mod 1 slide 1 (intro & hematopoiesis)
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
innate immune system
rapid response (hours)
non-specific response to foreign molecules
response fixed (non adaptive)
no immunological memory
adaptive immune system
delayed response (days)
highly specific response to antigen
response adaptive (changes over time)
immunological memory
innate immunity — first line defenses
defense against pathogens is mediated by the ____ reactions of innate immunity and the ____ responses of adaptive immunity
cellular and biochemical defense mechanisms are in place even ____ infection and is poised to respond rapidly to infections
______, _______, _______
early; late
before
mechanical, chemical, microbiological
______ _____ refers to the ability of the immune system to respond more rapidly and effectively to a pathogen that has been encountered previously
innate or adaptive?
immunological memory
adaptive
hematopoiesis
all immune cells are derived from what?
involves differentiation, proliferation, and maturation of cells from which pathways?
involves _____ of a small population of stem cells
involves cytokines (interleukins, growth factors), and other chemical mediators — what does this do?
bone marrow
myeloid and lymphoid pathways
self-renewal
it drives cloning-expansion to cell lineages
immune cell communication and cytokines
there are 3 modes of cytokine-mediated-cell-to-cell communication — what are they?
cells communicate through the exchange of ____ ____ in one of 3 modes
autocrine (same cell)
paracrine (cell to cell — nearby)
endocrine (cell to cell — distant)
secreted cytokines
what is the most obvious cell derived from bone marrow?
___ ____ cell type — transport of oxygen via hemoglobin
RBCs are a ____ resource with a _____ lifespan of about 120 days, and have an intracellular content of about ___ hemoglobin
RBCs are ____ ___ cells that have ____ ____ ____ including nuclei, ribosomes, mitochondria, and most intracellular machineries during their maturation process
erythrocytes
most abundant
renewable; limited; 95%
terminally differentiated; lost all organelles
ABO blood groups and antigens
what describes surface glycoproteins on RBCs?
example: if you are B blood type, you have B-antigens on RBC and circulating antibodies against A-antigens
if a B recipient is given A type donor blood, an antibody response is mounted against the A blood — incompatible — ______
antigens
agglutination

__ ____ = universal donor
__ ____ = universal recipient
O-
AB+
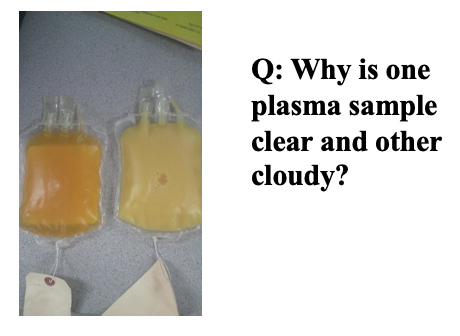
what you eat displays in your plasma
erythrocytes (RBCs) and erythropoietin (EPO)
_____ is a glycoprotein hormone that regulates the daily production of 200 billion new RBCs in the human body
EPO binding to ____ ___ cells promotes their survival, proliferation, and differentiation to mature eryhtrocytes
EPO production is ____ ___ and is made in the interstitial cells in the ___ ___ in response to anemia, ischemic stress or high altitude
EPO has ____ function in bone marrow
erythropoietin (EPO)
erythroid progenitor
hypoxia inducible; adult kidney
endocrine
anemia management in chronic kidney disease (CKD)
in CKD, anemia is caused by low erythropoietic activity, consistent with ____ ____ __ ____ in the kidneys, leading to inflammation and increased ____ levels — which block ____ ___ ____ and macrophage iron recycling, causing iron restricted erythropoiesis and anemia
insufficient production of EPO
hepsidin
intestinal iron absorption
erythropoietin stimulating agents (ESA)
ESA’s are indicated for… (5)
anemia associated with…
HI infection
chemotherapy
renal failure
CKD
iron deficiency
erythropoietin stimulating agents (ESA)
ESA use found to… (3)
significantly raise Hb levels
reduce the need for blood transfusions
improve hematocrit levels
production, regulation, and utilization of growth factors
what 2 things represent the current standard of care in patients with anemia in CKD?
note: the development of RBCs from bone marrow also requie ____ and ____ ___
current guidelines support partial treatment of anemia in patients with CKD when Hb level is <___ g/dL
ESAs
adjuvant IV iron supplementation
folate; vitamin B12
10
ESAs and adverse events
using ESAs to target a hemoglobin level of greater than 11 g/dL increases the risk of what?
the latest product labeling no longer specifies a target Hb level, bute use of what?
serious adverse cardiovascular events and has not been shown to provide additional patient benefit
lowest ESA dose sufficient to reduce the need for transfusions
mircera
methoxy polyethylene glycol-epoetin beta
Continuous Erythropoietin Receptor Activator
how is the half life?
what does PEG modification do to the stability of protein?
how is the dosing?
