Cholinergic and Cholinergic Blockers
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
Parasympathetic Nervous System (PNS)
Rest and Digest System
PSNS neurotransmitter is
Ach
PSNS receptors are
-Muscarinic receptors
-Nicotinic receptors
cholinergic agonists can also be called
parasympathomimetics
Direct-acting cholinergic agonists
Bind to cholinergic receptors, activating them
Indirect-acting cholinergic agonists (cholinesterase inhibitors)
-Inhibit the enzyme acetylcholinesterase (Ach-E), which breaks down Ach
-more Ach available at receptor sites
reversible
Bind to cholinesterase for a period of minutes to hours
irreversible
-Bind to cholinesterase and form permanent covalent bond
- body must make new cholinesterase to break these bonds
cholinergics overall mechanism of action
-Effects seen when the PNS is stimulated
-After binding, permeability of cell changes allowing flow of calcium and sodium into cells AND depolarization of cell membrane and stimulation of effector organ
cholinergics stimulate the _____ and ____ causing 3 things which are?
•Stimulate Intestine and Bladder
-Increased gastric secretions
-Increased gastrointestinal motility
-Increased urinary frequency
Cholinergics stimulate pupil causing
-Constriction (miosis)
-Reduced intraocular pressure
what do cholinergics do to salivation and sweating
increase it
CV effects of cholinergics
-Decreased HR
-Vasodilation
respiratory effects OF CHOLINERGICS
-Bronchial constriction= narrowed airways
Recommended doses of cholinergic medications effect which receptors and cause which effects?
•muscarinic receptors
- desired effects are from muscarinic receptor stimulation
at high doses cholinergic medicines affect which receptors and cause which effects?
cholinergics stimulate nicotinic receptors
- undesirable effects are from nicotinic receptor stimulation
bethanechol
–Increases tone and motility of bladder and GI tract
–Relaxes sphincters in bladder and GI tract, allowing them to empty
–Helpful for post-surgical atony of the bladder and GI tract
–Oral or subcutaneous (SC) injection
-after getting this drug takes 60 mins to urinate
-DIRECT ACTING
cevimeline
–Used to treat excessively dry mouth (xerostomia) -> Sjögren’s syndrome
-DIRECT ACTING
succinylcholine
-Used as a neuromuscular blocker in general anesthesia
-given before intubation
-DIRECT ACTING
block transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.
Indirect-Acting Medications MOA and example
-Increase Ach concentrations at receptor sites
- stimulates effector cells
-Cause skeletal muscle contractions
Pyridostigmine is used for
-Used for diagnosis and treatment of myasthenia gravis (MG)
-Used to reverse neuromuscular blocking agents
-Used to reverse anticholinergic poisoning (antidote)
What drugs are used for alzheimers and which is an indirect cholinergic
for treatment of mild to moderate Alzheimer’s disease: donepezil (indirect cholinergic)
–Other medication for Alzheimer’s disease - memantine
•Not a cholinergic drug
Contraindications: Cholinergics
-allergy
-Bradycardia
-Defects in cardiac impulse conduction
-Hyperthyroidism
-Hypotension
-GI or GU tract obstruction-can cause rupture in colon/bladder
-Chronic obstructive pulmonary disease (COPD)
-Parkinson's disease
-Epilepsy
Adverse Effects: Cholinergics
•CV System
-Bradycardia, hypotension, conduction abnormalities (AV block and cardiac arrest)
•Central Nervous System (CNS)
-Headache, dizziness, convulsions
•GI System
-Abdominal cramps, increased secretions, N/V
•Respiratory System
-Increased bronchial secretions/ bronchospasms
•Other
-Lacrimation, sweating, salivation, miosis
The C is WET
-increased secretions
-fluid build up
Cholinergic Crisis sx
-Circulatory collapse
-hypotension
-shock
-cardiac arrest
-bloody diarrhea
early signs of crisis and treatment
-Abdominal cramps
-flushing
-N/V
-transient syncope
-transient complete heart block
-dyspnea
-orthostatic hypotension
TREATED W / ATROPINE!
