09 - Periapical Pathoses
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
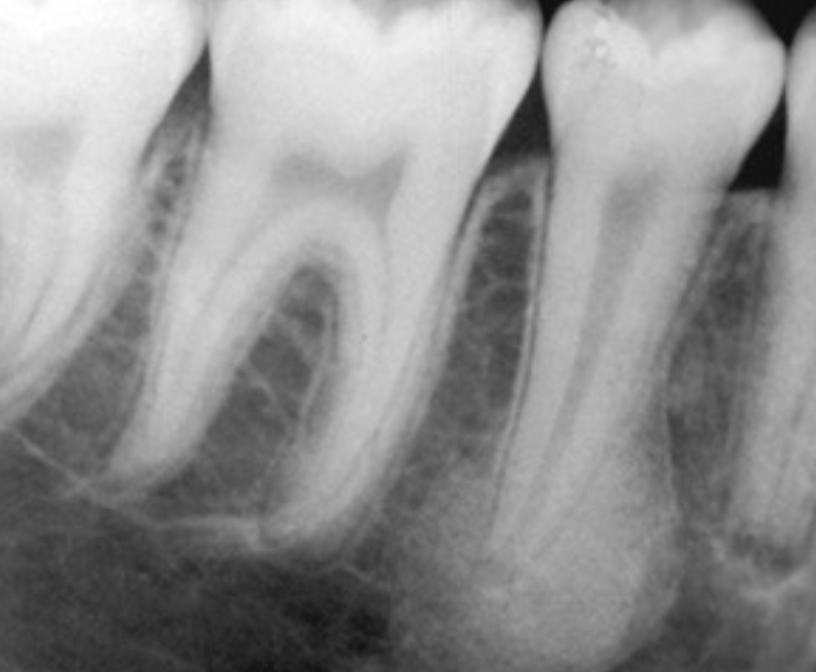
radiographic components of teeth
can see enamel, dentin, pulp
cementum is radiographically indistinguishable from dentin
pathogenesis
apical periodontitis is not the same as periodontal disease
caused by pulp necrosis → bacterial invasion or tooth trauma
necrotic pulp metabolites exit root apex and trigger inflammation in PDL and bone, causing apical periodontitis
early-stage vs late-stage caries
early-stage caries → incipient decay
late-stage caries → decay spreads more rapidly in all directions when it passes through DEJ
dentin is less mineralized and more prone to decay
pulp may recede from decay due to deposition of secondary dentin
periapical inflammatory disease
synonymous terms: apical periodontitis, periapical/radicular/periradicular abscess, periapical/radicular/periradicular granuloma, periapical/radicular/periradicular cyst
