SSS Week 7
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
10 Terms
Dermatitis vs eczema
terms are used interchangeably but … technically eczema is a type of dermatitis.
Dermatitis refers to any cause of skin inflammation affecting the epidermis
Eczema - oedema within the epidermis (called spongiosis)
Acute vs chronic dermatitis
Acute - red, wet, oozing, even blistering
Chronic - skin thickened, dry, scaly, and fissured (lichenification - secondary lesion)
Subacute - stage between acute and chronic so will show features of both
Seborrhoeic dermatitis
(endogenous)
red itchy patches (which become scaly or crusted)
caused by combination of endogenous factors and overgrowth of malassezia furfur yeast
dermatitis may be aggravated by a combination of endogenous factors - illness, stress, fatigue, change of season, and reduced general health (eg. especially infection with HIV)
Infantile seborrhoeic dermatitis
characteristic cradle cap ‘greasy’
erythematous but non-itchy rash, well defined and covered in greasy scale… (sebaceous glands release a greasy substance that makes old skin cells attach to scalp as they try to dry and fall off)
the rash may spread to affect armpit and groin folds (via flexures)
possibly due to overactive sebaceous glands in skin of newborn babies due to maternal hormones still in baby’s circulation
super-infection with staph and candida albicans is common resulting in weeping and crusting
treatment: for
mild/localised - use gentle emollient or repeated shampooing, remove scales with a soft toothbruhs or comb
extensive/resistent - treat with low-potency topical steroid or antifungal for 1-2 weeks…. topical steroid preferred if significant inflammation
Adult seborrheic dermatitis
usually appears at any age after puberty
exacerbated by emotional and physical stress
clinical features: erythema and fine, greasy scale on cheeks, nose and nasolabial folds
scale and itching of scalp and eyebrows
well defined but non scaly, erythema of axillae, groin, scrotum and perianal skin
management:
scalp:
anti-dandruff shampoos containing selenium sulphide, ketoconazole, miconazole or zinc pyrithione (which all control malassezia)
tar containing shampoos are also helpful and combination of a tar and antifungal shampoo gives better control than either alone
non scalp areas:
topical steroids first and consider adding topical antifungal agent for malassezia
weak tar creams such as LPC 2% cream may assist (you used this! for something else tho)
Atopic dermatitis (+aetiological factors* (5), clin features (5), distribution, treatment 9) + pityriasis alba
(endogenous)
most common form of dermatitis
atopic eczema also associated with asthma, allergic rhinitis (hayfever), food allergies
aetiological factors
family history
immune dysregulation - increased IgE due to Th2 immune dysregulation
abnormal epidermal barrier - deficiency of fillaggrin (an epidermal protein) which causes impaired skin barrier which holds water poorly and is more susceptible to irritants and allergens
susceptibility to infection - epidermis is deficient in peptides known as defensins
environmental irritants - bc of the impaired epidermal barrier eg. soap, sand, woollen, synthetic fabrics and dust
clin features
a patchy erythematous, poorly defined rash
xeroderma - dryness of skin
excoriation (de to scratching and itching)
lichenification (prurigo may develop)
in bacterial infections crusting and weeping
Distribution
infants
cheeks are often first place
may have widely distributed small patches of eczema
napkin area is frequently spared due to mositure retention of nappies
tends to be vesicular and weeping
in babies of non-caucasian descent, a micropapular variant is common (instead of vesicular) and temporary hypo/hyperpigmentation may occur
toddlers and pre-schoolers
as children begin to mvoe around, eczema becomes more localised and lichenified
flexor aspects of joints (wrists, elbows, ankles, and knees +maybe genitals)
some individuals have reverse presentation where it affects the extensors
