Chapter 20: Structure & Function of the Heart
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
List the major functions of the heart:
Generation of blood pressure→
Creates the blood pressure required for blood flow through the vessels.
Routing of the blood→
Two pumps, the heart pumps the blood through both the pulmonary and systemic circulations.
Ensuring one-way blood flow→
Via the heart valves. (so theres no back flow of blood).
Regulation of the blood supply→
The heart adjusts blood flow by changing the rate and force of contractions as needed
Cite the size, shape, and location of the heart:
Location→
Anterior to the vertebral column.
Posterior to the sternum.
Left of the midline.
Deep to the second to fifth intercostal spaces.
Superior surface of diaphragm.
Housed within the mediastinum (just where the heart sits, resting on diaphragm). Central core of the thoracic cavity, houses everything but lungs.
Shape→
A blunt cone, with an apex and a base. Apex: inferior, comes to a point. Base: superior, rounded.
Size→
Approximately the size of your clinched fis
layers of the pericardium:
Fibrous pericardium→
(Double-walled sac that surrounds the heart)
SUPERFICIAL
Tough, fibrous.
Protects and anchors the heart.
Prevents overfilling of the heart with blood.
Serous pericardium:
→ pericardial cavity.
DEEP
Thin, transparent.
Allows for the heart to work in a relatively friction-free environment.
Pericardial cavity:
Filled with pericardial fluid that acts as a cushion and lubricant
Parietal layer:
lines the internal surface of the fibrous pericardium.
Visceral layer:
lines the surface of the heart (physically touches the heart).
Separated by the pericardial cavity.
layers of the heart wall:
Epicardium→
Visceral layer of the serous pericardium.
Provided protection against the friction of rubbing organs.
Myocardium→
thickest layer
Cardiac muscle layer that forms the bulk of the heart.
Responsible for contraction.
Endocardium→
most inner lying layer.
Endothelial layer.
Reduced the friction of blood passing through the heart
Trabeculae carneae→
muscular ridges and columns on interior walls of ventricles.
Pectinate muscles→
muscular ridges in the atrial walls.
Papillary muscles→
cone of nipple-like projection.
Cone-shaped muscles of the ventricles that play a role in valve function.
Describe the location and function of the large veins and arteries that enter and exit the heart:
Veins→
Superior vena cava: brings O2 poor blood from the head, neck, upper limbs, and thorax to the right atrium.
Inferior vena cava: brings O2 poor blood from the abdomen, pelvis, and lower limbs to the right atrium.
Arteries→
Pulmonary trunk: carries O2 poor blood from the right ventricle to the lungs.
Aorta: carries O2 rich blood to the systemic circulation.
Coronary arteries→
supply the heart itself with blood. Branch off of the aorta to provide blood to the cardiac tissue.
Cardiac veins→
drain blood from the coronary circulation into the coronary sinus. Returns blood into the right atrium.
four chambers of the heart:
ATRIA:
thin-walled, low pressure receiving chambers of the heart. Each atrium has a protruding auricle on its external surface.
Right Atrium: receives O2 poor blood from the systemic circulation. Receives blood from the coronary sinus, superior vena cava, and inferior vena cava.
Left Atrium: receives O2 rich blood from the lungs. Receives blood from the pulmonary veins
VENTRICLES:
thick walled, discharging chambers of the heart.
Right Ventricle: pumps O2 poor blood to the lungs to be oxygenated. Opens to the pulmonary trunk.
Left Ventricle: THICKER. Pumps O2 rich blood to the systemic circulation. Opens to the aorta.
four valves of the heart:
Tricuspid valve→
separates the right atrium and right ventricle. Prevents backflow of blood into the right atrium.
Bicuspid valve→
separates left atrium and left ventricle. Prevents back flow of blood into the left atrium.
Pulmonary semilunar valve→
separates the right ventricle from the pulmonary trunk. After contraction, the valve closes and prevents backflow of blood into the right ventricle.
Aortic semilunar valve→
separates the left ventricle from the aorta. After contraction, the valve closes and prevents backflow of blood into the left ventricle.
