Blood Physiology
1/203
Earn XP
Description and Tags
module 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
204 Terms
Blood
A liquid connective tissue connected to various types of cells dissolved in a liquid medium called plasma.
Gases, nutrients, and hormones are also dissolved in the liquid component of blood.
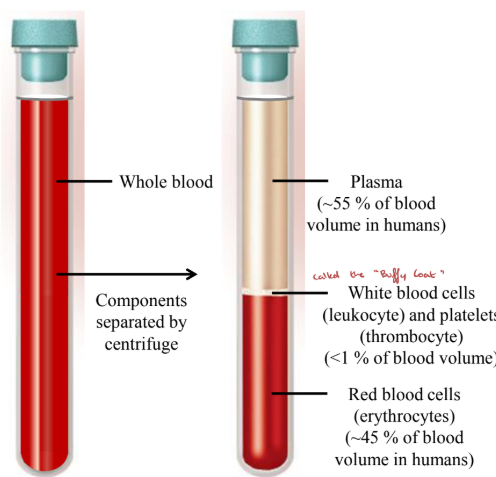
Heavier + more viscous than water and will sediment when allowed to rest (test tube).
Cellular components can be separated when centrifuged.
Blood Location
Flows through the circulatory system.
Some cellular components of blood can exit blood vessels to tissue sites.
Blood Functions
Transport: O₂, CO₂, nutrients, waste products, ions, hormones, and heat.
Regulation: ion and pH balance.
Defense: immune protection.
Hemostasis: prevention of blood loss.
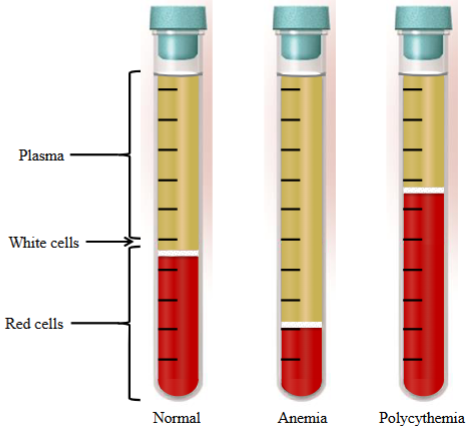
Hematocrit
The percent of total blood volume occupied by packed red blood cells.
Where (x = volume of RBC’s)/(y = total blood volume) × 100%.
42 ± 5% (Females).
47 ± 5% (Male).
Anemia
Decreased oxygen-carrying capacity of the blood due to a deficiency of RBC’s and/or hemoglobin contained in the RBCs.
The hematocrit value is significantly below the standard levels.

Polycythemia
Where the value of the hematocrit is significantly higher than the normal range.
A value of > 48% in women and > 52% in men is a sign of polycythemia.
Sometimes seen as an adaptation in mountain/high altitude dwellers who are frequently exposed to low O₂ levels, leading to increased RBC levels.
Sometimes seen in athletes that use erythropoietin (EPO) to artificially raise their RBC count to increase efficiency of performance.
Body Fluids
Refers to a watery solution containing dissolved substances (i.e. O₂, nutrients, waste).
Fluid Compartments
Intracellular: Inside cells → within the cells.
Extracellular: Outside cells → fluid present in blood and spaces surrounding the cells. Includes plasma and interstitial fluid.
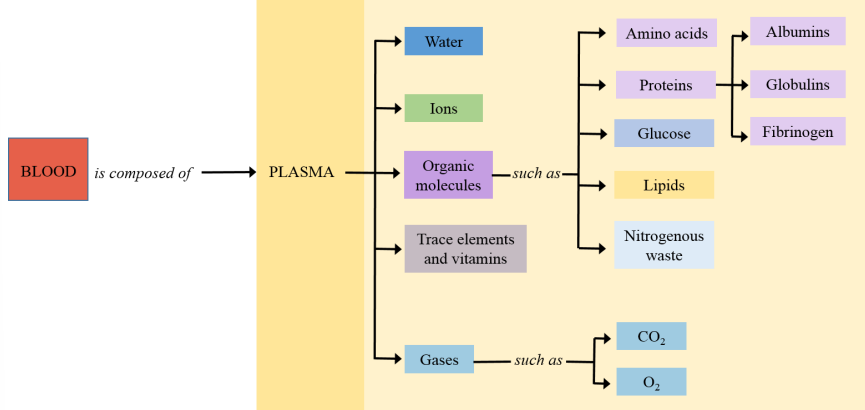
Plasma
Non-cellular portion of blood.
The liquid portion of blood.
Interstitial Fluid
Fluid found around and between cells.
Composition of Plasma
Liquid portion of the blood. Mainly water (>90%).
Electrolytes, organic molecules, trace elements and gases.
Substances being transported (O₂ and CO₂, nutrients, waste products, hormones).
Know the chart.
Albumin
Major contributors to the colloid osmotic pressure of plasma.
Carrier for various substances in the blood. They bind various ligands and act as transporters for these molecules.
Comes from the liver.
Globulin
Act as a clotting factor, enzymes, and antibodies.
Carriers for various substances in the blood.
Comes from the liver and lymphoid tissue. Some plasma proteins are produced in the B-cells of lymphoid tissue.
Fibrinogen
Forms fibrin threads essential for clotting.
Comes from the liver.
Transferrin
Transports iron and puts it in circulation.
Comes from the liver and other tissues.
Functions of Plasma Proteins - Body Water
Distribution of body water - contribute to colloid osmotic force and helps the distribution of water between the capillaries and the interstitial space.
Functions of Plasma Proteins - Buffering
Plasma proteins buffer the H⁺ concentration and help with pH balance.
Functions of Plasma Proteins - Transport
Many hormones are transported in the blood upon binding to plasma proteins.
Functions of Plasma Proteins - Defense
Things such as antibodies, which are proteins that contribute to immune defense.
Functions of Plasma Proteins - Hemostasis
Clotting proteins are plasma proteins, which help maintain hemostasis.
The stopping of blood flow from loss of blood (a damaged vessel).
Serum
Is a fraction of plasma from which fibrinogen and all other clotting factors have been removed.
Blood Cell Numbers
Red Blood Cell (Erythrocytes) | 4.2 to 5.1 × 10⁶ (F) 4.7 - 6.1 × 10⁶ (M) |
White Blood Cell (Leukocytes) | 4.5 × 10³ |
Platelets (Thrombocytes) | 1.5 - 4 × 10⁵ |
All values are in µL
Polymorphonuclear Granulocytes (PMNG)
Each type of granulocyte is identified based on the staining characteristics of the cytoplasmic granules and the structures of the nuclear lobes.
The naming of granulocytes originated from the cytoplasmic granules for the stains hematoxylin and eosin.
Used to identify these cells.
Eosinophils
Granules that stain pink/red because of an affinity with eosin.
Aids in defense against parasites.
A PMNG.

Basophils
Granules are dark blue/violet with the basic stain hematoxylin.
Aids in inflammatory response.
A PMNG.

Neutrophils
Have granules, but are not stained by either eosin or hematoxylin.
A phagocyte and a PMNG.

Monocytes
Largest white blood cell.
Leaves the bloodstream and transform into tissue macrophages.
Macrophages are phagocytic cells, playing a role in immune defense.
B-Cell
A lymphocyte.
Produces antibodies in the humoral immune response (the fluids).

