Contemporary issues in medical science
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
94 Terms
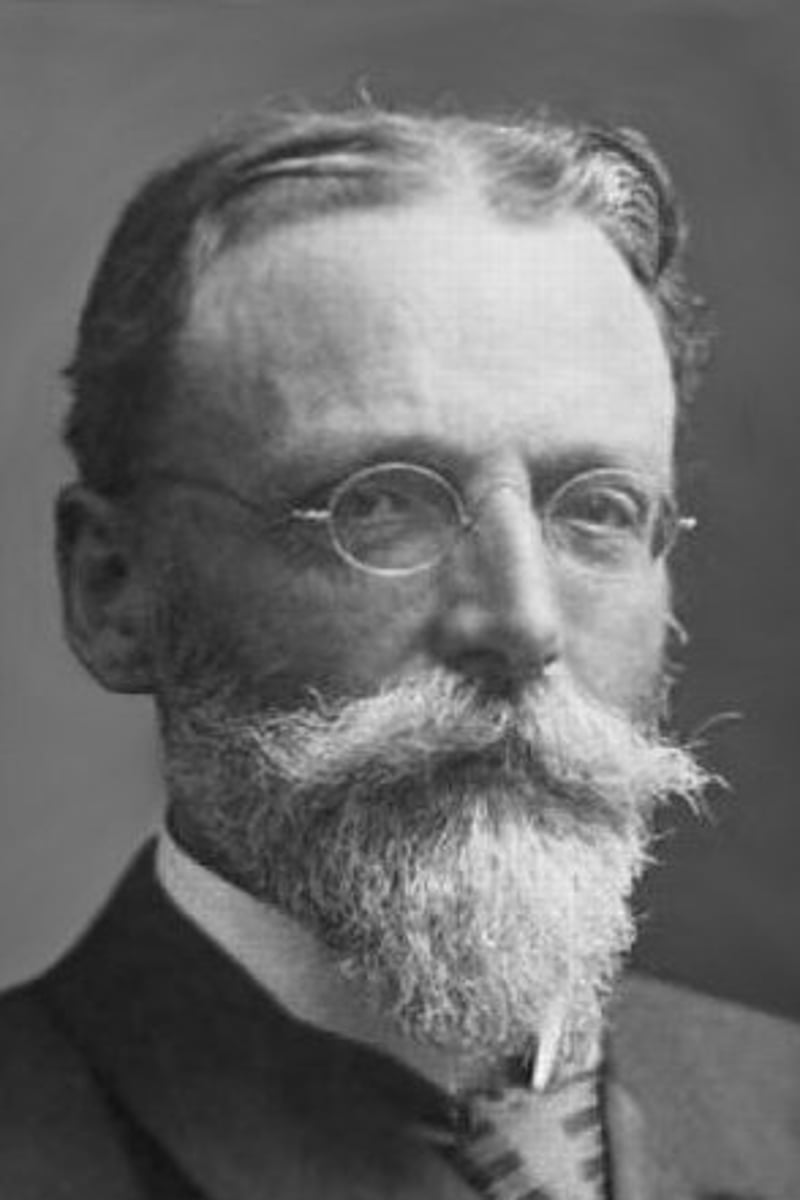
Theodor Escherich
(discovered e-coli)
Claimed meconium was sterile and intestinal colonisation was attributed to infants early environment (milk)
Necrosis
Accidental and unregulated, results from damage to cells and loss of ionic homeostasis, not energy dependent
