The Respiratory System L1
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
What are the functions of the Respiratory System
Breathing(pulmonary ventilation)
Gas exchange
filters and protects respiratory surfaces from pathogens and dehydration.
olfaction(smelling)
acid balance - regulating our blood PH
Vocalisation
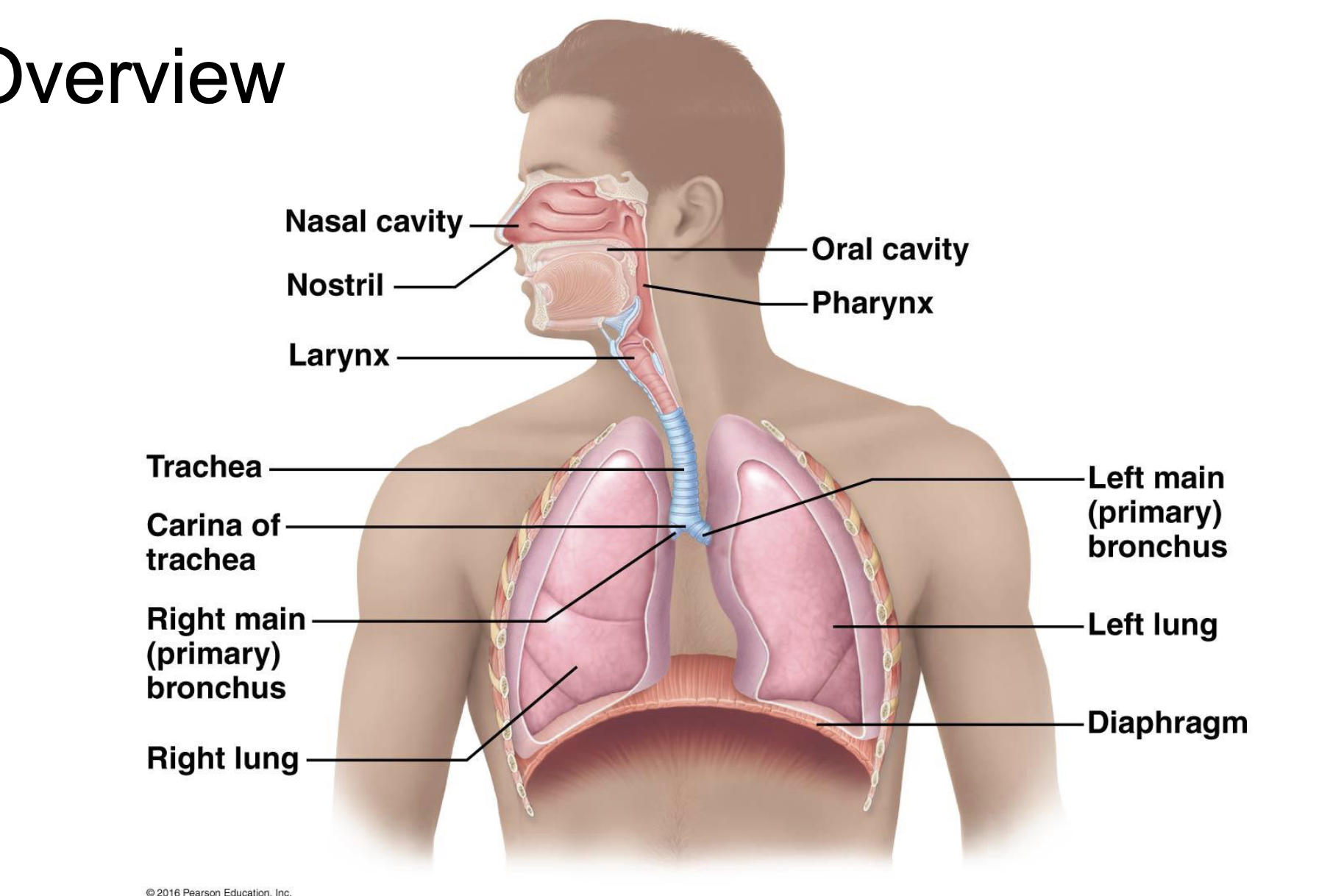
What are the structures of the upper respiratory Tract?