T-Cell
Aids in cellular immunity.

Platelet
Smaller than red blood cells.
Aids in hemostasis.
Also called thrombocyte.

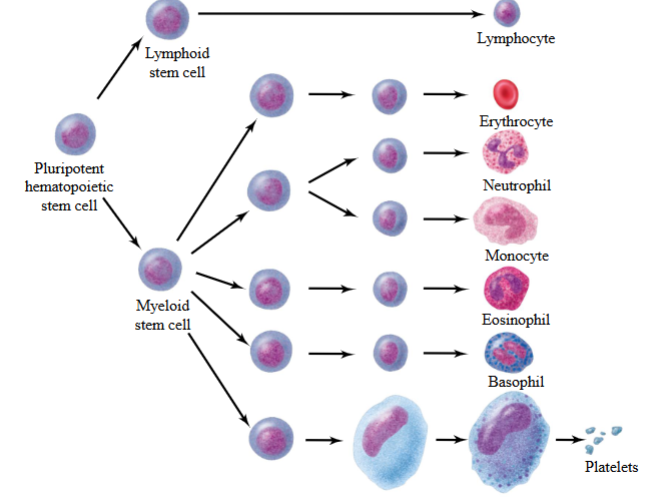
Hematopoiesis
The process of formation of blood cells.
Process of blood cell formation is controlled by different types of cytokines.
Prenatal = yolk sac, liver, spleen.
Postnatal = bone marrow.
Begins from a pluripotent hematopoietic stem cell and differentiates into different blood cells.
Pluripotent Hematopoietic Stem Cells
Undifferentiated cells capable of giving rise to any type of blood cell (i.e. RBC, WBC, and platelets).
All blood cells stem from a single a single population of hematopoietic stem cells.
Cytokines
Small secreted proteins released by cells and have a specific effect on the interactions and communications between cells.
Share a common property with hormones of being secreted to the bloodstream and other body fluids by all the cells that produce them.
They exert their effect by interactions with the receptors in their target cells.
Also called hemopoietins.
Act as growth factors.
RBC Biconcavity
Concave on both sides.
Its shape allows for twists and turns. Allows the cell to pass and bend through small arterioles and capillaries.
Offers a higher surface area to volume ratio, and therefore allows for easy diffusion of O₂ in and out of the cell.
Red Blood Cells
Originates in the bone marrow.
Mature RBC’s lack organelles such as mitochondria, ribosomes, and the nucleus to make space for oxygen.
Primary function is O₂ transport.
Lifespan: 120 days.
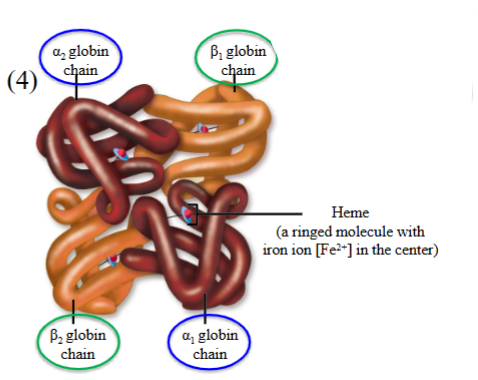
Hemoglobin (Hb)
= heme (non-protein) + globin (protein)
Dominant iron-binding protein in red blood cells.
Responsible for ~98-99% of O₂ transport.
Binds to oxygen in loose and reversible manner.
Hemoglobin A (HbA) - α2β2
Made of 4 globin chains, two α chains and two β chains.
These chains are normally found in their highly-folded structure.
Inside each pocket of the chain, there lies a heme-containing group.
At the center of a heme group contains a ferrous or divalent iron molecule.
Each of these ferrous irons can bind to a single molecule of oxygen.
∴ a single HbA molecule has four globin chains, four heme groups, four ferrous irons, and can bind to a max of four O₂ molecules.
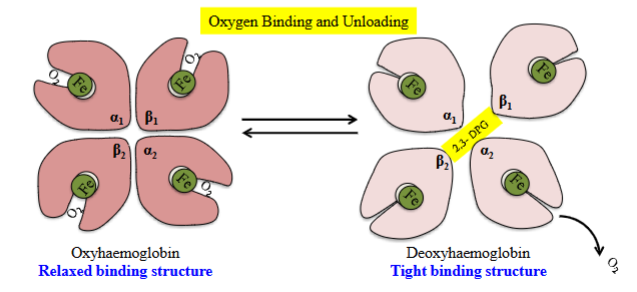
Oxyhaemoglobin
During oxygen binding, the O₂ molecule exists in a loose/relaxed structure.
Allows for the quick and cooperative binding of oxygen.
The binding of O₂ to hemoglobin is known as cooperative binding.
The binding of successive oxygen facilitates binding of the next.
Each ferrous (Fe²⁺) iron combines with one molecule of O₂ by the process of oxygenation.
O₂ increase within a tissue.
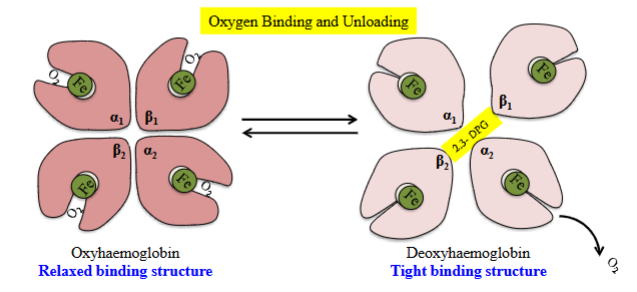
Deoxyhaemoglobin
Once giving away oxygen to peripheral tissues, the hemoglobin switches to a tight structure.
Does not contain oxygen.
Carbon Monoxide Inhalation
Hb can bind to other gases (i.e. CO₂, CO, NO). A colourless and odourless gas.
CO has a extremely high affinity for the O₂ binding site on hemoglobin.
200x greater affinity for CO.
This allows CO to bind to hemoglobin easily and cannot be displaced from the binding site.
When CO and O₂ are present, hemoglobin prefers to bond to CO.
Very fatal.
Factors for RBC Synthesis
Cytokines.
Erythropoietin (EPO).
Dietary factors: iron, folic acid, and vitamin B12.
Protein factor released from stomach, called intrinsic factor (IF).
Folic Acid
Needed for any developing cell.
During cell division and growth, all newly forming cells go through DNA.
Helps to add thymine (T in DNA).
However, its actions cannot be executed without vitamin B12.
