1 - Intro to Basic Principles of Physiology
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
Total body water about _____% of total weight.
Total body water about 50-70% of total weight.
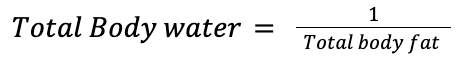
TBW correlates _______ with total body fat.
TBW correlates inversely with total body fat.
What is a key difference between men and women in terms of body composition?
Women tend to have a higher % of body fat (adipose tissue) → ↓ water content in their bodies compared to men
What are the compartments water is divided into?
1) Intracellular fluid (2/3)
2) Extracellular (1/3)
Intravascular
Extravascular/ISF
What type of fluid does the Intravascular compartment include?
Blood
Lymphatic fluid
Synovial joint, CSF-filled spaces
Aqueous & vitreous humors
Interstitial spaces are almost always _____________ spaces.
Interstitial spaces are almost always connective tissue spaces.
What does the solubility of solutes depend on?
concentration
charge
pH
temperature
pressure
miscibility with the solvent
What are the metabolites? From the metabolites, which can create a concentration gradient and osmotic pressure across a membrane?
Metabolites = ions, fats, proteins, or sugars
everything EXCEPT lipids create a conc gradient (lipids can’t cross b/c they are hydrophobic)
Different mechanisms exist for mixing solutes within and moving them between compartments. What are they?
Diffusion
Convective flow
What is convective flow? Provide examples of Convective Flow in the eye.
→ fluid movement caused by temp differences, where warmer fluid rises and cooler fluid sinks,
allows for faster mixing/transport of solutes compared to diffusion
In the eye (3 examples):
Avascular structures live off of aq humor (which has waste + nutrients)
Movement via convection shifts wastes to the anterior chamber
warmer iris (98.6°F) results in particulates (pigment granules, WBC) rising near the iris and falling along the cooler inner surface of the cornea (93.7°F when eye is open)
Uniform mixing/unregulated diffusion is usually undesirable. How do we regulate equilibration between the 3 main compartments within the body?
separate the compartments from each other with an epithelial or endothelial cell layer (semi-permeable membrane)
What is the charge of most proteins?
(-)
What is the charge of most cell surfaces?
(-)
Make a table showing the amount of ions in ECF vs ICF.
Na+
K+
Ca2+
Cl-
HCO3-
pH
Osmolarity
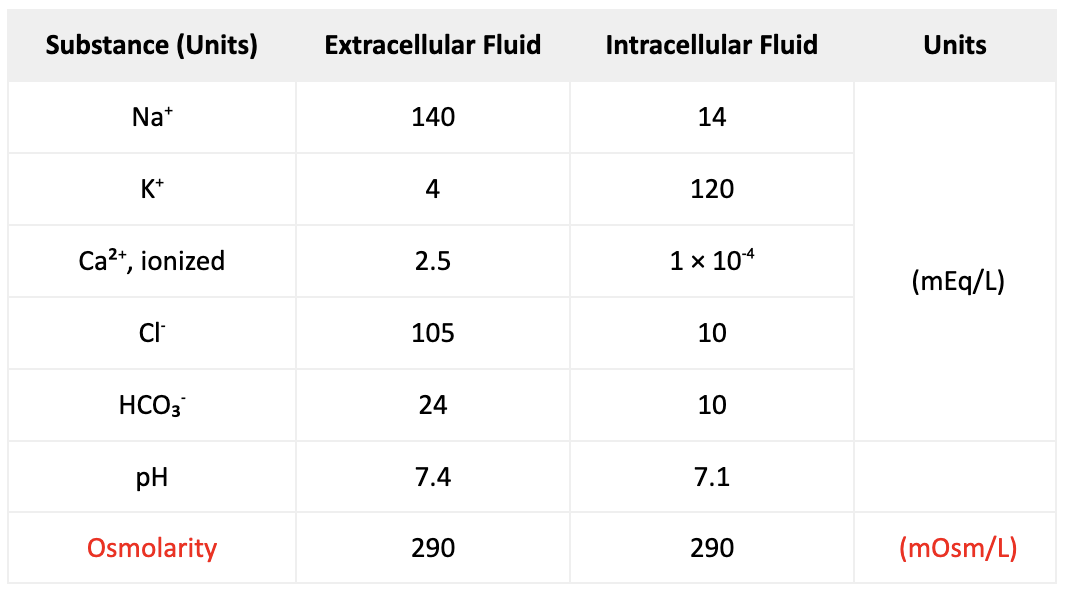
Which two ions are play an important role INSIDE the cell?