Nasel cavity + pharynx
pseudo-stratified columnar-goblet cells - muscin/mucus glands/lysozymes
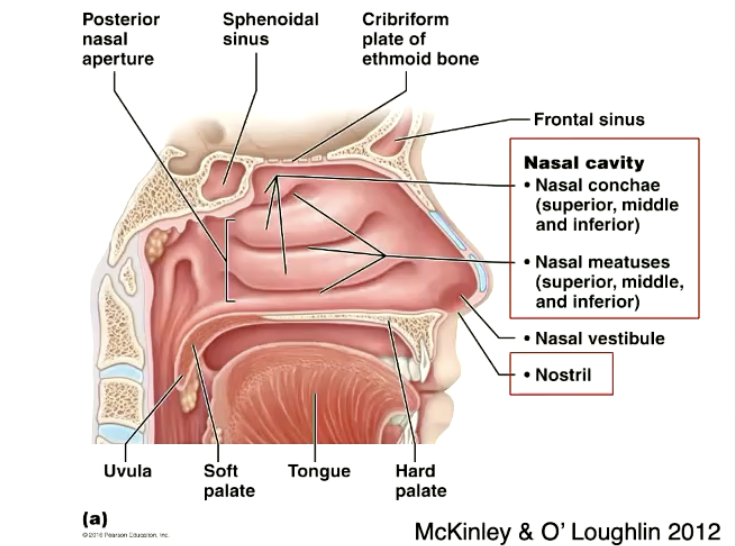
What is the Nasal septum
a central wall of bone and cartilage that divides the nasal cavity
All bone on one side, all cartilage on the other
cartilage on top bone underneath
Explain the wall of the nasal cavity
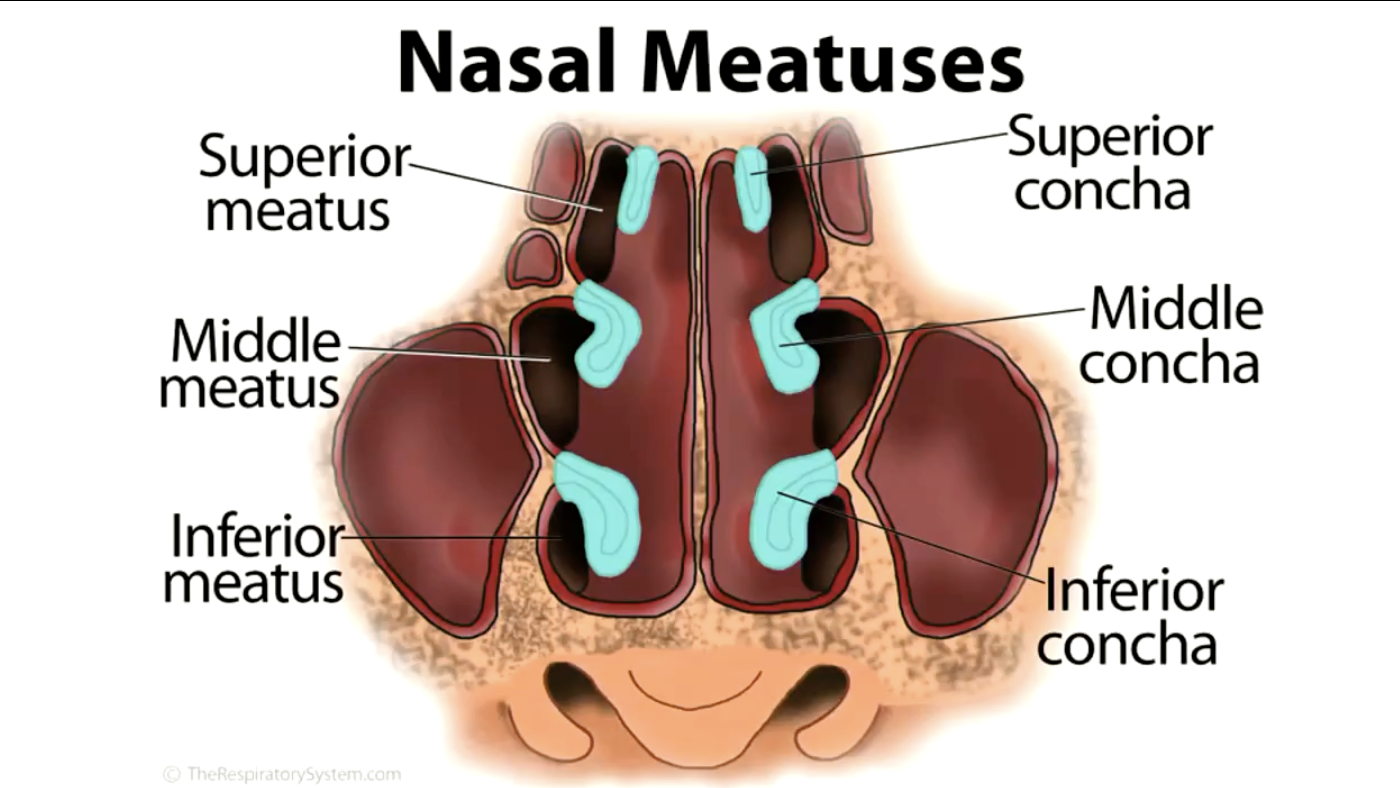
conchae: bony plates found on the lateral walls of the nasal cavity that increase the surface area of the mucous membrane
Function is to create turbulance, stays longer in your nasel cavity= warms up gets humidified → gives you a chance to smell
Explain the anatomy of the Nasal Meatuses
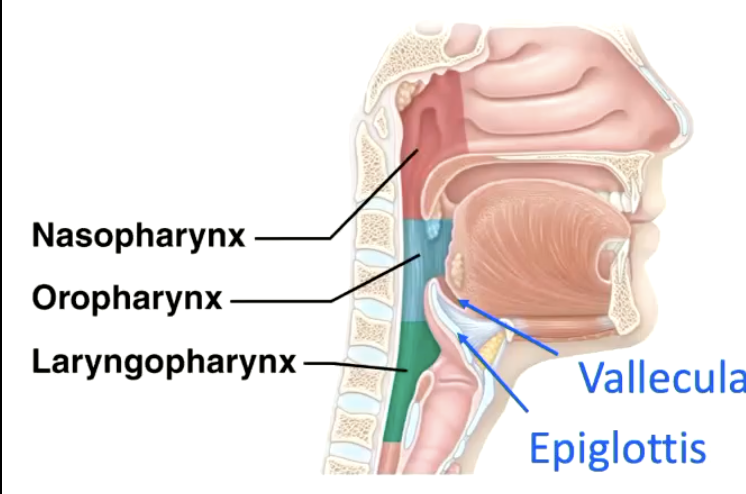
How is the pharynx divided?
3 different regions
Nasopharynx