Necrosis mechanism
1. Damage to lysosomal membrane leads to spillage of hydrolytic enzymes into cytoplasm which digests cellular contents.
2. Cell content leaks through damaged plasma membrane into extracellular space and elicit inflammation
3. nuclear changes all due to non-specific breakdown of DNA (karyolysis, pyknosis, karyorrhexis)
4. Leads to ischaemia, infections, trauma and exposure to toxins
Mitochondrial damage results in:
Decreased ATP giving multiple downstream effects
Increased ROS so damage to lipids, proteins and DNA
DNA damage effect
Activation of pro-apoptotic proteins
Membrane damage effect
Plasma: loss of cellular components
Lysosomal: Enzymatic digestion of cellular components
Homeostasis definition
The maintenance of a constant internal environment. Purpose of physiological regulation is to clamp internal parameter at a 'setpoint'
Allostasis definition
Stability through change. Parameters are not constant and variations are designed to reduce error
Aetiology
Cause of disease
Pathogenesis
Mechanism of disease
Inheritance of mitochondrial DNA (mtDNA)
Normally inherited exclusively from the mother
The mitochondria in mammalian sperm are usually destroyed after fertilisation
Structure of mitochondria DNA (mtDNA)
Compact, circular, double stranded. One mitochondria has dozens of copies of mito genome and each cell has numerous mitochondria
mtDNA defects
Proportion if mtDNA pathogenic variants must exceed a threshold before abnormality is expressed (threshold effect)
Heteroplasmy
Mitodisorders: mix of mutated and wild type mtDNA
Homoplasmy
At birth: all mitochondria identical
Mitochondrial disorders
Inherited, reduced ATP production.
E.g. Leigh syndrome, Pearson syndrome
Clinical presentation of mitochondrial disorders
Organs and tissues with high energy demands (brain, nerve, eye, cardiac/skeletal muscles susceptible)
Symptoms diverse: developmental delay, seizures, myopathy, retinopathy
Mitochondrial replacement Therapy
Ccombine the nuclear DNA of a woman carrying a mtDNA mutation with DNA of a sperm and the egg of a healthy donor, allowing her to give birth to a child free from mitochondrial disease.
Mitochondrial replacement Therapy techniques
Pronuclear transfer
Maternal spindle transfer
Pronuclear transfer technique
1. Patient couple and donor egg both fertilised making a pro nuclear zygote
2. Discard the nucleus of donor egg
3. Insert nucleus of patient couple egg into donor egg
Maternal spindle technique
1. Remove karyoplast (containing meiotic spindle) from patient couple and donor egg.
2. Discard karyoplast of donor egg
3. Insert patient couple karyoplast into donor egg
4. Fertilise egg resulting in pronuclear zygote
Phosphatidylinositol
On the inner membrane leaflet,
Can be phosphorylated, serving as an electrostatic scaffold for intracellular proteins,
(poly)phosphoinositides can be hydrolyzed by PLC (phospholipase C) to generate intracellular second signals (diacylglycerol and IP3.)
Phosphatidylserine
Found on inner leaflet but flips to extracellular in cells during apoptosis,
Can act as a cofactor in blood clotting
Structural changes in response to alterations in physiological states and some pathological stimuli
Hypertrophy, hyperplasia, atrophy, metaplasia
Hypertrophy
Increases sizes of cells/ affected organ (e.g. myocardial hypertrophy)
Hyperplasia
Increase in number of cells
Atrophy
Reduction in size of tissue/organ due to decrease in cell number (can be resulted from reduced protein synthesis and increased protein degradation)
Can be proteasomal or autophagic
(E.g Cerebrovascular diseases, Alzheimers)
Metaplasia
Reversible change where one differentiated cell type is replaced by another cell type (e.g. in smokers: columnar to squamous in respiratory tract)
Metaplasia from squamous to columnar cells
In respiratory tract in response to chronic irritation
Metaplasia from columnar to squamous cells
Barrett oesophagus
Mechanism of reversible cell injury
1. reduced oxidative phosphorylation leads to depletion of ATP
2. Changes of ion concentrations and water influx causes cellular swelling
3. Mitochondrial/ cytoskeleton alterations
4. Calcium ions play a central role in progression to irreversible cell death
Fundamental causes of necrotic death
Depletion of ATP
1. Reduction of plasma-membrane energy dependent sodium pump
2. Increase in anaerobic glycolysis
3. Failure of Ca ion pump, influx of Ca ions
4. Disruption of protein synthetic mechinery
5. Deprevation of oxygen/ glucose leads to protein misfolding
Influx of Ca and loss of Ca homeostasis effects
1. Accumulation of Ca2+ in mitochondria results in opening of MPTP and failure of ATP generation
2. Can cause inappropriate activation of enzymes (e.g. phospholipase, proteases, endonuclease, ATPases)
3. Direct activation of caspases
Major consequences of mitochondrial damage
1. MPTP channel opens leading to loss of mitochondrial membrane potential, resulting in failure of oxidative phosphorylation and progressive depletion of ATP leading to necrosis
2. Abnormal oxidative phosphorylation also leads to formation of reactive oxygen species (ROS)
3. Mitochondria sequester various proteins capable of inducing apoptotic pathways between outer and inner membranes
CASPase
A family of proteases that, when activated, mediates the destruction of the cell by apoptosis.