many terms are histopathologic, requiring microscopic confirmation and not radiographic imaging
rarefying vs sclerosing osteitis
rarefying → increased radiolucency
sclerosing → increased radiopacity
apical periodontitis
inflammation and destruction of apical periodontium of pulpal origin
no periapical changes are noted yet
sometimes cannot be diagnosed by radiographic images alone
variable presentation → asymptomatic, mild toothache, severe pain and swelling
clinical features of periodontitis
acute stage
severe pain, swelling, fever, lympadenopathy
tooth mobile, tender to percussion, may be elevated in socket
chronic stage
may develop from acute lesion or arise de novo
often flare-ups of tooth pain
tooth may be mobile or percussion-sensitive asymptomatic or with intermittent
imaging examination
purpose to assess extent of lesion and identify involved teeth
initial imaging → intraoral periapical and occlusal images, panoramic radiographs
early lesions → subtle changes in periapical tissues
diagnosis can rely on clinical signs and symptoms
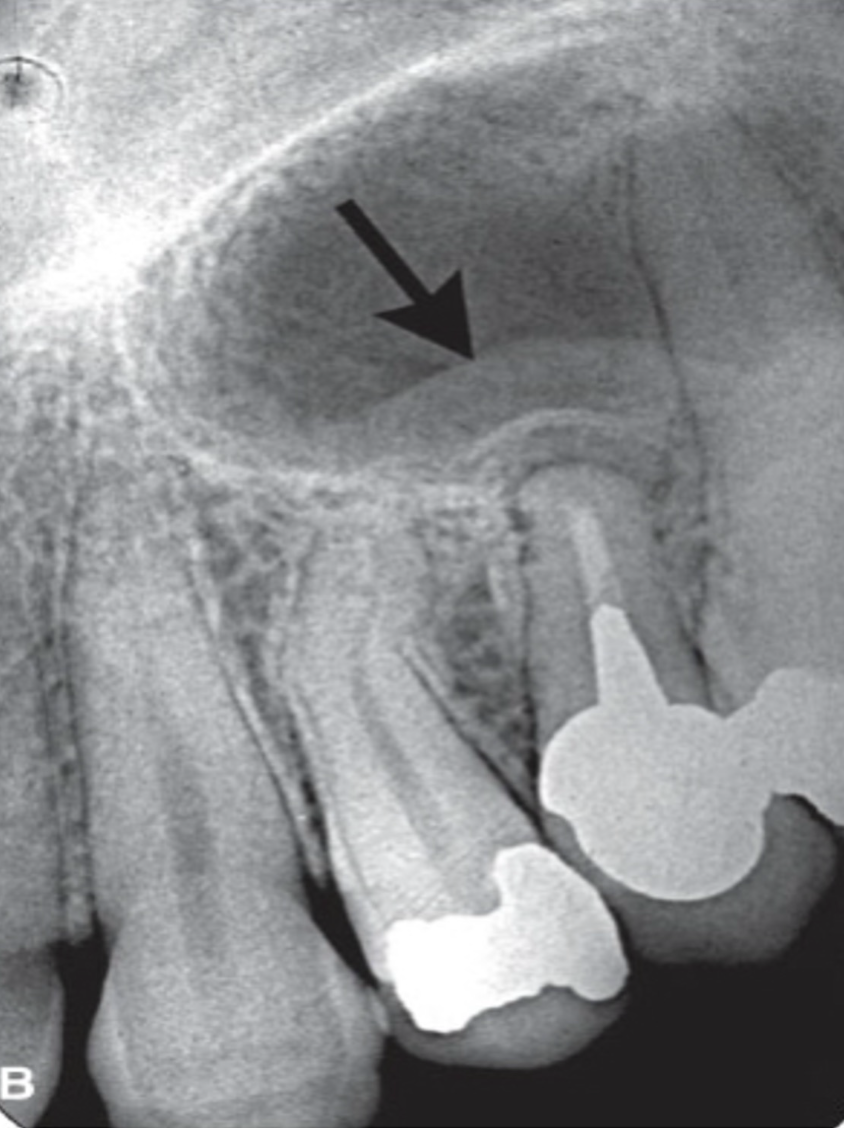
long-standing lesions → radiolucency at root apex with surrounding radiopacity
imaging appearance varies on disease stage and bone response
location → mostly apical, but can be accessory canals or root perforations and fractures
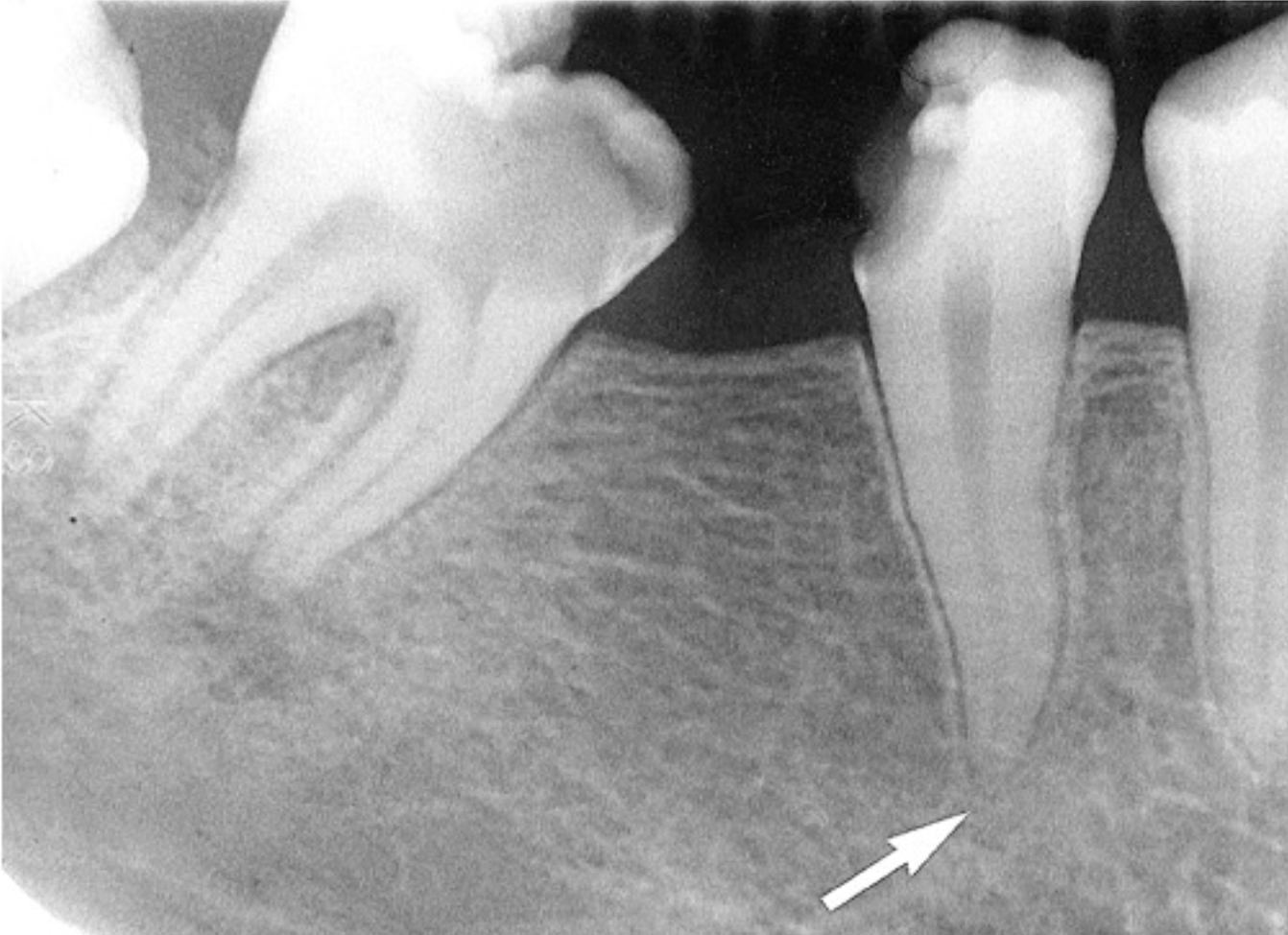
widening of PDL space
loss of lamina dura definition
different radiographic presentations of apical periodontitis
reactive changes → remodeling of floor of maxillary sinus, with maxillary sinus mucosal thickening
dense, reactive bone formation → radiopacity around periapical lesions
effects on adjacent teeth
tooth response mirrors bone response