some develop discoid pattern
adults
become quite localised involving hands, eyelids, nipples, genital area, lips or face
in severe: it may involve entire skin (erythroderma)
TREATMENT
explanation fo chronicity and overall good prognosis (requires long term management not just reactive care, also need to treat flareups)
modification of lifestyle to avoid exacerbating factors
use of moisturisers and bath additives (use of emollients and bath oils)
investigation and treatment of infection (MCS if flare ups, antibiotics), for recurrent or chronic, add a very dilute chlorine bleach to water
discussion, possible investigation and treatment of allergy (allergy testing)
use of topical anti-inflammatory agents (MAINSTAY- TOPICAL CORICOSTEROIDS)
understanding role of anti-histamines (minimal use as not much benefit)
use of wet dressings
understanding psychological issues
other options
Pityriasis alba
low-grade type of atopic dermatitis mainly seen in children
mild scattered areas of facial eczema complicated by depigmentation on face
several round or oval slightly scaly pink patches appear, leaving pale marks when redness faded
regresses spontaneously
more apparent in summer, especially in dark-skinned children
management: weak topical corticosteroid, emollient and soap avoidance
once dermatitis is controlled, sun exposure will return the pigment
Discoid dermatitis (two forms)
(endogenous)
affects middle age and elderly
OFTEN with a previous history of atopic dermatitis
pink, red, brown and well defined, dry cracked surface and can have blistered or crusty surface
TWO FORMS
exudative (wet) nummular dermatitis: oozy papules, blisters and plaques
dry nummular dermatitis: red scaly, very itchy, discrete, round or oval plaques with well defined edge
may be symmetrical
lichenification can occur rapidly due to intense scratching
affects any part of body particularly lower leg
treatment: similar to atopic dermatitis
moderately potent topical steroids are usually requried
lichenified lesions may require very potent topical steroids or intralesional steroids
wet wraps
antibiotics if bacterial infection
Stasis dermatitis (+complications (8) and management)
occurs on lower legs due to chronic venous hypertension
mainly in elderly women
look for venules, phlebactasia and brown haemosiderin deposition around ankles (early signs)
characteristic dryness, scale and brown hyperpigmentation (due to diapedesis of red blood cells from peripheral circulation into dermis, eczema and ulceration can subsequently develop
usually associated varicose veins, woody oedema (due to lipodermatosclerosis)
allergic contact dermatitis may coexist (eg. bandages or leggings for chronic venous hypertension may be an irritant/allergen)
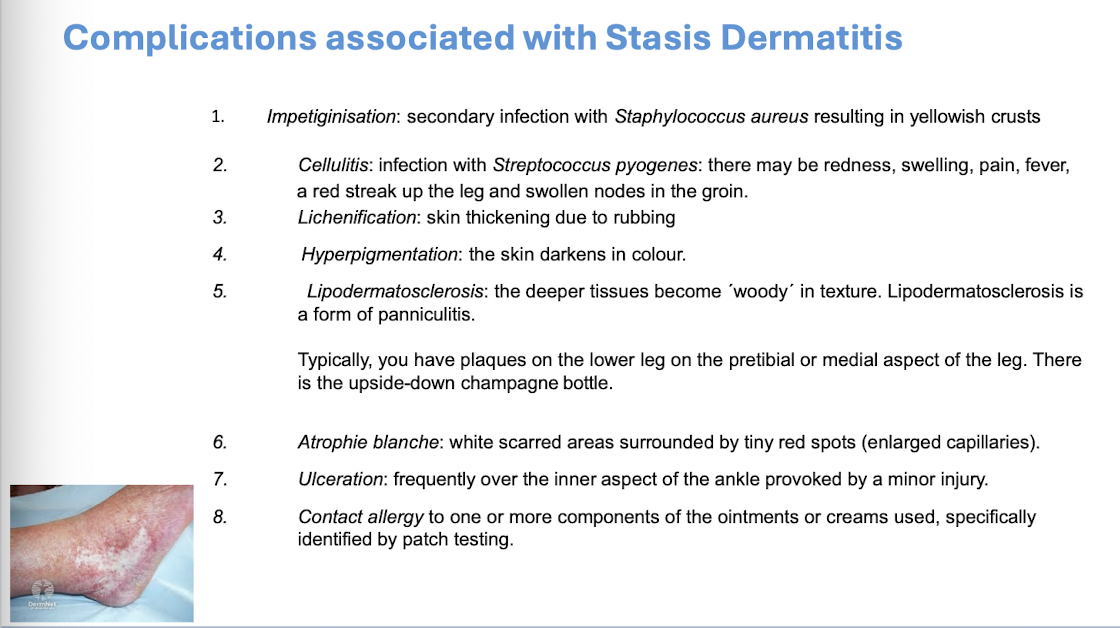
Management
dryness is managed by avoidance of soap, using a soap substitute and application of a greasy moisturiser at least twice a day
inflammation treated by moderate topical corticosteroid
acute attacks are settled by short bursts of potent topical corticosteroids, wet dressings and antibiotics if an infection (like discoid and atopic management)
In order to treat and prevent you need to treat the cause of the stasis dermatitis by attention to the underlying venous insufficiency. This involves compression bandaging or stockings and elevation of the foot of the bed at night
Pompholyx (dyshidrotic) dermatitis
(endogenous)
a vesicular or bullous dermatitis
affects palms, sides of fingers and soles of feet
cause: unknown, may be precipitated by stress, sweating and overheating
acute stage: vesicles deep in skin of palms, fingers, instep or toes, the blisters are often intensely itchy or have a burning feeling, the condition may be mild with only a little peeling or very severe with large blisters and cracks
Management
Management is the similar as for other dermatitis.
Potent topical corticosteroids should be used initially with wet dressings and antibiotics if secondary bacterial infection.