long half life
enhances
once a month (SC injection)
* anything with PEG = long acting drug and better than predessecor
the short life and quick death of peginesatide (OMONTYS) RIP
peginesatide is a synthetic peptide-based ESA which was FDA approved in March 2012 for the treatment of ____ in patients with chronic kidney disease
oncologic drug advisory committee (ODAC) voted 15-1 that peginesatide demonstrated favorable benefit/risk profile
Feb. 23, 2013: affymax and takeda pharm voluntarily recall OMONTYS injection due to what?
to date, fatal reaction reported in 0.02% of patients (25,000 patients)
anemia
new post-marketing reports of severe hypersensitivity reactions, including anaphylaxis, which can be life-threatening or fatal
daprodustat
in patients undergoing dialysis, daprodustat was noninferior to ____-____ agents in both hemoglobin levels and MACE
erythropoiesis-stimulating
2 years ago — FDA approval of JESDUVROQ (daprodustat)
FDA approved GSK’s anemia frug jesduvroq for kidney disease patients on dialysis
daprodustat: first-in-class ___ hypoxia-inducible factor prolyl hydroxylase inhibitor (HIF-PHI), for the once-a-day treatment of anemia due to chronic kidney disease (CKD) in adults who have been receiving dialysis for at least 4 months
what is the boxed warning?
what are the contraindications?
oral
same boxed warnings as ESAs
strong CYP2C8 inhibitors (such as gemfibrozil)
daprodustat: MOA
daprodustat is a hypoxia-inducible factor (HIF2α) prolyl hydroxyase 2 (PHD2) inhibitor
HIFs are transcription factors that function as master regulators of what?
prolyl hydroxylase is enzyme that catalyzes hydroxylation of ___ residue on HIF2α
oxygen homeostasis
proline
daprodustat: MOA
PHD2 is ____ due to lack of oxygen (hypoxia) or in the presence of an inhibitor (top) in these cases, HIF2α is _____ and can ____ ____ ___ ___
when PDH2 is ____ (bottom) due to sifficient oxygen (normoxic), HIF2α is ____, and consequently recognized by the ____ __ ___, resulting in ____ of HIF2α
ubiquitylated HIF2α is then destroyed by the proteasome is then destroyed by the proteasome
no HIF2α = no ____ produced
inactive; functional; induce expression of EPO
active; hydroxylated; ubiquitin E3 ligase; ubiquitylation
EPO
daprodustat: MOA
hypoxia — or inhibition - HIF is ____
normoxia - HIP is ____
stabilized
degraded
neutrophils
_____ subpopulation of WBC (65-60% of total WBC count)
14 days to mature from stem cell in bone marrow
_____ — capture and digest bacteria
_____ (decrease neutrophil count), result of chemotherapy, severe infection and sepsis
treatment of decrease neutrophil count is accomplished by using what?
neutrophils classified as ____ or ____ — depending on maturity
largest
phagocytes
neutropenia
therapeutic growth factor
band or segmented
chemotherapy - induced neutropenia
_____ ____ (oncology) target rapidly proliferating cells which include normal hematopoietic cels (bone marrow)
neutrophils are _____ produced by the bone marrow
therefore, use of cytotoxic drugs may lead to what?
dose-limiting aderse event
chemotherapeutic agents
continuously
neutropenia
how is neutropenia diagnosed?
neutrophils are measured in terms of an “____ ____ ___“
contain both band (_____) and segmented (____) neutrophils
what is the calculation?
“absolute neutrophil count“ (ANC)
immature; mature
total WBC % x total neutrophils (immature and mature)
how is neutropenia diagnosed?
grade 0 = _____
grade 4 = ____ ____
febrile neutropenia = neutropenia + fever > 101 = emergency
normal
severe neutropenia
rG-CSF (recombinant granulocyte colony stimulating factor)
recombinant G-CSF acts to ____ neutrophil proliferation and function while ____ the incidence and severity of neutropenia
accelerate
decreasing
rG-CSF (recombinant granulocyte colony stimulating factor)
what does G-CSF target?