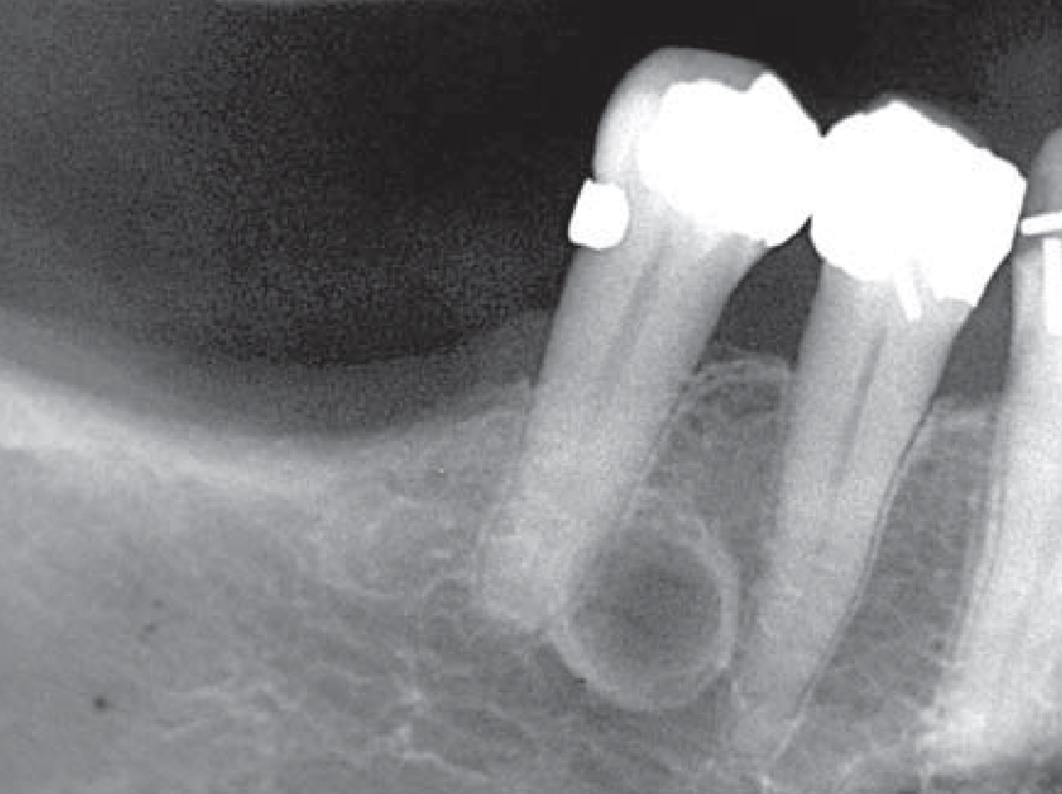
external resorption → irregular root surface
hypercementosis → bulbous-shaped roots
in deciduous teeth, eruption of permanent teeth may be disrupted
lateral radicular cyst
same disease entity as apical periodontitis
lesions form on lateral portion of root
pulp has lateral canals which are often microscopic
bacteria may be in lateral canals
lateral periodontal cyst
originate from epithelial rests in periodontium
usually unilocular
multilocular variant exists → botryoid odontogenic cyst
very well-defined and well-corticated
cemento-osseous dysplasia
benign, fibro-osseous lesion, with teeth remaining vital
relatively harmless change in bone
can appear radiolucent, radiopaque, or become more radiopaque and less radiolucent as patient ages
often confused with apical periodontitis

idiopathic osteosclerosis / dense bone island
can mimic sclerosing osteitis (condensing osteitis)
