Heart & Neck Vessels | Chapter 20 | NURS122
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
160 Terms
precordium
area on anterior chest overlying heart and great vessels
(basically the general area on the front where the heart is)
the heart has ______ chambers
4
what are the great vessels that connect to the heart?
superior & inferior vena cava
pulmonary artery
pulmonary veins
aorta
what are the different layer of the heart wall (from outside to inside)?
pericardium (fibrous + parietal + visceral)
pericardial cavity
myocardium (heart muscle)
endocardium (endothelial tissues lining the heart chamber)
atrium
thin-walled reservoir for holding blood (like ventricle, also pump blood)
ventricle
thick-walled, muscular pumping chamber
what are the different valves of the heart?
atrioventricular (AV) valves (tricuspid and bicuspid)
semilunar valves (pulmonic & aortic)
during diastole, _______ open to allow blood into the ventricle
AV valves (both tricuspid & bicuspid)
the ventricle finished contraction, AV valve open, passive filling start, atria contract and pump out the remaining blood for active filling
during systole, _________ close to prevent backflow of blood from the ventricle back into the atria
AV valve (both tricuspid & bicuspid)
when talking about diastole and systole, we are referring to the resting and contracting of the ____________
ventricles
true or false: no valves exist between the vena cava and right atrium or between the pulmonary veins and left atrium
true
what kind of symptoms would be expected if there is high pressure in the left side of the heart?
pulmonary congestion (AKA pulmonary edema) —> left-sided heart failure symptoms
shortness of breath
coughing
wheezing
chest pain
anxiety
rapid breathing
heart palpitation
sweating
skin color
swelling
weight gain (especially in the leg)
why does high pressure in the left side of the heart cause pulmonary congestion (AKA pulmonary edema)?
pressure in the left side of the heart cause pressure to build up in the pulmonary vein, forcing fluid to leak into the lung tissues and leading to fluid build up in the lung
what kind of symptoms would be expected if there is high pressure in the right side of the heart?
right-sided heart failure symptoms
peripheral edema
abdominal edema
neck veins (jugular vein) distension (visibly swollen)
hepatomegaly (liver congestion)
general fluid retention over the body
left-sided heart failure vs. right sided heart failure
left side
concerning the lung due to high pressure in the pulmonary veins (pulmonic)
breathing/oxygenation issues
fluid build up in the lung tissues
right side
concerning the rest of the body due to high pressure in the systemic veins (vena cava) - (systemic)
fluid buildup in different area of the body
what is the complete flow of blood through the heart starting from unoxygenated blood draining into the vena cava?
unoxygenated blood drains into the vena cava from periphery
blood move from the liver and lower extremities to the right atrium via the inferior vena cava
the superior vena cava drain from the heart and upper extremities
blood travel flow from the RA through the tricuspid to the RV
RV —> pulmonic valve —> pulmonic artery
lung oxygenate the blood
oxygenated blood return to the LA via pulmonary veins
mitral —> left ventricle
LV eject blood through the aortic valve into the aorta
aorta deliver oxygenated blood to the body
loop around through continuous shifting pressure gradient
diastole occupies _____ of the cardiac cycle
2/3 (protodiastolic filling + presystole)
protodiastolic filling vs. presystole (atrial systole)
(FIRST) Protodiastolic Filling (Early Passive Filling, basically passive filling phase)
• Definition: The phase of ventricular filling where the AV valves open, and blood flows passively into the ventricles from the atria due to the pressure gradient, occurring after ventricular relaxation (diastole).
• Normal/Abnormal: Normal phase of the cardiac cycle.
(SECOND) Presystolic Filling (Atrial Systole)
• Definition: The phase when the atria contract to actively push the final portion of blood into the ventricles before ventricular contraction (systole).