Proteins, organic phosphates & K+
Which two ions are play an important role OUTSIDE the cell?
Na+ & Cl-
Why can't proteins and Na+ move passively through cell membranes, and how does this affect ion concentrations?
Proteins are too large to move out of the cell
Na+ cannot passively move through cell membranes (due to selective permeable membrane)
K+ can move in small amounts, but to maintain electrical neutrality, other ions must move in or out
this results in unequal ion concentrations inside and outside the cell
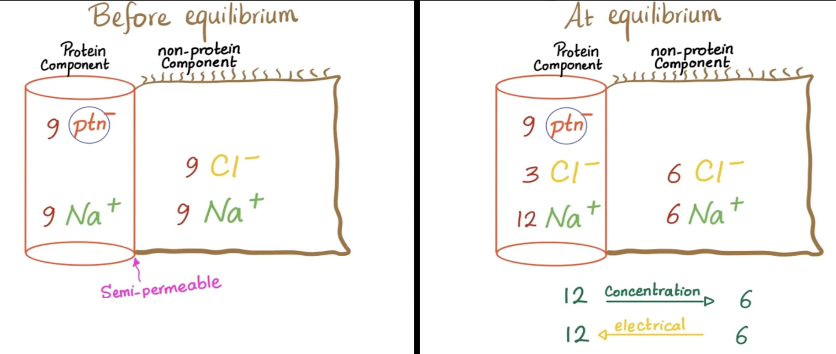
What must each fluid compartment (ICF, extracellular intravascular, extracellular extravascular) maintain?
→ maintain electroneutrality within itself
Electroneutrality: total cations = total anions (in mEq/L)
Net charge = 0
Note: Charges DON’T need to match across compartments
inside can be 9⁺ & 9⁻ while outside is 3⁺ & 3⁻, as long as each compartment is individually neutral
What’s the difference b/w electrical gradients and concentration gradients?
Electrical gradients = sum of the total charges of all ions in that compartment
Concentration gradients = relative concentrations of individual ions across the membrane
What creates the voltage differences across cell membranes?
Electrical and concentration gradients of ions often oppose each other to reach balance
Small differences in ion distribution create charge differences (voltage) across membranes
Cells’ inside is more (-) than the outside
average transmembrane potential is –50 to –70 mV
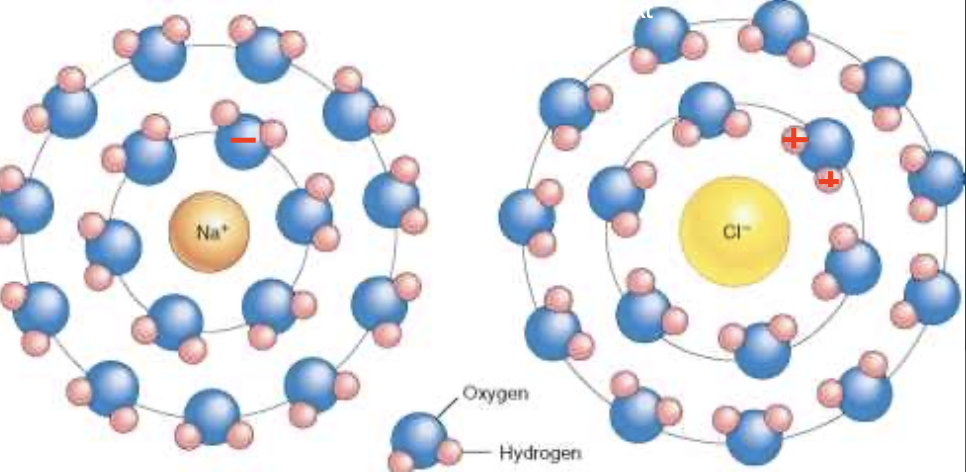
Why can’t Na+ easily diffuse through membranes?