Pseudostratified ciliated columnar epithelium
alot thinner than..
Oropharynx, laryngopharynx:
non keratinised stratified epithelium
alot tougher, sustain constant friction with the food.
all structures are named by what they are behind
e.g oropharynx is behind the oral cavity
Where is the pharynx?
originates posterior to the nasal and oral cavities and extends inferiorly near the level of the bifurcation of the larynx and esophagus
What is the Pharynx lined with
walls lined with mucosa and contains skeletal muscle that permits swallowing
What structures are oposite the Propharynx and the laryngopharynx?
Vallecula
Epiglottis
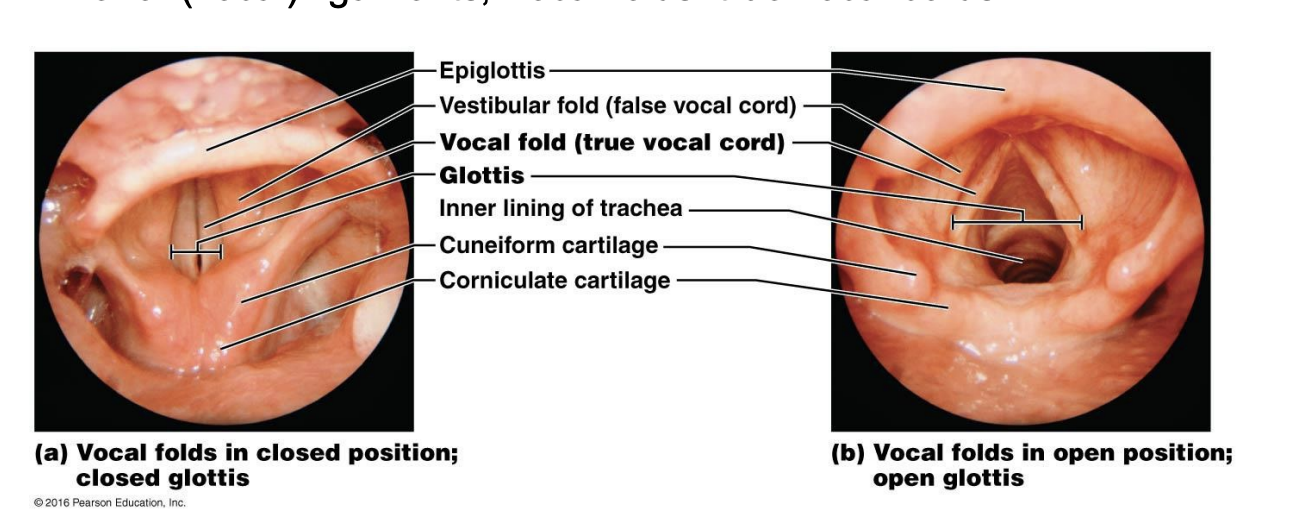
Larynx
A cartilaginous structure located between the pharynx and trachea, playing a crucial role in phonation and protecting the airway.
