Urinalysis ACS lecture 2
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Urine production
Kidneys filter blood, the filtrate is urine.
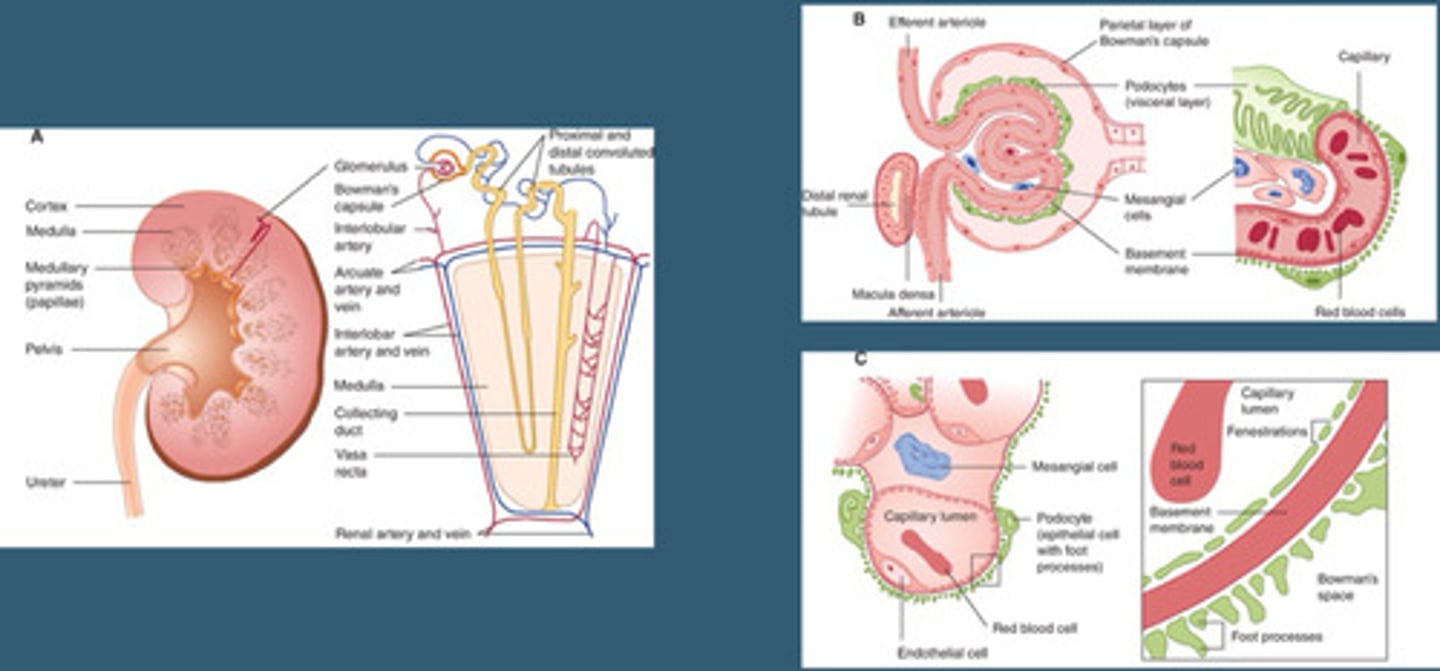
The glomerulus is...
A capillary
Red blood cells go through...
Capillary of glomerulus
What doesn't go through the capillary of the glomerulus?
Big molecules like protein, glucose and other materials that diffuse out of urine
After diffuse out of glomerulus capillaries...
The body reabsorbs its materials
At high blood glucose levels
Your kidneys cannot reabsorb all the glucose being filtered out, so it gets pee'd out.
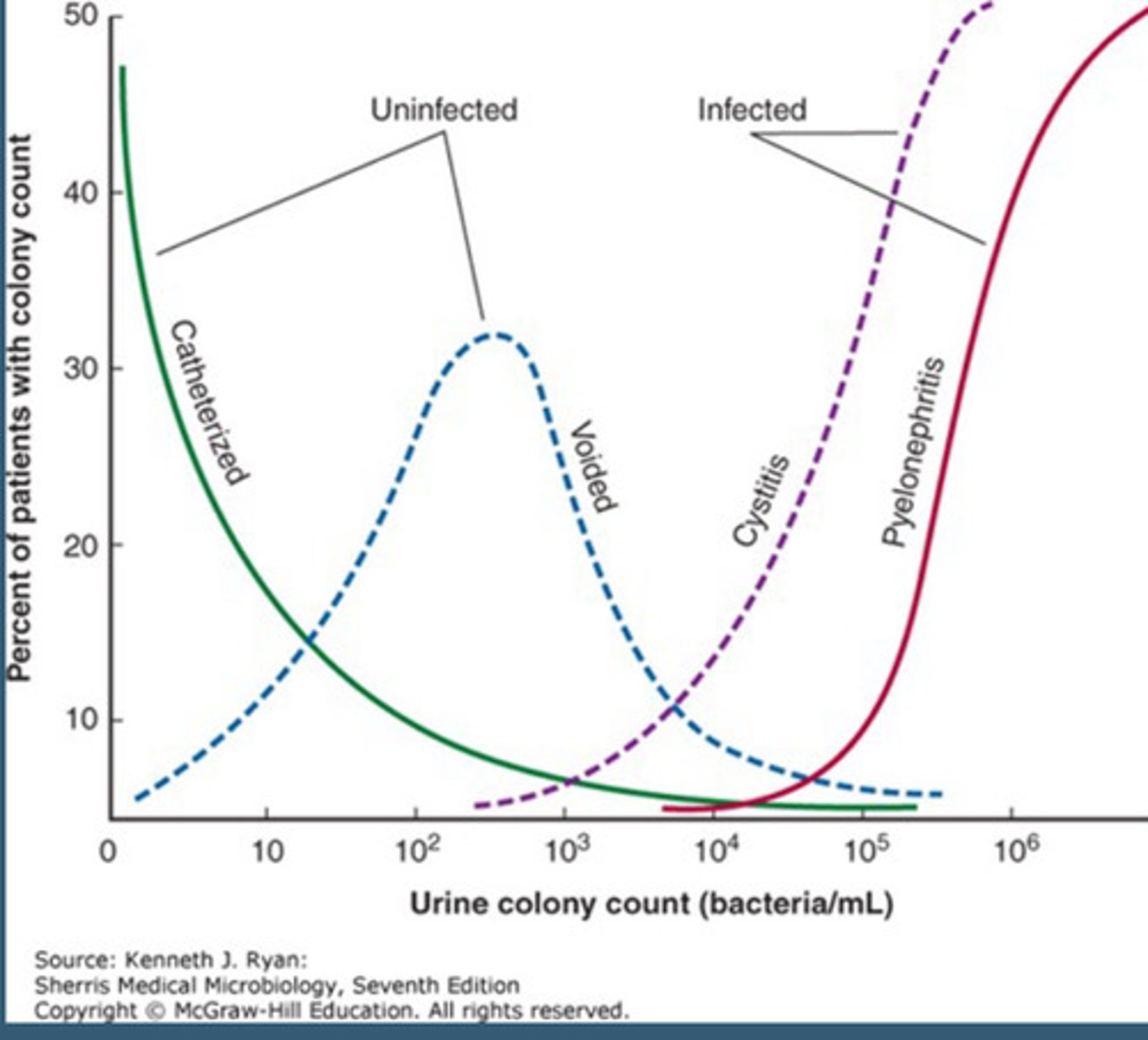
Obtaining a urine sample
Midstream "Clean Catch" Urine Acquisition
- Sterile Container
- Sterile Wipes
Catheter Acquisition
- Indwelling-Foley
- One-time Sampling
Uralysis photo
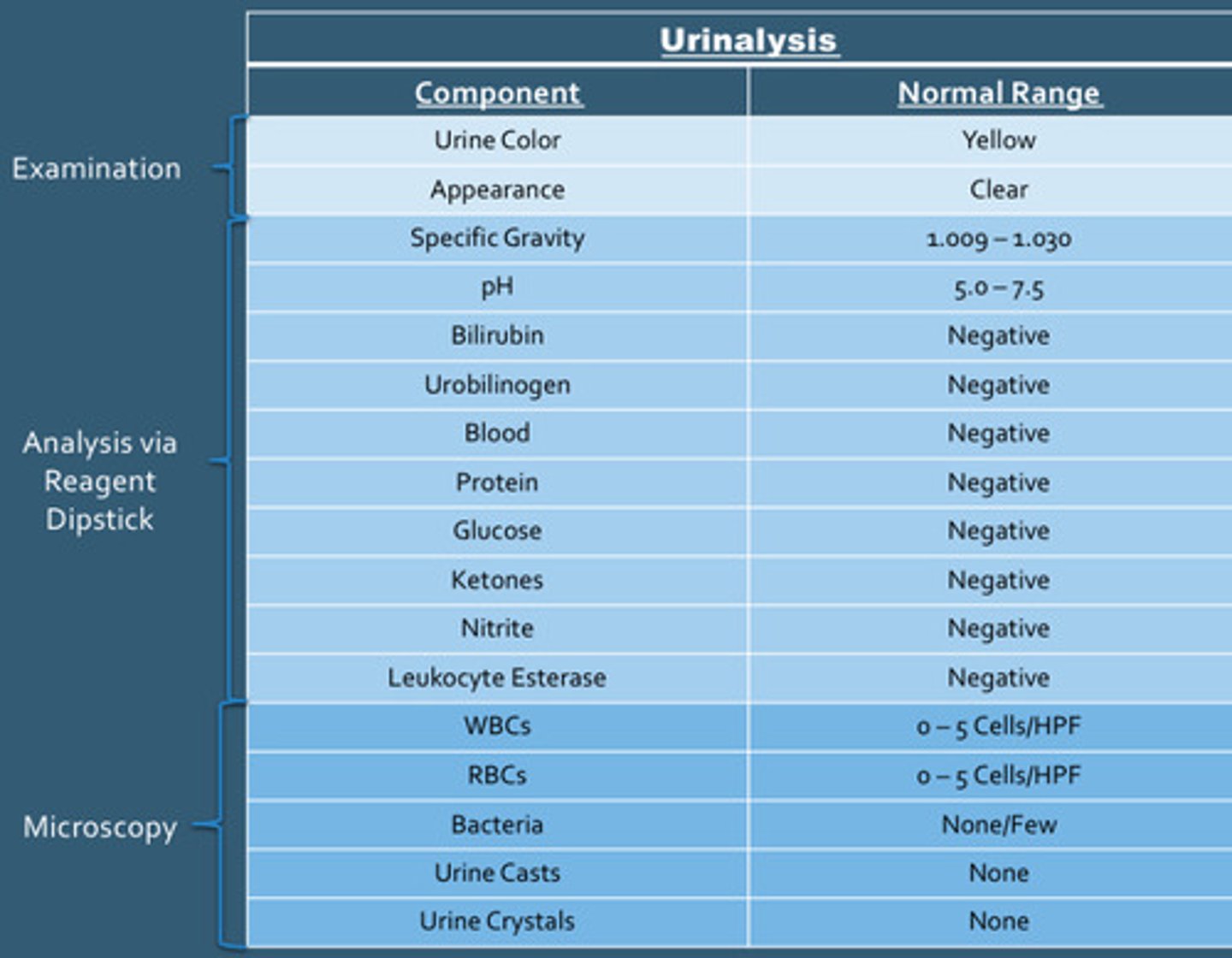
Examination urinalysis
Urine color and appearance
Analysis via reagent dipstick of urinalysis
Specific gravity, pH, bilirubin, urobilinogen, blood, protein, glucose, ketones, nitrites, leukocytes esterase
Microscopy urinalysis
WBC, RBC, Bacteria, urine casts, urine crystals
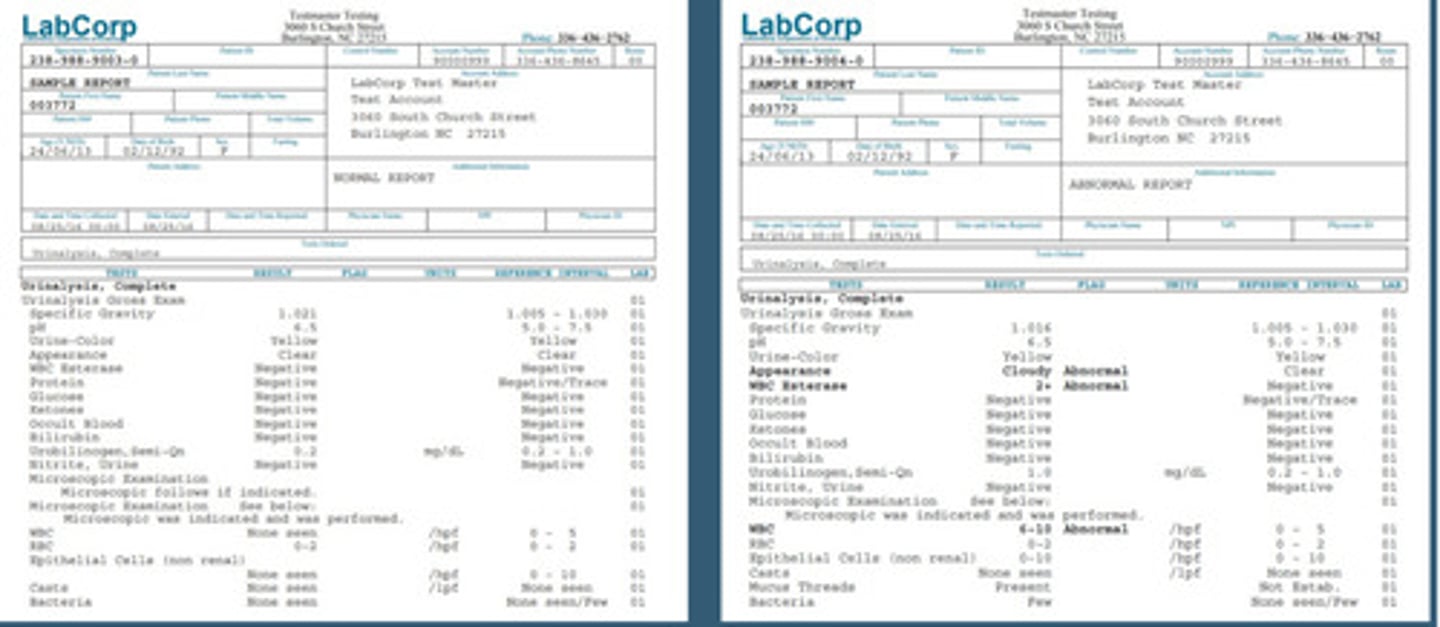
LabCorp documentation
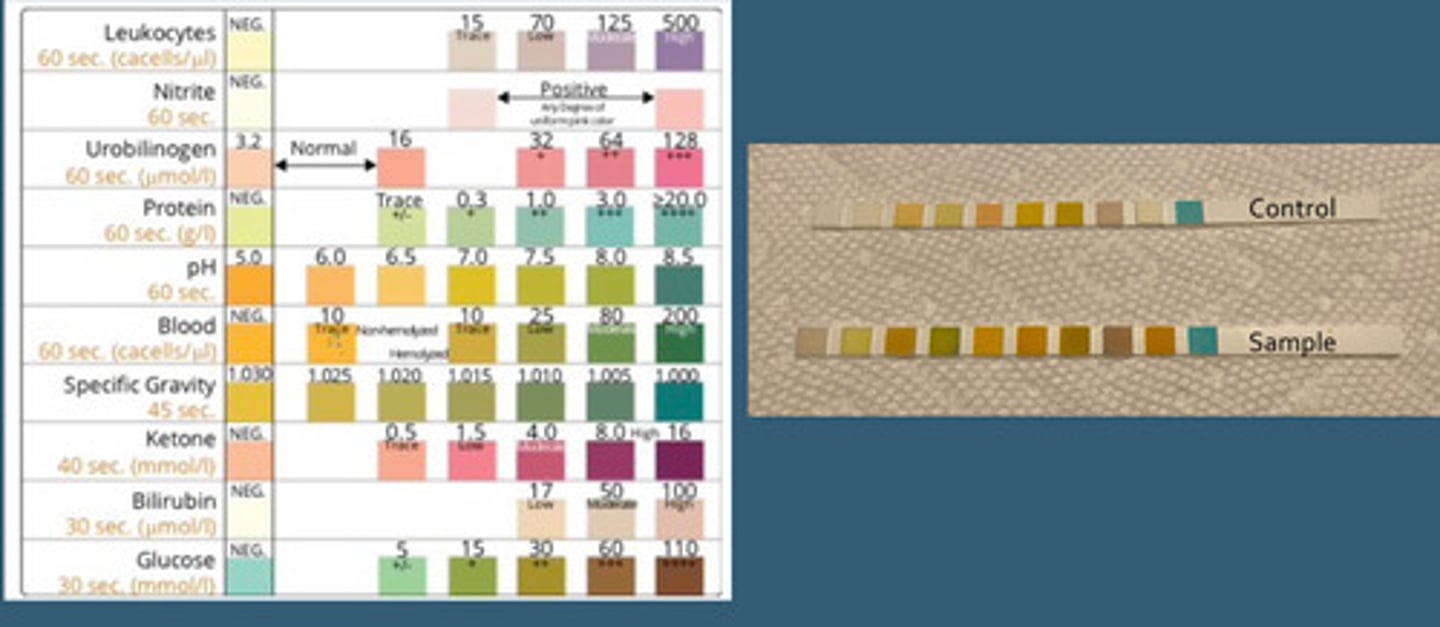
Urine dipstick photo
Yellow urine color
Pale: Volume replete, hydrated
Dark: Volume depleted, hyperbilirubinemia
Red urine color
Can centerfigue
Gross Hematuria
- Red Sediment
Hemoglobinuria
-Red Supernatant
Myoglobinuria