→ due to the hydration Sphere
it’s a chemical structure (e.g., water) that surrounds a solute (Na+ or Cl-) b/c the individual water molecules stick to the ion, forming a sphere
K+ has a smaller hydration sphere, which is why it can diffuse through membranes, whereas Na+ & Cl- can’t easily cross
Why must cytosolic calcium be kept extremely low, and what happens when Ca²⁺ levels become abnormally high?
Outside = 2.5 mEq/L
Inside = 1 × 10-4 mEq/L (very low)
↑ Ca2+ = common signaling trigger (e.g., muscle contraction, insulin release in β-cells)
close GJ
uncouple TJ
↑ permeability b/w epithelial cells
eliminate intercellular communication
What’s the difference between Osmosis and Oncotic pressure? What do both prompt?
Osmosis - involves ions moving toward higher solute concentration.
Oncotic/Colloid osmotic pressure - involves macromolecules (proteins, sugars) moving toward higher solute concentration
both prompt water to move toward higher solute concentration, but only if the solute can’t cross the membrane
as compartments approach equilibrium → force weakens
at equilibrium, no water moves
List the 3 main force vectors.
Electrical gradients (charge differences)
Concentration gradients (for each individual ion)
Osmotic gradients
Why must hyperosmotic agents be used before topical drops when IOP is above 40 mmHg?
IOP > 40 mmHg causes iris ischemia → drops are ineffective
Hyperosmotic agent (oral glycerin or IV mannitol) is given
This ↑ blood osmotic pressure → pulls water out of the vitreous (which is >98% water)
↓ IOP
Drops are added once IOP falls below 40 mmHg
What is the primary difference between the two compartments of extracellular fluid (Intravascular vs Extravascular/ISF)?
[protein]
Plasma (intravascular) = ↑ protein (albumin)
Interstitial tissues (extravascular) = ↓ protein
Why does the extravascular compartment have ↓ protein?
Plasma proteins are large, so they can’t easily pass through endothelial cells in capillaries (since capillaries have tight junctions)
How do plasma proteins, which carry a (-) charge, affect ion distribution?
Small ions redistribute themselves across the membrane to maintain electrical neutrality (since proteins carry a (-) charge and can’t cross the membrane/redistribute)
Plasma proteins repel anions and attract cations → difference in [ion] across the membrane
Plasma will have ↑ [cations -Na+ and K+] & ↓ [anions - Cl-]
What happens to individual concentration gradients when ions redistribute to maintain electrical neutrality?
As ions redistribute, they are affected by their individual ion concentration gradients, which push them in the opposite direction (e.g., if electrical neutrality is pushing one way, concentration gradient pushes the opposite way)
this continues until the 2 forces (electrical neutrality & concentration gradient) are balanced
When is a diffusion potential created?
when a membrane is permeable to an ion, allowing it to move from high to low concentration
What two factors does ion movement affect?
Concentration gradient (diffusion potential)
Charge gradient (electrical potential)
What is electrical potential (in mV)?
is the electrical potential measured across the membrane when ion movement stops (forces are equal)
What does the Nernst equation calculate?
→ equilibrium potential for 1 ion at a time
aka the membrane voltage needed to balance that ion’s concentration gradient
What does the Nernst equation compare?
strength of the electrical force vs. concentration force (gradient) for a single ion
What does membrane potential represent by convention?