Rest is important and because of the location on the hands this can mean time off work for adults.
After an acute attack, the skin is vulnerable, and patients need to protect their hands from irritating substances including soap for three months.
Very severe attacks of bullous Pompholyx may require a 2-to-3-week course of oral prednisone.
Asteatotic Dermatitis
(miscellaneous)
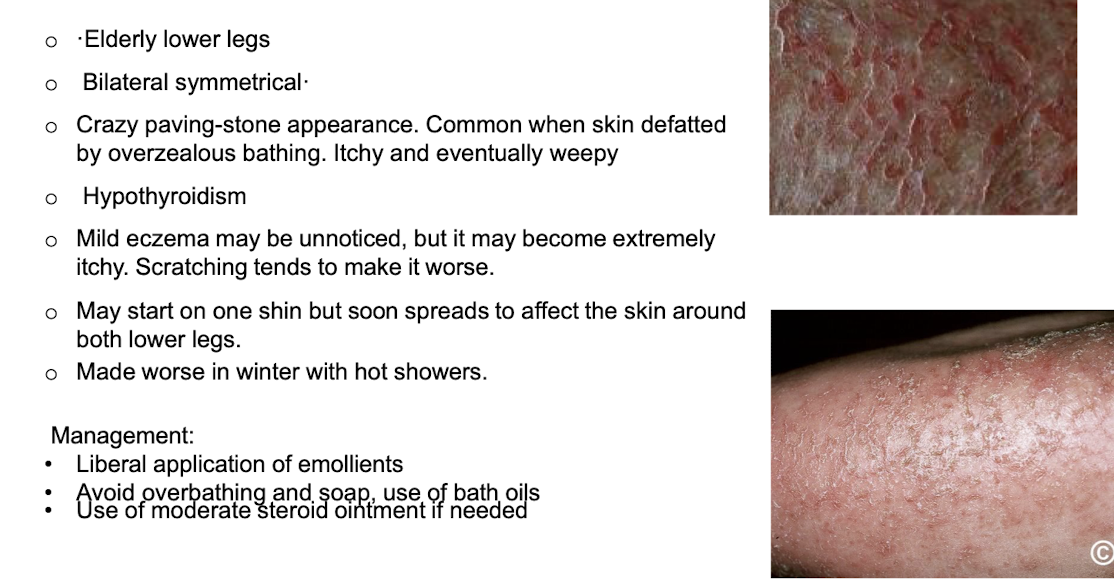
hypothyroidism can contribute to condition
Irritant dermatitis
(exogenous)
Cause
Strong irritant elicit an acute reaction after brief contact
Sometimes a weak irritant over many years
Usually, hands and forearms