Treatment of severe CV reactions/bronchoconstriction
epi
SLUDGE
CHOLINERGIC CRISIS
•Salivation
•Lacrimation
•Urinary incontinence
•Diarrhea/digestion
•Gastrointestinal motility
•Emesis
which drugs interact with cholinergics and ANTAGONIZE their effects
•Anticholinergics, antihistamines (because they block muscarinic receptors), sympathomimetics (adrenergic)
-Antagonize cholinergic medications, resulting in decreased responses
should you use multiple cholinergic meds at the same time
No because it causes additive effects
Bethenechol is used for treatment of what?
-Treatment of acute postoperative and postpartum nonobstructive urinary retention
-Management of urinary retention associated with neurogenic atony of the bladder
Contraindications for bethenechol
-PUD
-CAD (or cardiac disease)
-active bronchial asthma
Adverse effects of bathenechol
-Hypotension with reflex tachycardia
-GI upset
-asthma attacks
Interactions of bathenechol
-Acetylcholinesterase inhibitors (i.e., indirect-acting cholinergics)
this would cause an over reaction
donepezil is a ___ acting cholinergic drug for which disease?
-Cholinesterase inhibitor leads to increase levels of Ach by inhibiting Ach enzyme
-Treatment of mild to moderate Alzheimer's disease
Adverse effects for Donepezil
-GI upset (including ulcer risk caused by increased gastric secretions)
-muscle cramps
-drowsiness
-insomnia
-hypotension with reflex tachycardia
-hypertension
donepazil interacts with
•anticholinergics (counteract donepezil effects)
-NSAIDs
MEMANTINE
•not a cholinergic medication; used to improve cognitive function and quality of life in clients diagnosed with Alzheimer’s
–Adverse effects:
-HTN
-HA
-GI upset
-fatigue
-muscle pain
-ataxia
Safety: Herbal Treatment - Gingko
-common uses?
-AE?
-Potential interactions?
•Common uses
–Prevent memory loss
–Vertigo
–Tinnitus
•May cause GI upset, HA, bleeding
•Potential interactions
–Aspirin (ASA)
–NSAIDs
–Anticoagulants
–Anticonvulsants
-Children have a ____ risk for AE
- how are doses calculated?
-what is used for diagnoses of MG in kids?
-Greater risk for adverse effects
-Doses based on weight
-Edrophonium is used only for diagnosis of MG in children
can pregnant or lactating women use cholinergic agonists?
only if benefits outweigh risks
-Older Adults have a _____ risk for AE
-Monitor them for ____ and ______
- start them on what kind of doses
- what should they take with cholinergic meds
-Greater risk for adverse effects and toxic levels
-Monitor for serious dysrhythmias or hypotension
-Start on lower doses
-Take with food or small meals; encourage fluid intake BC secretions could dry you out
Nursing Implications: Assessment
•Keep in mind that these agents will stimulate the PNS and mimic the action of Ach
•Assess for allergies, presence of GI or GU obstructions, COPD, asthma, PUD, or CAD
•Perform baseline assessment of vital signs (VS) and systems overview
Nursing Implications: Interventions
•Medications should be taken as prescribed and NOT abruptly stopped
•Doses should be spread evenly apart to optimize the effects of the medication
•Overdosing can cause life-threatening problems.