Inside of the cell relative to outside
so -70mV membrane potential means the cell’s inside is 70 mV less than the extracellular space
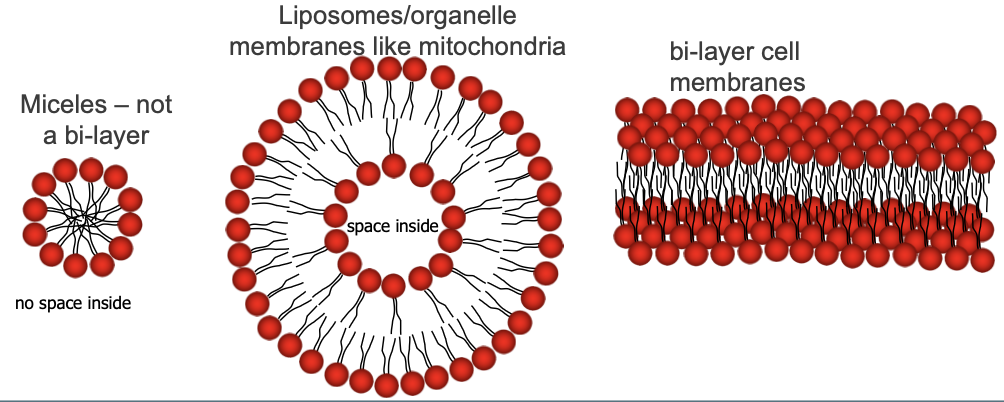
What are some structures the phospholipids (head and tails) assemble into?
Micelles (not a bilayer)
Liposomes/organelle membranes
Bilayers
List some phospholipid bilayer membrane components.
cholesterol
sphingolipids
membrane proteins
glycoconjugates
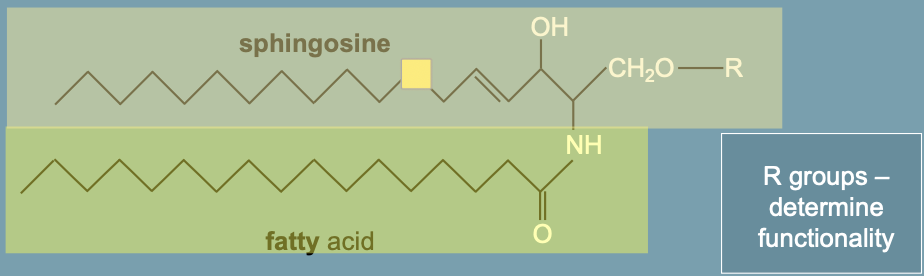
What are sphingolipids?
→ membrane lipids with larger hydrophilic moieties
Function: cell signal transduction (by forming caveolae), cell-cell communication, and endocytosis/uptake of viruses/bac
form "lipid rafts" (areas with more cholesterol)
What are lipid rafts associated with?
Signal transduction (IgE, T/B-cell antigen receptor signaling)
Preferential viral entry
List the types of membrane proteins.
Transmembrane/integral
Peripheral
Lipid-anchored (amphitropic)
List the functions of Transmembrane proteins.
Transport
Enzyme
gated ion channel formation
receptor function/signal transduction
→ these functions are carried out by these proteins acting as channels, ports, receptors, and intercellular junctions
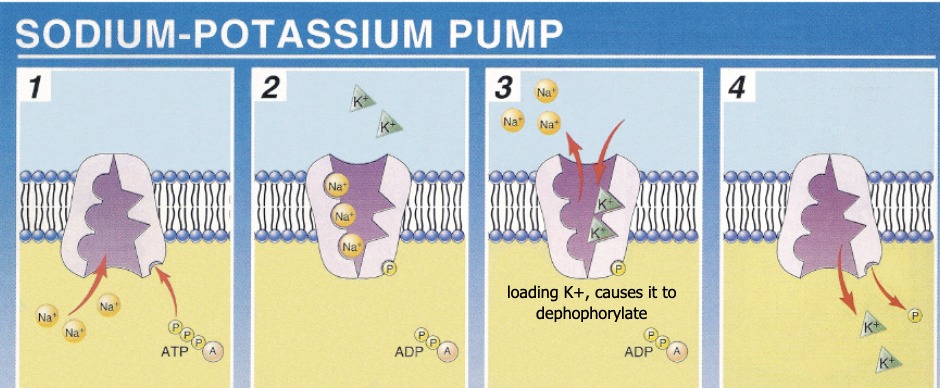
Outline the characteristics of the Na/K ATPase pump.
