Interpretation of Caries
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
What are the components of Caries Assessment?
Patient history + Clinical Exam + Radiographic Exam —> Caries Diagnosis
What are the components of clinical detection?
Location
Extent
What is the G.V Black Classification of caries?
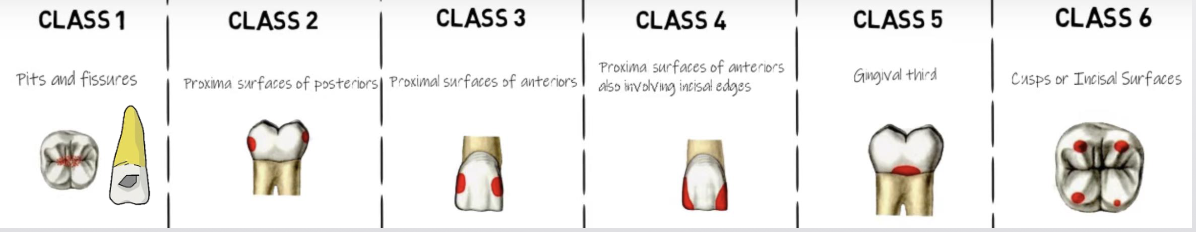
What is the importance of clinical detection
Can identify lesions on directly visible/exposed tooth surfaces clinically
Caries on proximal surfaces are nearly impossible to identify clinically until cavitation has occurred
At this point, more invasive treatment is usually indicated
Transillumination can help identify Class 3 caries earlier

What is the caries process?
Demineralization → destruction
Greater rate of demineralization in dentin due to lower mineralized component than enamel
What is the radiographic importance of caries process
Decrease in density → greater x-ray penetration in carious area → radiolucency
Degree of radiolucency increases with extent
What is the imaging modality for caries assessment?
Intraoral (BWs > PAs) 7-20 lp/mm depending on the receptor type
BWs have the highest spatial resolution
The role of bitewings is to detect small interproximal caries before they can generate symptoms or become clinically visible
Imaging Modality for Panoramic Images
Caries visible on a panoramic image are often large enough to be
clinically apparentShould not rely on panoramic to detect caries (especially small lesions)
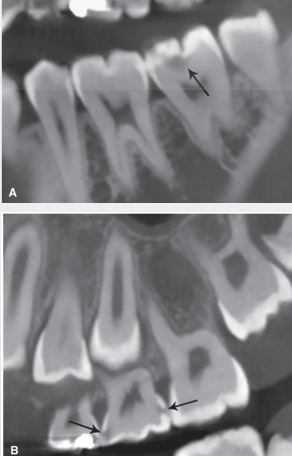
Imaging Modality for CBCT
Many studies show CBCT caries detection rates are approximately equivalent to intraoral modalities for non-restored teeth
Beam-hardening and streak artefacts from metal objects are limiting factors
Use of CBCT solely for purpose of caries detection is discouraged and not evidence based
Increased patient dose and cos
What are the steps for radiographic evaluation of caries detection?
Location
Tooth number
Involved surfaces
Depth
Primary vs. recurrent/secondary caries
What is primary caries?
Unrestored tooth surface
What is recurrent/secondary caries?
Associated with a restoration, caries associated with restorations/sealants (CARS)
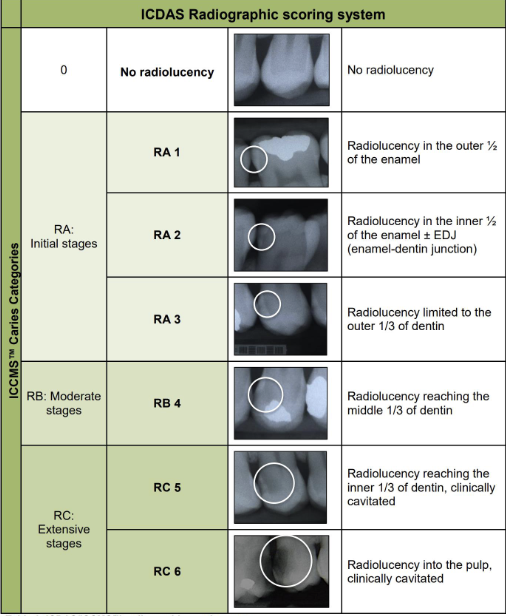
What are the classification systems for radiographic interpretation of caries?
