthodontic forces
Misaligned teeth
Cysts/tumors/pathologies
Systemic
Calcium deficiency
Hypothyroidism
Paget disease
Idiopathic
Appears as resorption lacunae
Reversal line is new cementum deposited in location of removed cementum
Ankylosis
Fusion between cementum and alveolar bone (no ligament)
No mobility
Infraocclusion (below normal occlusal height)
Common in primary teeth
Radiographs may see resorption
CEJ
65% of cementum overlap enamel
30% of cementum meet at enamel
5% of cementum do not meet enamel (dangerous)
Alveolar Bone
Part of maxilla and mandible that form tooth socket
Forms during tooth eruption from dental follicle
“Tooth dependent” (lack of tooth for 6 months includes loss of alveolar bone, trabeculae, and ligament)
Alveolar bone composition
2/3 inorganic (HA)
1/3 organic (90% type 1 collagen + non-collagen proteins)
Harder than cementum, softer than dentin and enamel
HA crystals are parallel to collagen to help reinforce bone strength
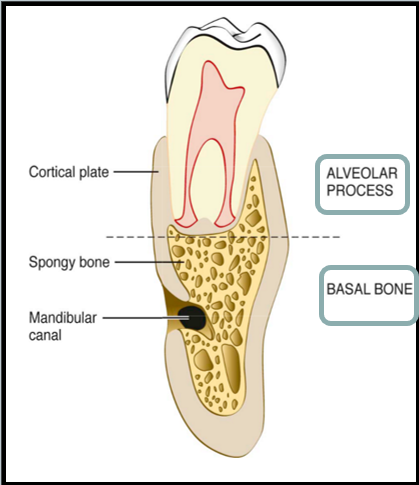
Alveolar and Basal Bone Components
External cortical plate (compact bone)
Alveolar Bone Proper (inner socket wall; also compact)
Bundle bone (histological name) - Where sharpey’s fiber inserts
Lamina dura (radiographic name)
Cancellous Bone
Found between compact bone
Interdental septum
Has blood vessels and nerves
Basal Bone
Below apex and not part of alveolar process
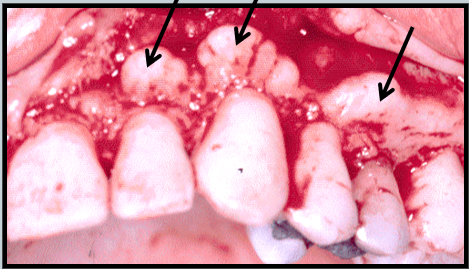
Bony Septum
Interradicular septum (bone between roots)
Interalveolar/interdental septum (bone between teeth)
If root of teeth contact one another, periodontium of one tooth contacts periodontium of another and you may lose septum forming a “boneless window”
Parallel line between adjacent CEJs and interdental crest indicates healthy bone
Periosteum
Covers outer surface of bone
Outer layer of bone has blood vessels, nerves, collagen, and fibroblasts
Inner layer of osteoblasts
Must be surgically maintained because of blood supply
Endosteum
Internal surface of bone
Active site of bone formation and remodeling
Osseous Topography
Shape of alveolar bone depends on arrangement, alignment, position and flaring of tooth roots
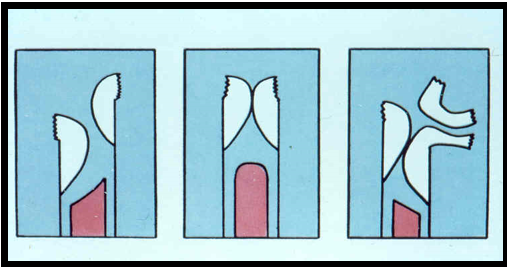
Fenestration
“Window” where exposed root is covered only by periosteum and gingiva, not bone

Dehiscence
Root exposure as V or U shape
From cervical region that extends inferiorly
Anterior teeth, premolars, and mesiobuccal roots of first molars

Buttressing Bone