→ integral membrane protein (enzyme) localized to virtually all cell membranes.
aids in transport, aq production, maintaining corneal transparency, etc
creates the gradients essential for cell function
At rest: 50% of produced ATP runs the Na-K pumps
Cells under stress can add more pumps to the membrane
Mechanism: exports Na to maintain a higher Na gradient outside the cell
Describe the Na/K ATPase pump pathway.
3 Na+ leave and 2 K+ enter
The pump (facing the inside of the cell) binds 3 Na⁺ ions + 1 ATP
ATP → ADP + Pi
Pi attaches to the pump → phosphorylation → pump changes shape → open to the outside
3 Na⁺ released outside
While facing the outside, the pump binds 2 K⁺
Binding triggers the pump to lose the Pi → dephosphorylation → pump changes shape again (original inward-facing shape)
2 K⁺ released inside
Ions can also move using transmembrane proteins that serve as ion channels. What are the 2 main types of regulated ion channels?
1) Voltage gated - controlled by changes in transmembrane potential
2) Ligand gated - controlled by hormones, neurotransmitters & 2er messengers
What do ports, symports, and antiports have in common?
all are integral membrane proteins that don’t use directly ATP
What is a uniport (port)?
→ undergoes facilitated diffusion acting as a channel or carrier protein.
Carrier proteins - bind 1 solute at a time, transporting it WITH the solute gradient
transport occurs only with the solute gradient (not against it)
Channel proteins - open to a stimulus allowing free flow of specific molecules
There are many ways the opening of uniporter channels may be regulated. What are they?
1) Voltage - regulated by the diff in voltage across the membrane
2) Ligand - regulated by a ligand binding to the intracellular or extracellular side of the cell
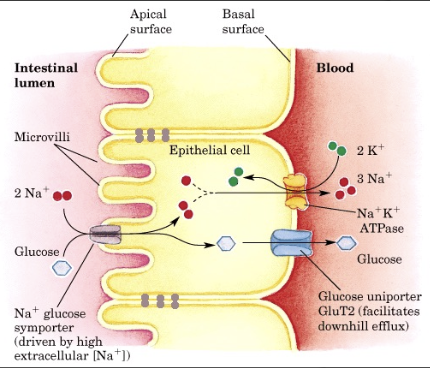
What are symports? Provide an example.
→ simultaneously move diff molecules/ions across the membrane in the same direction
1 ion moves passively along its electrochemical gradient, dragging the 2nd molecule AGAINST its conc gradient (to an area of higher concentration)
Eg: SGLT1 transports Na+ & glucose from the intestinal lumen into the bloodstream (which has higher glucose concentration)
Eg: Gatorade + electrolytes
What are antiports?
→ move molecules in opposite directions
1 molecule moves WITH its conc gradient, while the other moves AGAINST
same valence & sign between the 2 molecules
Ex: Na+/Ca2+ exchanger removes cytoplasmic Ca2+ to maintain low levels
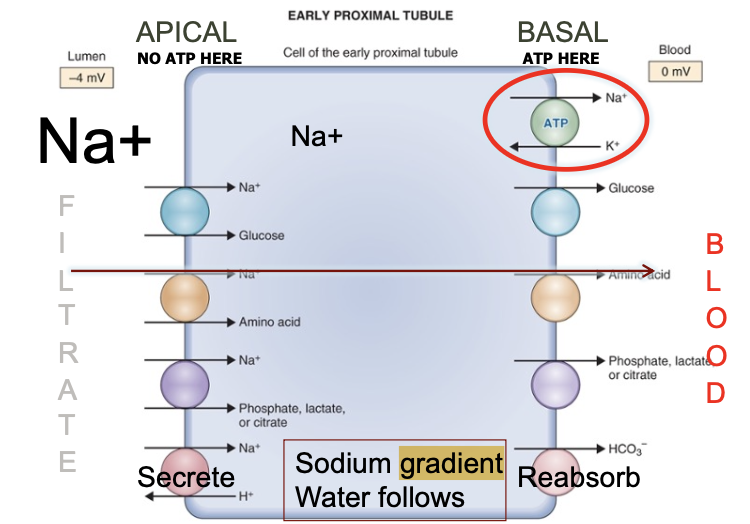
Virtually all transport of ions, amino acids, and glucose exploits the Na-K ATPase pump's energy-dependent movement of Na. Describe how.