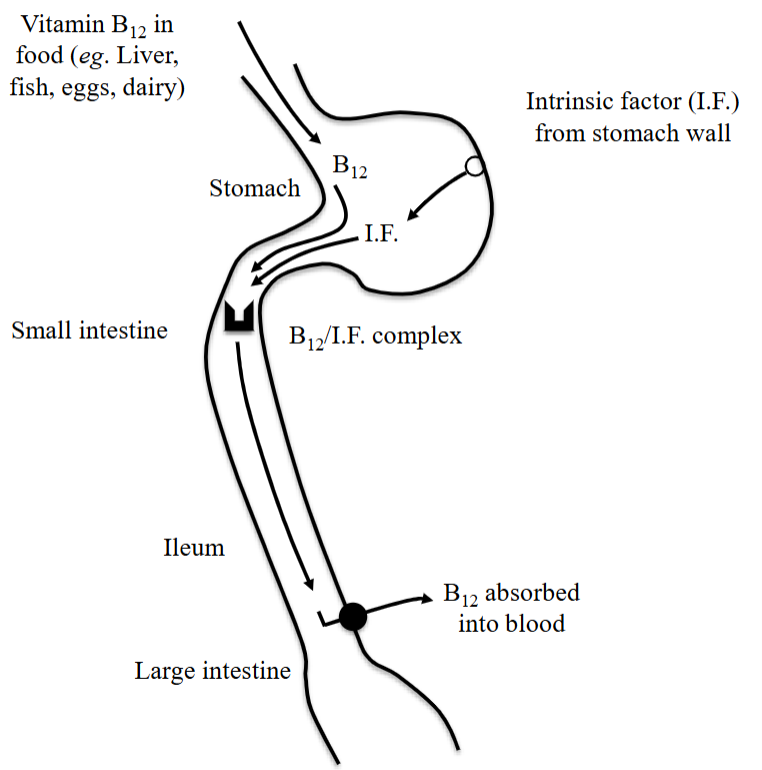
Vitamin B12
Can only be acquired through diet and must go through a process before it can be absorbed by the body.
Intrinsic Factor (IF)
The protein is synthesized by stomach cells.
Required for the absorption of vitamin B12 and RBC synthesis.
Erythropoietin Synthesis
Hypoxia (low O₂) is sensed by the kidney cells, which then increase EPO levels.
EPO levels in the plasma increase.
EPO is carried by blood to the bone marrow, acting on the hematopoietic stem cells to stimulate RBC synthesis.
RBC’s are synthesized, which increases the blood hemoglobin conc, increasing oxygen-carrying capacity.
Results in tissue oxygenation, decreasing EPO levels.
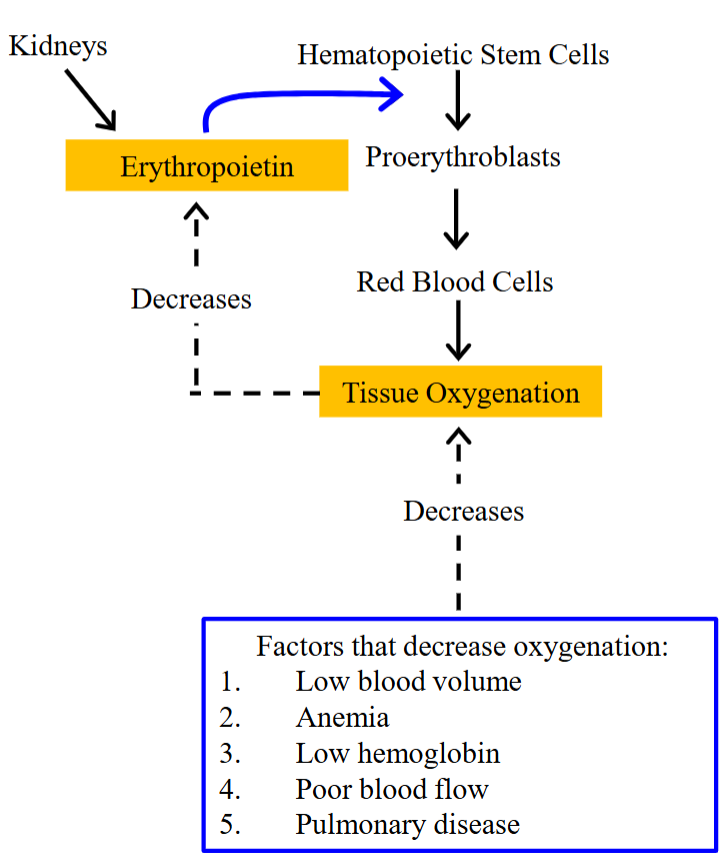
Hypoxia
Factors that decrease oxygenation, contribute to low oxygen levels.
Low blood volume.
Anemia.
Low hemoglobin.
Poor blood flow.
Pulmonary disease.
Recirculation of Iron
Iron levels are kept at a constant homeostatic balance because the rate of absorption from the intestine is dependent on the amount of iron lost.
If iron loss is high, then the rate of absorption from the intestine increases.
Extra iron is stored (liver) or lost though urine, skin cells, sweat, and menstrual blood.
Iron is bound to transferrin & iron-transport plasma protein.
It is carried to the bone marrow where it is utilized in synthesizing hemoglobin.
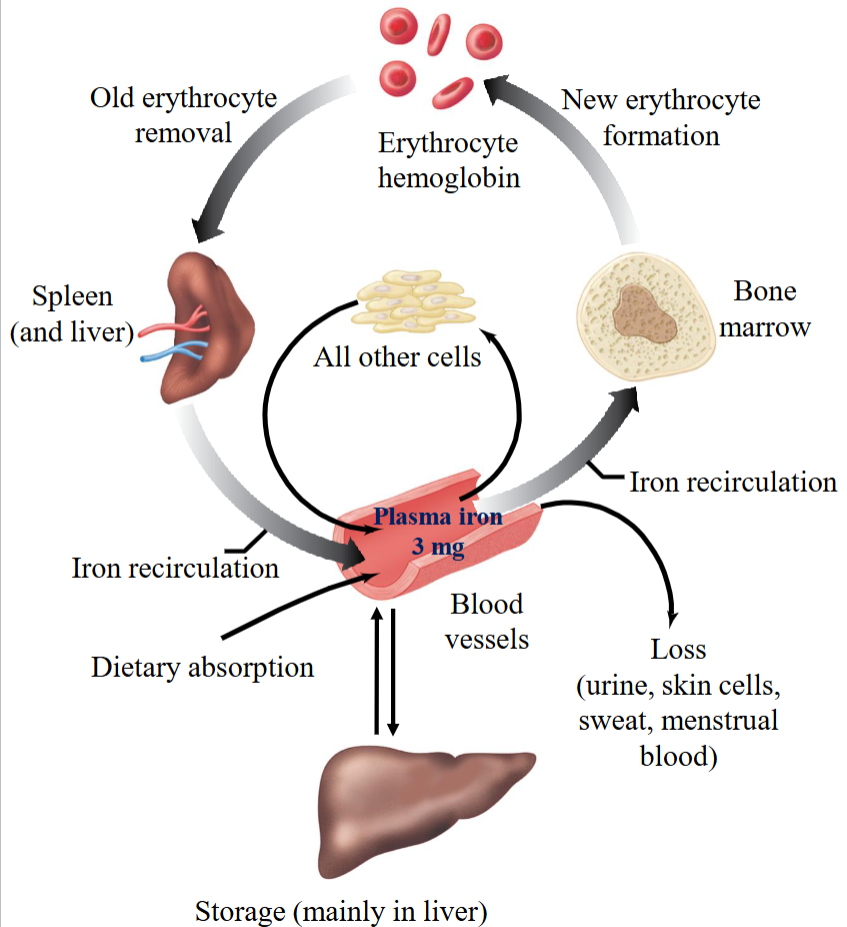
Body Iron Reserve
50%: hemoglobin (released by recycling dying RBC’s).
25%: other iron-containing proteins.
25%: Bound to a protein called ferritin (stored in the liver).
