Ischaemic heart disease
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
IHD
▪ Ischaemia: insufficient blood supply (oxygen and nutrients supply), due to CAD or increased demand of oxygen or nutrients that can’t be satisfied.
The cardiac muscle of the myocardium doesn’t extract oxygen and nutrients from the blood that is flowing through the atrium into the ventricles. Heart muscle cells depend on its own blood supply via the coronary arteries
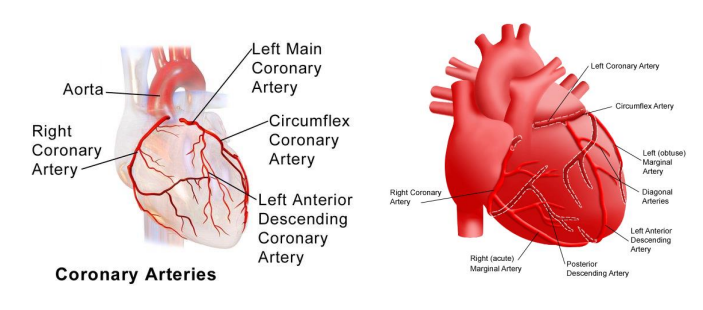
Coronary circulation
left coronary arteries divide into two branches
the bigger the artery that is affected the worse the ischaemia
Ischaemic heart disease causes
Reduction of blood supply
Atherosclerosis
Embolus
Vessel inflammation
Vasospasm of coronary arteries
Increased demand
tachycardia
left ventricle hypertrophy - ventricle wall becomes thicker so more and bigger cells require oxygen
exertion due to exercise
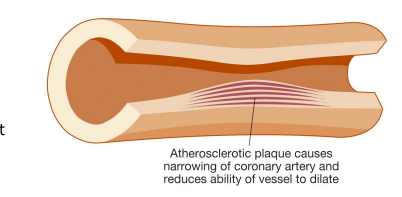
Atherosclerosis
Formation of plaque in the coronary arteries reduces the vessel lumen and therefore the blood flow
Modifiable and non-modifiable risk factors
Modifiable
hypercholesterolaemia
HT
diabetes
diet
sedentarism
obesity
smoking
alcohol
stress
Non - modifiable
age
genetics
gender
ethnicity
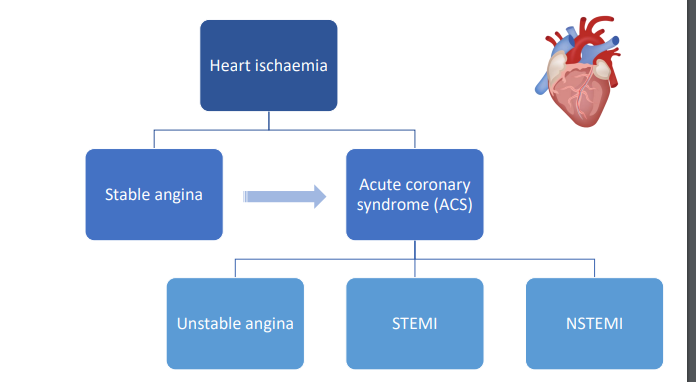
IHD classification
Angina (angina pectoris)
Partial reduction in the blood flow
Stable or unstable
usually does not result in permanent damage of the myocardium
Myocardial infarction - heart attack
prolonged or complete blockage of the blood flow
necrosis of cardiac muscle cells and replaced by scar formation which is more fibrous so cannot pump
permanent damage
heart function becomes reduced
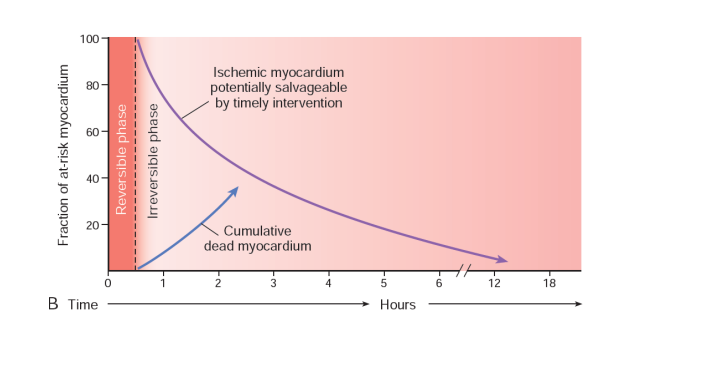
Symptoms depend on rate at which blood flow is reduced
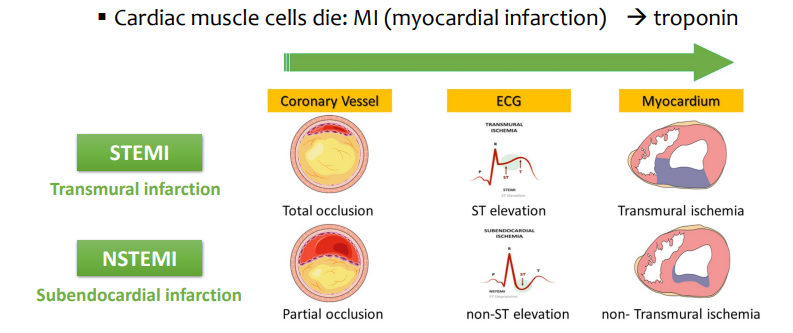
STEMI AND NSTEMI are prolonged ischaemia or full blockage of the blood flow - cardiac muscle cells die
IHD - Stable angina
Atheroma in coronary artery reducing the blood flow
Stable: plaque with fibrous cap that prevents rupture
flow is reduced but nothing else happens
No ECG changes
Intense chest paint
Physical exertion - increased demand of oxygen
Emotional stress - increased demand of oxygen
symptoms relieved by rest
IHD – Unstable angina
Rupture of the surface of an atheroma → platelet plug & thrombus formation. Break in lining causes haemostasis
Unstable: unpredictable, fast progression, can happen at any time regardless if there is oxygen demand or not