• Normal/Abnormal: Normal phase of the cardiac cycle.
systole occupies ______ of the cardiac cycle
1/3
diastole
ventricle relax and fill with blood
systole
ventricle contract and pump blood through the pulmonary and systemic arteries
true or false: atrial systole occurs during ventricular diastole
true
isometric (AKA isovolumic) relaxation
start of ventricular diastole - a brief period where all four valves of the heart closed and the ventricle relax
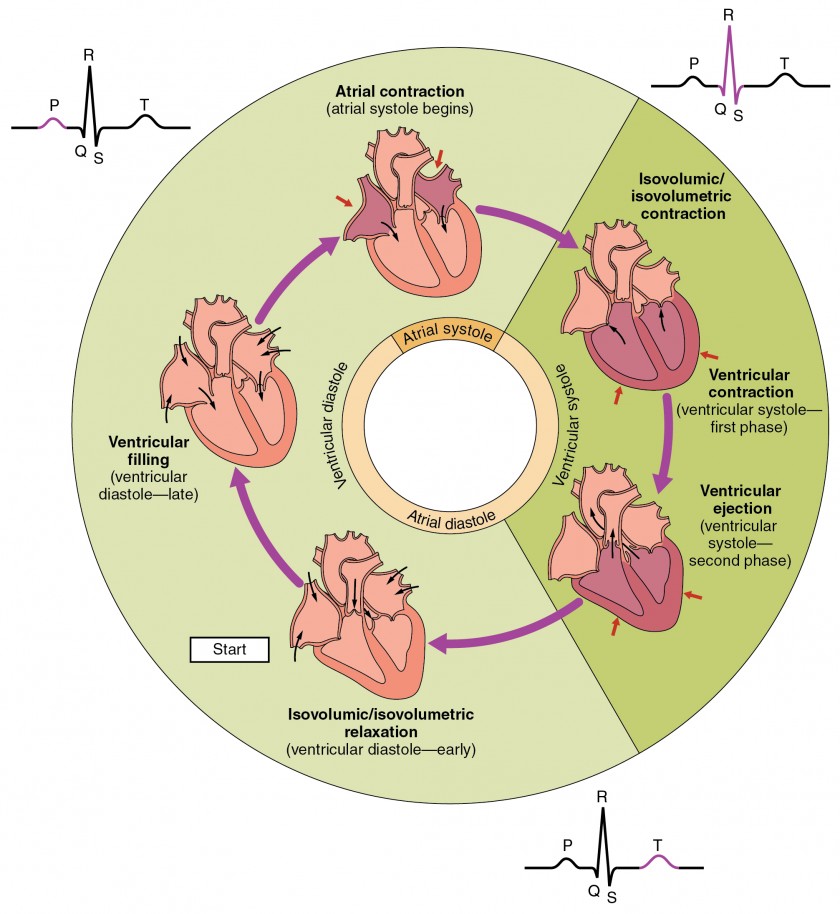
isometric (AKA isovolumic) contraction
a brief where the contraction of the ventricle does not generate high enough pressure to open the semilunar valves
ventricular ejection
a brief period where the contraction of the ventricle generate high enough pressure to open the semilunar valve
atrial diastole
atria passivel fill with blood from the vena cava (right) and pulmonic vein (left)
the blood would push open the AV valve and fill the ventricle also in a relaxed state
atrial systole
action potential from the SA node trigger atrial contraction (synchronous)
active filling of the ventricles
different phases of ventricular diastole
first 1/3 of diastole: early ventricular diastole (ventricular rapid inflow)
second 1/3 of diastole: late ventricular diastole (passive inflow/diastasis)
last 1/3 of diastole: active ventricular filling due to atrial contraction
different phases ventricular systole
isovolumetric contraction - AV and semilunar remain closed due to not enough pressure
ventricular ejection - AV closed and semilunar valve open (end-sytolic volume - how much blood remain after contraction)
S1 sound (what is it, its anatomy, and phase of cardiac cycle)
first heart sound (LUB sound)
occurs with the closure of AV valves (mitral first, M1, then tricuspid, T1)
indicate the beginning of systole
S2 sound (what is it, its anatomy, and phase of cardiac cycle)
second heart sound (DUB sound)
occurs with the closure of semilunar valves (aortic first, A2, then pulmonic, P2)
indicate the end of systole
how does inspiration affect heart sounds?
increased venous return to the right heart —> delays pulmonary valve closure
decreases venous return to the left heart —> aortic valve closes earlier
S2 split (A2 and P2 heard separately)
how does expiration affect heart sounds?
decreased venous return to the right heart —> pulmonary valve closes sooner
increased venous return to the left heart —> aortic valve closes later
S2 splitting narrow or disappear (P2 is closer to A2 then during inspiration so the effect is minimal)
true or false: S3 sound can be normal some times an pathologic other times
true
true or false: S4 is almost always pathologic unlike S3 sound
true
what are some of the quality that can be use to describe heart sound?