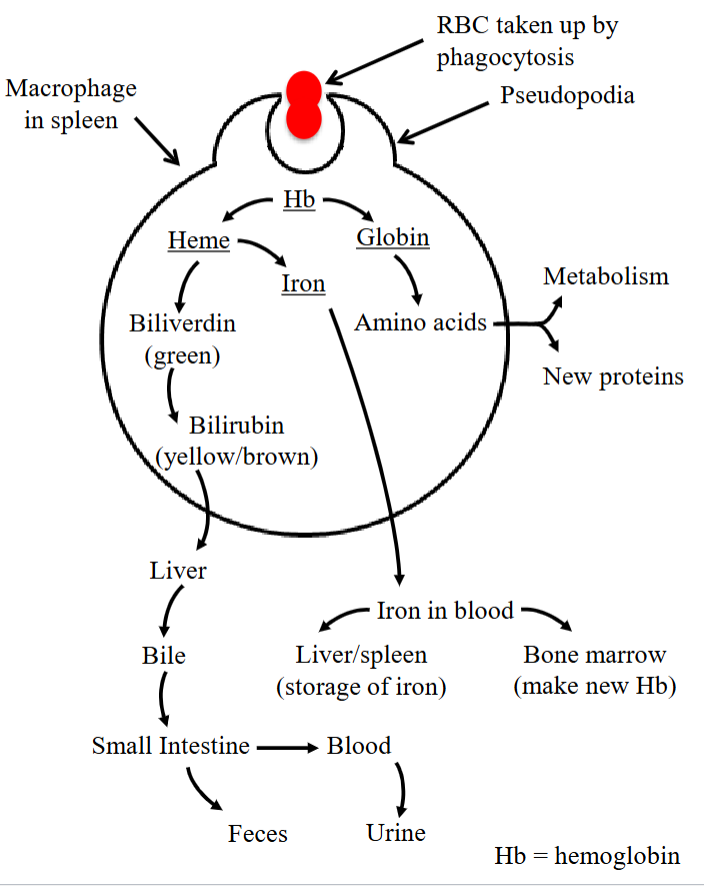
Recycling Iron - Pseudopodia
Step 1 of the process.
The dead and degenerated RBC’s are handled in the spleen to recycle iron from hemoglobin.
The cells that are involved in the process are the macrophages.
As they pass through the spleen, the macrophages engulf them using their cytoplasmic pseudopodia-like structures.
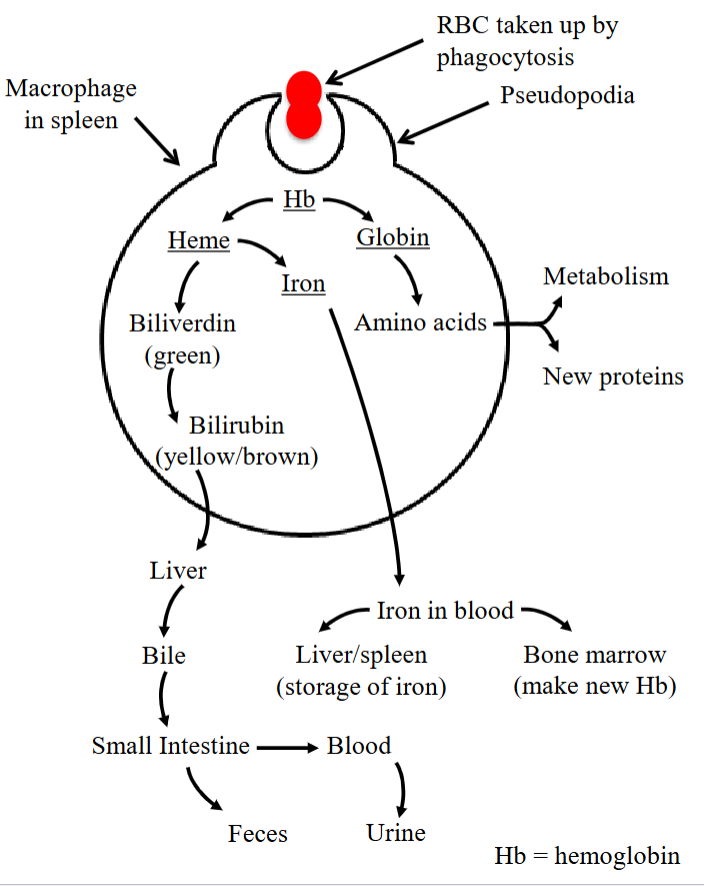
Recycling Iron - Globin
Hemoglobin is broken down into a heme group and a globin group.
The protein group (“globin”) is converted into amino acids and either used up in metabolic pathways or synthesized into new proteins.
The heme group (non-protein group) undergoes further breakage.
Step 2 in the process.
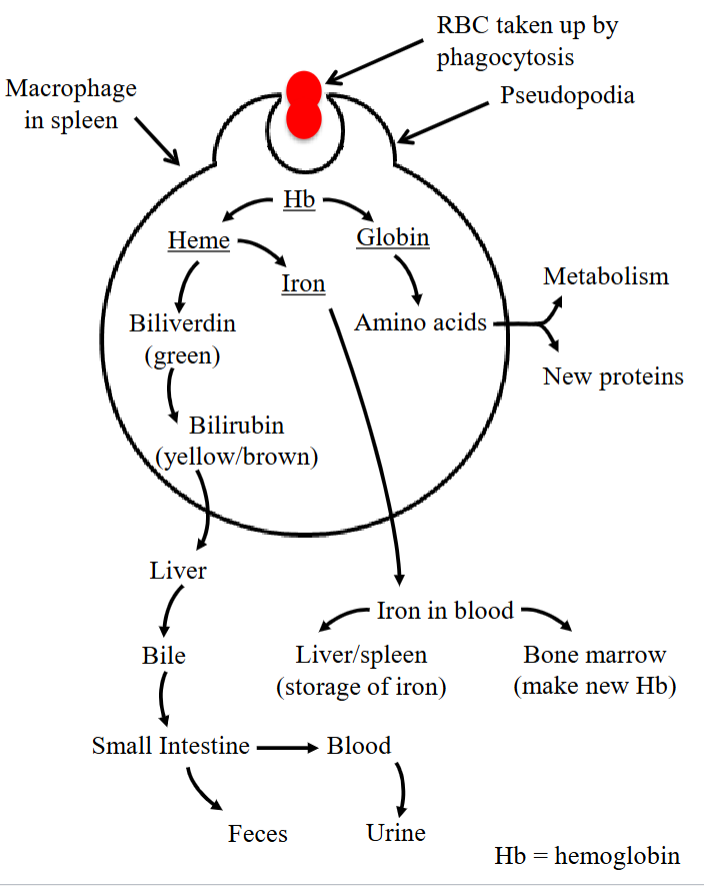
Recycling Iron - Heme
The heme group splits into iron and biliverdin (green).
Iron enters the blood and is either stored in the liver/spleen (as ferritin) or sent to the bone marrow to make hemoglobin (for EPO).
Biliverdin is converted into bilirubin (yellow/brown), which the liver turns into bile and secretes into the small intestine.
From there, it either enters the blood and is excreted in urine or exits as fecal waste.
This is the final step in the process.
Absorption of Vitamin B12
Vitamin B12 can only be consumed through diet (i.e. liver, fish, eggs, dairy).
Absorption of vitamin B12 requires intrinsic factor (IF) secreted from the stomach wall.
It goes to the small intestine, where B12 will complex with IF.
These bind to sites on epithelial cells in the ileum of the small intestine.
In the large intestine, B12 is absorbed into the blood.