–Clients should not adjust dosages unless directed by the healthcare provider (HCP)
•Encourage clients with myasthenia gravis to take medication 30 minutes before eating to help improve chewing and swallowing (pyridastygmine)
Be honest with caregivers and clients diagnosed with Alzheimer's that the medication is for
meds are for management of symptoms, not a cure
–Therapeutic effects of Alzheimer’s medications may not occur for up to 6 weeks
antidote for cholinergics is
atropine
Nursing Implications: Client Teaching
for oral forms when should meds be taken
•Medications should be taken before meals or without food with oral forms
•Instruct clients to notify HCP if experiencing
–Muscle weakness
–Abdominal cramps
–Diarrhea
-Difficulty breathing
Nursing Implications: Evaluations
•Monitor for adverse effects
•Monitor for therapeutic effects
–Alleviated manifestations of MG
–Increased bowel sounds, passing gas, and bowel movements in postoperative clients with decreased GI peristalsis
–In clients with urinary retention/hypotonic bladder, urination should occur within 60 minutes of bethanechol administration
–Improvement of symptoms, mood, and decreased confusion in clients diagnosed with Alzheimer’s disease
Cholinergic-Blocking Medications
Medications that inhibit Ach in the PNS
-inhibit ACH from binding to the receptor
-ANTICHOLINERGICS
-ANTIMUSCARINICS
-CHOLINERGIC ANTAGONISTS
-PARASYMPATHOLYTICS
Cholinergic-Blockers: Mechanism of Action
•Competitive antagonists
•Compete with Ach for binding at muscarinic receptors in the PSNS
-Ach unable to bind to receptor site
-inhibits nerve transmission and cholinergic effect
CV effects of anti-cholinergics (small vs large dose)
-Small doses: decrease HR
-Large doses: increase HR
CNS effects of anti-cholinergics (small vs large dose)
-Small doses: decrease muscle rigidity and tremors
-Large doses: drowsiness, disorientation, hallucinations
Eye effects of anti-cholinergic meds
-Dilated pupils (mydriasis)
-Decreased accommodation due to paralysis of ciliary muscles (cycloplegia)
GI effects of anti-cholinergic meds
-Relax smooth muscle tone of GI tract
-Decrease intestinal and gastric secretions
-Decrease motility and peristalsis
-Constipation
GU effects of anti-cholinergic meds
-Relaxed detrusor muscle
-Increased constriction of internal sphincter
Result: urinary retention
Glandular effects of anti-cholinergic meds
–Decreased bronchial secretions, salivation, sweating
respiratory effects of anti-cholinergic meds
-Decreased bronchial secretions
-Dilated bronchial airways
Contraindications: Cholinergic-Blockers (A4, M, G)
-allergy
-Angle-closure glaucoma
-Acute asthma or other respiratory distress
-Acute CV instability
-MG
-GI or GU tract obstruction
Toxicity and Overdose: Cholinergic-Blockers
•Symptomatic and supportive therapy
•Continuous HEART monitoring
•Activated charcoal: binds to med and renders it inactive if it was taken recently and still in the GI tract
•Treatment of shock
Antidote for Anti-cholinergic toxicity is
Physostigmine
interactions for anticholinergics are ____ and ____
-why do they interact?