Superior(vestibular) ligaments; vestibular folds: false vocal cords
inferior(vocal) ligaments; vocal folds: true vocal folds
what are the Larynx cartilages
In summary, the nine laryngeal cartilages are:
Unpaired: thyroid, cricoid, epiglottis
Paired: arytenoid, corniculate, cuneiform
What cartilage supports the vocal and vestibular ligament?
Attachment for vestibular ligament: corniculate cartilage
Attachment for vocal ligament: Arytenoid cartilage.
What are the traits and functions of the trachea
flexible, slightly rigid tube in the mediastinum
Runs from C6 to T4/T5, where it bifurcates into the primary bronchi
Functions
Filter, warm, humidify air
contains 15-20 U-shaped hyaline cartilages and trachealis muscle posteriorly - to help contract and expand to help swallow food
annular ligaments connect cartilage rings.
How many bronchi and then what does it divide into
Primary bronchus 1
secondary Bronchus 2
tertiary bronchi 2
then divides into to small airways - they now have no cartilage. now replaces by muscles.
what are bronchioles
Small airways that branch from tertiary bronchi, leading to alveoli. They lack cartilage and are primarily composed of smooth muscle.
Lined by columnar cuboidal epithelium(facilitates gas diffusion
terminal bronchioles branch into respiratory bronchioles
what are terminal bronchioles
The last generation of bronchioles before the alveolar ducts. They are small airways that lead directly to the alveoli and are involved in gas exchange.
Branch into respiratory bronchioles, which branch into alveolar ducts and alveoli
what are alveoli
functional unit of the lung - where gas exhange happens
Type 1 and type ll alveolar cells (epithelial cells)
endothelial cells
very thin respiratory membrane - 0.5um
What are type 1 alveoli cells
very thin and it stretches out forming most of the surface area of the alveolus 90-95%
gas exhange- gas moves past them easily
What are type 2 alveoli cells
secrete surfactant to reduce surface tension in the alveoli, preventing collapse - help in the repair and maintenance of alveolar epithelium
what are the types of pleura and what are their features
Parietal pleura lines the outside of the pleural cavity and visceral pleura lines the inside.
visceral pleura
the layer of coelomic epithelium that adheres to the tissue of the lungs (Insensitive to pain)
Parietal pleura
They layer that lines the walls of the thoracic cage (Sensitive to pain)
innervated by somatic nerves
separated from the intercostal muscles by the endothoracic fascia
Pleural layer are continuous at the hilum of each lung. goes around and folds in on itself.