Lack of vitamin B12 causes pernicious anemia.
Causes of Anemia
Decreased production of RBCs in the bone marrow.
Increased destruction of RBCs in the body (hemolytic anemia)
Where blood is being destroyed faster than it can be created.
Increased blood loss leading to loss of RBCs (hemorrhagic anemia).
Abnormal hemoglobin production → will affect O₂ carrying capacity.
Factors Leading to Anemia
Lack of iron.
Lack of IF or Vitamin B12 (pernicious anemia).
Damage of bone marrow due to radiation/drugs (aplastic anemia) → does not make enough RBCs, WBCs, and platelets.
Chronic kidney disease (reduced level of EPO).
Increased breakdown due to abnormal shape of RBC or immune reactions during transfusion (hemolytic anemia).
Increased blood loss due to injury, bleeding, ulcers, or chronic menstruation (hemorrhagic anemia).
Abnormal structure of hemoglobin.
Sickle Cell Disease
Abnormal globin chain (HbS = α₂β*₂). A single amino acid mutation in the β chain causes hemoglobin to form stiff rods, which distort red blood cells into a sickle shape.
Cell membranes are hard and nonflexible.
Passage through capillaries cause damage of sickled RBCs (hemolytic anemia).
Expressed by autosomal recessive gene carriers.
Immunity
Deals with the processes that help the interior of the cell or the body of the host to defend against anything foreign.
Defense of “self” vs. “non-self.”
Non-Specific Defenses (Innate Immunity)
“Physico-chemical.”
Physical barriers such as skin, enzymes in saliva, tears, mucus, and acidic gastric secretion.
No memory and fast response (s/min/hr).
Major cells involved include the neutrophils and macrophages (the phagocytes)
Cells that are always present and help with innate defense.
Major molecules involved include the complement system.
Specific Defenses (Acquired Immunity)
Immunity obtained from the development of antibodies (in response to antigen exposure).
Major cells involved include lymphocytes (B and T-Cells).
Has memory but takes time to develop (days/weeks).
Antibodies and cytotoxic molecules are the major molecules involved.
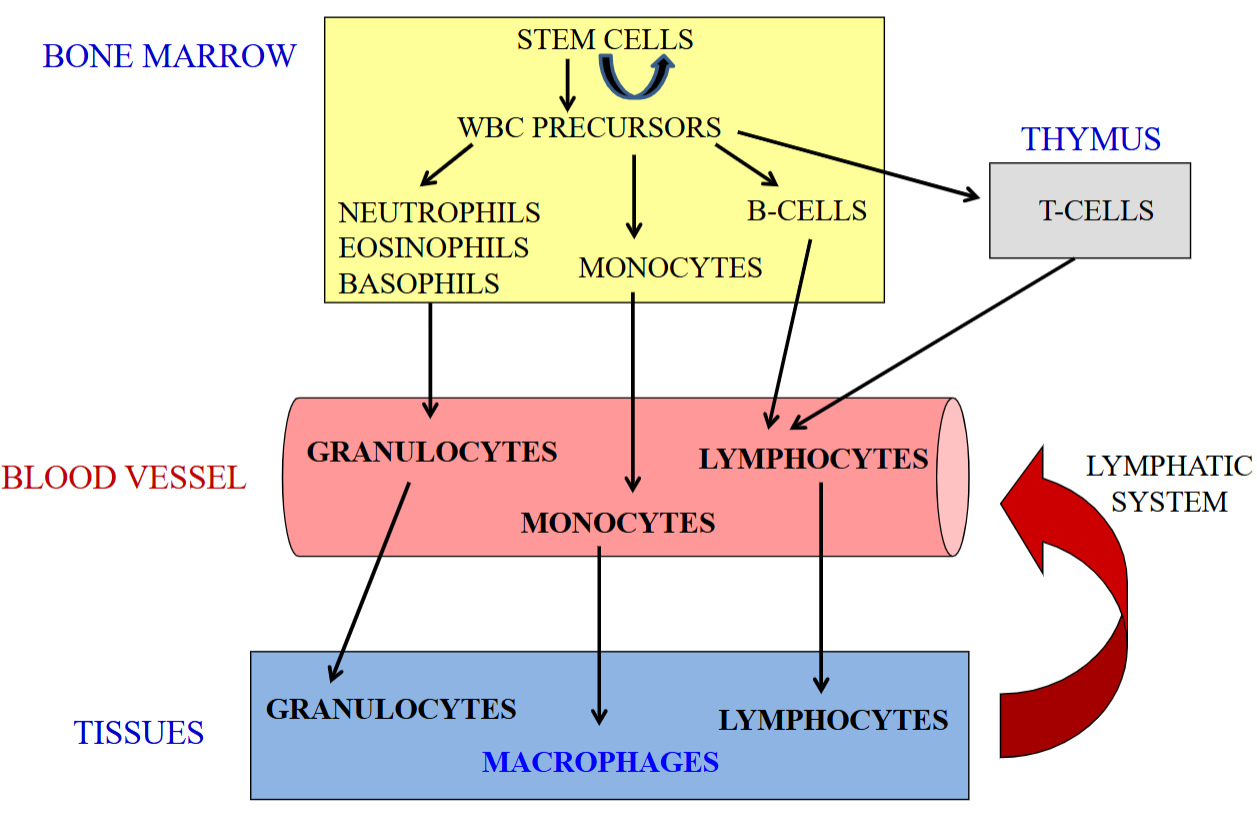
Synthesis of WBCs
Begins in the bone marrow. Under the influence of specific cytokines and growth factors, stem cells can be converted to granulocytes, monocytes, and lymphocytes.
Neutrophils, eosinophils, and basophils into the blood vessel (now granulocytes) goes into the tissues.
Monocytes go into the blood vessels but become macrophages once in the tissue.
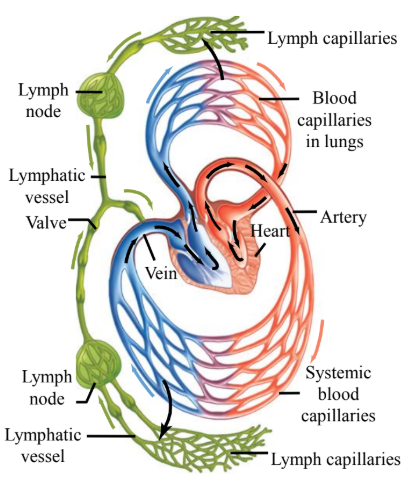
B-Cell and T-Cell development starts in the bone marrow; T-Cells finish developing in the thymus before returning to circulation.
Granulocytes and macrophages can exert their functions on peripheral tissues and die.
However, lymphocytes can go back into circulation via lymphatic circulation.
Innate vs. Acquired Immunity Table
Type of Immunity | Innate/Natural | Acquired/Adaptive |
Key Features | Non-specific. No memory. Fast. | Specific Has memory. Slow |
Major Cells Involved | Phagocytes (neutrophils and macrophages) | Lymphocytes (B-Cells and T-Cells) |
Major Molecules Involved | Complement System | Antibodies Cytotoxic molecules. |
Inflammation
The cells in our body are generally protected by a physical barrier (i.e. skin).
The inner cavities are either protected by a mucus layer or antibacterial secretions.
The barrier can be compromised, resulting in inflammation.
Non-specific innate response to tissue injury initiates inflammation.