-Red Supernatant
Diet-Related: Beets, Rhubarb, Blackberries
Orange urine color
Medication-induced: Rifampin, Azo (Phenazopyridine for urinary pain, it is OTC)
Blue-green
P. Aeruginosa UTI
Urine appearance
Normal = clear, Cloudy = Pyuria (infection), Foam/Frothy: Proteinuria
Urine specific gravity/osmolality
Measured with dipstick, normal: 1.009-1.030
Measure of urine relative to water
Presence of urinary glucose, protein or RBCs can invalidate assessment and urine osmolality must be used (in lab)
Urine osmolality
Concentration of particles per kg of a solution
Normal: 50-1200 mOsmol/kg
Specific gravity correlation with urine osmolality
1.001 = 40 mOsmol/kg
1.030 = 1200 mOsmol/kg
Dilute urine
Will have a lower specific gravity or osmolality
Concentrated urine
Will have a higher specific gravity or osmolality
Arginine vasopressin (AVP) aka Antidiuretic hormone (ADH)
Acts on renal tubules to increase water retention. Increases concentrations of the urine
Diabetes insipidus
Their body has inadequate AVP production
- Nephrogenic: Impaired AVP Action on Kidney
Clinical Manifestations
- Polyuria, Polydipsia, Large Urine Output
- Hypernatremia
- Low Urine Specific Gravity
Syndrome of inappropriate antidiuretic hormone (SIADH)
Excessive production of AVP
- Neoplasms, CNS disorders, medications or infections
Clinical manifestations:
- H/A, confusion, N/V, coma
- Hypoatremia
- Elevated urine specific gravity
Specific gravity can indicate...