Cysteine Aspartyl Specific Protease.
Accumulation of Oxygen-Derived Free Radicals
Cell damage through membrane lipid peroxidation, protein modification and DNA breakage as they as highly reactive.
reperfusion injury.
ROS
1. Superoxide
2. Hydrogen peroxide (H2O2)
3. Hydroxyl radical (OH)
Apoptosis features
1. Cell shrinkage
2. Chromatin condenstion
3. Formation of cytoplasmic blebs and apoptotic bodies
4. phagocytosis of apoptotic cells
Mechanism of apoptosis
1. Enzymatic cleavage of inactive zymogens to synthesise and activate CASPases
2. Cleave their substrates after specific tetrapeotide motifs
3. Initiator caspase (8) and executioner caspases (3.6,7) degrade critical cellular components
B-cell lymphoma-2 (BCL-2)
Critical regualtors of apoptosis
Devided into 3 groups: anti-apoptotic, pro-apoptotic, pro-apoptotic activators.
Anti-apoptotic
BCL-2, BCL-XL and MCL1 have 4 BH (1-4) domains.
They prevent efflux of cytochromeC (and other apoptotic proteins) into cytosol
Pro-apoptotic
BH-3 only proteins sense damage and activate BAX and BAK (effectors) to form oligiomers within the outer mito membrane to induce permeabilisation/ leakage of mitochondrial proteins
Pro-apoptotic activators
BAD, BIM, BID, Puma and Noxa. Only 1 BH domain (BH-3 only proteins).
Act as sensors of cellular stress and damage, regulate balance of other groups.
Regulation of apoptosis
1. Survival signals/ growth factors stimulate synthesis of anti-apoptotic proteins
2. Deprivation of growth factors is sensed by BH3-only proteins and pro-apoptotic effectors activated
3. Cytochrome C released into cytosol binds to APAF-1 to form apoptosome, binding cascade 9 leading to autoamplification
4. Other mitochondrial proteins enter cytoplasm to neutralise IAPs (inhibitors of apoptosis)
Probiotics
Introducing known microbes back into the body
Prebiotics
Non-digestible nutrients that promote growth of friendly bacteria
Symbiotics
Contains both pre/probiotics
Father of microbiology
Anton van Leeuwenhoek
Microbiota first sighting
Anton Van Leeuwenhoek examined plaque from teeth using microscope. He saw microbes moving around. Realised that drinking coffee stopped their movement so they must be alive. Called them animalcules
Holobiont
Co-dependent relationship between humans and microbes
Where are microbes present in humans
Skin, mouth, pharynx, respiratory system, urogenital tract, stomach, intestinal tract (high density, 70%)
Microbiota
Community of micro-organisms that colonise normal healthy people
Microbiome
the collective genome of all microbes in a microbiota, can influence fitness, phenotype and health of host
Ratio of Human Cells to Bacterial Cells
1:1
Parasitism
One species benefits and the other is harmed
Commensalism
One species benefits, and the other is unaffected
Mutualism (symbiosis)
Both species benefit from the relationship
How do you acquire your microbiome
Mother is principle source, breast-feeding can provide useful bacteria (formula fed has fewer probiotic bacteria), solid foods
Benefits of intestinal microbes
Digestion,
Microbial antagonism,
Vitamins (K and B12),
Development,
Immune system
Microbial antagonism
Microbes take up space and secrete anti-microbial agents, preventing harmful pathogens taking hold
Obligate aerobes
Can only survive in presence of oxygen
Facultative anaerobes
Can use and grow faster with oxygen but doesn't require it to grow
Aerotolerant anaerobes
Don't use oxygen but can tolerate it
Microaerophilic
requires only a small amount of oxygen
Obligate anaerobes
Die in the presence of oxygen
Major phyla in gut microbiota
Bacteroidetes,
Firmicutes,
Actinobacteria,
Proteobacteria
Gram positive bacteria
Firmicutes, Acrinobacteria,
1 phospholipid bilayer and thick outer layer of peptidoglycan
Gram negative bacteria
Bacteroidetes, Proteobacteria,
2 phospholipid bilayers with a thin peptidoglycan layer in-between
Syntrophy
some bacteria live together and supply each other with essential nutrients
Metagenomics
the study of genetic material recovered directly from environmental samples
GALT (gut associated lymphoid tissue)
Learns to tolerate microbes and rejects new-comers, meaning we maintain stable gut microbiota composition
The best way of determining species diversity in human faecal microbiota is to use:
Metagenomics
3 multiple choice options
Two 16S rRNA genes are considered to be from different species if they have less than ... % similarity
97%
3 multiple choice options
Limitations of 16S approach
Highly dependent on choice of primers, some pairs may not amplify 16S DNA from whole classes of bacteria.