Extra bone formation as a result of trauma
Not organized bone
Bulge or lip on facial or lingual surface
Exostoses
Bony projections in mandible or maxilla
Can affect dentures but are not symptomatic

Bone Remodeling
Coordinated effort between osteoclasts (large and multi-nucleated cells that use acids and sequester ions) and osteoblasts (lay down osteoid)
Physiologic Tooth Migration
Pressure side undergoes bone resorption (medial side during mesial drift)
Tension side undergoes bone formation (distal side during mesial drift)
Pressure and tension are acted on ligaments from normal and parafunction (tilting/rocking) forces
Interradicular bone is lost in furcation defect as a result of parafuncational forces
Tooth Hypofunction
Occurs when a tooth does not have opposing tooth to antagonize with
Causes PDL to narrow, bony trabeculae decreases, and tooth mobility occurs
Dental Pulp
Derived from ectomesenchyme
Soft connective tissue that functionally supports dentin
Two parts - Coronal pulp (pulp chamber and horns) and radicular pulp (root canals)
Age Affects of Pulp
Pulp gets smaller as you age (root canal becomes more difficult) because of secondary dentin formation
Blood and nerve supply also decrease with age
Number of dead dentinal tracts increase
Reparative (tertiary) dentin is formed as well
Pulp Anatomical Features
Apical foramen - Opening of pulp at root with neurovascular structures
Accessory Canal - Formed from break in HERS that communicates with PDL
Histological Zones of Pulp
Odontoblastic zone (line outer surface of pulp)
Cell-free zone of Weil (cell-free zone inside pulp)
Subodontoblastic plexus of Raschkow (has nerve cells)
Cell-rich zone
Pulp core (has nerves)
Cells include odontoblasts, fibroblasts, mesenchymal cells, macrophages, and stem cells
Pulpal Matrix
Fibers (Type 1 and 3 Collagen)
Ground Substance
90% water bound by PG
GP allow for movement, communication and proliferation of cells
Pulp innervation
Sensory afferents of CN 5
Post-ganglionic sympathetic branches from superior cervical ganglion
Adelta fibers
Myelinated fibers with sharp localized pain when dentin is first exposed
C fibers
Nonmyelinated fibers that are slow conducting, dull and diffuse
Most nerves terminate at subodontoblastic plexus while others enter intratubular nerves and do not synapse
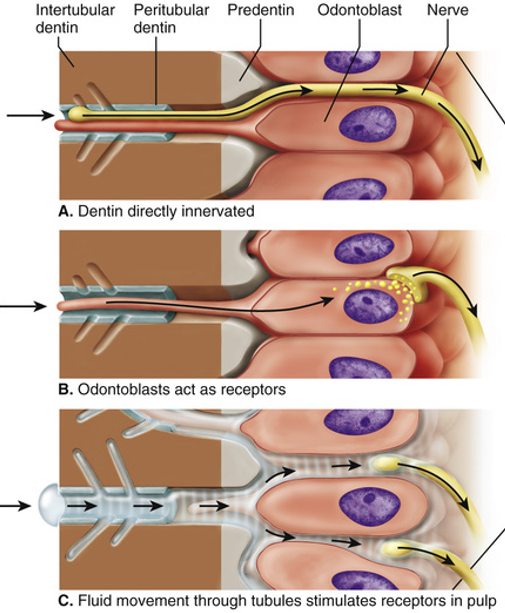
Sensory Perception in Pulp
When you experience extremes of pressure or temperature, it is perceived as pain