Diabetes insipidus or SIADH
Acidotic urine
Urine pH <5
Metabolic acidosis
Alkalotic urine
Urinary pH >7
Metabolic Alkalosis
Infection with Urea Causing Organisms (Proteus spp.)
Standing Urine Samples (Delayed Analysis)
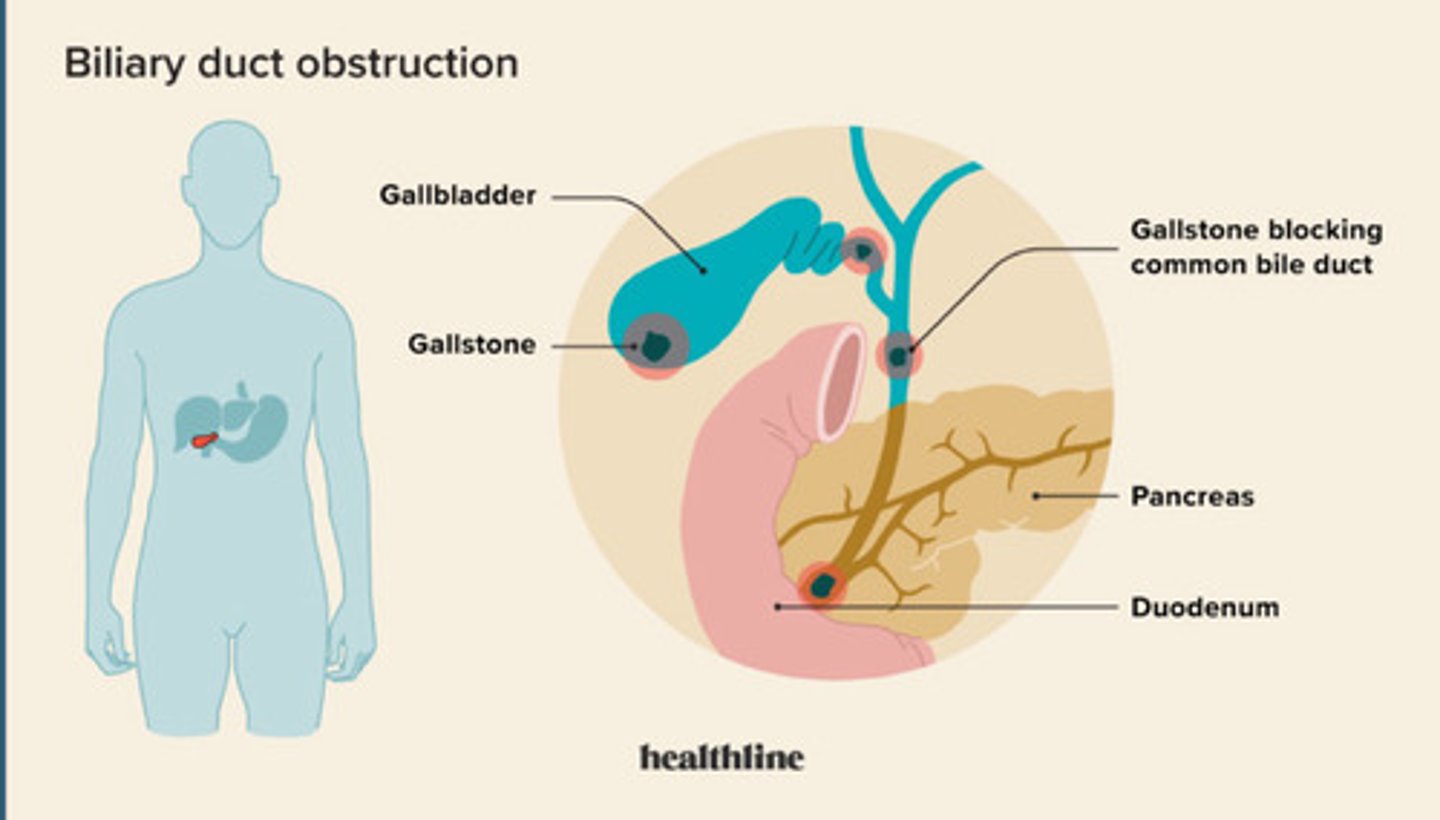
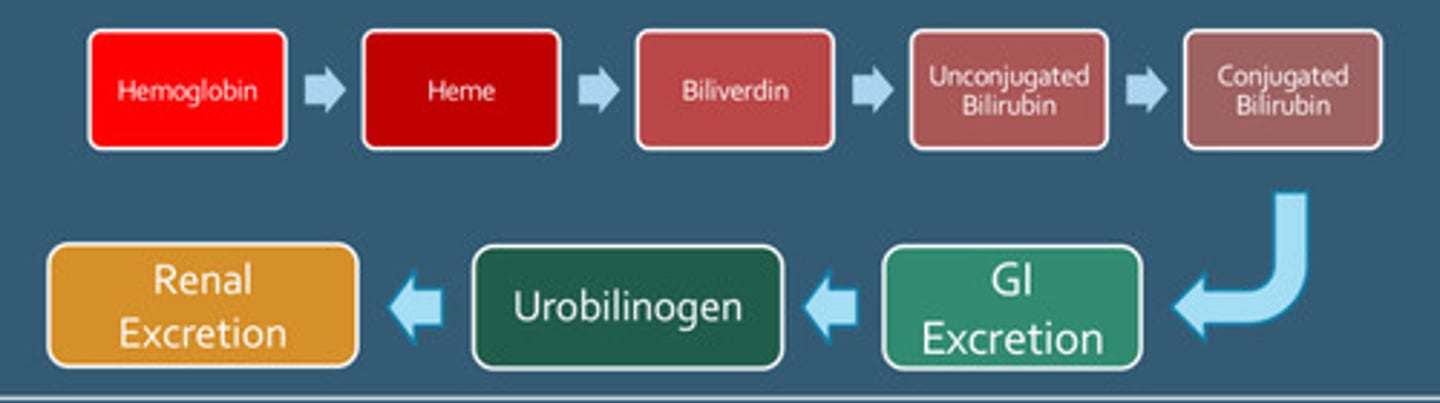
Urine bilirubin
Bilirubin is either direct (conjugated) or indirect (unconjugated).
Unconjugated bilirubin
Is bound to albumin so not filtered by the kidney
Conjugated bilirubin
Is filer but most is reabsorbed within the proximal tubules
Presence of bilirubin in urine
is always conjugated bilirubin and is typically indicative of a hepatocellular disease (liver damage)
May occur in presence of jaundice.
Urobilinogen
Conjugated Bilirubin is catabolized by Gut Bacteria and leads to the formation and absorption of urobilinogen.