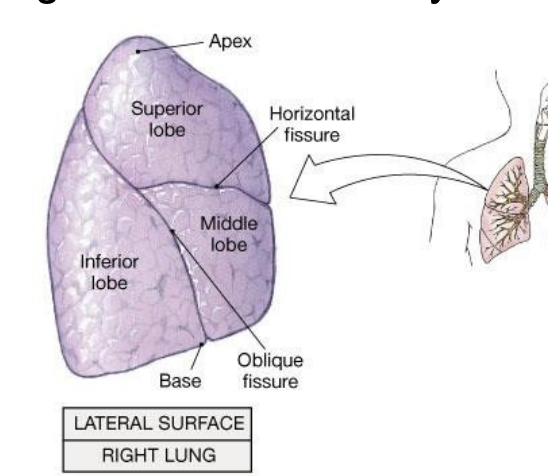
Lobes and fissures
both lungs are conical, with concave base resting on diaphragm and blunt
lung divided into lobes by fissures
name the lobes and fissures for the right lung
name the lobes and fissures for the left lung
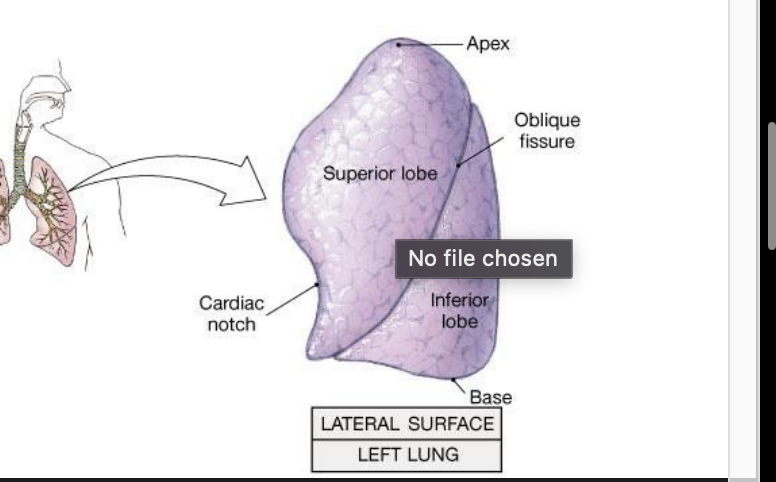
Name the lung surfaces
mediastinal(medial)
diaphragmatic(base)
costal( most lateral, faces the rib cage)
name the lung borders
anterior
posterior(smooth)
Inferior
What is pulmonary circulation?
Pulmonary circulation refers to the blood vessels and system that carries blood between the heart and the lungs to facilitate gas exchange.
what is bronchial circulation?=
component of the systemic circulation. it consists of tiny bronchial arteries and veins that supply the bronchi and bronchioles of the lung,
where do bronchial arteries branch from?
bronchial arteries branch from the anterior wall of the descending thoracic aorta and supply structures in the bronchial tree
larger bronchial veins collet venous blood and drain into the azygos and hemiazygous systems of veins
Pulmonary ventilation
from lungs, oxygen transported to body cells through cardiovascular system