E.g. water, detergents, chemicals, oils o Previous Atopic dermatitis increases the risk
Often on backs of hands, between fingers, Napkin area
Dry "chapped". Later thickened and fissured
more likely in Cleaners, catering, hairdressing, engineering, health workers
Investigations - patch testing with irritants is not helpful but with common allergens may be
treatment
avoidance of irritant
protective gloves and clothing
barrier cremes more for prevention
avoid harsh solvents when cleaning hands
emollients
corticosteroids
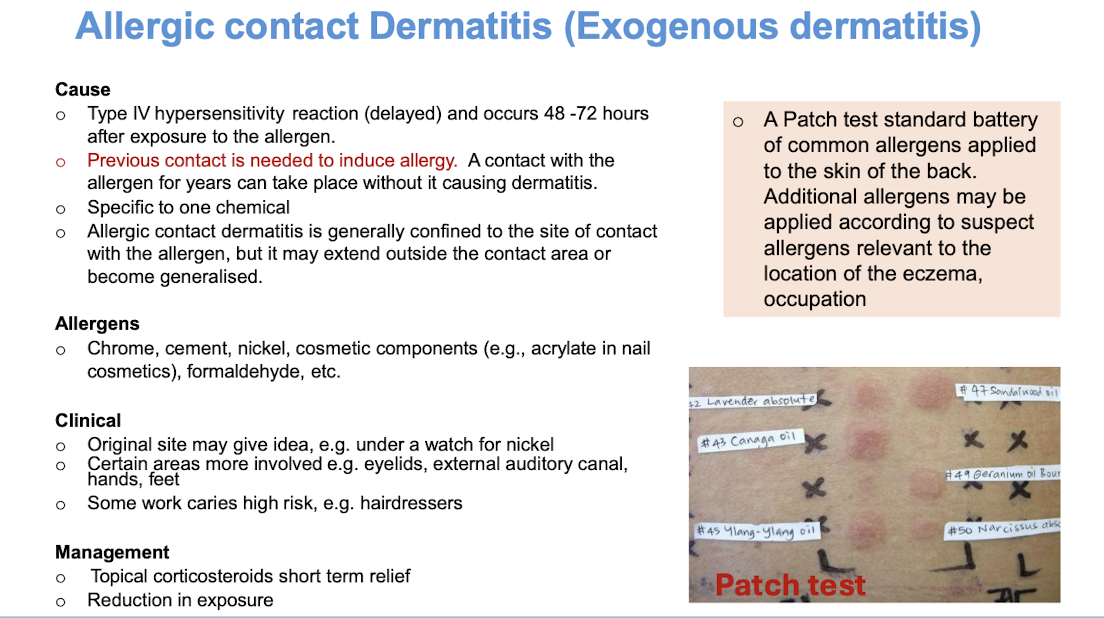
Allergic contact dermatitis
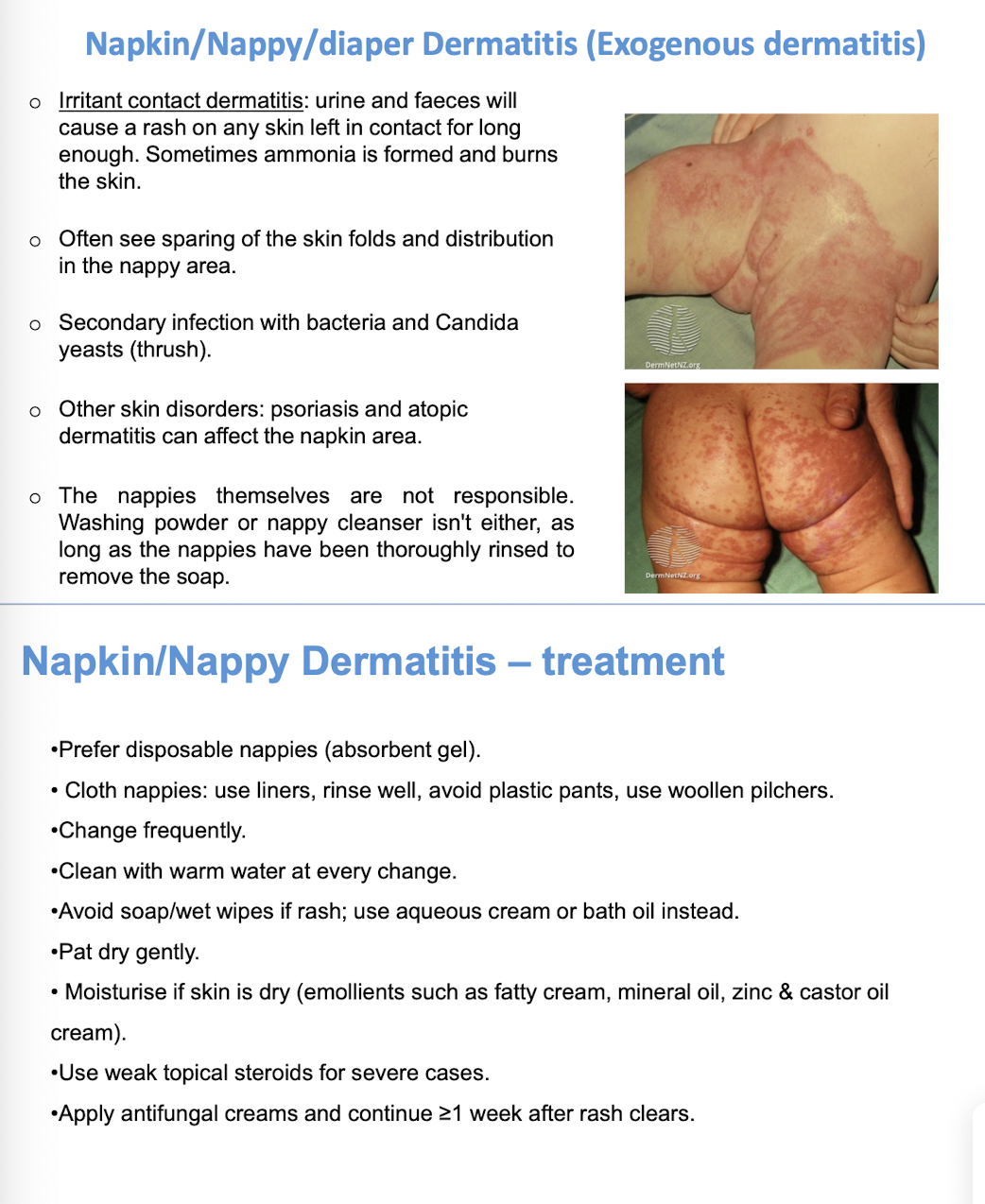
(exogenous)