Multiple classification or scoring systems to categorize caries size and depth
International Caries Classification and Management System (ICCMS) builds on International Caries Detection and Assessment System (ICDAS) for caries staging by including patient information (caries risk)
Merged ICDAS/ICCMS assigns caries progression to one of four stages of tooth involvement
Sound surfaces (code 0) – No radiolucency
Initial stage caries (RA) – outer half of enamel (RA1), inner half of enamel with or without DEJ involvement (RA2), and outer third of dentin (RA3)
Moderate stage caries (RB) – middle third of dentin (RB4)
Extensive stage caries (RC) – inner third of dentin (RC5), reaches the pulp (RC6)
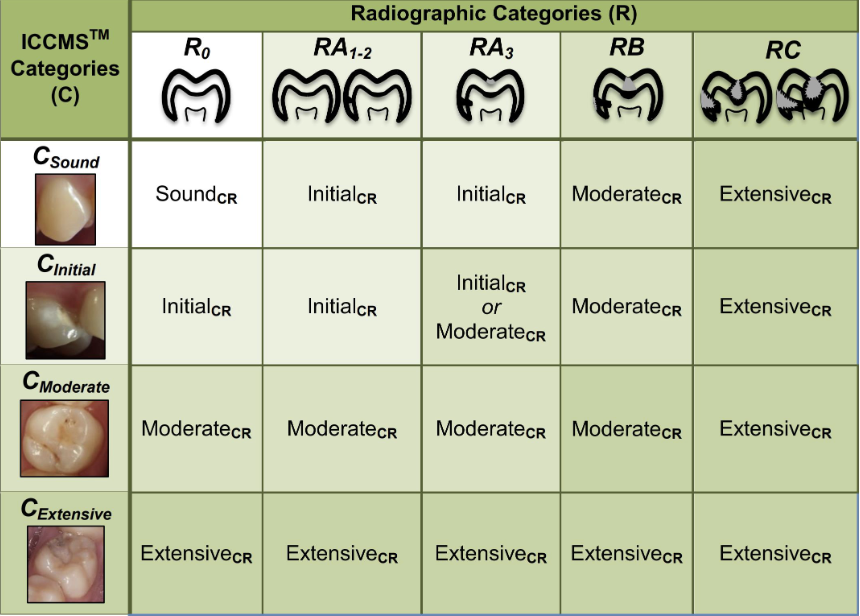
Radiographic depth and cavitation
Once cavitation occurs, bacteria will maintain carious lesion activity unless it is surgically managed