intensity
pitch
location
quality
timing in the cardiac cycle
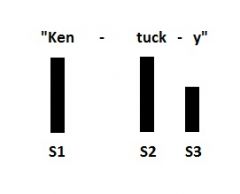
S3 (what is it, its anatomy, and phase of cardiac cycle)
third heart sound (KENTUCKY GALLOP)
occurs when ventricles already somewhat filled and there is a rapid inflow of blood from eht atrium, making it resist the passive rush of blood that enter early in diastole (high ESV than normal)
occurs immediately after S2, when AV valves open and atrial blood first pours into the ventricles
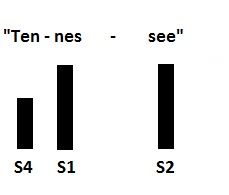
S4 (what is it, its anatomy, and phase of cardiac cycle)
fourth heart sound (TENNESSEE GALLOP)
occurs at the end of diastole, at presystole, when ventricle resist the active rush of blood that enter when the ventricle contract (occur during active filling when the atria is contracting)
occur just before S1 (when the valves closes) which it mean occur during atrial contraction)
listen to S1 sound…
listen to S2 sound…
listen to S3 sound…
listen to S4 sound…
differentiate between physiologic and pathologic S3 heart sound…
physiologic
—> common in children, young adults, athletes and pregnant women
—> due to rapid ventricular filling
—> no medical significance
pathologic
—> common in adults over 40 (especially w/ heart disease)
—> due to volume overload or decrease ventricular compliance
—> more pronounced than physiologic S3
—> indicate heart failure
heart murmurs
gentle, blowing, swooshing sound that can be heard on the chest wall
turbulent blood flow and collision currents
different from a bruit in that it can only be found in the chest and bruit are elsewhere
what are the conditions that lead to heart murmurs?
increased velocity of blood
decreased viscosity of blood
structural defects in valves (that lead to the rapid flow of blood)
what are the three types of murmurs?
systolic
diastolic
continuous
heart has the unique ability of _________
automaticity
impulse pathway of electrical activity
SA node
AV node
bundle of His
purkinje fibers
electrocardiogram (ECG/EKG)
records heart’s electrical activity via PQRST waves
—> P wave - atrial depolarization
—> P-R interval - time for impulse to travel to ventricles
—> QRS complex: ventricular depolarization
—> T wave: ventricular repolarization
echocardiogram (AKA heart ultrasound, heart sonogram)
uses sound waves to create pictures of the waves
show blood flow through the heart and heart valves
health care provider can use picture from test to find heart disease and other heart conditions
stress test
test designed to determine how well the heart works when it’s pumping blood
some heart diseases are easier to find when the heart is working its hardest to pump blood through the body
can be administered while individual exercise on a treadmill or stationary bicycle or medication that simulate the condition of exercising
what are some other option beside heart ultrasound to get pictures of the heart?
XR, CT, MRI
cardiac output
heart rate x stroke volume
what is the normal/expected stroke volume in adults?
4-6 L/min
preload
the amount of blood in the fill of the ventricles from venous return —> more blood = greater stretch = stronger contraction
afterload
the resistance the ventricle must overcome to eject blood (the higher the preload, the more the afterload)
characteristics of carotid artery pulse (normal, dicrotic notch, abnormalities)
normal: smooth with rapid upstroke and rounded peak
dicrotic notch: presence of notch indicate proper aortic valve closure
abnormalities: weak or absent pulse might suggest issues like arterial blockage, heart failure, or valvular problem
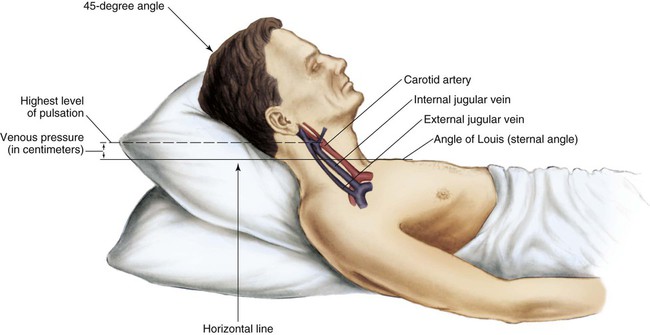
characteristics of jugular venous pulse (normal, elevated) and what would an elevated jugular venous pulse indicate?