Most is excreted via liver and small amounts are excreted by kidneys
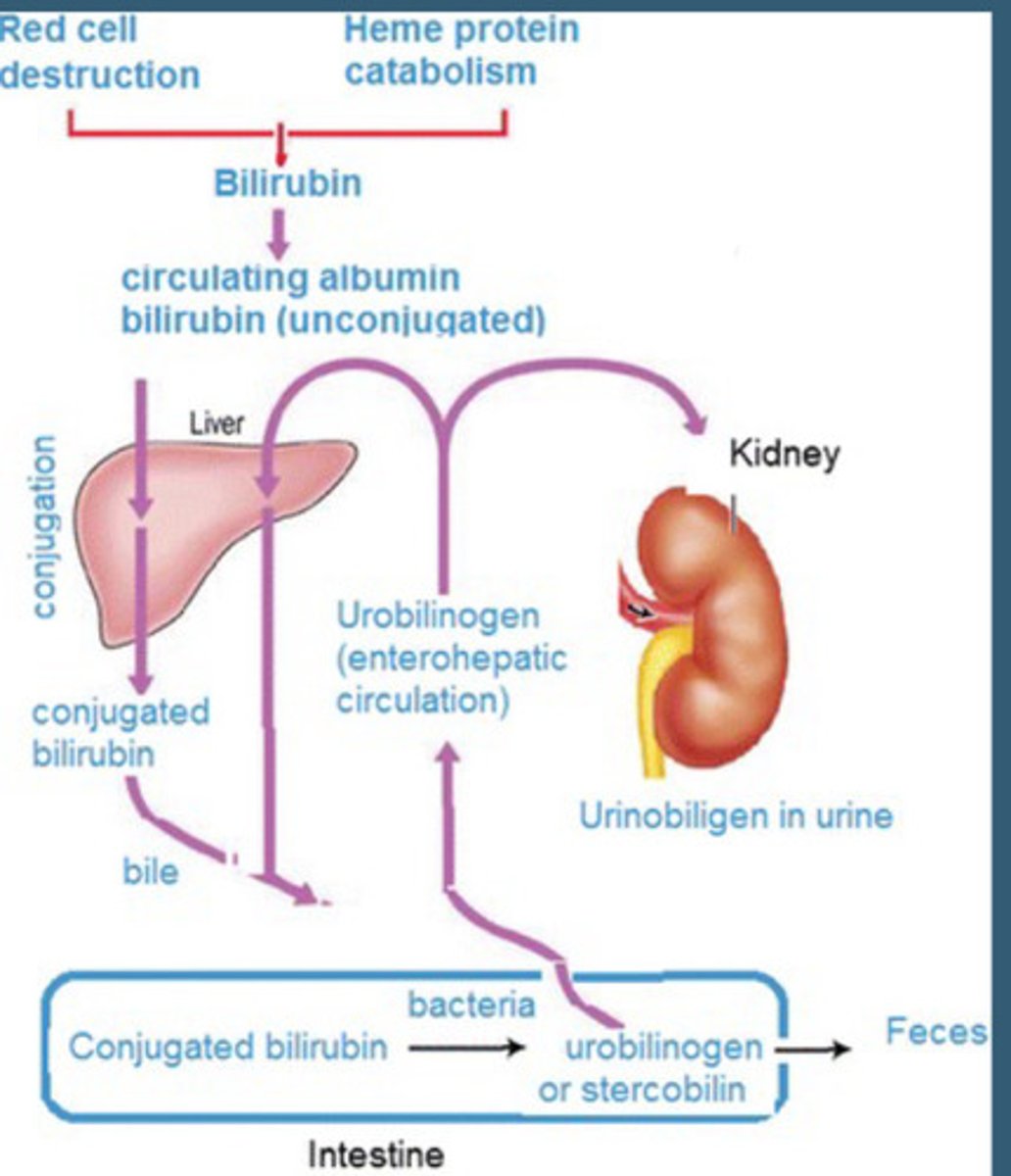
In liver failure
The liver will be unable to clear urobilinogen, leading to increased levels of urinary excretion
Urinary blood
Urine dipsticks assess for heme molecules within urine.
Positive heme means positive microscopic RBC.
Gross hematuria and microscopic hematuria will be positive.
Positive heme, negative microscopic RBC
Hemoglobinuria (hemolysis), and myoglobinuria (Rhabdomyolysis, can be from working out or drugs).
Distinguished by clinical diagnosis.
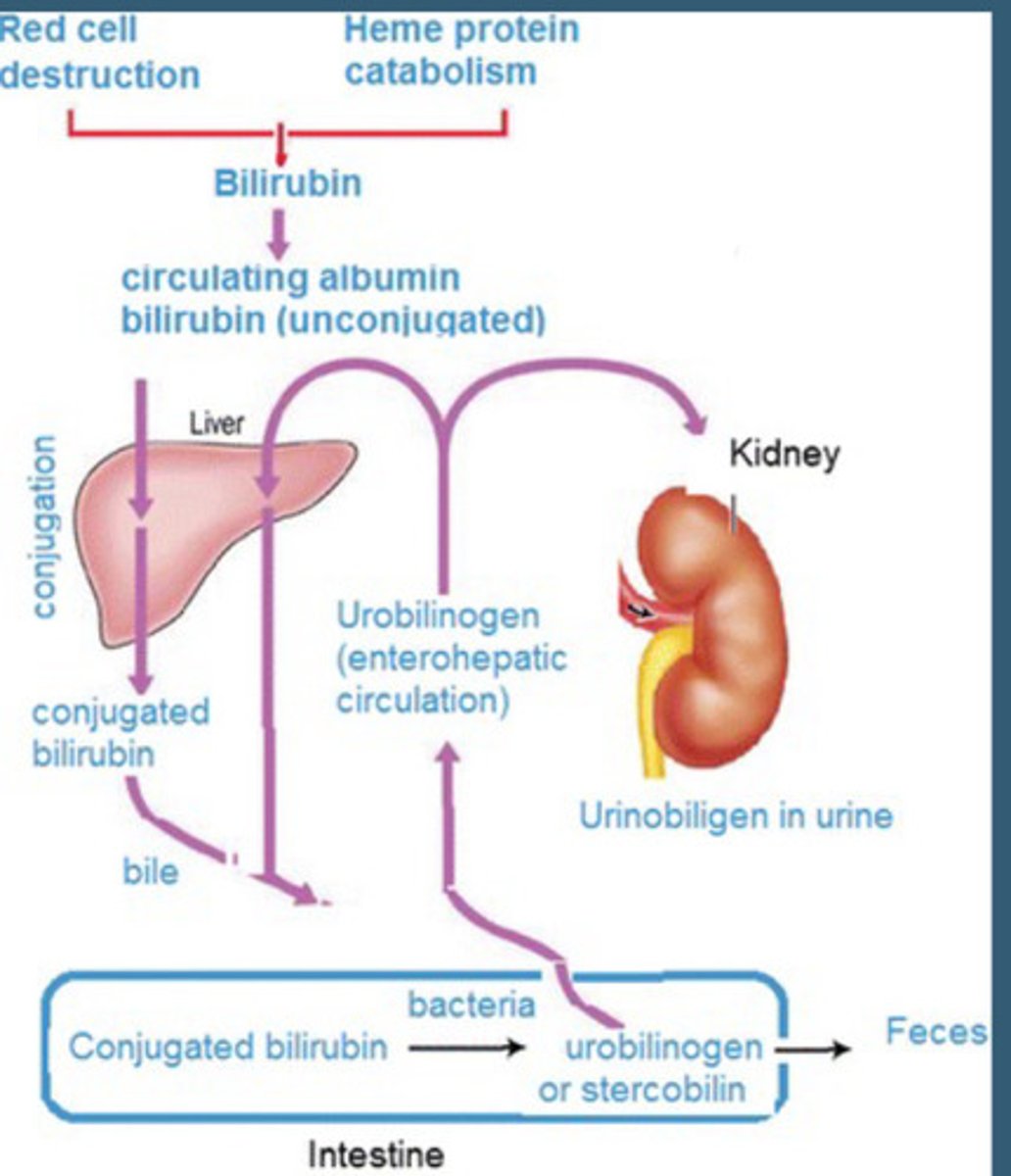
Obstructive jaundice
Urinalysis
Color: Dark yellow
Bilirubin: Positive (conjugative)
Urobilinogen: Variable depending on degree of obstruction (if completely blocked, we get none)
Blood: Negative
Hemolysis
Color: Red
Bilirubin: Negative
Urine gen: Positive
Blood: Positive
Microscopy: RBC = none (Hemoglobinuria)
Urine protein
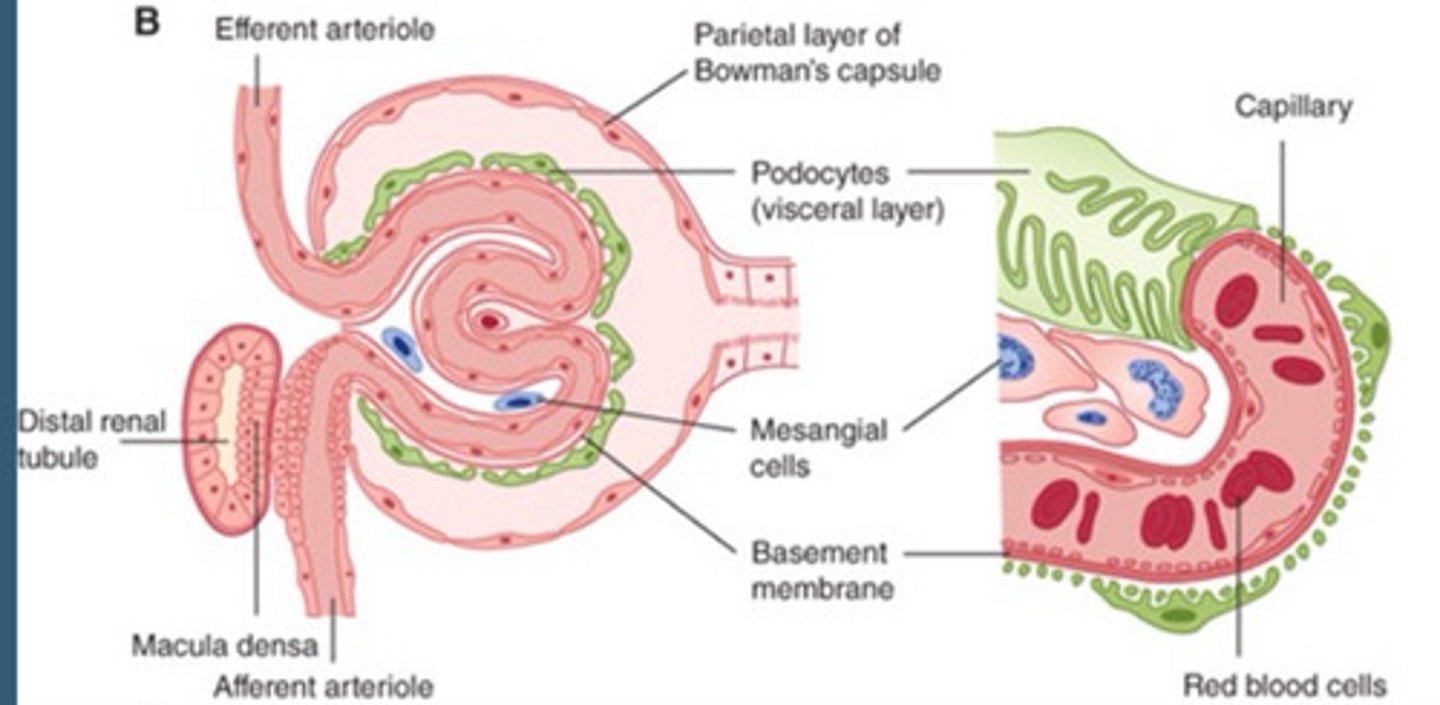
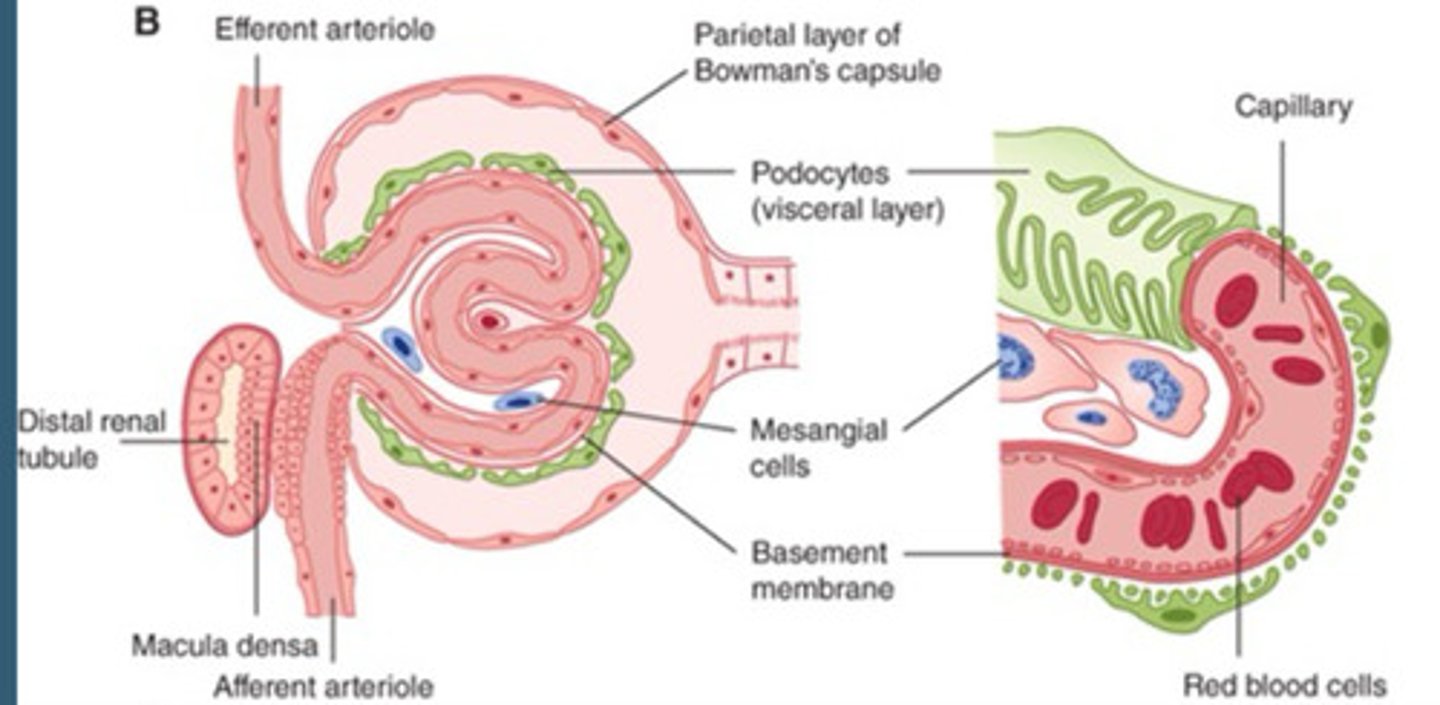
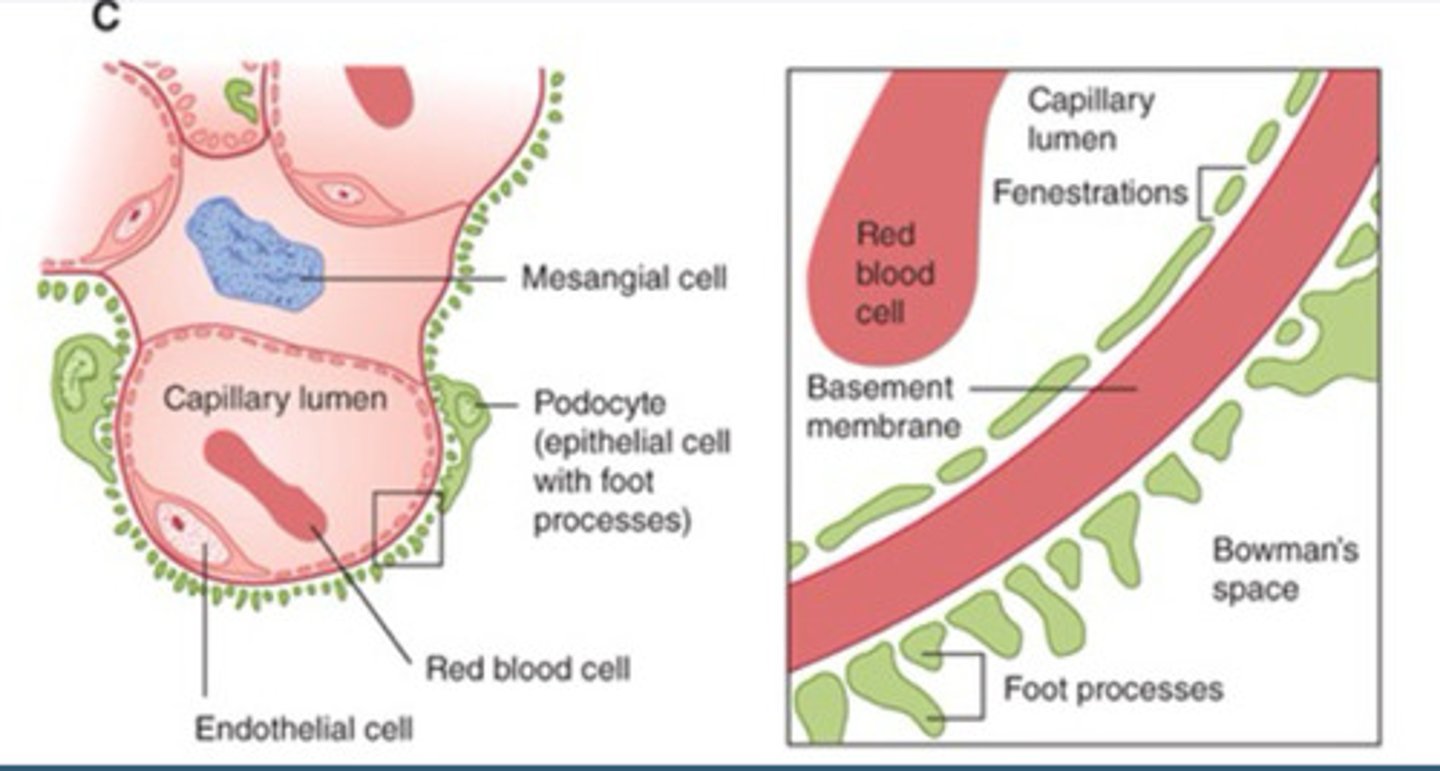
Protein molecules are too large to pass through the glomeruli and in theory urine should be absent of proteins.
Urine Dipsticks can detect albumin concentrations from 200 to 300 mg/L.
- Urine Dipsticks typically are insensitive for non-albumin proteins
- Semi-Quantitative
-Measure as Negative, 1+, 2+, 3+, 4+
-Used as a screening tool for Renal Disease
Protein in urine
Renal disease
Glucose in urine
DM
Medications like sodium-glucose co-transporters 2 (SGLT 2) inhibitors
Sodium-glucose co-transporters 2 (SGLT2) inhibitors
Increase urinary output of glucose to reduce blood sugar
Urine glucose
Glucose is continuously filtered by glomeruli and reabsorbed within the renal tubules.
Glucosuria occurs when the Renal threshold for glucose reabsorption is exceeded.
- This is typically associated with serum glucose levels > 180 mg/dL
UTIs and glucose
Increased UTIs when blood glucose is high
Urine ketones
Ketones are a byproduct of fatty acid metabolism (Lipolysis)
Theoretically, ketones should not be present in the urine.
Ketonuria
Uncontrolled DM, ketogenic diet, starvation.
Can be associated with a metabolic acidosis.
Urine nitrite
Common by-product of certain species of gram-negative nitrate metabolism.