Odontoblasts have free nerve endings where pain originates from
Three theories
Dentin directly innervated
Odontoblasts act as receptors
Hydrodynamic Theory - Tooth sensitivity arises from fluid movement within the dentinal tubules
Ion channels are involved in pain perception
Pulp Stones
False pulp stones (concentric) are circular and concentric
True pulp stones (denticles) look like they have actual dentinal tubules
They can be free floating or attached to pulp
Only an issue when you do a root canal and it is in the way
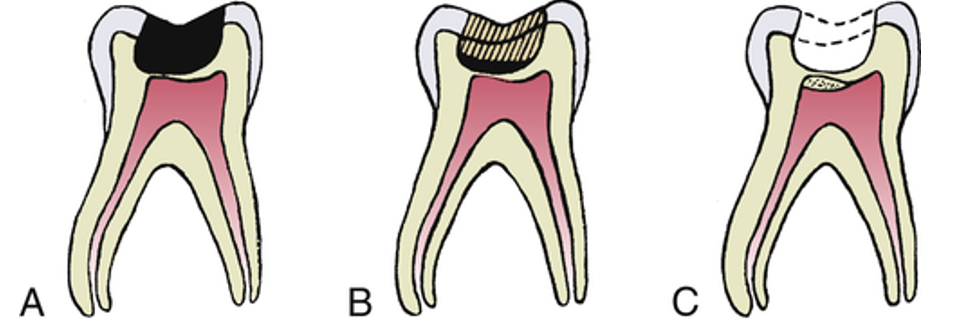
Pulp Exposure
Can happen naturally from caries or from caries excavation
Can be saved or lost be necrosis
Indirect pulp therapy:
Remove a large portion of deep caries but seal with biocompatible cement
After 6-8 weeks, reopen cavity and remove remaining caries. Sound dentin barrier protects the pulp and tooth is ready for restoration
Direct pulp therapy:
Accidentally perforate pulp
Place medicated restoration over exposed pulp
Requirements:
Field needs to be sterile
Size of perforation must be minimal
No pain is felt
Clotting can occur
Calcium hydroxide or MTA stimulate “dentin bridge” formation
More successful in young teeth because apical foramen is larger, contains more cells, more vascular, more tissue fluid, and less collateral circulation
Infected vs Affected Dentin
Infected Dentin
Soft
Must be fully removed
Affected Dentin
Leatherlike
Can be partially removed
Periodontal Ligament
Highly vascular connective tissue
Develops from dental sac/follicle
Connects tooth root to alveolar bone
Radiolucent space between bone and cementum
Portion of fibers that are inside cementum/bone and calcified is called Sharpey fibers
If Sharpey fibers are removed, the perforated bones are called bundle bone
Has ground substance (GAGs, PGs like fibronectin and laminin, and 70% water)
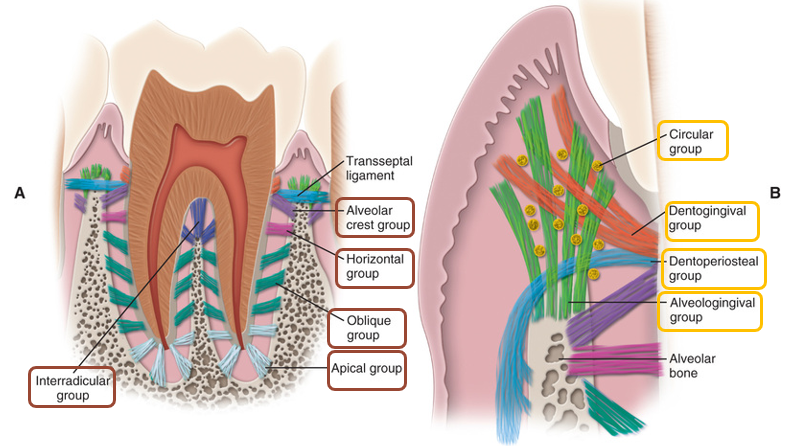
PDL Fibers
Periodontal fibers (Type 1 collagen)
Alveolar crest
Extend obliquely from crest to cervical part of root
Prevents extrusive lateral movement of teeth
Horizontal
At right angles to long axis of tooth
Oblique
Largest group
Extend from cementum obliquely to bone
Bear most vertical masticatory stress
Apical
Irregularly radiate at apical portion of socket
Only on teeth with complete root
Interradicular
Found in furcation areas of multi-rooted teeth
Resist non-axial occlusal forces