normal: visible but not prominent
elevated: indicate increased central venous pressure —> signs of right-side heart failure, fluid overload, or obstruction
upstroke of the carotid pulse (the initial, rapid rise in pressure and pulse wave as blood is ejected from the left ventricle into the aorta.) reflects the __________ and __________
driving force; vessel compliance (like more compliance = less resistance)
downstroke of the carotid pulse reflect the _________ and __________
distensibility of vessels; peripheral resistance
isolated systolic hypertension
increase in systolic blood pressure due to thickening and stiffening of the arteries (it is isolated because only systolic pressure is not within normal limit while diastolic could still be consider regular)
true or false: as one get older, the left ventricular wall becomes thicker but the overall size of the heart does not change
true
pulse pressure _________ as we age
increases (bigger difference in upper and lower numbers of blood pressure)
true or false: despite aging, there should be no change in the resting heart rate or cardiac output at rest
true
ability of heart to augment cardiac output with exercise is _________ as we age
decreased (thus decreasing overall exercise capacity)
presence of supraventricular and ventricular dysrhythmia ___________ with age
increases
_________ (extra or skipped beats) is common in aging people
ectopic (usually asymptomatic in healthy older people)
ectopic beats may compromise cardiac _________ and blood _________ when disease are present
outputl; pressure
in older individual, the P-R and Q-T interval are ___________, but the QRS is ____________
prolonged, unchanged
incidence of CAD (coronary artery disease) ___________ sharply with advancing age
increases
true or false: CAD accounts for about half of death in older adults
true
true or false: lifestyle habits significantly impact heart disease risk
true (e.g., smoking status, diet, alcohol use, exercise, and stress)
increased physical activity in older adult ___________ the risk of cardiovascular and respiratory related death
reduces
older adult should be monitor for ______________ hypotension
orthostatic (drop in BP when standing)
true or false: occasional ectopic (extra or skipped) beats are common and are not a sign of cardiac pathology unless frequent or symptomatic
true
what is the number one cause of death worldwide:
coronary artery disease (complex interplay betweem genetics and lifestyle factors)
what are the key lifestyle recommendations for good heart health?
no current smoking
maintain a healthy weight (no obesity)
engage in physical activity at least once a week
follow a healthy diet
review the contributing risk factors for CVD (cardiovascular disease)…
family history of premature ASCVD
metabolic syndrome
chronic kidney disease
chronic inflammatory conditions
high-risk race/ethnicity
high cholesterol
high blood pressure
smoking
diabetes
obesity
physical inactivity
poor nutrition
review the CVD risk factors specific to women…
premature menopause
history of pregnancy-related cardiovascular complications
true or false: hypertension accelerates atherosclerosis (hardening of the arteries) as hypertension damages the artery walls, making them more susceptible to cholesterol buildup and plaque formation. This accelerates atherosclerosis by promoting inflammation, arterial stiffening, and an increased risk of blood clots, which can lead to heart attacks or strokes.
true
true or false: glycemic and cholesterol control is essential for prevention of CVD
true; for cholesterol LDL (bad cholesterol) contributes to plague formation
how is CVD difference for each gender?
men tend to develop CVD at younger ages and have a higher risk of coronary heart disease, while women often experience stroke at older ages and may have different symptom presentations. Furthermore, women often experience worse outcomes after acute cardiovascular events, despite potentially lower overall prevalence before menopause.
when inquiring about the severity of a patient’s orthopnea, why would asking how much pillow a patient use matter?
since orthopnea is shortness of breath that occurs when lying flat, the more people they use (the more ‘sitting’ they are to help breathing, the worse)
1 pillow - mild
2 pillows - moderate
3+ pillows - severe
orthopnea is commonly associated with ______________ as fluid builds up in the lungs when lying down, making breathing difficult
left side heart failure
what are the factors that the student nurse should ask the patient when inquiring about their edema?