Can reliably predict tooth surface is cavitated and dentin heavily infected when radiographic penetration depth is deeper than outer 1/3 of dentin
32% of radiographically visible lesions that extended into the outer third of dentin show cavitation
72% of lesions extending into the middle third of the dentin or deeper were cavitated
Clinically classified under ICDAS/ICCMS as moderate and extensive stage
ICDAS-ICCMS Classification System
Radiographic Categories and Clinical Categories
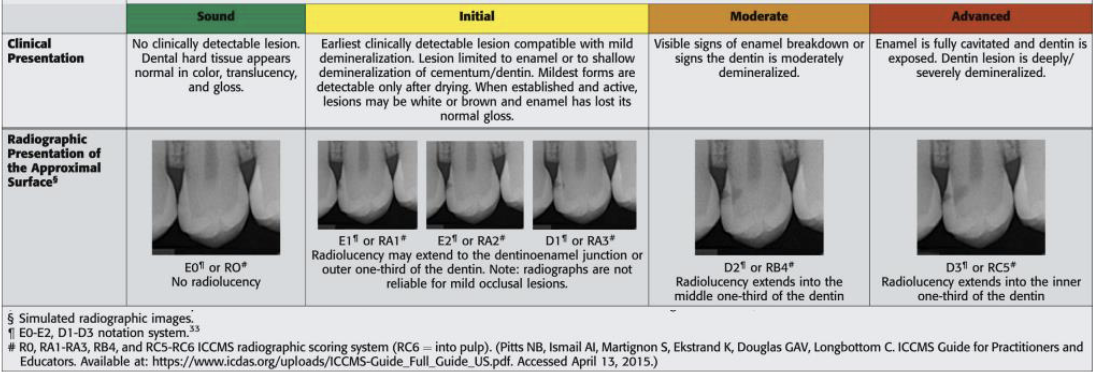
ADA Caries Classification System
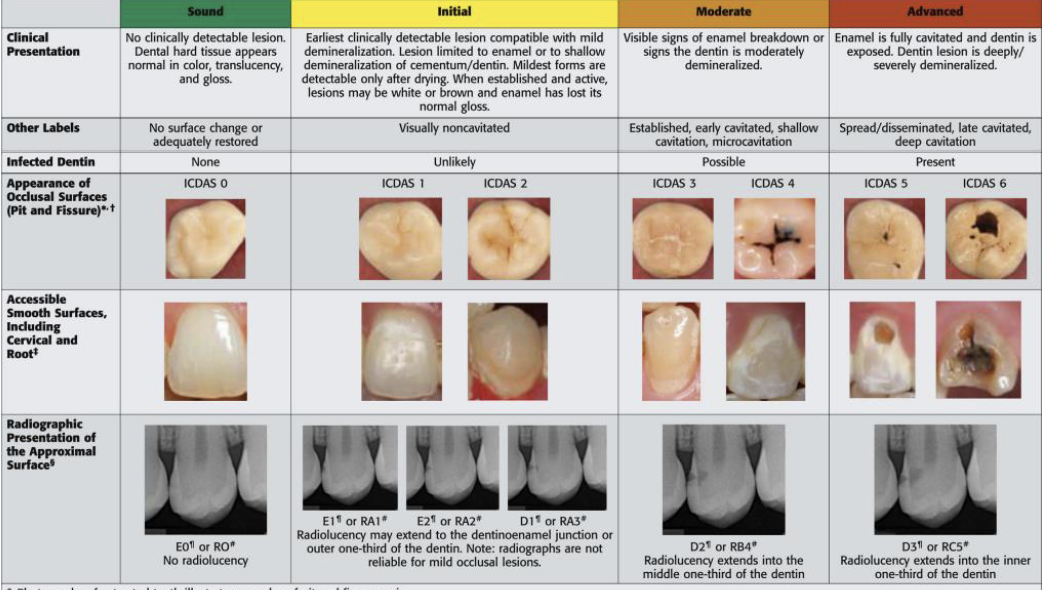
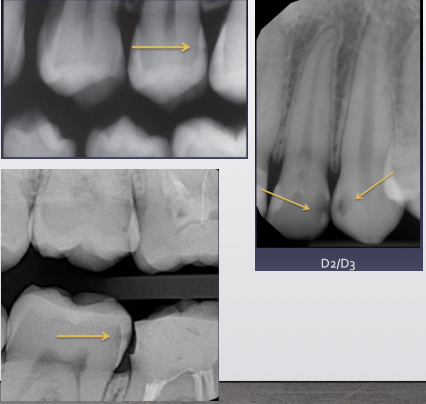
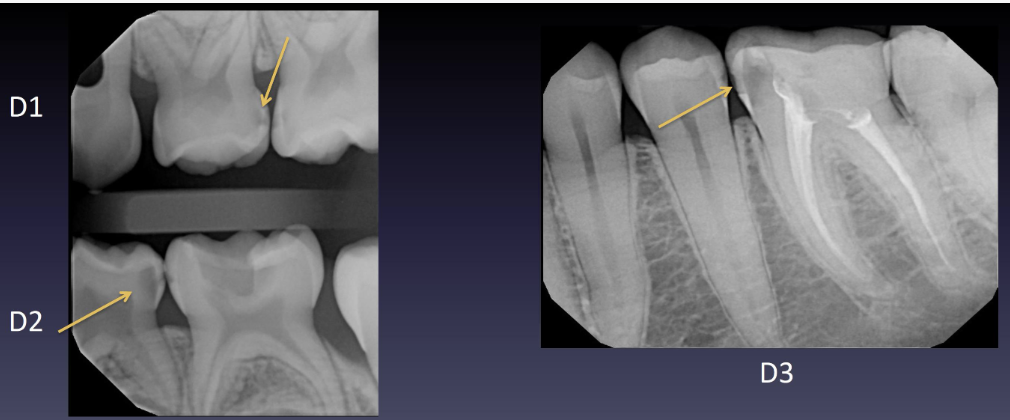
What is the ADA caries classification system?
To outer ½ enamel (E1)
To inner ½ enamel ( E2)
To outer 1/3 dentin (D1)
To middle 1/3 of dentin (D2)
To inner 1/3 of dentin (D3)
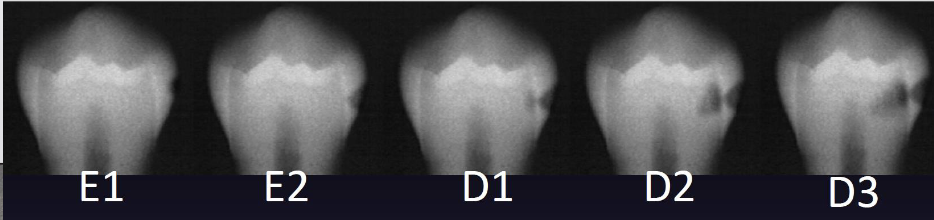
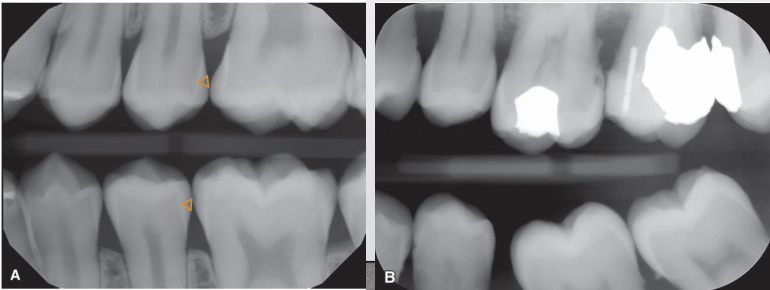
What does this image show?