Common agents: E. coli and other Enterobacteriaceae — includes Klebsiella spp. & Proteus spp
NOT produced by gram-positive organisms
Leukocyte esterase
An enzyme within WBCs
Will be positive in cases of infection or possibly inflammation
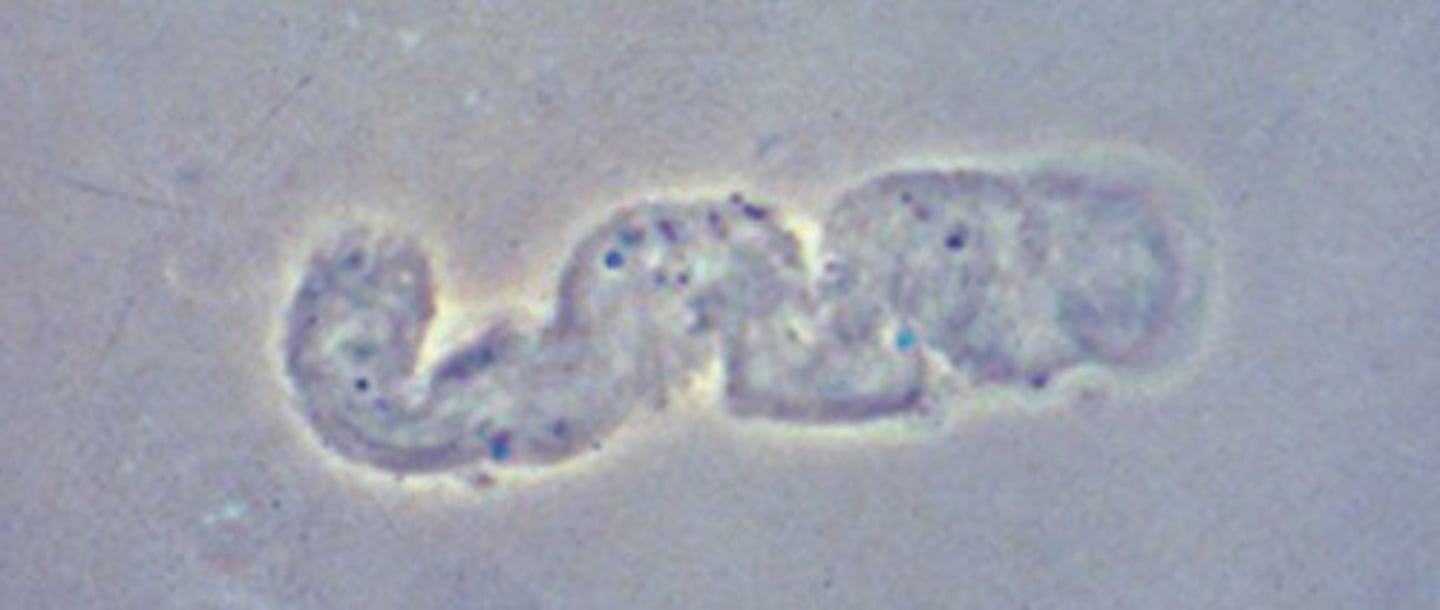
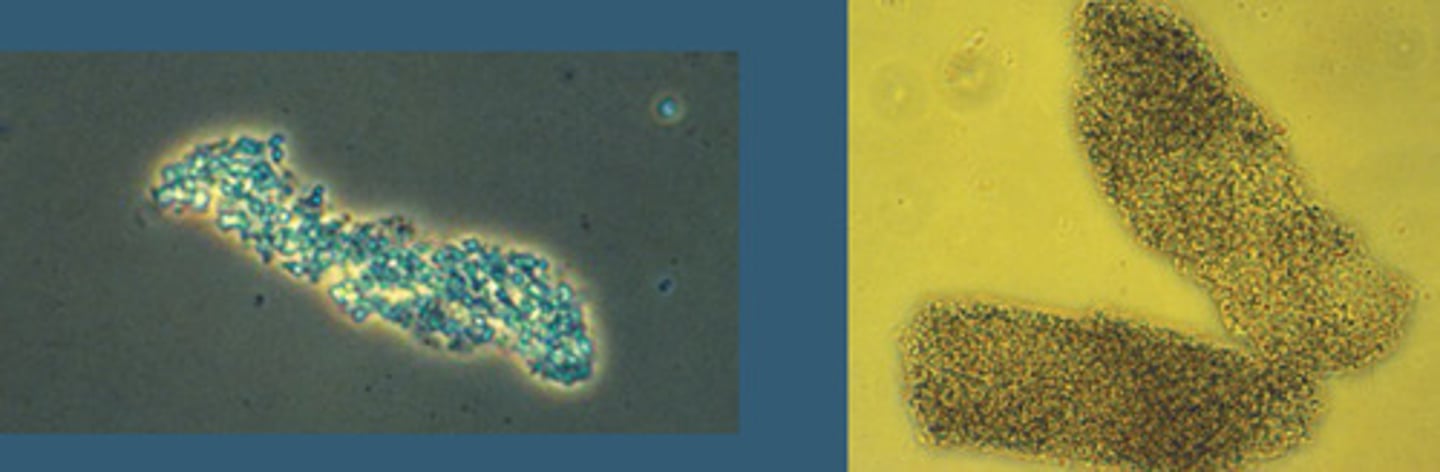
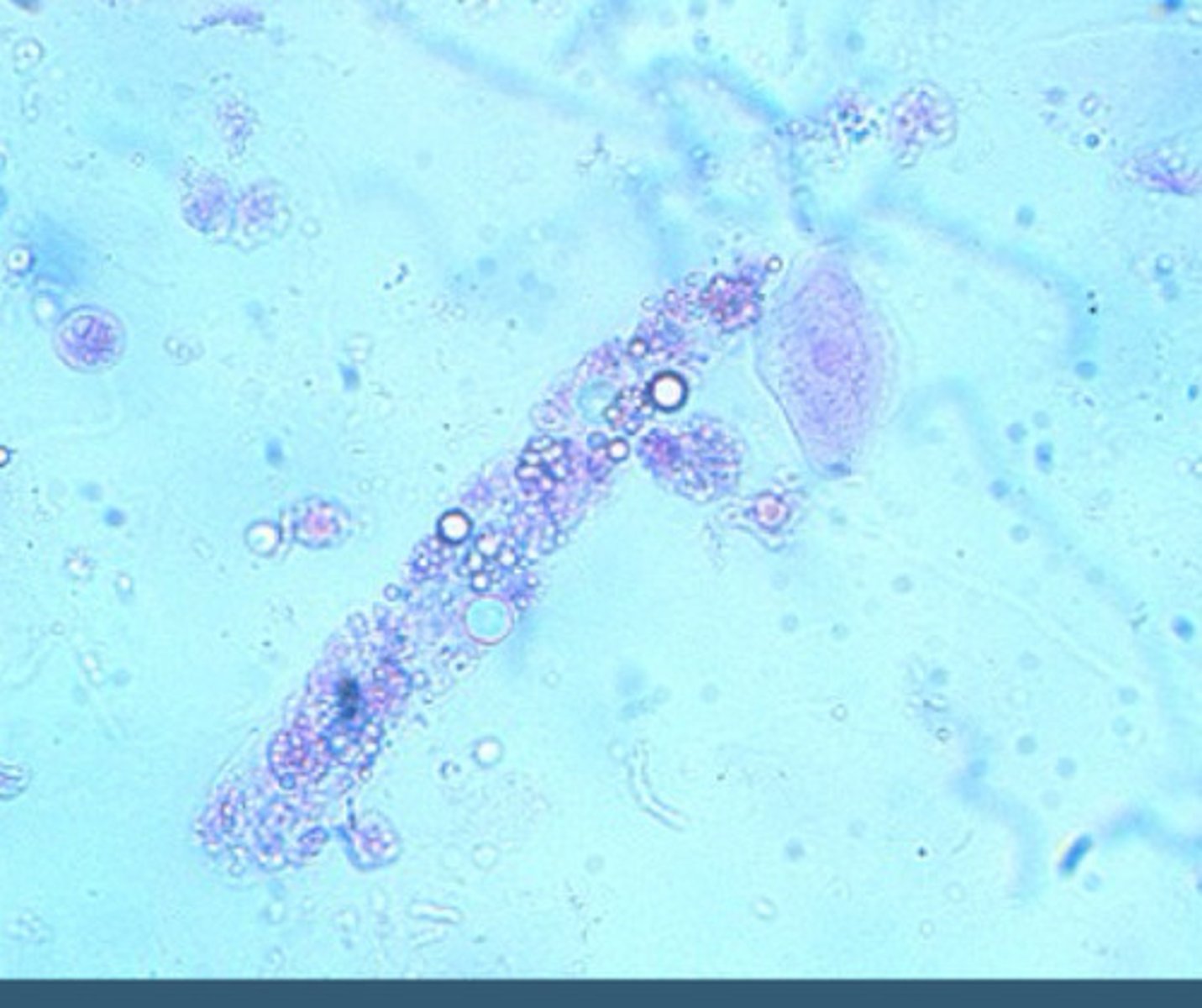
Urine microscopy
Urinary casts: Distal tubules and collecting ducts
Red/white blood cells and bacteria
Urinary crystals
Urinary casts
gelatinous structures that take the shape of the renal tubules
Acute tubular necrosis
Renal tubular damage which results in AKI
Major causes: Ischemia, nephrotoxins, sepsis
Signs/syms: AKI + Reduced urinary output
Glomerulonephritis
Inflammation of the renal glomeruli
Major causes: Autoimmune process, infection related
Signs/symps: Hematuria, AKI, edema, proteinuria, HTN
Nephrotic disease
Spectrum of glomerular disease which results in alterations of basement membrane permeability
Major causes: DM, amyloidosis
Signs/symps: Proteinuria, hypoalbumemia, edema, HLD
Hyaline casts
Faint, colorless
Concentration of mucoproteins secreted from renal tubules
Non-specific; Present in normal/non- renal disease patients
Granular casts
Broad, fine or coarse
Composed of degraded cellular products and serum proteins (Albumin, IgG, Transferrin, etc.)