onset and timing
amount and location
relief of symptoms
presence of associated symptoms
review the types of question the student nurse would ask the patient when inquiring about their cardiac history…
past cardiac history (medical and surgical)
diagnostic testing and imagine studies done (EKG/ECG, ECHO, chest Xray, Stress test)
family history
and applicable questions: nutrition, smoking, alcohol, exercise, medication
additional questions: review absence of comorbidities, Rx/OTC, aware of side effects, compliance with therapy, environment, impact on ADLs
to evaluate carotid arteries, the patient can either be ________ or __________
sitting; lying
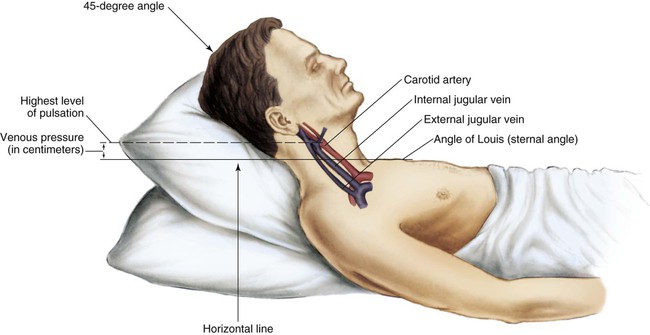
to assess the jugular veins and precordium, the patient should be ________ with head and chest slightly _________ (30-45 degrees)
supine, elevated (basiclally in a semi-sitting-laying positions)
what are the equipment needed to do a carotid arteries and jugular veins assessment?
small centimeter ruler
stethoscope with diaphragm and bell end piece
alcohol wipe to clean endpiece
what is the order of a heart and blood vessels assessment>
pulse
blood pressure
neck vessels
precordium
what are the characteristics the student nurse need to take note of when assessing peripheral pulse?
rate - the number of beats per minute
rhythm - the regularity of the beats
symmetry - pulses on both side of the body should be similar
amplitude
—> 4 - bounding
—> 3 - increased
—> 2 - normal
—> 1 - weak
—> 0 - absent or nonpalpable
review the different position and their names…
prone
supine
right lateral recumbent
left lateral recumbent
trandelenburg
fowler’s
what does assessment of jugular venous pulse tell us?
the central venous pressure (CVP)
evaluate heart efficiency as a pump
steps to assess the jugular venous pulse…
position patient supine at a 30-45 angle
observe for jugular vein pulsation
look for jugular vein distention (JVD) - may suggest heart failure
how to differentiate between the jugular and carotid pulsations?
jugular pulse
location: lower, varies with position
quality: undulating, not palpable, but observable
changes with respiration
carotid pulse
location: higher, independent of position
quality: sharp, palpable, but not observable
unaffected by respiration
true or false: jugular vein is observable, but not palpable while the carotid artery is palpable but not observable
true

true or false: when palpating the carotid artery, the student nurse should only palpate one at a time
truel; this is to avoid interrupt blood flow to the brain
at what location should the student nurse apply the stethoscope to auscultate for the carotid artery?
angle of the jaw
mid cervical area
base of the neck
carotid bruit
whooshing sound indicating turbulent flow in the carotid artery
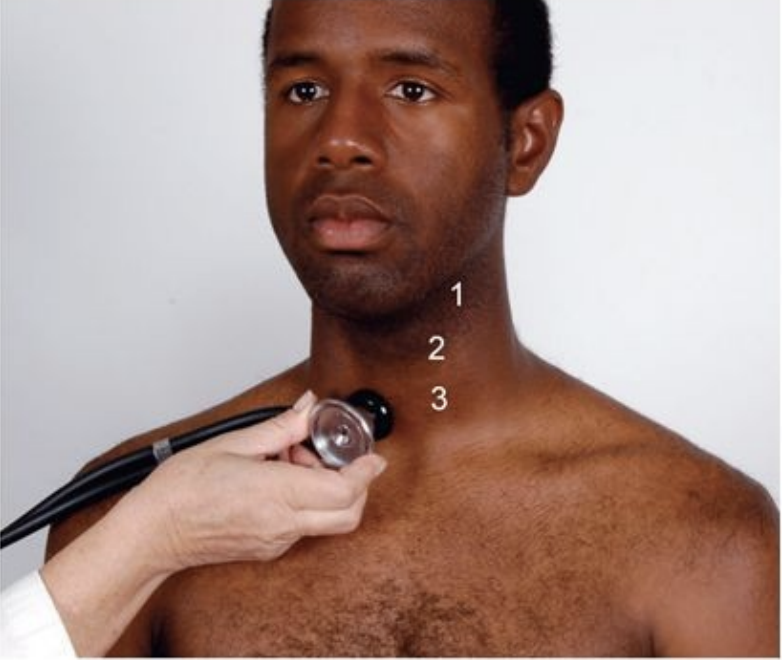
should the student nurse use the bell or diaphragm to assess for carotid bruit?
bell