Inflammation from periodontal disease affects these fibers and causes bone loss between roots (called periodontal furcation involvement)
Gingival fibers (not between alveolar bone and cementum)
Dentogingival (dentin and gingiva)
Alveologingival (alveolar bone and gingiva)
Dentoperiosteal
Circular (not connected)
Trans-septal (cementum to cementum of adjacent teeth)
PDL Fiber Composition and function
80% Type 1 collagen, 20% Type 3 collagen
Collagen fiber proteins have high glycine, proline, hydroxyglycine, and hydroxyproline
Fibronectin is needed for tooth structure attachment from collagen fibers to cementum/bone
Elastic fibers have oxytalan which run parallel to root and attach to cementum in cervical 1/3rd. They regulate blood flow and support blood vessel
PDL fibers have high turnover rate due to occlusion functional demands
PDL Cells
Connective tissue cells
Defense cells/Immune system cells
Neurovascular cells
Fibroblasts (principal cells of PDL, ovoid or spindle-shaped, synthesis of collagen)
Cementoblasts
Osteoblasts
Osteoclasts
Odontoclasts
Epithelial Rests of Malassez
Remnant of HERS for periodontal tissue maintenance by acting as stem cells
Calcify to become cementicles (asymptomatic)
Can proliferate to form lateral or periapical cysts
PDL Functions
Physical - Transmits and resists occlusal forces to bone (tipping/tilting, bodily, extrusive/pulling, intrusive/pushing, or rotational)
Different types of forces occur: axial, horizontal, shear, etc
Tensional theory - PDL fibers are normally relaxed, but presence of force tightens fibers and transmit force to bone
Viscoelastic theory - Tightening of fibers causes extracellular fluid movement from PDL to bone. Depletion from PDL causes tightening. Tightening causes blood vessel stenosis, ballooning and arterial back pressure, resulting in tissue fluid replenishing
Formative and Remodeling
Factors affecting tooth movement include transduction (physical force to biologic response), time, and magnitude of force
Hyalinization happens from high force at high-speed resulting in loss of cell activity and vascularity
Undermining resorption happens with hyalinization; resorption happens on other side of bone without compensatory bone formation (BAD)
Nutritional and Sensory
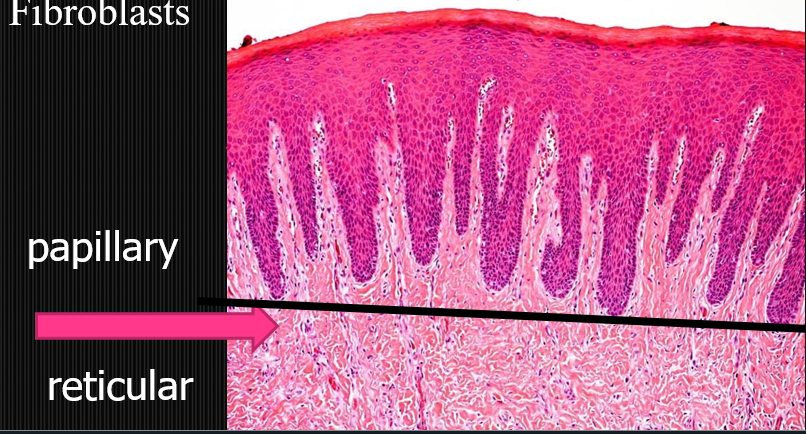
Oral mucosa
Mucous membrane (stratified squamous epithelium)
Sublingual mucosa has thinnest epithelium for drug delivery
May be orthokeratinized (full; cells with no nucleus), parakeratinized (partial; some cells with no nucleus) or non-keratinized