Na is pumped out on the basal side → creates ↓[Na]intracellular
ATP use occurs on the basal side but not the apical side
So Na enters through the apical side
This gradient drives ports, symports, and antiports, moving other ions/glucose AGAINST their gradients + moving water toward Na via osmosis
Once inside the cell, these substances move WITH their concentration gradients (high to low) and enter the blood
Membrane Receptors
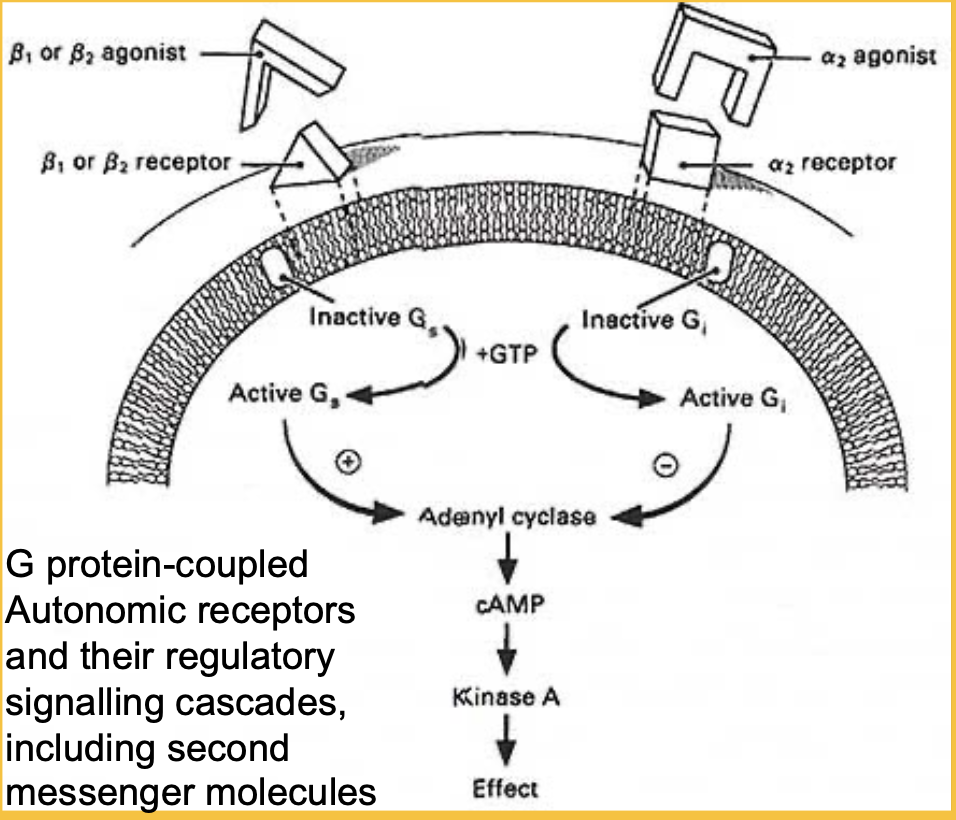
From the β1, β2, α1, α2 receptors, which ones share the same cascade? What is this cascade?
β1, β2, α2 - share the same type of G-protein signaling, but produce different cascades depending on the tissue (e.g., iris, vascular smooth muscle)
Ligand binds to the GPCR
This activates the G-protein inside the cell.
The G-protein becomes phosphorylated (activated form)
Activated G-protein triggers a signal transduction cascade (STC)
This leads to upregulation of adenylyl cyclase (AC)
AC increases cAMP production.