Caries within the outer half of the enamel (RA1, E1)
What does this image show?
Caries within the outer third of the dentin (RA3, D1)
What does this image show?
Caries within the inner third of the dentin (RC5, D3)
What does this image show?
Caries within the inner half of the enamel (RA2, E2)
What does this image show?
Caries within the middle third of the dentin (RB4, D2)
What does this image show?
Caries in contact with the pulp (RC6, D3)
Decision to treat a carious lesion surgically is based on
Caries risk status of the patient
Depth of the lesion
Whether there is cavitation
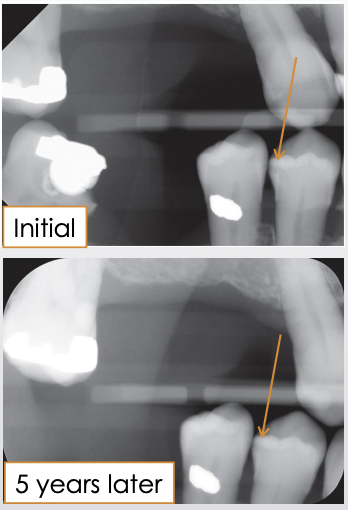
When decision made not to manage lesion surgically, follow-up imaging schedule developed to monitor
Follow-up period based on patient’s caries risk
New images should be as similar as possible to original for accurate comparison
See if lesion has grown (active) or not (arrested)
If lesion has progressed, decision regarding surgical treatment may be revised
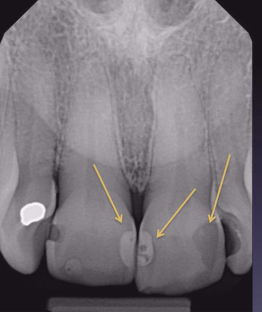
What is the susceptible zone?
Between the contact point of the teeth and gingival margins. And it may extend apical to this zone only if there is periodontal bone loss
Where is there a higher risk of caries developing?
On interproximal surface in contact with carious lesion or restoration
What are some treatment considerations?
Conservative interventions (oral hygiene, fluoride) for ICCMS RA categories (involvement of enamel or *outer 1/3 of dentin)
Surgical management when there is cavitation or the lesion has reached middle third of dentin (RB4, D2)
Differences in management strategies mostly based on caries risk status
Higher risk would benefit from more proactive approach
What are incipient caries?
DO NOT extend into DEJ, most often defined at extending ½ through enamel
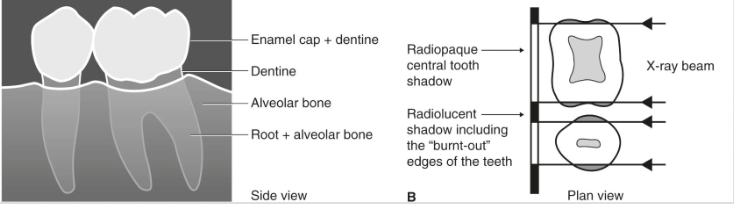
What shape would you see in incipient caries?
Triangle with broad base at outer surface
Demineralization occurs along long axes of enamel rods (oriented 90 ̊ to enamel surface)
Other shapes: band, rectangle, semicircular notch
What are primary caries?
Involves DEJ or extends through
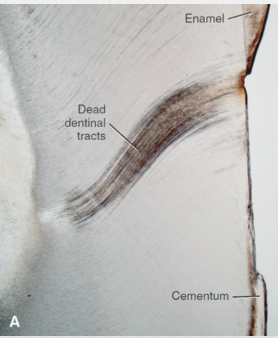
What is the caries progression of primary caries?