Has underlying lamina propria to protect submucosa (basement lamina may exist separating epithelium and lamina propria)
Papillary layer - Under epithelium with loose CT
Reticular layer - Under papillary layer with dense CT
May have keratohyaline granules (deeply stained in cytoplasm)
Lack of Langerhans cells make mucosa susceptible to allergens (tonsils in mouth compensate for this)
Oral Mucosa Function
Mechanical protection from friction and abrasion
Sensation as taste, touch or pain
Secretion of saliva or sebum
Rete Pegs
Folds of epithelium
Prominent in papillary layer of keratinized epithelium
Not as prominent in non-keratinized epithelium
Submucosa
Submucosa may exist with blood vessels or nerves along with salivary glands and adipose tissue
May have muscles and bone underneath submucosa
When submucosa is absent, mucosa is tightly bound to bone (mucoperiosteum such as palatine raphe or attached gingiva) using its own rete pegs
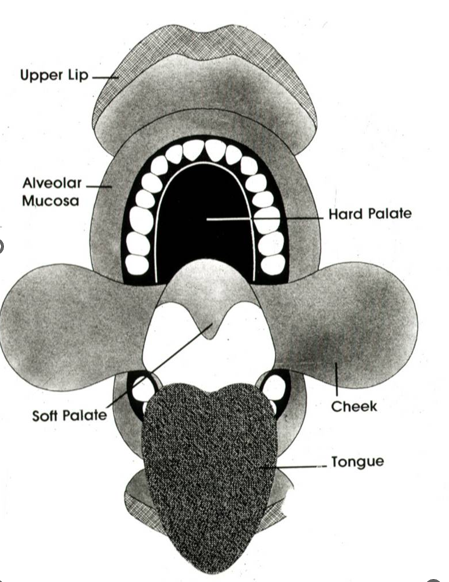
Classification of Oral Mucosa
Based on functions:
Resistance to abrasion of keratinized epithelia
Flexibility of non-keratinized epithelium
Classification
Specialized mucosa (dorsal side of tongue)
Papilla and taste buds, lamina propria, and tongue muscles
Can be keratinized or non-keratinized
Filiform is most numerous, covers entire dorsal tongue, but no taste buds
Fungiform is mushroom shaped on anterior tongue with taste buds
Circumvallate is largest in size and along sulcus terminalis surrounded with taste buds on lateral surface of trench (has serous von Ebner glands)
Foliate is at posterolateral border and has furrows
Masticatory mucosa (gingiva and hard palate) is keratinized
Keratinized stratified squamous epithelium, lamina propria, and bone
Orthokeratinized to resist abrasion and heat
Has deep rete pegs for maximum adhesion and resisting movement
Free and marginal gingiva has sulcular epithelium
Attached gingiva has stippling and includes mucogingival junction
Interdental papilla
Col is valley-like depression between teeth where inflammation and periodontitis start
Lining mucosa (lips, cheeks, floor of mouth, alveolar bone, soft palate, ventral surface of tongue) are non-keratinized
Non-keratinized stratified squamous epithelium, lamina propria, submucosa, and muscle
Highly flexible
Epithelium is thin
Mucocutaneous Junction
Transition between skin and oral mucosa (Vermillion border)