cells use oxygen and generate carbon dioxide as a waste product
blood transport the carbon dioxide from cells to lungs
carbon dioxide expelled during exhalation
pulmonary ventilation and boyles law
the pressure of a gas decreases if the volume of the containers increases, and vice versa
PV= constant
Increasing volume of the thoracic cavity during inhalation decreases intrapulmonary pressure relative to the atmospheric pressure and air flows into the lungs until equilibrium is reached.
the volume of the thoracic cavity decreases during exhalation relative to outside atmospheric pressure, air is forced out of the lungs
Alveolar pressure changes… beginning of inspiration
beginning of inspiration
contraction of muscles & increase of thoracic volume
expansion of lungs and increase in alveolar volume
decrease in the intrapulmonary pressure below atmospheric pressure
air flows into the lungs
Alveolar pressure changes… end of inspiration
alveoli and thorax stop expanding
air flow into the lungs causes Patm=Palv
no more movement of air occurs
Alveolar pressure changes… beginning of expiration
decrease of thoracic volume
decrease in alveolar volume
increase in the intrapulmonary pressure above
atmospheric pressure (Palv>Patm)
Air flow out of the lungs until Palv=Patm
Alveolar pressure changes… end of expiration
Patm=Palv
no more movement of air occurs
respiratory muscles - Eupnea
Eupnea: Quiet breathing at rest. It can be diaphragmatic or costal
Diaphragmatic breathing (deep breathing): Diaphragmatic contraction expands the thoracic cavity (innervation phrenic n.) Exhalation is passive. The diaphragm relaxes
Costal breathing (shallow breathing): Ext. Intercostal muscles contract, elevate the ribs and enlarge the thoracic cavity (innervation intercostal n.) Exhalation is passive. The muscles relax
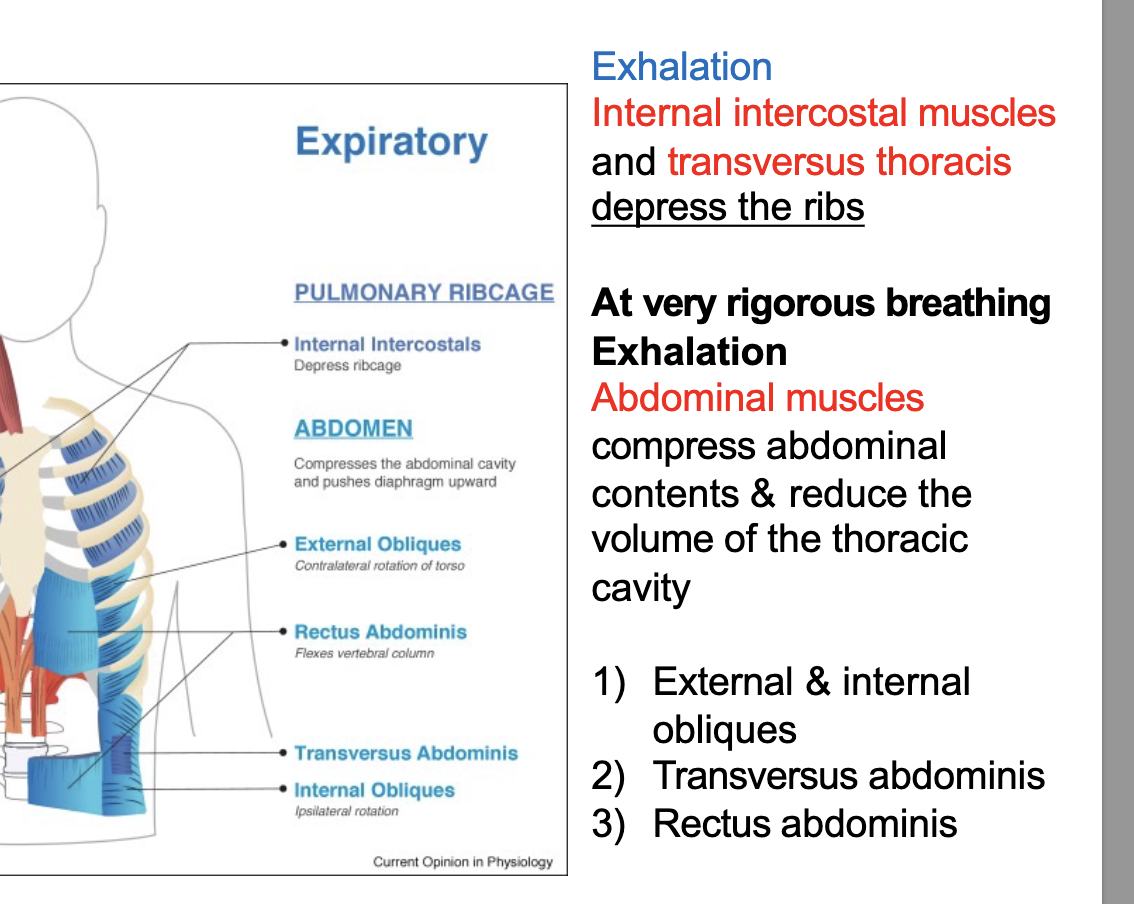
Respiratory Muscles - Hypereupnea
Hypereupnea: Fast-forced breathing
Hypereupnea inspiration
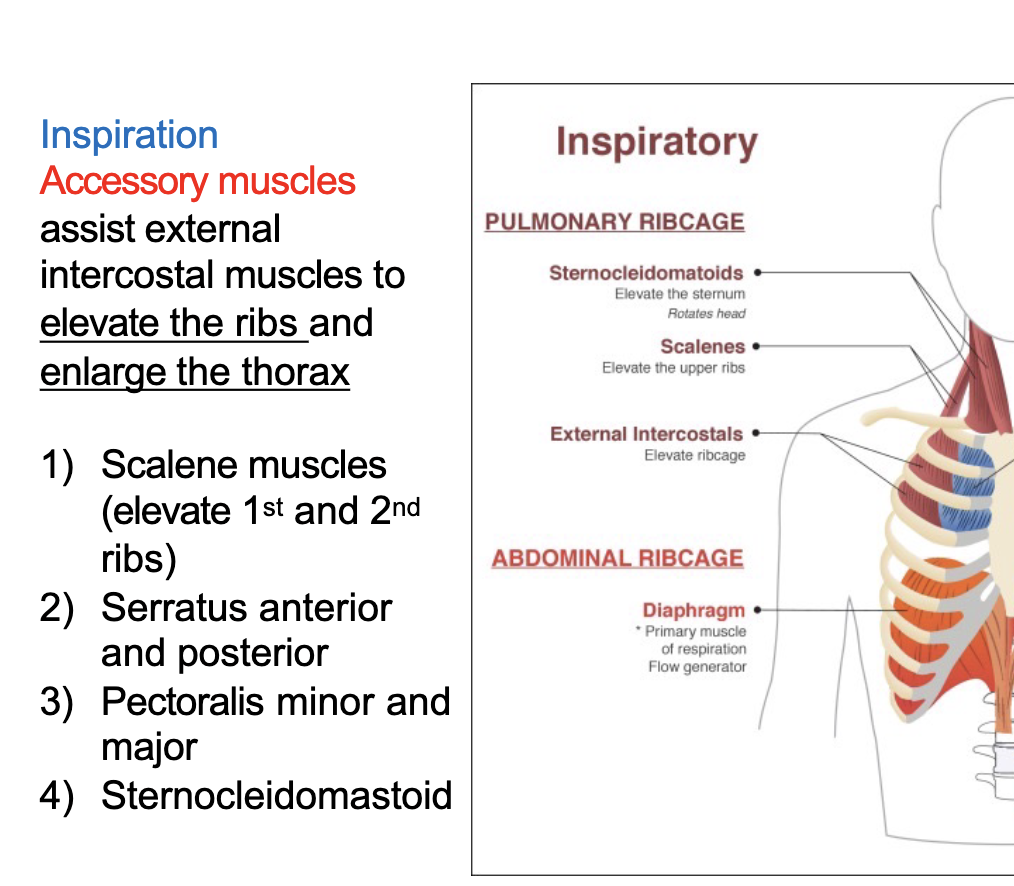
Hypereupnea Exhalation
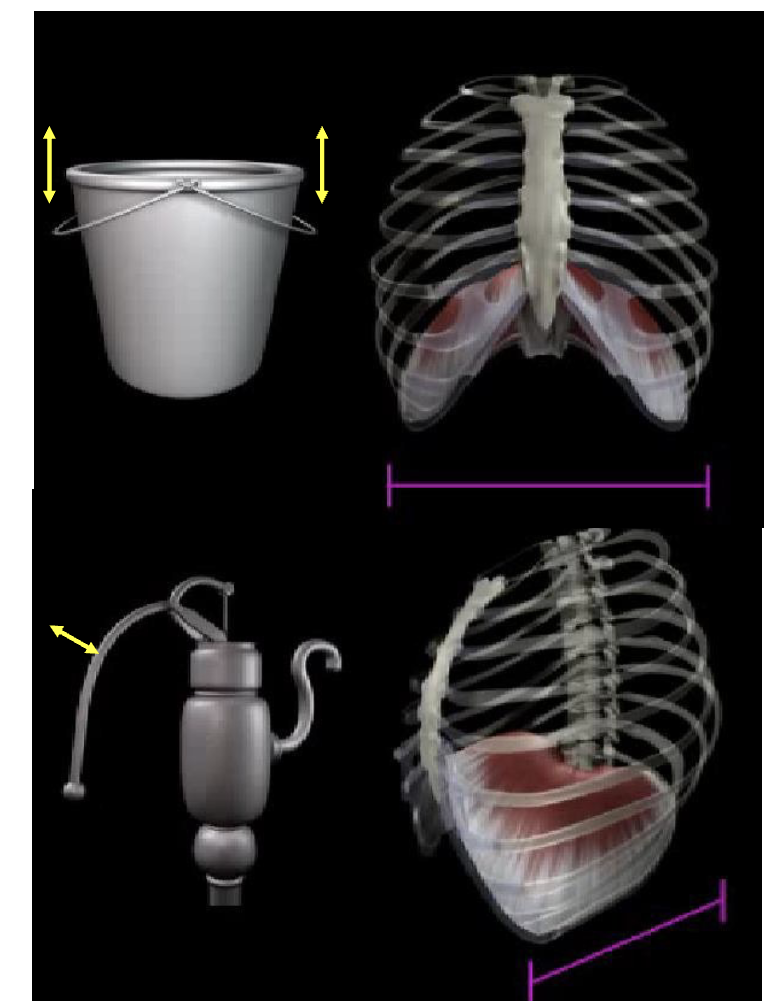
What are the movements of the Thorax
“bucket and pump handle”
The thorax undergoes "bucket handle" and "pump handle" movements during breathing, which change the dimensions of the chest cavity.