Once lesion reaches DEJ, demineralization spreads across the interface
Second triangle forms with broad base at DEJ
Dentin triangle has a wider base than enamel
Lesion progresses through dentinal tubules toward pulp
Triangular shape may be lost as lesion gets bigger due to curvilinear or “S-shaped” arrangement of dentin tubules
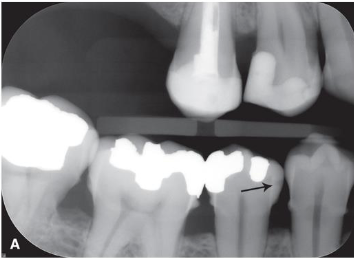
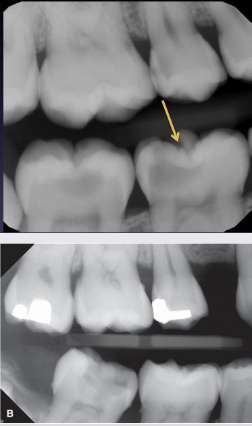
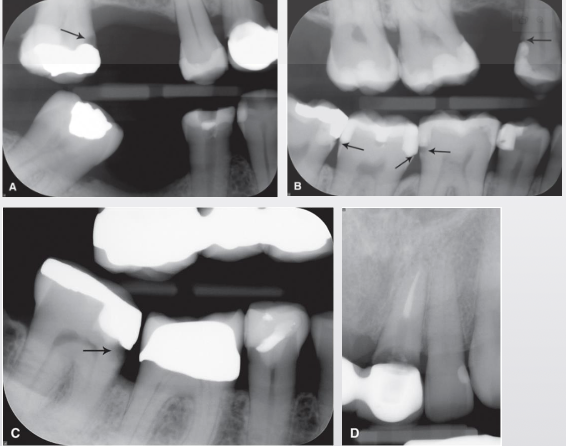
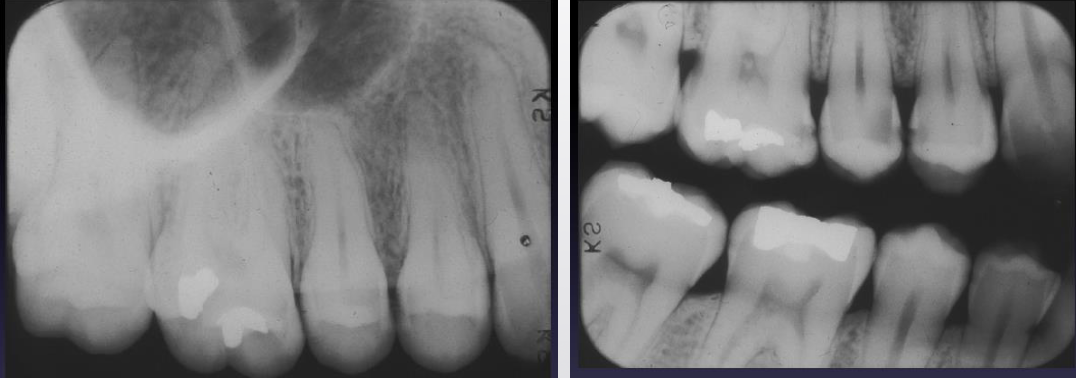
Interproximal Lesion Examples
Primary dentition
Primary teeth have thinner enamel
Dentin reached more quickly
More rapid progression
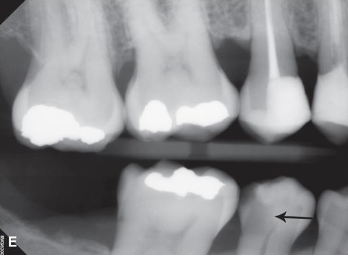
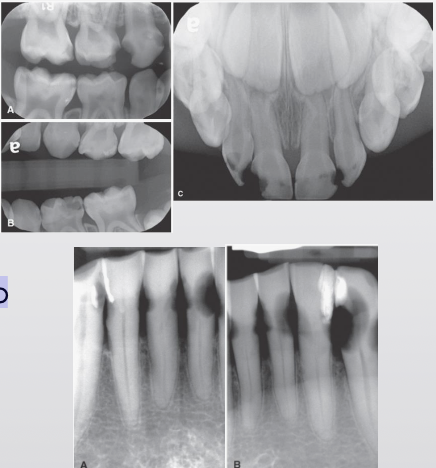
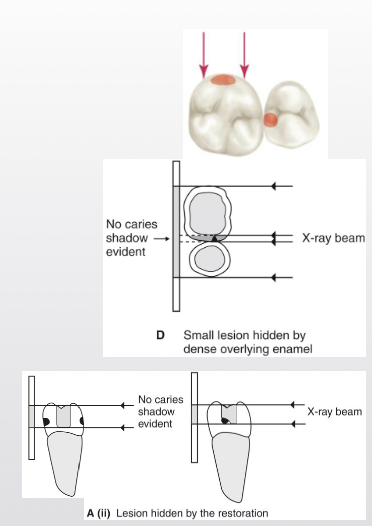
What are occlusal caries?