**BOTH VALVES ARE OPEN DURING CONTRACTION. AFTER CONTRACTION IS WHEN THEY CLOSE
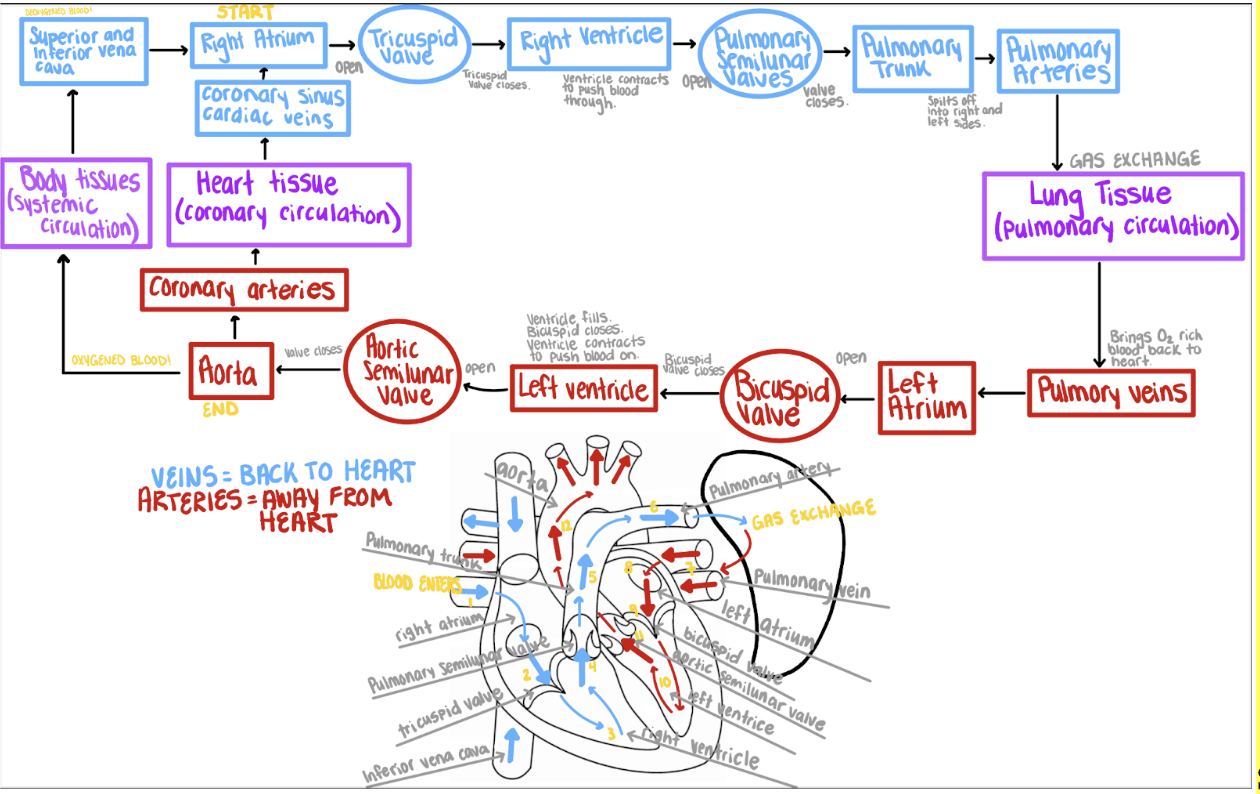
Trace the flow of blood through the heart from the right atrium through the aorta, naming the chambers, valves, and vessels in the correct order:
Describe the structure and function of the fibrous skeleton:
Consists of a plate of fibrous connective tissue between the atria and ventricles. Gives us the structure of our heart valves.
Forms fibrous rings around the AV and SL valves for support.
Provides a point of attachment for cardiac muscle.
Electrically insulates the atria from the ventricles.
Describe the structural and functional characteristics of cardiac muscle cells:
Branched and have a centrally located nucleus.
Actin and myosin are organized to form sarcomeres (striated).
Rely on aerobic respiration for ATP production:
(constant delivery of O2) many mitochondria, well supplied with blood vessels.
Joined by intercalated disks:
Allow action potentials to move from one cell to the next, thus cardiac muscle cells function as a unit.
phases of action potentials in cardiac muscle and the corresponding ion channel openings:
Depolarization phase:
Voltage-gated Na+ channels open.
Voltage-gated K+ channels close.
Voltage-gated Ca2+ channels begin to open.
Early repolarization and plateau phase:
Voltage-gated Na+ channels close.
Some voltage-gated K+ channels open, causing early repolarization.
Voltage-gated Ca2+ channels are open, producing the plateau by slowing further repolarization.
Final repolarization phase:
Voltage-gated Ca2+ channels close.
Many voltage-gated K+ channels open.
Explain what is meant by the autorhythmicity of cardiac muscle:
Intrinsic conduction consists of autorhythmic (non-contractile) cardiac cells that are specialized to initiate impulses.
Individual cells can depolarize without outside stimulation:
- have unstable resting potentials and depolarize continuously creating waves of depolarization that spread to contractile cardiac cells.
- when a threshold of depolarization is reached, fast Ca2+ channels open to produce an action potential.
Explain the importance of a long refractory period in cardiac muscle (vs. skeletal):
Refractory periods:
absolute refractory period:
cardiac muscle cells are insensitive to further stimulation
Relative refractory period:
stronger than normal stimulation can produce an action potential.