Normal ECG or subtle changes
Intense chest paint
Mild exercise
At rest
Symptoms not relieved by rest
urgent treatment
avoid progression to MI
IHD - STEMI AND NSTEMI
Rupture of the surface of an atheroma (both are usually a consequence of atherosclerotic plaque that breaks from the vessel) → platelet plug & thrombus formation
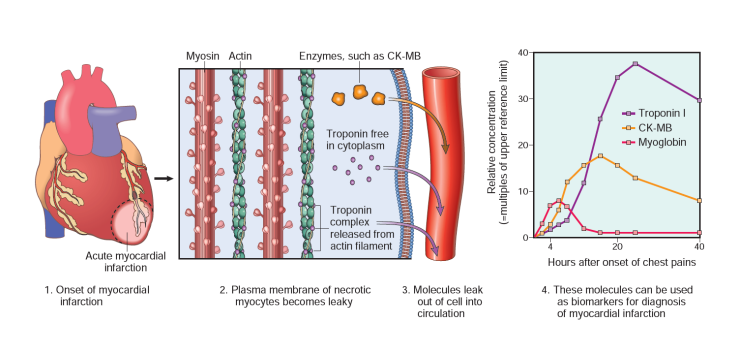
Cardiac muscle cells die: MI (myocardial infarction) → troponin
MI can also happen as a result of coronary artery dissection, for e.g. in accident or dure to spasm because of cocaine consumption or emotional stress
if troponin is found then that means cardiac cells are dying
IHD - Molecular mechanisms of MI
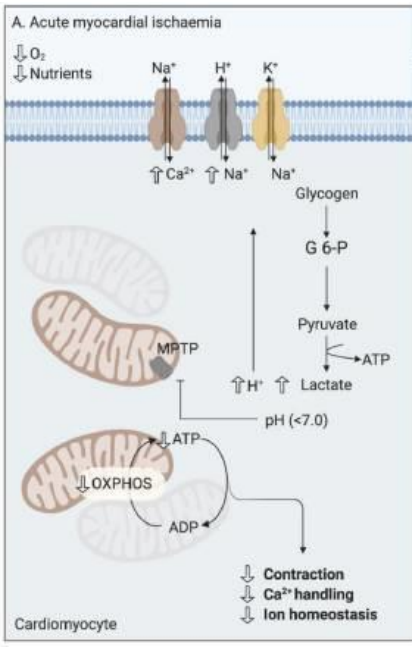
Cardiomyocytes are dependant on oxygen to produce ATP in a process called oxidative phosphorylation. If oxygen is reduced then cellular metabolism switches to glycolysis resulting in build up of lactate and hydrogen ions. This lowers the pH affecting ion transport in the cell membrane, leading to increased calcium ions in cell, oxidative stress due to the production of R.O.S. Furthermore contractility of cells is reduced as there is less ATP being formed. This induces cell death by apoptosis or necrosis. Therefore there is contractile dysfunction, decreasing CO, and potentially leading to death
Release of extracellular compounds can cause arrythmias and ventricular fibrillation which decrease CO, leading to death
***
Graph
Troponin
As cardiac muscle cells die the plasma membrane becomes leaky, and release cellular components to the blood stream which can be measured and used as a diagnostic tool
most important is troponin which is a protein that is essential for the contraction of cardiac muscle
in angina troponin levels are normal as cells aren't dying
cardiac protein, CKMB, myoglobin,
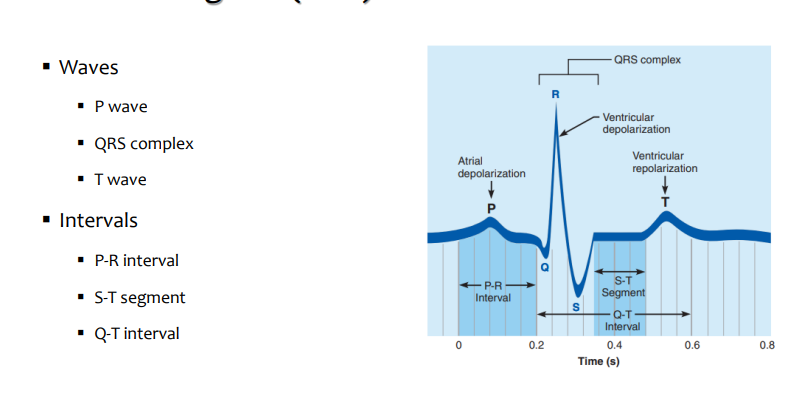
ECG
Stable angina pharmacology
Symptom relief (pain)
Short-acting nitrates
symptom control
beta blocker OR calcium channel blocker
beta blacker AND calcium channel blocker
alternative medications : long acting nitrates, nicorandil, ranolazine, ivabradine
beta blocker OR CCB AND alternative medications
comorbidity treatment as plaque will not disappear but need to prevent unstable angina
HT
Diabetes
hyperlipidaemia
preventative treatment
aspirin - deals with oxygen demand by either supplying more or decreasing demand
Nitrates
Short-acting nitrates: GTN spray (glyceryl trinitrate)