Some bacteria are harder to get DNA out of than others.
Dysbiosis
Microbial imbalance, found in autoimmune diseases (e.g. obesity, cardio metabolic)
Metabolic syndrome
A cluster of interrelated metabolic abnormalities: (obesity, dyslipidemia, hyperglycemias and hypertension) that enhance the risk for CV disease and type 2 diabetes
Pathogenic factors for metabolic syndrome
Insulin resistance and visceral obesity
Insulin resistance
Defect in insulin action but normal production by beta cells of pancreas, caused by abundance of circulating fatty acids
How do fatty acids reduce insulin sensitivity
Inhibit insulin-mediated glucose uptake, blocking transport of glucose into cells. This increases circulating levels of glucose which elevates pancreatic insulin secretion causing hyperinsulinaemia
Adipose tissue specialised for:
Storage and mobilisation of lipids, also an endocrine organ that releases cytokines: (FFAs, TNFa, C-reactive protein, interleukin-6, adiponectin and leptin)
Adiponectin
Produced by adipose cells that inhibits inflammation and protects against insulin resistance, type 2 diabetes, and cardiovascular disease
Leptin
Increased during obesity, decline with weight loss.
Elevated levels do not suppress appetite and increases BP through activation of sympathetic nervous system
Leptin resistance
Fundamental pathology in obesity
Insulin sensitive phenotype
normal body weight, no abdominal/visceral obesity, moderately active, diet low in saturated fats
Insulin resistance pathophysiology
1. pancreatic beta cells secrete more insulin to overcome hyperglycemia
2. overexpression of insulin activity in normally sensitive tissues
3. exaggeration of insulin action and resistance to other actions lead to clinical signs of MetS (metabolic syndrome)
4. Over time pancreas beta cells are unable to produce sufficient insulin leading to hyperglycemias and type 2 diabetes
Insulin receptor
Ligand-activated tyrosine kinase
Insulin signalling
Binding of insulin receptor (tyrosine kinase) results in tyrosine phosphorylation of downstream targets and activation of two pathways: (PI3K and MAPK pathway)
Obesity definition
Accumulation of adipose tissue that is of sufficient magnitude to impair health. BMI over 30kg/m*2
Hunger and satiety
controlled by complex neuroendocrine system- bidirectional crosstalk between feeding centres in brain and periphery
Short term regulators of food intake
Ghrelin, CCK (cholescystokinin), PYY (peptide tyrosine tyrosine), GLP-1 (glucagon-like peptide), GIP (glucose-dependent insulinotropic polypeptide), OXM (oxyntomodulin), glucagon, GFG21
Long term regulators of food intake
Leptin, insulin, amylin
How is obesity related to cancer
(Proposed)
Altered levels of adipokines, disrupted insulin signalling, local and systemic effects of inflammation, modifications of microbiome
Why is diabetes a major healthcare problem
How does necrosis happen?
- Damage to lysosomal membrane leads to spillage of hydrolytic enzymes into cytoplasm and digest cellular components