Cardiac muscle→
has a prolonged depolarization and thus a prolonged absolute refractory period, which allows time for the cardiac muscle to relax before the next action potential causes a contraction (NO TETANUS).
Explain the structure and function of the intrinsic conducting system of the heart:
Sinoatrial (SA) node:
Sets the pace of the heart as a whole. About 100 bpm (sinus rhythm). Known as the “pacemaker”.
From the SA node, depolarization spreads to both atria via conduction tracts (allows both atria to contract simultaneously).
Depolarization reaches the atrioventricular (AV) node:
A slight delay (0.11 seconds) occurs at the AV node so the atria can finish contraction before the ventricles.
From the AV node, the AV bundle extends into the interventricular (IV) septum and gives rise to the right and left bundle branches.
Purkinje fibers complete the IV septum and run within the ventricular walls. Purkinje fibers carry the impulse to the contractile cardiac muscle. This causes simultaneous ventricular contraction. Contraction begins at the apex of the heart and moves superiorly.
Indicate the HR set by the SA node as well as normal resting HR and explain why they differ:
The SA node sets the pace of the heart as a whole around 100 bpm and is considered the “pacemaker”.
A normal resting HR is around 72 bpm because the parasympathetic nervous system slows the HR because it doesn’t need to beat that quickly to direct blood through the body at rest.
Trace the pathway of intrinsic conduction from the SA node to the Purkinje fibers:
SA node → AV node → AV bundle → through the fibrous skeleton and into the interventricular septum → AV bundle divides into right and left bundle branches → action potentials are carried by the Purkinje fibers to the ventricular walls and papillary muscles
Describe extrinsic regulation (influences) of the heart and its effects on cardiac function:
Sympathetic influence:
Cardioacceleratory center in the medulla oblongata.
Signals motor neurons in T1-T5.
Sends signals to the SA node.
Norepinephrine is released at cardiac synapses which increases HR and strength of contraction.
Parasympathetic influence:
Cardio-inhibitory center in the medulla oblongata.
Signals to the vagus nerve.
Signals travel to the SA node and AV node.
Acetylcholine is released which lowers HR.
P-wave:
corresponds to atrial depolarization (SA node)
QRS complex:
corresponds to ventricular depolarization
T wave:
corresponds to ventricular repolarization
Atrial repolarization:
masked by the larger QRS complex
Events occurring during ventricular systole:
Ventricular depolarization:
Produces the QRS complex
initiates contraction of the ventricles, which increases ventricular pressure
**The AV valves close (tri/bicuspid)
**Semilunar valves open
**Blood is ejected from the heart
Events occurring during ventricular diastole
Ventricular repolarization:
produces the T-wave
ventricles relax
**Blood flowing back toward the relaxed ventricles closes the semilunar valves
**The AV valves open and blood flows into the ventricles
passive ventricular filling occurs
Events occurring during ventricular diastole
Atrial depolarization:
produces the P-wave
the atria contract and complete ventricular filling (active ventricular filling)
Systole→
contraction phase.
Atrial systole is contraction of the atria.
Systole is contraction of the ventricles.
Diastole→
relaxation phase.
Atrial diastole is relaxation of the atria.
Diastole is relaxation of the ventricles.
heart sounds to the closure of the AV and semilunar valves:
First sound (lubb) →
occurs as the AV valves close and signifies the beginning of systole.
Second sound (dupp) →
occurs when SL valves close at the beginning of ventricular diastole.
Mean arterial pressure (MAP):
average blood pressure in the arterial system.
Cardiac output (Q):
volume of blood pumped by the heart per minutes.
Total peripheral resistance (TPR):
total resistance to blood flow through the blood vessels.
MAP and Q equations:
MAP = Q x TPR Q = HR x SV
Explain the importance of regulating MAP:
Adequate blood pressure is necessary to ensure the delivery of blood to the tissues.
Define stroke volume:
volume of blood pumped out by a ventricle with each beat.
indicate the three factors that can modify stroke volume:
Preload:
increased venous return to the heart increases stroke volume by increasing end-diastolic volume.
Positive on SV.
Afterload:
the pressure against which the ventricles must pump blood
increased afterload increased end-systolic volume and decreases stroke volume.
Negative on SV
Contractility:
increases stroke volume by decreasing end-systolic volume.
The more powerful the contraction, the less blood is left in the ventricles.
Positive on SV
End-systolic volume:
the amount of blood remaining in a ventricle after contraction
End-diastolic volume:
amount of blood collected in a ventricle just before contraction (preload)
List the major age-related changes that affect the heart:
Decreased cardiac output and heart rate
Increased cardiac arrhythmias
Hypertrophy of the left ventricle
Development of stenoses or incompetent valves
Development of coronary artery disease and heart failure