Inducers: cut, bullet wound, sun burn, infected sutures during surgery, and infection of tonsil (cold).
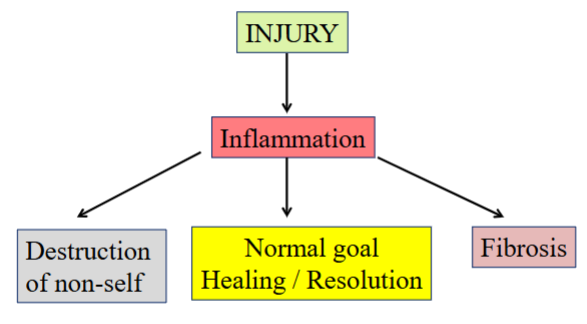
Purpose of Inflammation
To cause healing and resolution of the injury.
After injury, inflammation occurs. There are three different pathways that can occur afterwards.
Destruction of non-self. In the process, it can destroy any non-self agent that may invade the self.
Healing/resolution (normal goal).
Fibrosis (scar tissue).
Inflammatory Pathway
Generally has three components.
Inducers: Causative agents. They are the signals that initiate inflammatory responses.
Sensors: Sense the presence of foreign, non-self agents and activate mediators.
Mediators: Repair.
Characteristics of Inflammation
Act as pillars to support the process of inflammation.
Redness (rubor).
Swelling (tumor).
Heat (calor).
Pain (dolor).
Loss of function.
Vascular Changes during Inflammation
Histamine is released by mast cells (found in the skin tissue).
This inflammatory mediator causes expansion (vasodilation) of the blood vessels, increasing blood flow (associated with redness & heat).
It also increases the permeability of small blood vessels.
The “leakiness” allows proteins and cells to move out into the extracellular space.
Fluid also moves out, causing swelling.
Acute Inflammation - Vascular Events
Release of histamine, making local blood vessels dilate, resulting in blood vessels becoming leakier.
Accumulation of protein and fluid in the extracellular spaces.
Inflammatory mediators are released: bradykinin, prostaglandins, and complement proteins.
Bradykinin and prostaglandins are known to cause sensations of pain.
Acute Inflammation - Cellular Events
Resident macrophages entrap and kill pathogens, releasing chemical signals.
Increased movement of WBCs (neutrophils and monocytes) into infected area.
In the process, macrophages release chemical signals such as cytokines, which cause neutrophils to move to the site of injury.
Phagocytosis and destruction of foreign “non-self” agent.
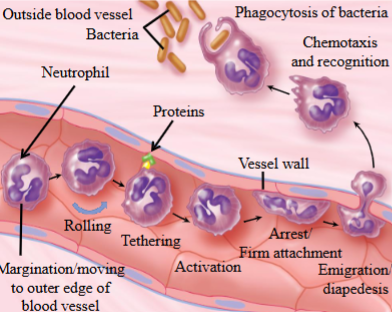
Cellular Events with Inflammation - Margination
Goal: to accumulate leukocytes (WBCs) in the inflamed tissue and kill the “non-self.”
This is step one in the process.
Margination of WBCs: if there is an entry of foreign bacteria, the WBCs (i.e. neutrophils) start moving towards the outer edge of the blood vessel.
They keep flowing along the vessel wall.
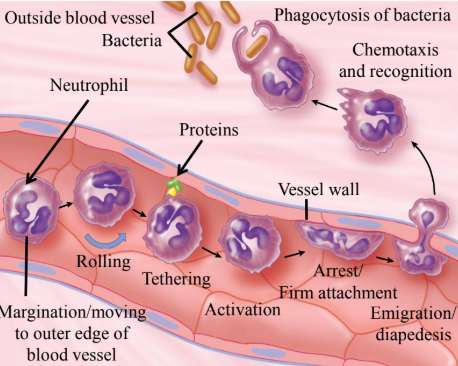
Cellular Events with Inflammation - Tethering
Initially, the WBC pace is fast.
Soon, the neutrophils begin tethering lightly to some proteins expressed on the surface of endothelial cells.
The WBCs begin to slow down and they begin rolling.
This is step 2.
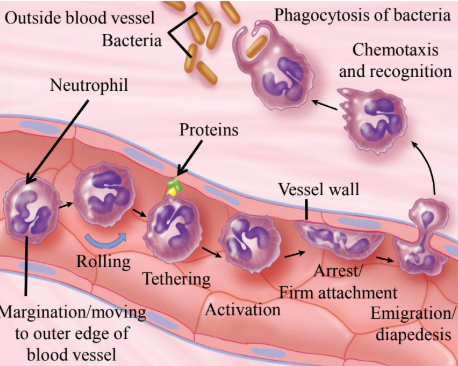
Cellular Events with Inflammation - Activation
Activation involves neutrophils, which under the influence of cytokines & other inflammatory mediators, start expressing specific proteins on their surface.
Simultaneously, endothelial cells also express proteins that help binding WBCs.
Step 3 in the process.
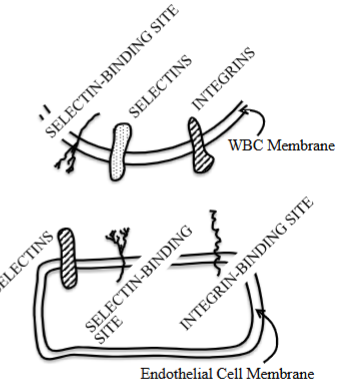
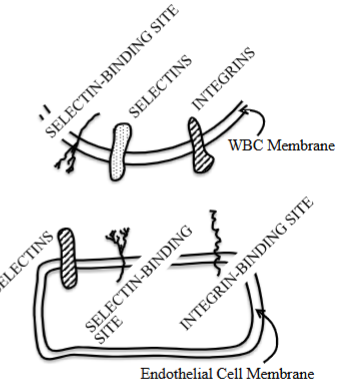
Cellular Events with Inflammation - Arrest
Neutrophils are firmly attached to the endothelial cell surface.
The protein expressed on the neutrophils usually attaches to complimentary binding proteins on the endothelial cells, which in turn produce proteins recognized by specific proteins on neutrophils.
The types of proteins are generally selectin or integrin.
Once the neutrophil proteins are tightly attached to proteins on the endothelial cell surface, the neutrophils stop rolling.
Step 4.
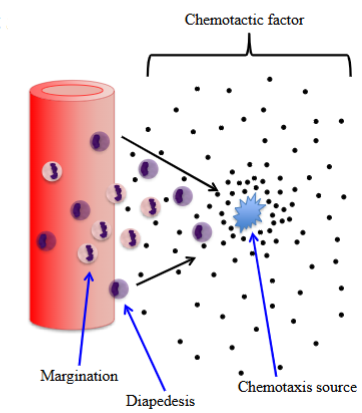
Cellular Events with Inflammation - Diapedesis
Where the WBCs can squeeze themselves in between the adjacent endothelial cells to exit out of the blood vessel and into tissue spaces.
Also called emigration.
Step 5 in the process.
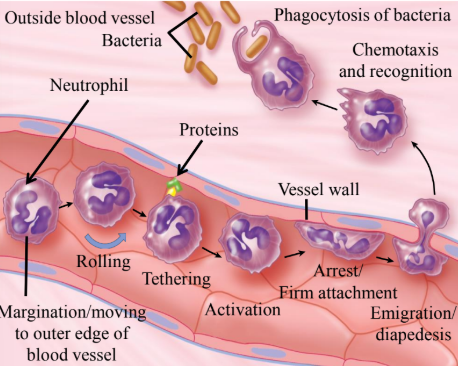
Cellular Events with Inflammation - Chemotaxis
Once the WBCs are outside the blood vessel, they move towards the site of inflammation by a process of cell movement.