Increased cAMP activates PKA
PKA produces the cellular effect (e.g., making aq humour)
β1 & β2 pathway - promote the “effect”
α2 pathway - inhibits the “effect” (via the same pathway)
β-blocker = α-agonist
Membrane Receptors
In the signalling cascade, what’s the difference between an agonist and antagonist?
Agonists bind + activate the receptor (like pressing the gas pedal)
Antagonists (blockers) bind the receptor but prevent activation (like taking your foot off the gas pedal)
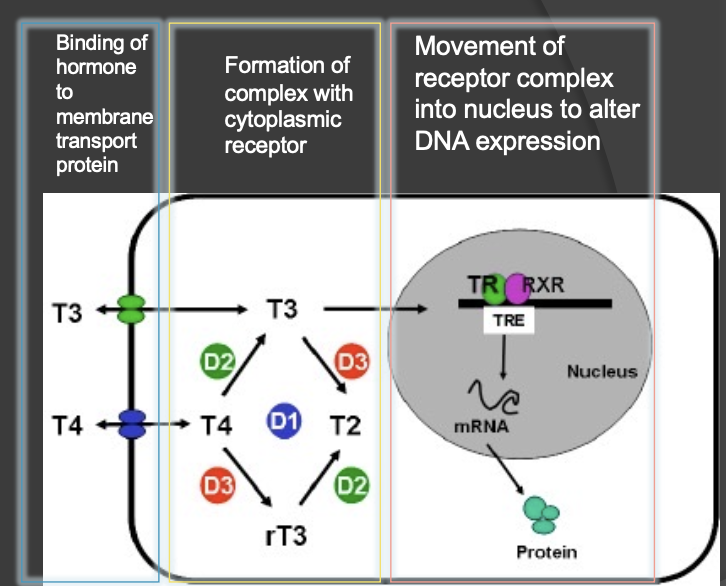
Cytoplasmic Receptors
How do the cytoplasmic receptor pathways differ from other receptor pathways?
→ Agonists (e.g., T3, T4) bind to cytoplasmic receptors, enter the nucleus, and alter DNA transcription
slower pathway (e.g., since steroids also follow this process, they must be tapered slowly)
Agonist binds to transmembrane membrane transport protein (lipid-soluble)
Agonist binds to cytoplasmic receptor
Receptor complex moves to the nucleus to change DNA expression
List the functions of Peripheral proteins.
Transport
Enzyme (e.g., blood clotting cascade)
Structure (attach to cell surfaces)
e- carriers (ETC in mit)
regulators (e.g., apoptosis)
How do tight junctions affect membrane protein diffusion?
TJ restrict the diffusion of membrane proteins to the apical or basal surface of the cell, maintaining polarity
Proteins such as pumps, pores, and channels are localized to their respective domains (apical or basolateral)
Why must Na-dependent ports be on the opposite side from Na+/K+ ATPase pumps?
→ to maintain a gradient
If both are on the same side of the cell, the system won’t function properly
What happens when tight junctions in iris blood vessels break down?
→ Allows plasma proteins to enter the aq humor
Effect: Plasma proteins scatter light, causing "flare" (light distortion in the eye)

What are Gap junctions?
→ Multiple focal junctions that allow direct electrical communication b/w cells via the transfer of 2er messengers (IP₃, Ca²⁺) = allow groups of cells to act as a “syncytium”
Different connexin subunits can create different single-channel conductances (allow ions to pass easily/not easily) (≈30 pS to 500 pS), pore sizes & charge selectivity (+ or -)
allows molecules <1000 Daltons to pass
large biomolecules (e.g., nucleic acids, proteins) can’t pass through gap junctions
Why are gap junctions important in the lens?
Lens is avascular, and added cell layers ↓ nutrient access
GJ allow nutrients and metabolites to move from superficial, metabolically active cells to deeper lens fiber cells
Which connexins are found in lens fiber cells?
Connexins Cx46 and Cx50
Which connexin is found in the anterior lens epithelium?
Connexin Cx43
How much of the plasma membrane do gap junctions account for in lens cells?
30–60% of plasma membrane area (compared to 3–4% in typical epithelial cells)