Large lesions easily observed clinically and radiographically
Large, dark circles in crowns
Pulp exposure can not always be determined
Not very effective at detecting small lesions
Minimum or no changes in enamel
Near impossible to identify enamel-only lesions (enamel too thick)
Thin line, triangle or cup shaped zone under enamel with base at DEJ
Easier to identify in panoramic radiographs
Clinical exam important
High false negative rate in 2D radiographs
Examples of occlusal caries

What are buccal and lingual caries?
Identified from clinical exam
Arise in cervical region, pits or fissures
Well-defined ovoid radiolucency
Surrounding structure intact
Need 2 images at different angles to localize (SLOB)
Can be confused with occlusal due to superimposition
Occlusal usually not as well defined
What are root caries?
Patients with gingival recession and/or bone loss
Cratering on buccal/lingual/proximal root surfaces of teeth involving cementum
Cementum is soft and thin
Often involves CEJ
Most can be detected clinically
Saucer like irregular cavitation
Can be confused with cervical burnout
What are rampant caries?
Rapid progression with severe widespread involvement
Most often in
Young children – poor hygiene and dietary habits
Patients with xerostomia – often secondary to head/neck radiation therapy
“Radiation caries” seen on surfaces and teeth that do not usually present carious
Often cervical location
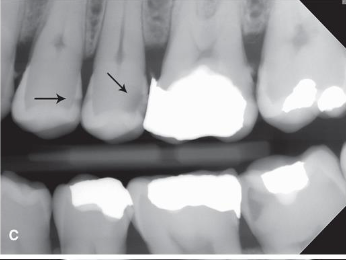
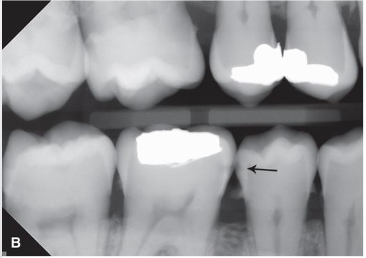
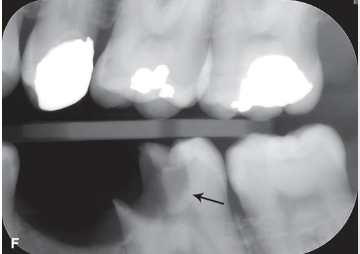
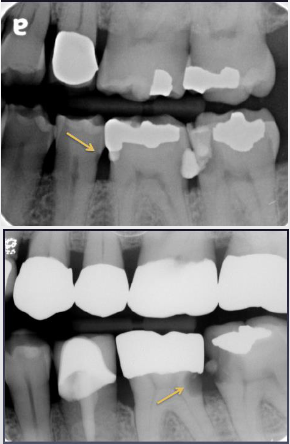
What are recurrent (secondary) caries?
New areas of demineralization that develop at margin of existing restorations
Can be caused by defective restoration and/or ineffective hygiene
Radiolucencies in tooth structure at junction of restoration and tooth
Best image for detection is BW due to beam angulation
Can use 2nd image at different angle to help distinguish if in doubt
What are residual caries?
Represent areas of demineralization that remain when the original lesion has not been completely removed
Can be involuntary
Most often purposeful when a large lesion encroaches on the pulp
Examples of recurrent caries

What are some limitations and pitfalls?
False Positives
Cervical burnout
Mach band effect
Radiographic vs. clinical depth
Caries activity
Impact of angulation and superimposition in 2D images
What are false positives?
When a carious lesion is thought to be detected on image but tooth structure is actually intact
Studies show observers consistently have < 100% agreement on caries diagnosis
Especially true with enamel caries
Most common source of false-positives: misinterpretation of cervical burnout
Lack of training or experience
Technical errors (ex. contact overlap)
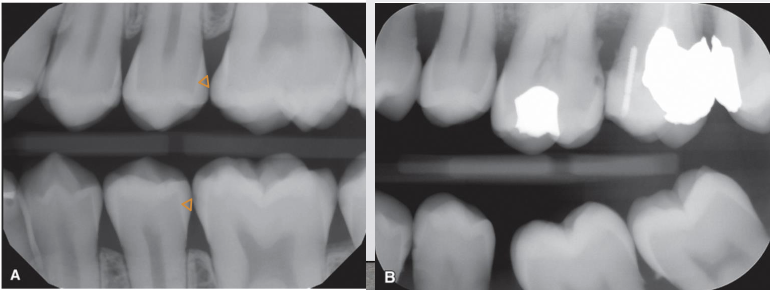
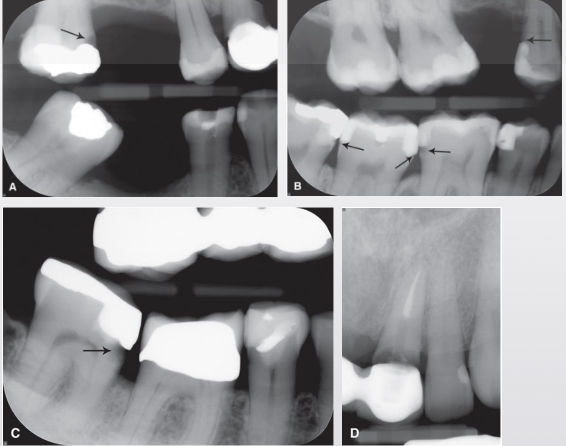
What is cervical burnout?