This is known as chemotaxis.
This is step 6 in the process.
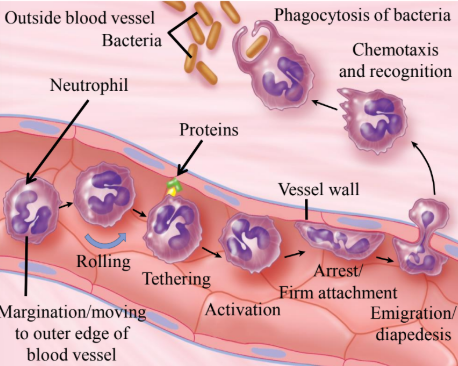
Cellular Events with Inflammation - Recognition
The recognition of “non-self” by WBCs.
At the site of infection, the WBCs recognize the foreign agent by the chemical molecules on their surface.
This is step 7.
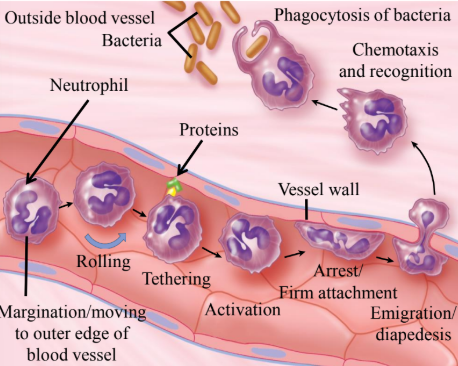
Cellular Events with Inflammation - Phagocytosis
The phagocytosis of “non-self” pathogen by WBCs.
The foreign pathogens/bacteria are engulfed by neutrophils by phagocytosis.
This is the last step.
Chemotaxis
Ability of WBCs to move against a concentration gradient (low > high) in response to chemical factors (chemotactic factors).
The WBCs move towards the source of a chemotactic substance.
Chemotactic Factors
Also called chemical factors.
They include:
Complement products (C5a).
Chemokines (IL-8).
Bacterial products.
Damaged membrane products (arachidonic acid metabolites)
Not one factor, but many factors that come into play to help the movement of WBCs to the source of infection.
Phagocytes
Refers to cells that can eat non-self pathogens or other dying cells by engulfing them.
Monocytes (macrophages), dendritic cells and granulocytes are phagocytic in nature.
They engulf foreign bacteria/dead cells using temporary cytoplasm-filled extensions (pseudopodia) which reach at the matter to be ingested.
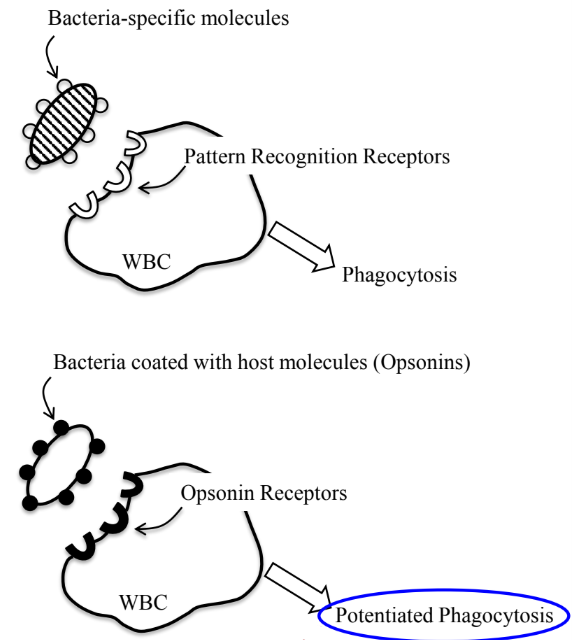
Sequence of Phagocytosis - Recognition
Recognition of foreign body → Step one.
Foreign body to be ingested is recognized by phagocytes.
Macrophages have cell surface receptors that recognize certain molecules on the surface of the various pathogens.
Sequence of Phagocytosis - Attachment
Attachment of the foreign body → step 2.
Phagocytes attacks the foreign body, activating phagocytosis.
Sequence of Phagocytosis - Internalization
Step 3.
Internalizes/ingests a foreign body using pseudopodia.
The ingested body now enclosed in a vesicle (called phagosome) which then fuses with a lysosome.
Sequence of Phagocytosis - Destruction
Step 4.
Destruction of the “non-self” pathogen.
Pattern Recognition Receptors (PRR)
Located on monocytes and macrophages, dendritic cells, and mucosal epithelial cells of the intestine, lymphocytes, and endothelial cells.
Help in recognition of common pattern → non-specific foreign organisms or dying cells.
Macrophages express several receptors specific for bacterial constituents.
Toll-like receptors.
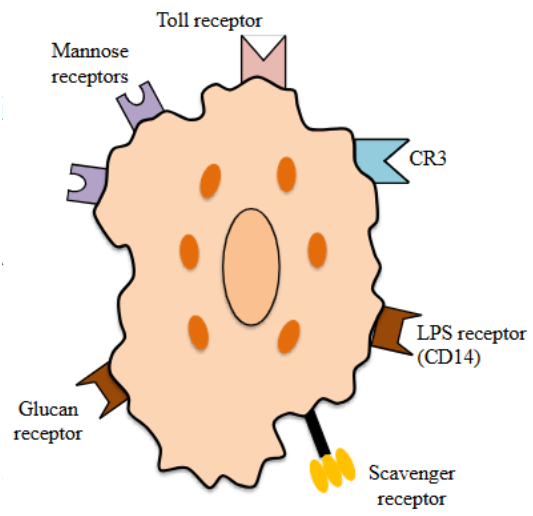
Lipopolysaccharide (LPS) Receptors
Which recognize LPS on gram-negative bacteria.
The macrophage does not have to recognize a specific type of bacteria of the gram-negative stream, but must recognize the pattern of LPS.
Opsonization
Opsonins are molecules which, when added to the surface of a bacteria, help speed up the rate of phagocytosis by macrophages or phagocytic cells.
They are produced by the self or host body and are usually of the antibody or complement protein type.
Coating the bacteria with opsonins produced by the host facilitates its attachment and phagocytosis by the phagocytic cell.
Potentiated Phagocytosis
Once the bacteria are coated with opsonin’s produced by the host body, phagocytosis is potentiated.
The immune system more effectively engulfs and destroys invaders when opsonins mark them for clearance.
Engulfment
Injurious agent surrounded by pseudopods and internalized in membrane bound phagocytic vacuole.