PDL space remains uniform
narrow transition zone between IO and adjacent bone
sometimes mild root resorption
periapical scar
previous periapical cyst can heal with bone
occasionally heals with fibrous tissue instead
fibrous tissue is radiolucent
always asymptomatic
can be difficult to differentiate between periapical scar and periapical cyst radiographically
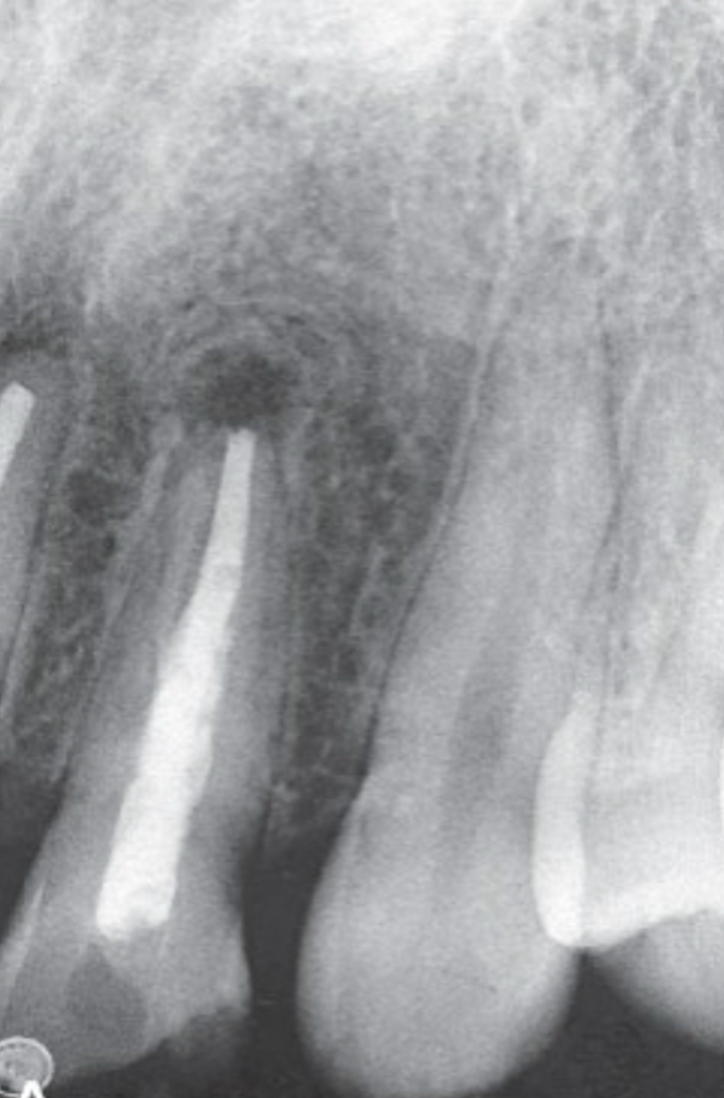
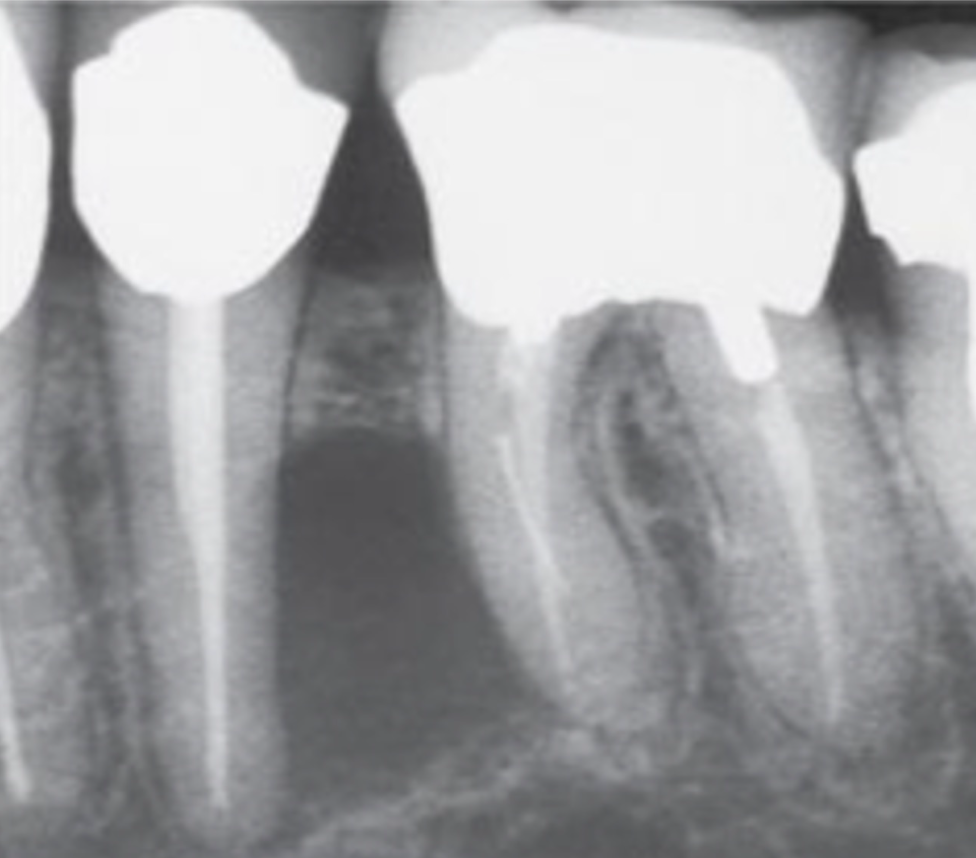
post-treatment changes
radiolucent areas may persist after successful orthograde or retrograde endodontics
central radiolucency may represent healing connective tissue
periophery may show granular bone or radiating trabeculae → “rolled border” or doughnut/fibrous scar pattern

rare cases
metastatic lesions or blood-borne malignancies may develop in periapical region
close inspection may reveal subtle cancellous bone destruction