Artifact that can mimic caries
Commonly at or just apical to CEJ near alveolar crest
X-rays passing tangentially through proximal area encounter less structure
Thinner tooth structure absorbs fewer x-rays → appears relatively more radiolucent
Shallow depression/concavity on mesial/distal root surface can make area appear more radiolucent
Imperfect mesiodistal overlap of roots in multirooted teeth
Confirm by identifying PDL spaces of each roo
Radiographic interpretation of PA
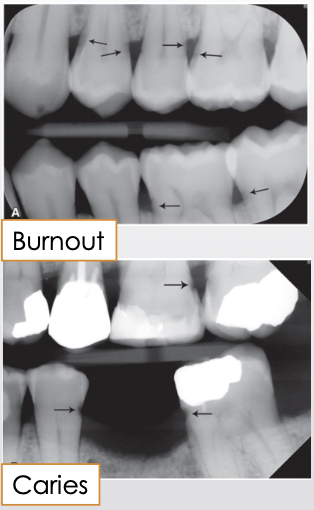
What is the Mach Band Effect?
Artifact caused by differential contrast between more opaque enamel and less opaque dentin
Optical illusion from differential stimulation and inhibition of neighboring receptors in retina
Retinal receptors overstimulated by enamel opacity inhibit adjacent receptors that perceive more radiolucent dentin
Results in perception of a radiolucent band in the superficial dentin adjacent to DEJ
To overcome Mach-band effect
Mask the more radiopaque enamel
If the radiolucent band disappears, not caries
If continues to be seen, caries
If lesion visible only on image without clinical evidence
Monitor/observe to avoid unnecessary treatment

What are some depth limitations?
Caries are further advanced clinically than radiographs indicate
Bacterial penetration of dentinal tubules and early demineralization do not produce enough change in density to affect x-ray attenuation
Estimated that enamel demineralization must be > ~35% before lesion can be observed on image
What are some activity limitations?
Demineralization (radiolucency) detected on image does not equate to active carious lesion
Can represent older, inactive (arrested) lesion (scar in enamel)
Remineralization of surface is possible due to contact with calcium and phosphorus in saliva
Cannot penetrate deeper
Second image at another time point is required to differentiate active from arrested caries
What are some 2D superimposition limitations
Degree of radiolucency is determined by extent of caries in buccolingual plane
Caries depth relative to pulp
Appearance of exposure could be result of superimposition