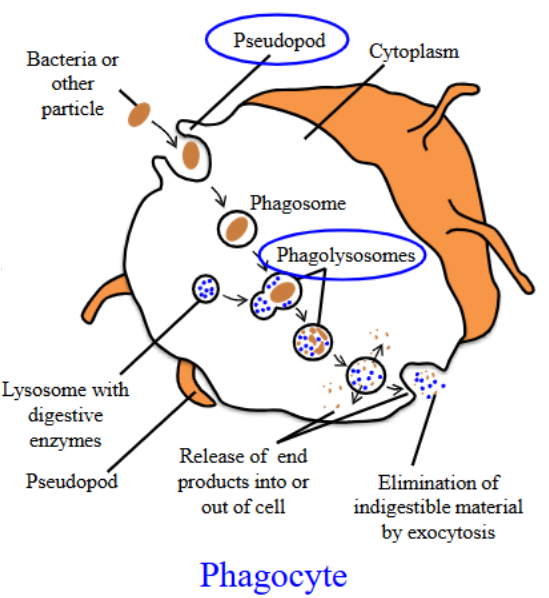
Phagolysosomes
It is the fusion of the phagosome and the lysosome.
Creates a specialized compartment where ingested materials can be destroyed.
The proteolytic enzymes of lysosome can now digest the bacteria/foreign body and destroy it.
Killing by Neutrophils
When neutrophils gather at an inflammation site, their main purpose is to kill bacteria at that site.
Killing by neutrophils can be done in a number of ways.
Oxygen-dependent.
Oxygen-independent.
Oxygen-Dependent Killing
Corrosive oxygen free radical products (can kill any microbe) are synthesized to destroy a foreign body.
Occurs when the neutrophils ingest a foreign body.
Oxygen-Independent Killing
Neutrophils use enzymes to kill bacteria as part of their immune response.
Lysozymes: enzymes that work inside phagolysosomes to degrade entire bacteria by proteolytic breakdown.
Lactoferrin: binds to iron and reduces iron in the environment so bacteria cannot grow.
Defensins: can drive holes into the surface of bacteria, killing the bacteria.
Complement System
A part of the immune system and consists of a series of proteins that interact with one another in a regulated manner to eliminate pathogens.
Made up of distinct, plasma proteins that react with one another to opsonize pathogens to induce a series of inflammatory responses that fights infection.
Complement Proteins
Inactive proteins in plasma (about 30 proteins).
They are activated via proteolytic cleavage and through a cascade.
Results in a large amplified signal and distinction of bacteria.
There are 3 pathways on depend on different molecules for their initiation.
Involved in innate defense.
Classical Pathway
One of the pathways that lead to complement activation.
Binding of a free, circulating antibody to a bacteria as an opsonin can trigger activation.
This can lead to another three pathways: recruitment of inflammatory and immunocompetent cells, opsonization of pathogens, lysis of pathogens.
OIL.
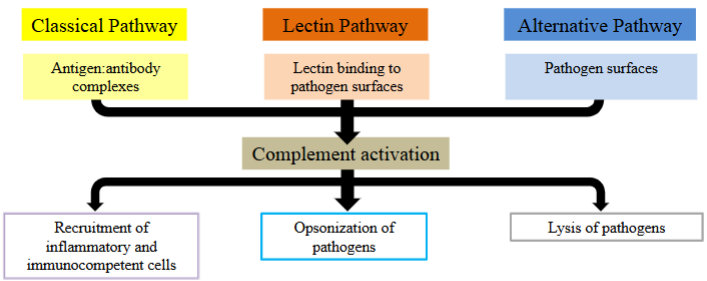
Alternative Pathway
One of the pathways that lead to complement activation.
The presence of bacteria (the pathogen’s surface) can initiate activation by a alternate pathway.
This can lead to another three pathways: recruitment of inflammatory and immunocompetent cells, opsonization of pathogens, lysis of pathogens.
OIL.
Lectin Pathway
The binding of lectin to the surface of bacteria.
This leads to complement activation, which can lead to another 3 pathways.
Recruitment of inflammatory and immunocompetent cells, opsonization of pathogens, lysis of pathogens.
OIL.
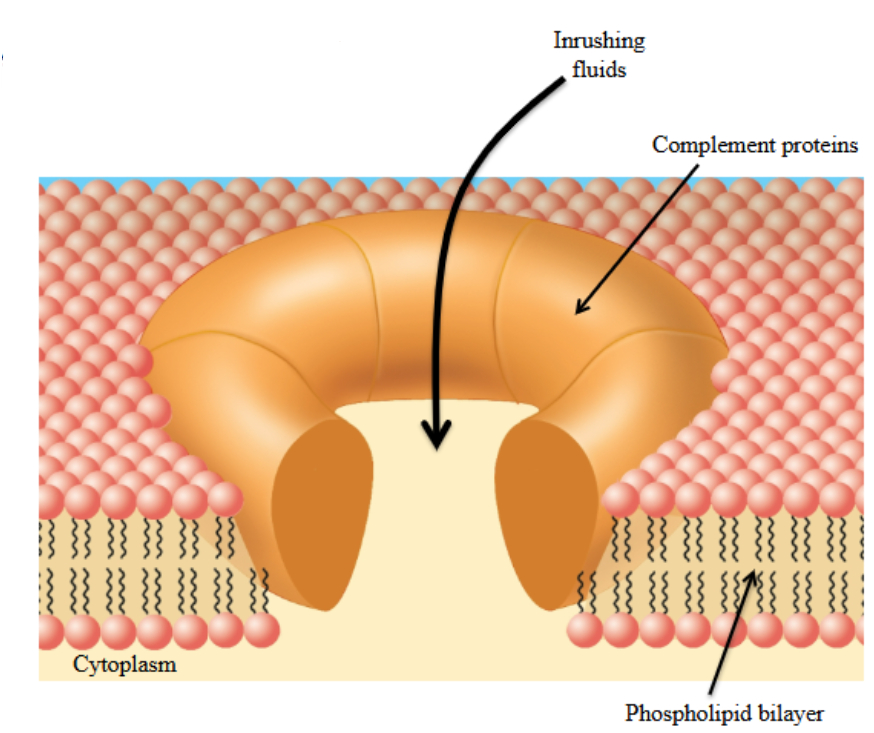
Membrane Attack Complex (MAC)
Complement proteins form a pore in the surface of bacteria.
ECF rushes through the pore into the bacteria, making them susceptible to lysis.
∴ Compromising the lifespan of the bacteria.
The formation of a cluster of activated complement proteins, which come together to form a pore.
Such a event does not happen to our self-cells because we have protective proteins in our body which prevent the formation of attack on our cells.
Primary Lymphoid Tissue
Bone marrow and thymus.
Sites of lymphocyte differentiation and “education.”
Sites where B-Cells and T-Cells are developed, no pathogen exposure.
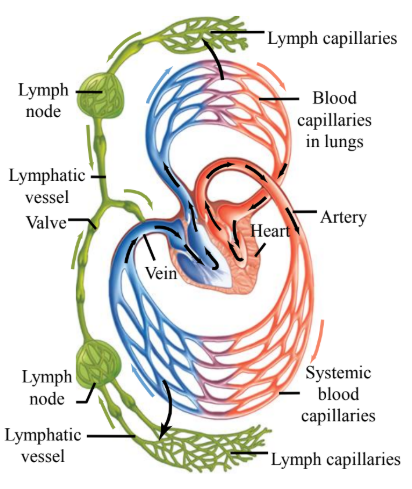
Secondary Lymphoid Tissue
Lymph nodes, etc.
Sites where lymphocytes encounter antigens and become activated.
Where B-Cells and T-Cells mature upon pathogen encounter.
RRR
All lymphocytes (B and T cells) must be able to do the following:
Recognize antigens (foreign agents) in a specific manner.
Respond to antigens (bring about their destruction).
Remember the first encounter with an antigen, so they can better respond if exposed to the same antigen again.