Non-specific, Indicative of Renal Parenchymal Disease; ATN
Renal Tubular Epithelial Cell Casts
Collection of Renal Tubular Epithelial Cells
Associated with Acute Tubular Necrosis (ATN)

Fatty casts
Hyaline casts which contain lipid droplets and can be overserved in patients with Liguria
Associated with nephrotic syndromes
Asymptomatic microscopic hematuria
Bladder or renal cell cancer until otherwise determined.
RBC, WBC and bacteria in microscopic
Graded in cells/hpf. (Can add information to initial dipstick)
Initial Gram Staining to guide in treatment choice
Followed by subsequent Culture and Sensitivity
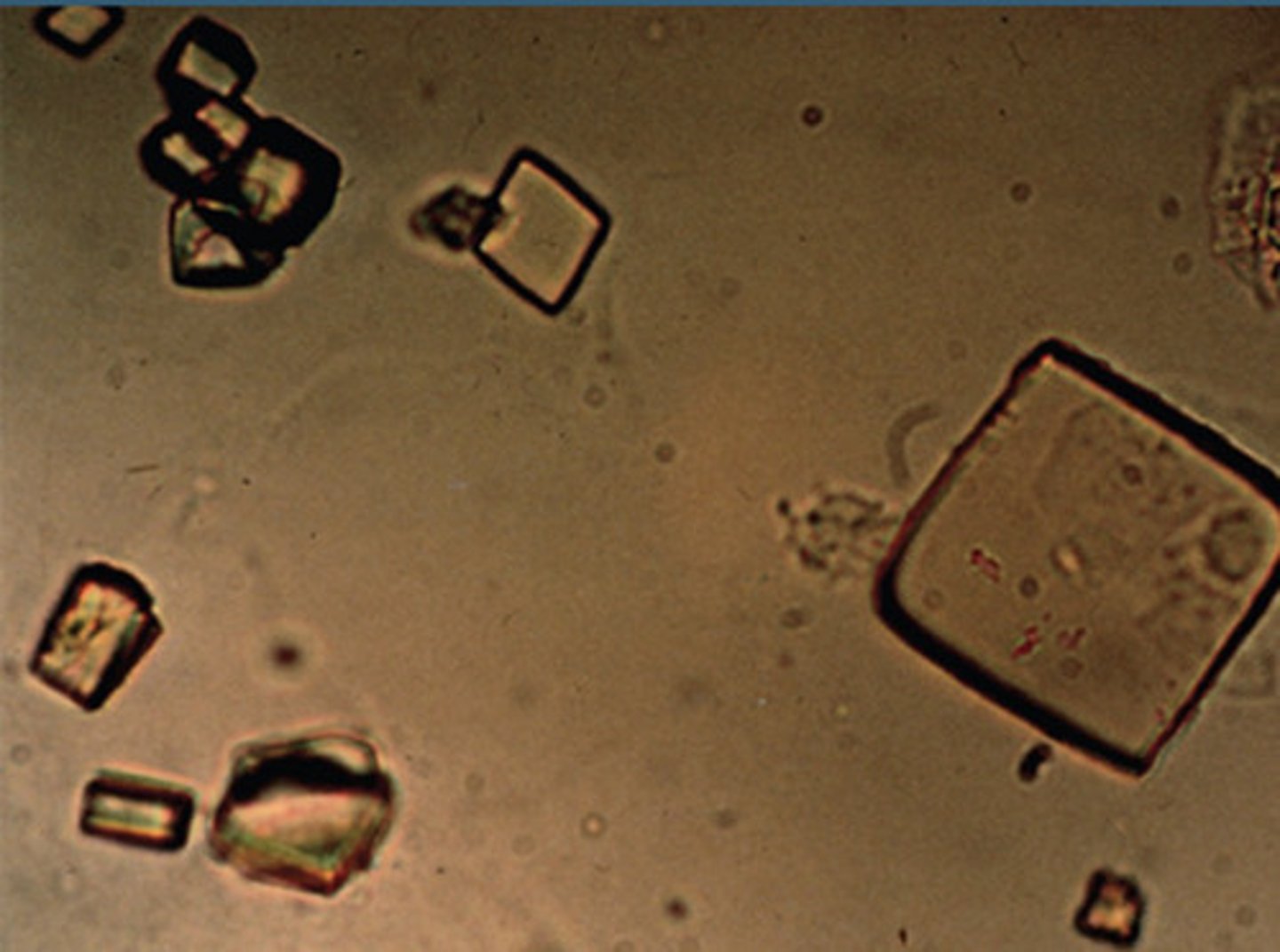
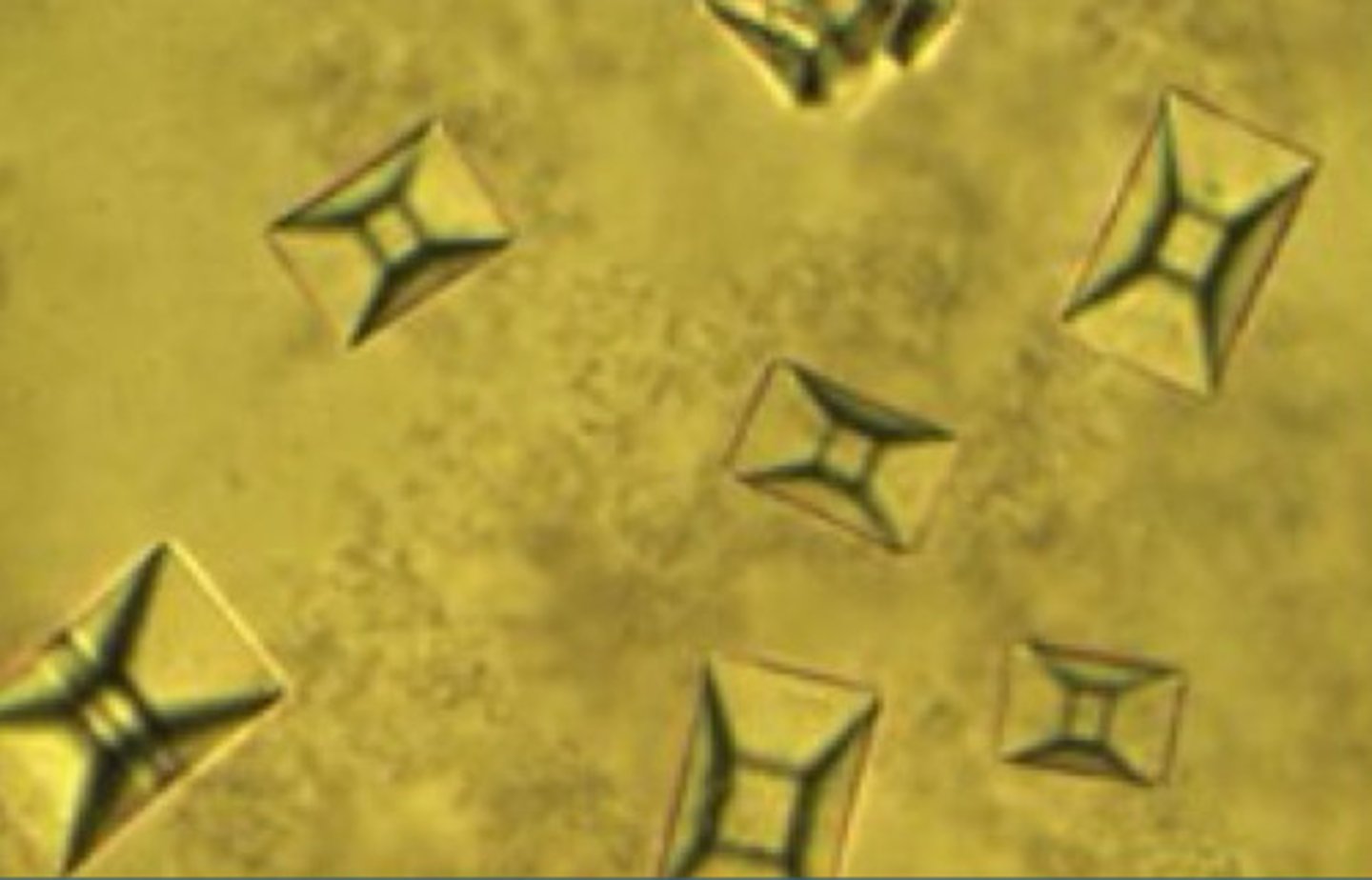
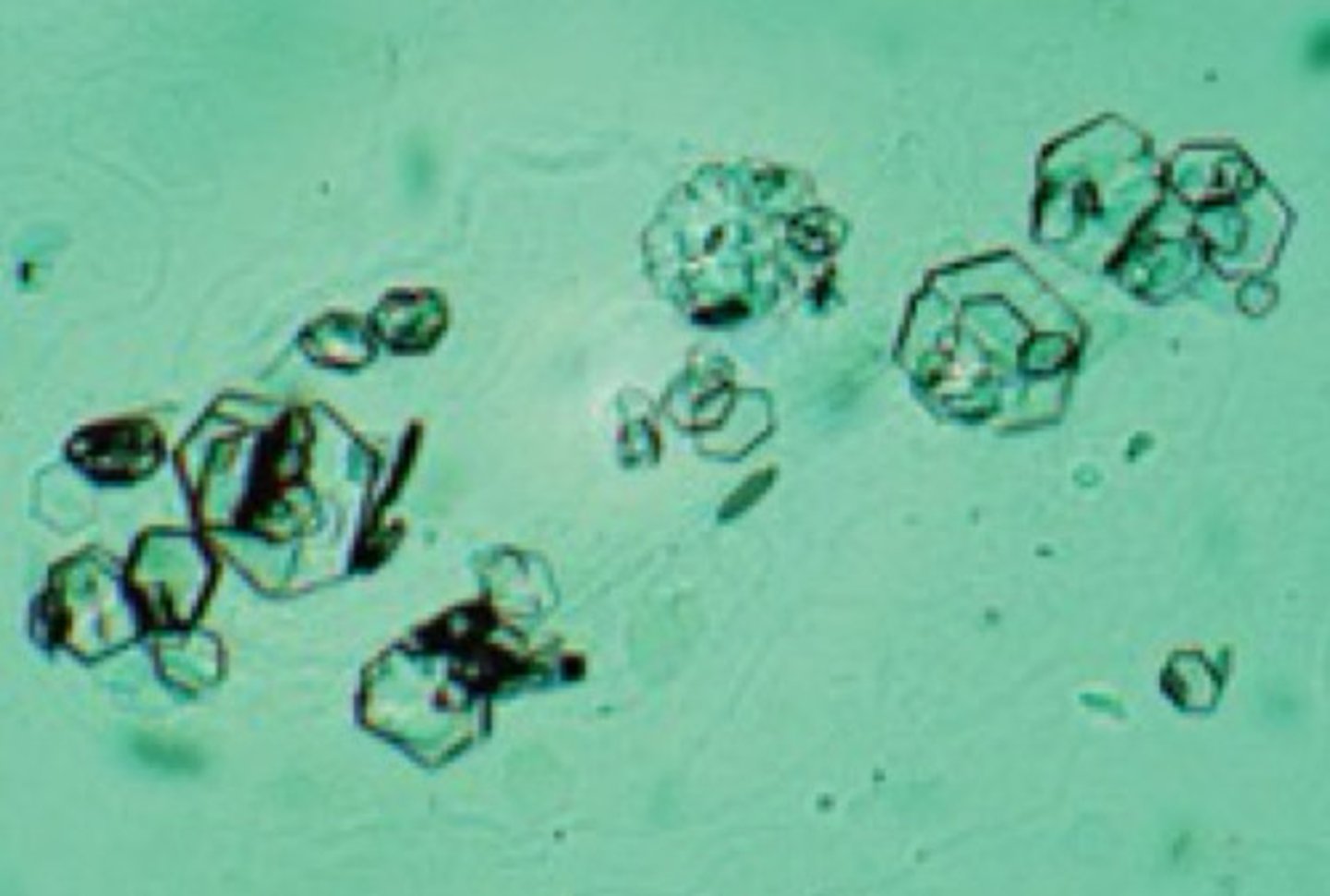
Urine stones and crystals
Calcium oxalate, uric acid, stuvite, cystine
Calcium oxalate
Small Square crystals with Central Cross
Most Common Stone Type
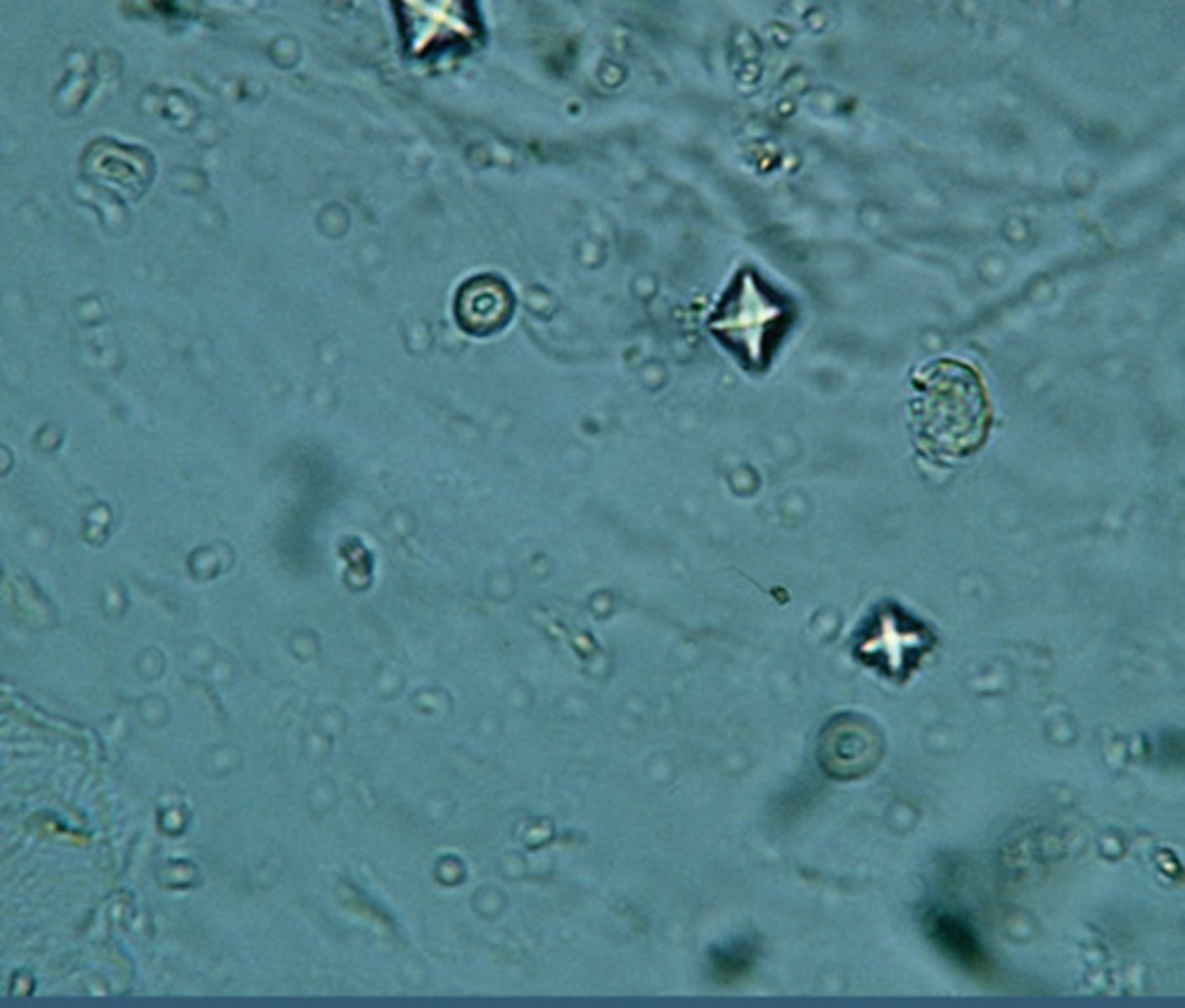
Uric acid
Rhomboids, Hexagons, or Squares
Acidic Urine (Gout)
Struviate (staghorn)
Triple phosphate
"Coffin-lids"
Alkaline urine
Drystone
Colorless hexagons, seen in patients with cystinuria
Red blood cell casts
Collection of grouped red blood cells which have leaked into the renal tubules through damage of the glomerular basement membranes.
Occurs in glomerulonephritis

24 hour urine collection procedure
Procedure
1. First Urine is voided and discarded.
a. The time is recorded. This is the beginning of the 24 hour urine study
2. Each subsequent urine is collected in a container