what are the biologic effects of G-CSF? (3)
selectively targets neutrophil precursor cells
stimulates proliferation (replication) of neutrophil precursors
enhances differentiation and maturation of neutrophil precursors
activation and enhancement of mature neutrophils
NEUPOGEN
generic name: Fligrastim
description: a human recombinant granulocyte colony-stimulating factor (G-CSF)
indications: cancer patients receiving myelosuppressive chemotherapy or bone marrow transplant; patients with myeloid leukemia; patients with severe neutropenia
informational slide
NEULASTA
generic name: Pegilgrastim
description: a covalently linked analog of recombinant G-CSF (filgrastim) and monoethoxypolyethylene glycol (PEG); longer half life
indications: identical to Neupogen
informational slide
chemotherapy-induced neutropenia (CIN)
CIN is a major dose-limiting toxicity of systemic cancer chemotherapy — what does it do? (4)
____ _____ (FN) — oncologic emergency
fever 101ºF or greater + neutropenia
often requires hospitalization and broad-spectrum antibiotic use
associated with substantial morbidity, mortality, and cost
increases risk of infection
prompts dose delays/reductions
impacts effectiveness
impairs quality of life
febrile neutropenia
occurrence of neutropenic events
historically, CIN has been considered a ____ ____, with risk increasing over multiple chemotherapy cycles
recent data in different tumor types have shown that the greatest risk for CIN is in the ____ ____
cumulative toxicity
first cycle
in patients with breast cancer, most (67%) FN events in the initial placebo group occurred in the first chemotherapy cycle
in patients with non-hodgkin’s lymphoma, 50% of FN events occurred in the first chemotherapy cycle
what is the prevention of FN? (4)
dose reduction of chemo agents
different chemotherapy regimen
antibiotic prophylaxis
prophylactic colony-stimulating factors (CSFs)
Filgratim (Neupogen)
Pegfilgrastim (Neulasta)
colony-stimulating factors (CSF)
_____, _____
↓ incidence of FN by 50%
↓ FN-related hospitalizations and IV anti-infective use
↓ infection-related and all-cause mortality
↑ delivery of planned chemotherapy dose
dosing
_____ — 5 mcg/kg subcutaneously daily x 7-10 days, begin 24-72 hr AFTER chemotherapy
_____ — 6 mg (fixed) subcutaneously x 1 dose, given 24-72 hr AFTER chemotherapy
Fligrastim, Pegfilgrastim
Filgrastim
Pegfilgrastim
use of antibiotics
current guidelines recommend antimicrobial prophylaxis with fluoroquinolones in patients at high risk for infection-related ____ and ____, but this practice provides a ___-___ benefit to individual patients
while fluoroquinolone prophylaxis has reduced some of the collateral damage of intensive chemotherapy, the direct and indirect adverse effect of these agents may ____ ____ ____
morbidity and mortality; short-term
limit their utility
eosinophils
make up 1-3% of total WBC
mature in ____ ____ for 1-3 days, remain in ____ for minutes, enter ____
production and activity regulated by: IL-3, IL-4, ____
eosinophils kill pathogens by doing what?
eosinophils (increased) associated with allergic reactions, asthma, dermatitis, inflammatory GI disorders
high concentrations in ____ infections
bone marrow; blood; tissue
IL-5
releasing toxic granules
parasitic
eosinophils
eosinophils activation mediated by ___ __ ___
____ plays a critical role. in eosinophil differentiation, maturation, recruitment, and activation in tissues
IL-5 is ____ ____ to eosinophils and has been an important therapeutic target
other cytokines can also be ____ to mitigate negative eosinophil effector functions
helper T-cells
IL-5
extremely specific
blocked
eosinophils and asthma
interleukin-5 (IL-5) exerts selective action on eosinophils, which, in turn, do what?
interleukin-5 blockers are clinically used and indicated for ___ ____ treatment of patients with sever asthma with an _____ phenotype
IL-5 blockers reduce asthma exacerbations, improve health-related quality of life, and lung infection
these treatments roughly ____ the rate of asthma exacerbations in this population
sustain airway inflammation and worsen asthma symptoms and control
add-on maintenance; eosinophilic
halve
Mepolizumab (NUCALA)
some patients with severe asthma have frequent exacerbations associated with persistent eosinophilic inflammation despite continuous treatment with ___-___ ___ ____
Mepolizumab, a ____ _____ antibody (not fully human) against interleukin-5 (IL-5) (anti-IL-5 MAb), selectively inhibits eosinophilic airway inflammation and induces a significant reduction in sever asthma exacerbations, regardless of IgE levels in blood
indicated as ____ ____ treatment of patients with severe asthma aged 6 yrs and older, and with an eosinophilic phenotype
patients should do what with their current therapy? — which usually includes inhaled corticosteroids
high-dose inhaled glucocorticoids
humanized monoclonal
add-on maintenance
should NOT STOP their current therapy
EOHILIA (budesonide oral suspension) for eosinophilic esophagitis (EoE)
what is EoE?
eosinophilic esophagus — chronic inflammatory disease in the esophagus — can cause dysphagia, regurgitations, stuck food, and chest pain
EOHILIA (budesonide oral suspension) for eosinophilic esophagitis (EoE)
is budesonide first-in-class?
is it approved for other indications?
first in class
approved for EoE only
EOHILIA (budesonide oral suspension) for eosinophilic esophagitis (EoE)
how long should patients with EoE take this?
how do they take it?
12 wks
oral suspension
EOHILIA (budesonide oral suspension) for eosinophilic esophagitis (EoE)
do you take it with food or water?
no food or water 30 mins before or after
EOHILIA (budesonide oral suspension) for eosinophilic esophagitis (EoE)
the term “thixotropic“ is used when describing EOHILIA formulation — why is this important for this particular indication?
flows more freely when shaken (lower viscosity) before administration — becomes more viscous when swallowed (able to coat the esophagus and reduce inflammation)