Small amount of demineralization may not be visible
Tooth with broad contact does not show caries as well – greater density of tooth structure surrounding caries
True depth of lesion often greater than visible on image
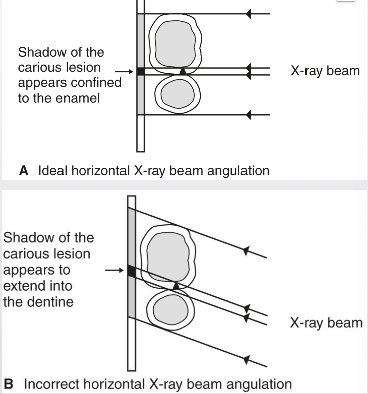
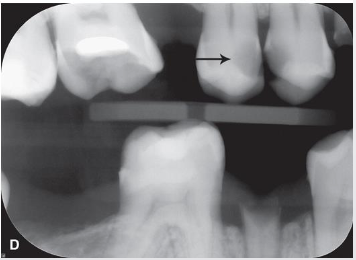
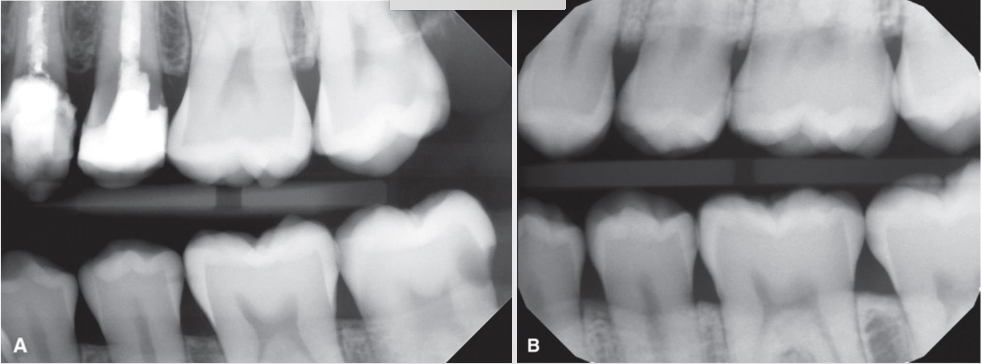
What are some 2D angulation limitations
Change in angulation impacts ability to detect and stage caries lesions
Horizontal angulation
Contact overlap can obscure lesion and DEJ
Changes projection of lesion relative to other structures
DEJ, pulp
What are some 2D vertical angulation limitations
In presence of restorations
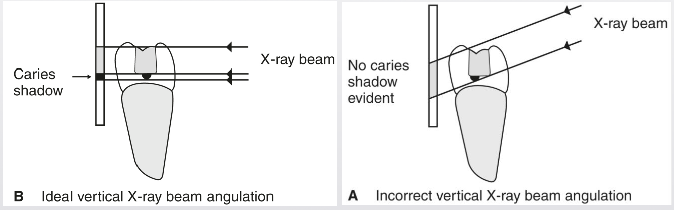
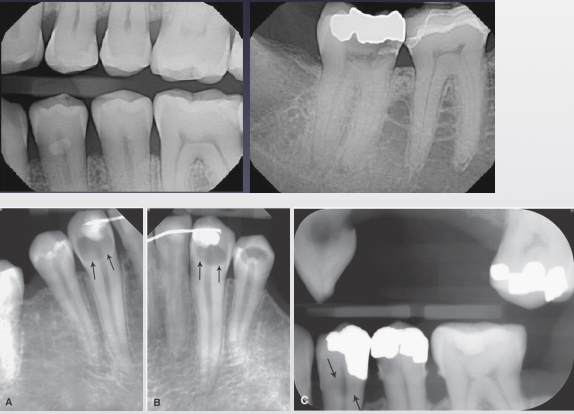
Examples of 2D angulation limitations
A. BW with correct vertical and horizontal angulation of x-ray beam demonstrating carious lesion on the distal surface of the maxillary left first molar.
B. BW of the same patient with incorrect horizontal angulation causing an overlap of the interproximal regions, hiding the carious lesion
C. PA of same patient with incorrect vertical angulation, causing an overlap of the coronal restoration with a portion of the root, again hiding the carious lesio
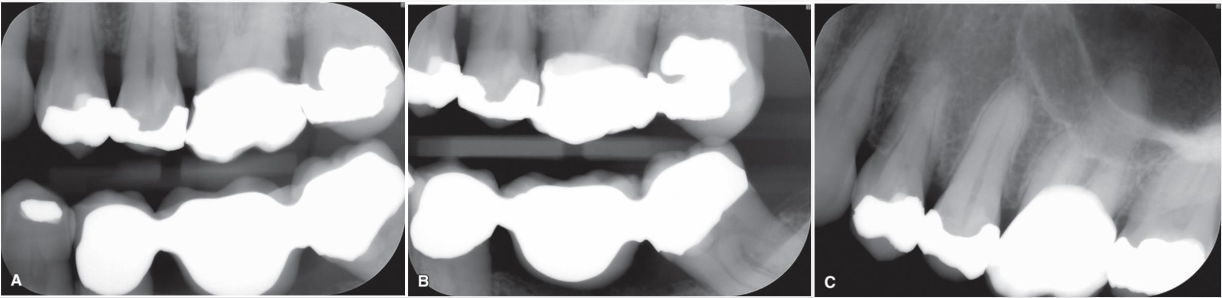
Examples of 2D angulation limitations
What are some differential diagnoses for caries?
Unfilled Cavity Preparations
Usually sharply marginated unless secondarily affected
Radiolucent restorations - older restorative materials completely radiolucent
"C" shape of prep helps distinguish
Cervical Burnout - overpenetration of cervical area of tooth due to decrease in mass and density of tooth structure
Can extend below level of bone; caries does not
Mach Band Effect - optical illusion producing radiolucency along DEJ
Idiopathic Cervical Resorption – type of external resorption
Dental Anomalies - irregularities and hypoplasias
Tooth Wear - physiologic (attrition) or non-physiologic (abrasion & erosion) wear will result in low-density areas that may mimic caries
Abfraction – non-carious cervical lesions