Vermillion zone which is thin keratinized epithelium, lacks salivary glands, and has capillary loops in papillae
Intermediate zone is between vermillion zone and labial mucosa and has para-keratinized stratified squamous epithelium
Hard Palate
Masticatory Mucosa
Palatine or median raphe (mucoperiosteum)
Anterior region (mucoperiosteum)
Anterolateral (adipose tissue)
Posterolateral (salivary glands)
Should not do injections here because of lack of submucosa preventing spreading of fluid
Dentogingival Junction
Has junctional epithelium at floor of gingival sulcus derived from REE and epithelial attachment (“glue”) consisting of basal lamina that have hemidesmosomes (to attach to enamel)
Basal laminas are on either end of epithelial cells and meet at CEJ
Extends apically along root to form seal
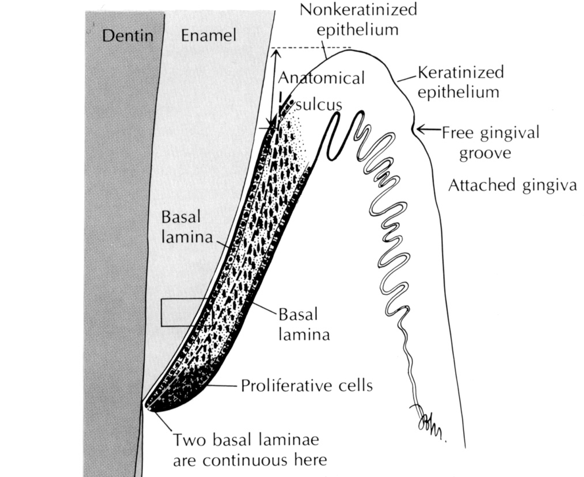
Gingival Sulcus
Area between unattached gingiva and tooth and above junctional epithelium
Healthy sulcus does not have rete pegs (it indicates inflammation)
Gingival, Sulcular, and Junctional Epithelium
Gingival Epithelium and Sulcular Epithelium mature because they are superficial and receive instructive influences
Junctional epithelium does not mature because it is lateral and has permissive influences. Hemidesmosomes can exist on both sides of epithelium. Also provides defense against periodontal bacterial infection
Gingival epithelium is not supported by CT containing inflammatory cells. Has keratinization
Sulcular and junctional epithelium is supported by CT containing inflammatory cells. Has no keratinization
Junctional epithelium can only proliferate apically with help of inflammatory cells causing periodontal pocket and attachment recession
Fordyce’s spots
Sebaceous glands
Inner buccal and corners of mouth

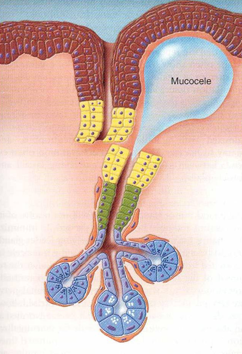
Mucocoele
Bubble in mucosa that is fluid filled caused by blockage of salivary glands or misalignment of gland and duct
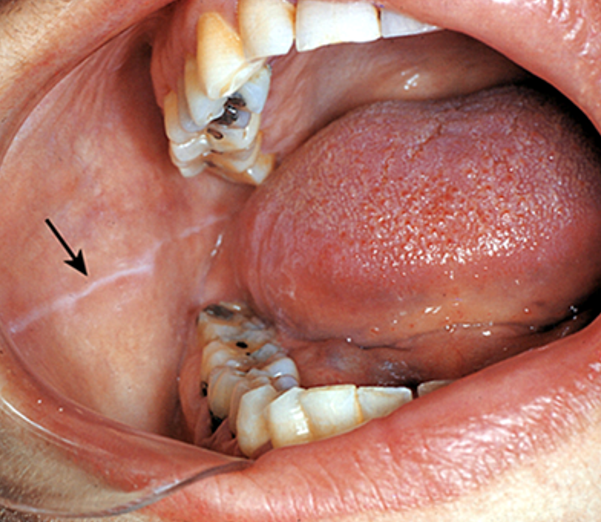
Linea Alba
Chronic irritation of teeth against buccal mucosa causes keratinization of lining mucosa
Results in white line
Black Triangles
“Open gingival embrasures” caused by interdental papillae not filling space between teeth
Can be normal or sign of dental problems like veneers or implants
Age Changes to Mucosal Tissues
Smoother and drier
Thinner epithelium
Losing filiform papillae and Langerhans cells
Ventral side of tongue starts having varicose veins