The upper ribs, particularly 2-6, exhibit pump handle movement, where their sternal ends lift up and down, increasing the antero-posterior diameter of the thorax
. The lower ribs (7-10) demonstrate bucket handle movement, where they swing outwards, increasing the transverse diameter of the thora
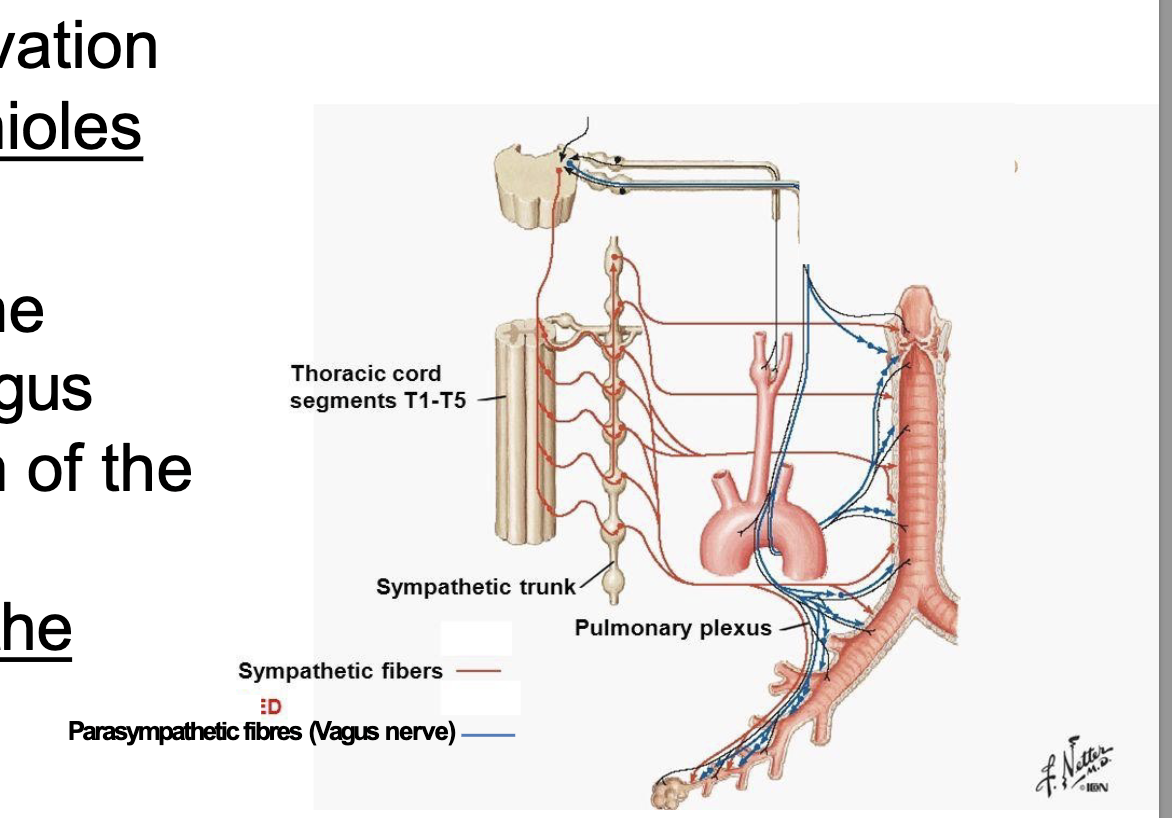
what are the 2 types of Innervation of Respiratory System
sympathetic innervation and parasympathetic innervation
sympathetic innervation Respiratory System
Sympathetic innervation to the lungs
originates from the T1–T5. The main
function of the sympathetic innervation
is to open up or dilate the bronchioles
parasympathetic innervation Respiratory System
Parasympathetic innervation to the
lungs is from the left and right vagus
nerves (CN X). The main function of the
parasympathetic innervation is to
decrease the airway diameter of the
bronchioles Parasympathetic fibres (Vagus nerve)
Innervation of Respiratory System anatomy
Test yourself: Draw a diagram of the passage of air as it enters from the environment through to the lungs, include the major organs that it passes through.