-digoxin
-other cholinergic blockers
compete for binding sites
cholinergic blocking meds are
• Atropine
• Dicyclomine
• Glycopyrrolate
• Oxybutynin
• Scopolamine
• Tolterodine
atropine used for
-Used primarily for CV disorders
–Diagnosis of sinus node dysfunction
–Symptomatic second-degree heart block
–Sinus bradycardia with hemodynamic compromise (advanced life support)
•Used as an antidote for anticholinesterase inhibitor toxicity or poisoning
•Used preoperatively to reduce salivation and GI secretions
if they are bradycardic and _____ we give
symptomatic we give atropine
Contraindications for giving Atropine
-hepatic and renal dysfunction
-intestinal atony
-hiatal hernia associated with reflux esophagitis
-severe ulcerative colitis
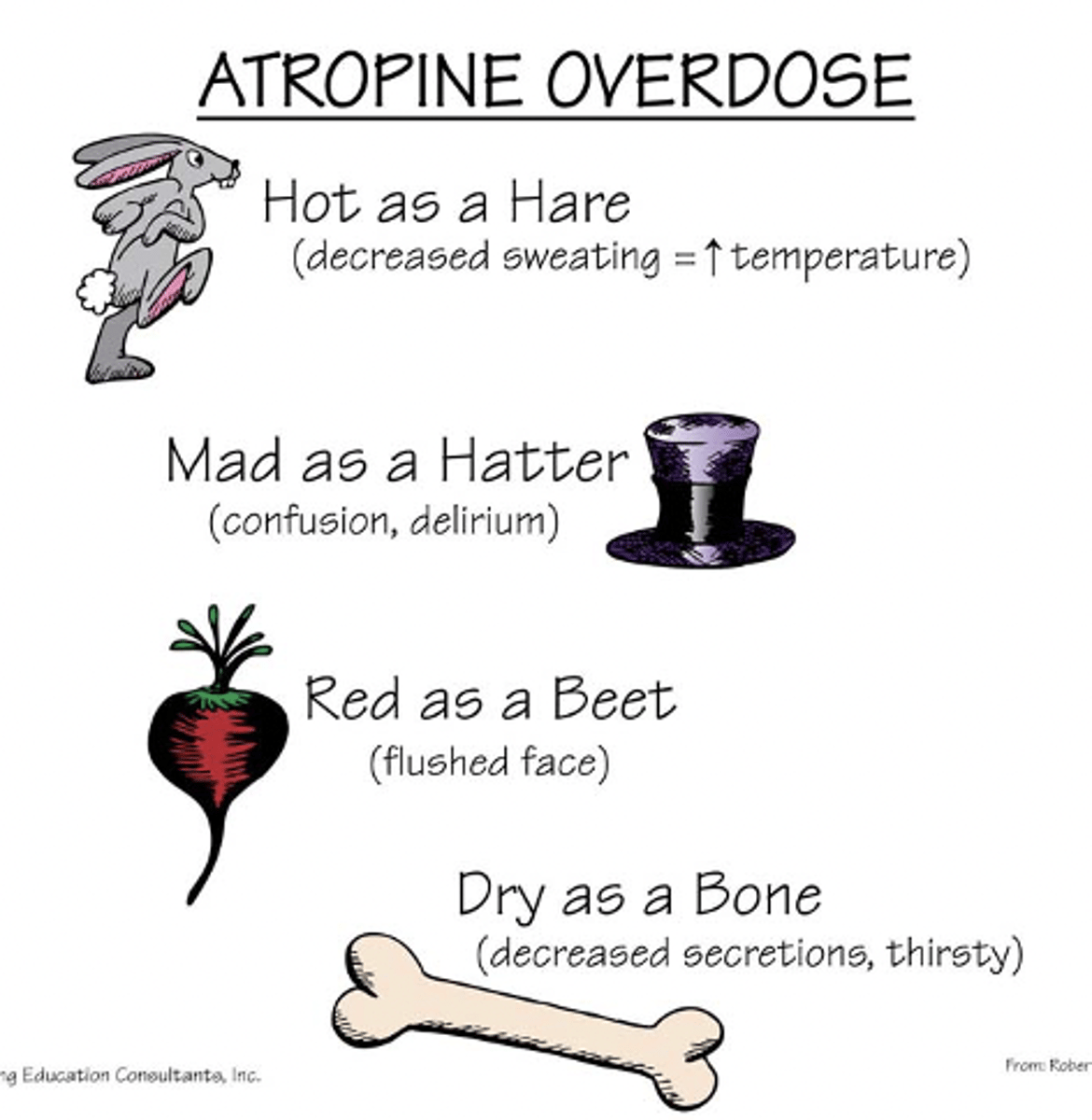
Atropine overdose
-decreased sweating=increased body temperature
-confusion/delirium
-flushing
-decreased secretions
-thirst
Dicyclomine is a synthetic ____ and is used for
•Synthetic antispasmodic cholinergic blocker
•Uses:
-functional disturbances of GI motility such as irritable bowel syndrome
Contraindications for dicyclomine
-paralytic ileus
-GI atony
-toxic megacolon
-myasthenia gravis
Glycopyrrolate is a synthetic anti______ receptor drug
used for
•Synthetic antimuscarinic drug
•Blocks receptor sites in the autonomic nervous system that control the production of secretions
•Use: preoperatively to reduce salivation and excessive secretions in the respiratory and GI tracts
Counterindications for Glycopyrrolate
-hepatic disease
-ulcerative colitis
-toxic megacolon
-myasthenia gravis
-tachycardia
-myocardial ischemia
Oxybutynin is a synthetic anti ______ receptor drug used for
•Synthetic antimuscarinic drug
•Uses:
-overactive bladder and antispasmodic for neurogenic bladder associated with:
- spinal cord injuries
-congenital conditions such as spina bifida
contraindication for oxybutinin
urinary or gastric retention
Scopalamine MOA and uses
•Naturally occurring cholinergic blocker and one of the principal belladonna alkaloids
•Uses: prevention of motion sickness and to help prevent postoperative/postanesthesia N/V
Contraindications for scopalamine
-advanced hepatic and renal dysfunction
-hiatal hernia associated with reflux esophagitis
-intestinal atony
-severe ulcerative colitis
Adverse effects for scopalamine
-drowsiness
-dry mouth
-blurred vision
•Using scopolamine with CNS depressants or alcohol may increase sedation
Tolterodine is a ____ receptor drug and it is used for
-Muscarinic receptor blocker
•Uses:
-urinary frequency
-urgency