Sublingual or transdermal administration
Rapid onset and short action duration
Long acting nitrates : isosorbide mononitrate
oral administration
slower onset of action
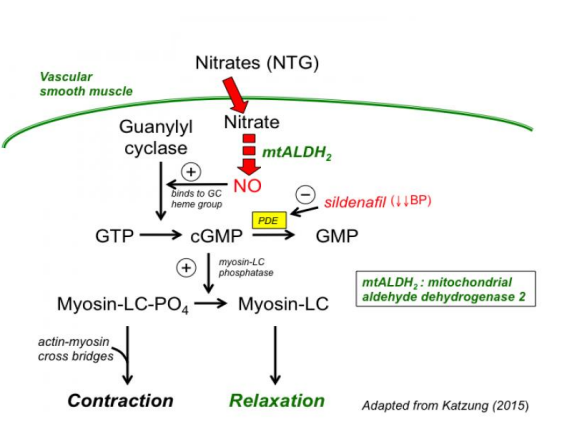
Vasodilators : metabolised with release of nitric oxide that induces vasodilation, reduces cardiac work by reducing preload and afterload. Also improves circulation.
tolerance can be reversed by drug free period
Nitrates being metabolised activates guanine cyclase increasing formation of cGMP. This activates protein kinase G leading to cascade which causes phosphorylation of the myosin light chain
Beta-blockers (Beta1-adrenergic receptor blockers)
Decrease cardiac output
Β1-adrenergic receptors are primarily found in the heart
Their activation increases the rate and strength of cardiac contraction
Drugs inactivating them:
↓ HR
↓ Stroke volume
↓ CO
therefore reducing oxygen demand at myocardium
Calcium channel blockers
Decrease entry of Ca2+ into vascular smooth/cardiac muscle cells
Calcium is needed for both cardiac and smooth muscle contraction
Dihydropyridines: affect blood vessels, anti-hypertensive properties
↓ contraction:
↑ vasodilation, ↓Peripheral resistance
↓ afterload, ↓ cardiac work
Non - dihydropyridines: affect heart, anti- arrhythmic properties
decrease contraction and HR
Decrease oxygen demand
****mechanism of action
Nicorandil
Nitrate like action
vasodilation
increased coronary flow
decreased preload
k+ATP channel activator
hyperpolarisation of plasma membrane, reducing electrical activity
vasodilation
Ranolazine
affects Sodium levels → ↓ intracellular calcium
reduces force of contraction without affecting HR
decreased myocardial oxygen demand
Ivabradine
decreases heart rate through affecting ion channels in the sinoatrial node
affects first step in conduction system of the heart
Aspirin
antiplatelet drug
irreversibly inhibits COX1
blocking formation of thromboxane A2 inhibiting formation platelet plug and therefore blood clots
Prophylactic treatment in angina: Prevention of clot formation
Other drugs
Fibrinolytic drugs
Alteplase, streptokinase (plasminogen → plasmin: breaks down fibrin)
Antiplatelet drugs
aspirin
prasugrel/Clopidogrel/Ticagrelor (ADP-mediated platelet aggregation inhibitors, target the ADP receptor in platelets)
Others
antithrombotic drugs (heparin)
analgesics (morphine) for pain
Secondary prevention
Dual antiplatelet therapy
Aspirin + Clopidogrel/Prasugrel/Ticagrelor
Beta blocker
ACE inhibitor
Statin
PPI
GTN spray