3. Urinate one last time at the end of the 24 hour period.
a. This is the end of the 24 hour urine collection
4. Urine is then analyzed for various electrolytes, proteins, catecholamines, etc.
Keep in fridge
White blood cell casts
Collection of white blood cells which have leaked into the renal tubules.
Typically occur in upper urinary tract infections (pyelonephritis)
Pathologies for 24 hr urine collection
Calcium
- Increased: Hyperparathyroidism, Sarcoidosis, Hyperthyroidism
- Decreased: Hypothyroidism, Renal Failure
Catecholamines
- Increased: Pheochromocytoma
Free Cortisol
- Increased: Cushing Syndrome (Screening Test of Choice)
Creatinine
- Decreased: Renal Disease (Used to help calculated Creatinine Clearance in conjunction with Serum Creatinine)
Protein
- Nephrotic Syndromes, Preeclampsia
Urine microalbumin
Used as a screening tool for diabetic patients to determine their risk of developing nephropathy. Dipsticks don't normally pick this up until it is in macro levels, so we typically send it out to a lab for this specific test if necessary.
Often used for diabetics
Urine Microalbumin levels
Normoalbuminuria
< 30 mcg/g Cr (Spot Urine)
< 30 mg/24 Hr
Microalbuminuria
30 - 299 mcg/g Cr (Spot Urine)
30 - 299 mg/24 Hr
Macroalbuminuria
> 300 mcg/g Cr (Spot Urine)
> 300 mg/24 Hr
Spot urine microalbumin often used for
Diabetes monitoring
Those diagnosed with microalbumin uric are given...
ACE inhibitor or ARB therapy
Urine spot testing
Can be used for various electrolyte abnormalities and metabolic states.