-urge incontinence caused by bladder (detrusor) overactivity
Mirabegron is a ______
•Newer agent used to treat overactive bladder
•Beta3 agonist; represents a new class of therapy for this condition
•Does not have same side effects as other medications to treat overactive bladder
kids have a _____ risk for AE when taking anticholinergics and they should not take ________
-Greater risk for adverse effects
-Dicyclomine is NOT recommended in children
adults do what when taking anticholinergics? Can preg/lactating women take these drugs?
-Monitor for adverse effects
-Drink plenty of fluids and avoid hot temperatures
-Pregnancy/lactation only if benefits outweigh risks
older adults are more susceptable to ____ and ______ so we start them on ______ doses?
- adverse effects and toxic levels
-More susceptible to heat intolerance and dehydration
-Start on lower doses
nursing implications for anticholinergics
•Assess for allergies, presence of benign prostatic hypertrophy (BPH), glaucoma, tachycardia, MI, HF, hiatal hernia, and GI or GU obstruction
•Perform baseline assessment of VS and systems overview
implication
•Medications should be taken exactly as prescribed to have the maximum therapeutic effect
•Overdosing can cause life-threatening problems
•Blurred vision may cause problems with driving or operating machinery
•Clients may experience sensitivity to light and may want to wear dark glasses or sunglasses
•When giving ophthalmic solutions, apply pressure to the inner canthus to prevent systemic absorption
implemntation
•Dry mouth may occur; can be handled by chewing gum, frequent mouth care, and hard candy.
•Clients should check with the HCP before taking any other medications, including over-the-counter(OTC) medications
•Antidote for atropine overdose is physostigmine
•Anticholinergics taken by older adult patients may lead to higher risk for heatstroke because of the effects on heat-regulating mechanisms
client teaching
•Teach clients to limit physical exertion, and avoid high temperatures and strenuous exercise
•Emphasize the importance of adequate fluid and salt intake
•Clients should report the following to the HCP
–Urinary hesitancy/retention -- Confusion
–Constipation -- Sedation
–Tachycardia -- Hallucinations
–Palpitations -- Decreased sweating
–Tremors
nursing implications
•Monitor for adverse effects
•Monitor for therapeutic effects
-For Parkinson's disease = fewer tremors and decreased salivation and drooling
For urologic problems=improved urinary patterns, less hypermotility, increased time between voiding